Abstract
Introduction
Plasma levels of amyloid-beta (Aβ) do not correlate well with different stages of Alzheimer's disease (AD) in cross-sectional studies. Measuring the changes in Aβ plasma levels with an acute intervention may be more sensitive to distinguishing individuals in earlier stages of AD (mild cognitive impairment [MCI]) from normal controls.
Methods
A total of 57 participants (18 with AD/MCI and 39 cognitively normal controls) underwent oral glucose tolerance testing (OGTT). Blood samples were obtained over a 2-hour period. Changes in plasma Aβ40 and 42 levels were measured from either baseline or 5 minutes to the 10-minute time-point.
Results
Compared with normal controls, subjects with AD/MCI had significantly less change (Δ) in plasma levels for both Aβ40 (−3.13 [40.93] vs. 41.34 pg/mL [57.16]; P = .002) and Aβ42 (−0.15 [3.77] vs. 5.64 pg/mL [10.65]; P = .004).
Discussion
OGTT combined with measures of plasma Aβ40 and 42 is potentially useful in distinguishing aging individuals who are in different stages of AD.
Keywords: Alzheimer's disease, Blood biomarker, Oral glucose tolerance test
1. Introduction
Alzheimer's disease (AD) is the most common type of dementia in the United States [1]. Thus far, only symptomatic therapies are available, and there is a great need for disease-modifying therapies. The results of recent clinical trials have been disappointing, which has led to a growing interest in clinical trials design and interventions that target early stages of AD [2] such as targeting patients in asymptomatic/preclinical or mild cognitive impairment (MCI) stages. This shift to early stages of AD has underscored the need for validated biomarkers to identify patient populations who will benefit most from a potential therapeutic intervention.
One of the most widely studied biomarkers for AD is amyloid-β (Aβ), thought to be an important protein in the pathogenic cascade of AD [3]. Cerebrospinal fluid (CSF) levels of Aβ42 and Aβ brain imaging measures have been extensively studied for use in clinical trials [4]. Although a blood-based biomarker would be even more widely applicable as it would be less invasive and less costly, most cross-sectional studies of plasma Aβ levels have not been able to show differences between individuals at various stages of AD compared with those of controls [5], [6]. In addition, the utility of plasma Aβ in earlier stages, such as MCI, is less clear [7], [8].
To overcome these limitations, efforts to improve the utility of plasma Aβ levels using an acute intervention to modulate plasma Aβ have been investigated such as using insulin infusion in humans to change plasma and CSF Aβ42 levels [9], [10]. More recently, oral glucose tolerance testing (OGTT) was used to compare AD patients with those with non–AD dementias [11]. However, it is still unknown whether a modulator of Aβ plasma levels, such as OGTT, can be used to distinguish individuals in the earlier stages of AD from those with normal cognitive function. The goal of this study was to assess whether the degrees of change in plasma Aβ40 and 42 levels are different in individuals with MCI/AD compared with those of cognitively normal controls (NC) in response to oral glucose loading.
2. Methods
2.1. Participants
This study was approved by the Johns Hopkins Institutional Review Board. Written informed consent was obtained from all subjects.
The study comprised 57 individuals, two with AD, 16 with MCI, and 39 with normal cognition (Table 1). AD and MCI participants were combined in the analysis (exclusion of the AD subjects did not change the results). Subjects with AD met probable AD criteria by National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disorder and Related Disorder Association. MCI participants had a memory complaint corroborated by an informant, MCI documented in medical or research records, and a clinical dementia rating (CDR) of 0.5. Cognitively, NC had no reported memory impairments by history, a CDR of 0.0, and mini-mental state examination (MMSE) ≥26 or modified MMSE ≥86. Subjects were excluded if they had significant neurologic diseases, liver and renal dysfunction, or history of diabetes or treatment for diabetes.
Table 1.
