Abstract
The risk of obesity is reduced when youth engage in recommended levels of physical activity (PA). For that reason, public health organizations in the U.S. have encouraged communities to implement programs and policies designed to increase PA in youth, and many communities have taken on that challenge. However, the long-term effects of those programs and policies on obesity are largely unknown. The Healthy Communities Study (HCS) is a large-scale observational study of U.S. communities that is examining the characteristics of programs and policies designed to promote healthy behaviors (e.g., increase PA and improve diet) and determining their association with obesity-related outcomes. The purpose of this paper is to describe the methods used to measure PA in children and the personal and community factors that may influence it. The study used both self-reported and objective measures of PA, and measured personal, family, and home influences on PA via three constructs: (1) PA self-schema; (2) parental support; and (3) parental rules regarding PA. Neighborhood and community factors related to PA were assessed using three measures: (1) child perceptions of the neighborhood environment; (2) availability of PA equipment; and (3) attributes of the child's street segment via direct observation. School influences on children's PA were assessed via three constructs: (1) school PA policies; (2) child perceptions of the school PA environment; and (3) school outdoor PA environment. These measures will enable examination of the associations between characteristics of community PA programs and policies and obesity-related outcomes in children and youth.
Introduction
Physical activity (PA) has long been recognized as a critical health behavior in children. In the late 19th century, medical and education professionals acknowledged its importance by advocating for physical education (PE) programs in American schools.1 In the mid-20th century, the significance of youth PA was highlighted by President Eisenhower, who founded the President's Council on Physical Fitness.2 And in the 21st century, the importance of PA to the health of American youth was formally recognized in the first federally approved Physical Activity Guidelines for Americans (PAG).3 These include a specific recommendation that youth engage in moderate-to-vigorous PA for at least 60 minutes per day.3 A federal advisory committee's review of the scientific literature on PA and health in children and youth served as the basis for the PAG recommendation.4
The advisory committee recognized that a reduced risk of overweight and obesity is a key health benefit of higher levels of PA. A recent review reinforced this conclusion, finding that PA was one of the few factors consistently associated with preventing excessive weight gain in prospective observational studies of youth.5 Such reports, along with the well-documented impact of PA on energy expenditure,6 have prompted researchers and health organizations to recommend increasing PA as a key strategy in efforts to reduce the prevalence of overweight and obesity in young people. These groups have consistently emphasized the importance of community programs and policies (CPPs) aimed at increasing PA in youth.7–9
Although promoting PA through implementing targeted CPPs is a widely accepted strategy for reducing childhood obesity, the scientific evidence supporting the effectiveness of this approach is limited. The recent PAG Mid-Course Report reviewed a wide range of interventions to promote PA in youth and concluded that only school-based strategies have consistently increased children's PA.10 The report also noted that the long-term effects of such programs on weight status in youth are largely undocumented.10 Accordingly, the design and protocol for the Healthy Communities Study (HCS) places a major emphasis on PA programs and policies. The purpose of this article is to describe the methods used to measure PA and related personal and community factors in children.
Methods
Details on study protocols and procedures are included in Arteaga et al.11 and John and colleagues12 in this issue.
Conceptual Framework for Physical Activity Measures
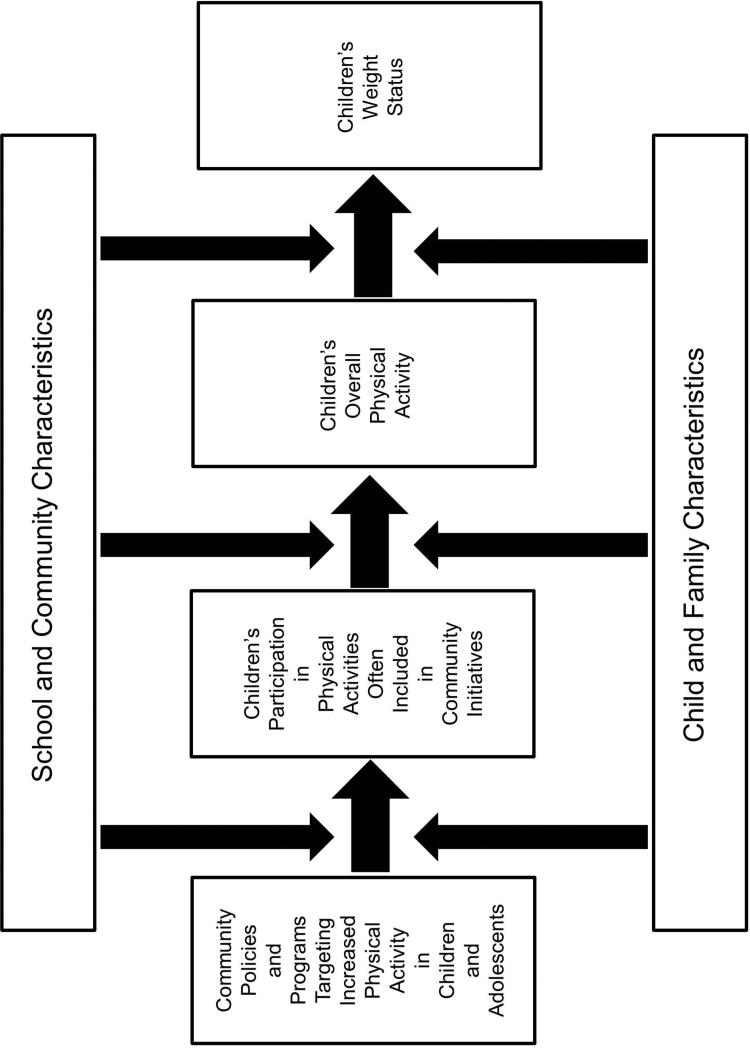
The HCS is examining the characteristics of CPPs designed to promote healthy behaviors (e.g., increase PA and improve diet) and determining their association with obesity-related outcomes.11,12 The PA component of the HCS protocol was designed to measure variables viewed as central to detecting the effects of community-based obesity prevention initiatives that focus on promoting PA in children and adolescents. Figure 1 presents the conceptual framework that guided the selection of the PA measures. A key focus of the protocol was measurement of child- and parent-reported child participation in the types of physical activities and PA programs that are most often implemented in community-based obesity prevention initiatives. In addition, the protocol included measures of key hypothesized community-level influences on child PA, including school characteristics and relevant neighborhood factors. Further, selected child social–cognitive factors and parental/home variables were measured. The HCS also collected information about community initiatives designed to support PA, using key informant interviews conducted by Community Liaisons (CLs). CLs were selected from existing Battelle staff; additional information about the community measures is described in Fawcett et al.13
Figure 1.