Baseline characteristics
| Characteristics | Normal (n = 39) |
MCI/AD (n = 18) |
P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Demographics | |||
| Age (y) | 68.2 (6.98) | 70.6 (7.31) | .25 |
| Sex (m, %) | 51.3 | 44.4 | .64 |
| Education (y) | 15.62 (2.37) | 15.28 (3.48) | .71 |
| MMSE | 29.3 (1.41) | 27.7 (2.27) | .01 |
| BMI | 28.23 (4.67) | 26.94 (4.07) | .28 |
| Laboratory values | |||
| Fasting glucose, mg/dL | 94.18 (15.48) | 91.22 (13.31) | .49 |
| Amyloid-β (40), pg/mL | 192.37 (73.79) | 180.11 (75.10) | .57 |
| Amyloid-β (42), pg/mL | 24.73 (23.77) | 17.85 (8.02) | .11 |
| Amyloid-β 42/40 ratio | 0.18 (0.39) | 0.11 (0.04) | .27 |
| Δ Amyloid-β (40), pg/mL | 41.34 (57.16) | −3.14 (40.93) | .002 |
| Δ Amyloid-β (42), pg/mL | 5.64 (10.65) | −0.15 (3.77) | .004 |
Abbreviations: MCI, mild cognitive impairment; AD, Alzheimer's disease; SD, standard deviation; MMSE, mini-mental state examination; BMI, body mass index.
NOTE. Aβ40 and 42 (Δ) values were calculated as the difference between the value at 10 minutes and the maximum value occurring before 10 minutes (at either 0 or 5 minutes).
2.2. Procedures
Subjects were asked to fast for 12 hours before a single early morning study visit. A 20-gauge peripheral intravenous was inserted, and blood was drawn at baseline before drinking a solution containing 75 g of glucose, then at 5, 10, 15, 30, 60, 90, and 120 minutes after drinking the solution.
Blood was collected in EDTA polypropylene tubes for plasma and centrifuged immediately after each collection at 542 relative centrifugal force for 15 minutes at 4°C. Plasma was separated from contact with cells immediately after centrifugation and stored at −80°C until analysis.
ELISA Aβ40 and Aβ42 levels were measured in plasma [6] using the MSD Multi-spot Abeta validated Triplex Assay (Meso Scale Discovery, Gaithersburg, MD, USA), by the Alzheimer's Disease Cooperative Study Biomarker Core using established standard operating procedures [7]. All samples were previously unthawed and run in duplicate. Internal standards were used to control for plate-to-plate variation.
2.3. Statistics
Baseline comparisons were made using two-sample t tests with Satterthwaite's approximation for degrees of freedom. Aβ40 and 42 (Δ) values were calculated as the difference between the value at 10 minutes and the maximum value occurring before 10 minutes (at either 0 or 5 minutes). Logistic regression was performed to adjust for age and body mass index (BMI). All analyses were conducted using STATA (StataCorp LP, TX, USA).
3. Results
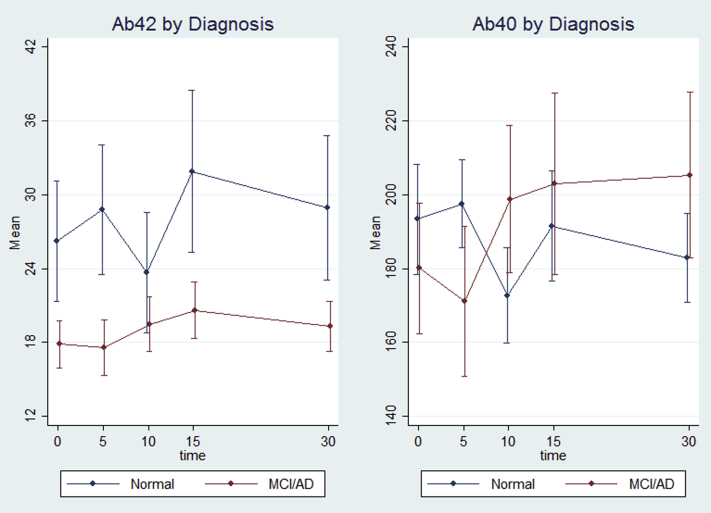
At baseline, no significant between-group differences were observed in age, sex, education, BMI, fasting glucose, baseline plasma Aβ40 and 42 levels, and Aβ42/40 ratios (Table 1). We calculated the change (Δ) in plasma Aβ as the higher level of plasma Aβ from either 0 (baseline) or 5 minutes after ingestion of oral glucose solution to the 10-minute time-point after ingestion. Subjects with AD/MCI had significantly less change (Δ) in plasma Aβ levels compared with that of controls in both Aβ40 (−3.13 [40.93] vs. 41.34 pg/mL [57.16]; P = .002) and Aβ42 (−0.15 [3.77] vs. 5.64 pg/mL [10.65]; P = .004). Characteristic changes (Δ) in plasma Aβ40 and 42 levels are shown in Fig. 1. We also performed sensitivity and adjusted analyses. Nine subjects had well-documented history of depression. Excluding these individuals did not change the differences significantly, with subjects with AD/MCI having less change (Δ) in plasma Aβ40 levels (−3.14 [40.93] vs. 41.73 pg/mL [60.99]; P = .004) and in Aβ42 levels (−0.15 [3.77] vs. 6.38 pg/mL [11.87]; P = .008). Although individuals with prior history of diabetes were excluded from the study, there were two subjects whose glucose levels at baseline (fasting) and 2 hours after OGTT met the American Diabetes Association criteria for type II diabetes on the day of testing. We performed a sensitivity analysis excluding these individuals, and the magnitude of change (Δ) and the inference did not change with Aβ40 (−3.14 [40.93] vs. 42.64 pg/mL [57.55]; P = .001) or with Aβ42 (−0.15 [3.77] vs. 5.75 pg/mL [10.91]; P = .005). In separate logistic regressions of change (Δ) on diagnosis category, the unadjusted odds ratio (OR) for Aβ40 (Δ) was 0.97 (95% confidence interval [CI], 0.94–0.99; P = .01) and for Aβ42 (Δ) was 0.74 (95% CI, 0.57–0.96; P = .02), which means that there is 3% less risk of being in the MCI/AD group for every 1-pg/mL difference in Aβ40 (Δ) and 26% less risk for every 1 pg/mL difference in Aβ42 (Δ). After adjusting for age and BMI, both ORs remained relatively unchanged and statistically significant; the OR for Aβ40 (Δ) was 0.97 (95% CI, 0.94–0.99; P = .008) and for Aβ42 (Δ) was 0.73 (95% CI, 0.56–0.95; P = .02).
Fig. 1.
Characteristic changes (Δ) in plasma Aβ40 and 42 levels in NC (n = 39) compared with the MCI/AD (n = 18) participants. Abbreviations: MCI, mild cognitive impairment; AD, Alzheimer's disease.
4. Discussion
These findings suggest that individuals with MCI/AD have different degrees of change (Δ) in plasma Aβ40 and 42 levels compared with those of cognitively NCs at the 10-minute time-point after an oral glucose load. Although OGTT has been used previously as a modulator of plasma Aβ [11], this study focused on comparing individuals with MCI or in the earlier stages of AD, whereas Takeda et al. [11] focused on comparing individuals with fairly advanced AD to those with non–AD dementias. In addition, our finding shows greater decline in plasma Aβ40 and 42 levels from baseline to 10 minutes in cognitive NCs compared with that of MCI/AD individuals, not evident in the previous study, which examined plasma Aβ levels over a 2-hour period but did not include the 5 or 10-minute time-points [11].
At this time, the mechanism explaining these differences in the change in plasma Aβ level is unclear. It is possible that OGTT modulated plasma Aβ levels by increasing insulin secretion, as insulin is known to increase the level of plasma Aβ42 in AD [10]. However, insulin level does not peak until 60–120 minutes after an OGTT [12], whereas the change in plasma Aβ levels occurred in the first 10 minutes after administration of glucose loading.
Another possible mechanism involves glucagon-like protein-1 (GLP-1), a gastrointestinal hormone which is secreted in response to a meal or after an oral glucose challenge. GLP-1 may be involved in hepatic clearance of Aβ. After production in intestinal cells, GLP-1 is transported to the liver via the portal vein [13], also thought to be the primary route of clearance for Aβ [14]. GLP-1 is also thought to play a role in amyloid precursor protein and Aβ regulation [15]. Although the mechanism remains speculative, both insulin and GLP-1 levels after OGTT will be examined in the future studies to further delineate their roles.
In summary, our study suggests that oral glucose loading as a plasma Aβ level modulator can “unmask” the differences between individuals with MCI/AD versus NCs. This method might be used to complement other existing biomarkers. For example, individuals with normal-like drops in Aβ levels might not be good candidates for further amyloid-oriented investigation via lumbar puncture for CSF collection or amyloid brain imaging in clinical trials or vice-versa. In addition, this method might differentiate those who are “cognitively normal” but already be in the preclinical stages of AD. In the latter case, normals with plasma Aβ changes similar to the MCI/AD group would undergo more invasive amyloid testing. Both scenarios would reduce costs for AD clinical trials, but more importantly, spare individuals less likely to have AD pathology from undergoing unnecessary tests. This would be especially applicable in the developing world where most future AD cases are anticipated but where resources are limited. OGTT has a distinct advantage as a safe, noninvasive, cost-effective, and widely available biomarker that is already being used in clinical settings world-wide.
Research in context.
-
1.
Systematic review: Most cross-sectional studies of plasma amyloid-β (Aβ) have not been able to show differences between individuals at various stages of Alzheimer's disease including mild cognitive impairment stage.
-
2.
Interpretation: Our method of an acute intervention using oral glucose tolerance test (OGTT) to modulate Aβ40 and 42 levels demonstrate that compared to cognitively normal controls, subjects with AD/MCI showed significantly less change (Δ) or drop in Aβ levels between 0 (baseline) or 5 minutes to the 10-minute time-point during the course of an OGTT.
-
3.
Future directions: OGTT combined with measures of plasma Aβ40/42 might be used in the future to determine ideal candidates for interventions that target amyloid along with other existing biomarkers. In addition, due to its current world wide availability, lower cost, and noninvasive nature, this method has the potential to be widely disseminated to developing nations.
Acknowledgments
This study was supported by R21AG0337695 (NIA/NIH), AG038893, MH086881 the Rosalinde and Arthur Gilbert Foundation/AFAR New Investigator Award in Alzheimer's disease, and the Hobson Gift Fund. E.S.O. was also supported by 5KL2RR025006, 1K23AG043504-01 (NIA/NIH), P50 AG005146, the Roberts Gift Fund, the Ossoff Family Fund. This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by grant number UL1 TR 001079 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS, or NIH. The authors thank Dr Pattie Green for her contribution and Shannon Campbell (ADCS Biomarker Core, UCSD) for technical assistance with bioassays.
References
- 1.Alzheimer's Association 2014 Alzheimer's disease facts and figures. Alzheimers Dement. 2014;10:e47–e92. doi: 10.1016/j.jalz.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Sperling R.A., Jack C.R., Jr., Aisen P.S. Testing the right target and right drug at the right stage. Sci Transl Med. 2011;3:111cm33. doi: 10.1126/scitranslmed.3002609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selkoe D.J. Translating cell biology into therapeutic advances in Alzheimer's disease. Nature. 1999;399:A23–A31. doi: 10.1038/399a023. [DOI] [PubMed] [Google Scholar]
- 4.Hampel H., Lista S., Teipel S.J., Garaci F., Nistico R., Blennow K. Perspective on future role of biological markers in clinical therapy trials of Alzheimer's disease: A long-range point of view beyond 2020. Biochem Pharmacol. 2014;88:426–449. doi: 10.1016/j.bcp.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Oh E.S., Troncoso J.C., Fangmark Tucker S.M. Maximizing the potential of plasma amyloid-beta as a diagnostic biomarker for Alzheimer's disease. Neuromolecular Med. 2008;10:195–207. doi: 10.1007/s12017-008-8035-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh E.S., Mielke M.M., Rosenberg P.B., Jain A., Fedarko N.S., Lyketsos C.G. Comparison of conventional ELISA with electrochemiluminescence technology for detection of amyloid-beta in plasma. J Alzheimers Dis. 2010;21:769–773. doi: 10.3233/JAD-2010-100456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donohue M.C., Moghadam S.H., Roe A.D., Sun C.K., Edland S.D., Thomas R.G. Longitudinal plasma amyloid beta in Alzheimer's disease clinical trials. Alzheimers Dement. 2014 doi: 10.1016/j.jalz.2014.07.156. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ritchie C., Smailagic N., Noel-Storr A.H., Takwoingi Y., Flicker L., Mason S.E. Plasma and cerebrospinal fluid amyloid beta for the diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI) Cochrane Database Syst Rev. 2014;6:CD008782. doi: 10.1002/14651858.CD008782.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watson G.S., Peskind E.R., Asthana S., Purganan K., Wait C., Chapman D. Insulin increases CSF Abeta42 levels in normal older adults. Neurology. 2003;60:1899–1903. doi: 10.1212/01.wnl.0000065916.25128.25. [DOI] [PubMed] [Google Scholar]
- 10.Kulstad J.J., Green P.S., Cook D.G., Watson G.S., Reger M.A., Baker L.D. Differential modulation of plasma beta-amyloid by insulin in patients with Alzheimer disease. Neurology. 2006;66:1506–1510. doi: 10.1212/01.wnl.0000216274.58185.09. [DOI] [PubMed] [Google Scholar]
- 11.Takeda S., Sato N., Uchio-Yamada K., Yu H., Moriguchi A., Rakugi H. Oral glucose loading modulates plasma beta-amyloid level in Alzheimer's disease patients: potential diagnostic method for Alzheimer's disease. Dement Geriatr Cogn Disord. 2012;34:25–30. doi: 10.1159/000338704. [DOI] [PubMed] [Google Scholar]
- 12.Meier J.J., Holst J.J., Schmidt W.E., Nauck M.A. Reduction of hepatic insulin clearance after oral glucose ingestion is not mediated by glucagon-like peptide 1 or gastric inhibitory polypeptide in humans. Am J Physiol Endocrinol Metab. 2007;293:E849–E856. doi: 10.1152/ajpendo.00289.2007. [DOI] [PubMed] [Google Scholar]
- 13.Dardevet D., Moore M.C., DiCostanzo C.A., Farmer B., Neal D.W., Snead W. Insulin secretion-independent effects of GLP-1 on canine liver glucose metabolism do not involve portal vein GLP-1 receptors. Am J Physiol Gastrointest Liver Physiol. 2005;289:G806–G814. doi: 10.1152/ajpgi.00121.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kulstad J.J., Savard C.E., Lee S.P., Craft S., Cook D.G. P2–020: Liver-mediated clearance of peripheral amyloid-beta (1-40) Alzheimers Dement. 2006;2:S237–S238. [Google Scholar]
- 15.Perry T., Lahiri D.K., Sambamurti K., Chen D., Mattson M.P., Egan J.M. Glucagon-like peptide-1 decreases endogenous amyloid-beta peptide (Abeta) levels and protects hippocampal neurons from death induced by Abeta and iron. J Neurosci Res. 2003;72:603–612. doi: 10.1002/jnr.10611. [DOI] [PubMed] [Google Scholar]