Conceptual model guiding the selection of physical activity measures.
Measurement Procedures
Child PA measures were completed as part of the HCS household interview (HHI), which was self-administered on tablet computers during home visits. For the child-report sections of the HHI, children aged 9–15 years were the primary respondents, with parents/guardians asked to assist children aged 9–11 years as needed. For children aged 4–8 years, parents/guardians responded to the questions. School PA measures, including the PE teacher interview and Physical Activity Resources Assessment (PARA), were administered by the CLs in and around participating schools. Both existing instruments and instruments developed for this study were included in the PA measures. The study was approved by the Battelle Memorial Institute IRB, and parents provided written informed consent for their child's participation. A description of the human subjects protections is included in John and colleagues.12
Self-Report of Physical Activity
Physical activity was measured in the full sample of child participants using self-report of participation in selected forms of PA that are hypothesized to be influenced by or intervened on through CPPs. The 7-day Physical Activity Behavior Recall (PABR-7) instrument is designed to elicit information about participation in 14 activities. These include PE, after-school programs, non-school sports, active classes or lessons, and active transport. Using a computer-assisted interview, children or parents/guardians indicated whether or not the child participated in each activity during the past week, the days on which they did the activity, and the average intensity of the activity (light, moderate, hard, very hard). To help with intensity rating, participants viewed cards with gender- and age-specific pictures depicting sample activities at the various intensities.
After answering questions about the 14 activities, participants then responded to additional items about activities completed on the previous day: the duration of the activity (minutes), the intensity, where they did the activity, with whom they did the activity, and the specific activity that was performed. Where, with whom, and specific activity answers were selected from predefined lists with options most common for the specific activity, with the option of adding an “other” response. Selected PA variables and operational definitions are presented in Table 1. Approximately 10% of families completed an enhanced protocol, which included accelerometry as an objective measure of child PA. These participants also responded to a previous-day PABR (PABR-1) during the second home visit. The PABR-1 matched the PABR-7 in layout and administration except that all questions refer to activities performed on the previous day. The PABR-7 and PABR-1 instruments were designed to meet the specific needs of the HCS, and the psychometric properties of the instruments have not been established previously.
Table 1.
Operational Definitions of Selected Physical Activity and Sedentary Behavior Variables Derived from the PABR-7
| Variable | Operational Definition |
|---|---|
| Physical Activity | |
| Participation in specific types of physical activity | Count of activities |
| MVPA Index: Moderate-to-Vigorous PA (Self-report) | Number of moderate-to-vigorous activities reported * frequency of participation in those activities |
| VPA Index: Vigorous PA (Self-report) | Number of vigorous activities reported * frequency of participation in those activities |
| TPA Index: Total PA (Self-report) | Number of activities reported * frequency of participation in those activities |
| MVPA: Volume of Moderate-to-Vigorous PA (Self-report; previous day activities) | Frequency * duration of reported MVPA activities |
| VPA: Volume of Vigorous PA (Self-report; previous day activities)) | Frequency * duration of reported VPA activities |
| TPA: Volume of Total PA (Self-report; previous day activities)) | Frequency * duration of reported Total PA |
| Participation in physical activities in specified settings | Count of activities in each location |
| Participation in physical activities in specified social contexts | Count of activities by group composition (i.e., by self, with one other person, with many people, with class/team) |
| Sedentary Behavior | |
| Participation in specific types of Sedentary Behaviors | Count of activities |
| Sedentary Behavior Index | Number of sedentary activities reported * frequency |
| Volume of Sedentary Behavior (previous day activities) | Frequency * duration of reported sedentary activities |
| Participation in Sedentary Behaviors in specified settings | Count of activities in each location |
| Participation in Sedentary Behaviors in specified social contexts | Count of activities in each group setting |
Self-Report of Sedentary Behavior
The PABR-7 and PABR-1 instruments also included four forms of sedentary behavior. The procedure for reporting sedentary behaviors was similar to that used with the physical activities. Selected sedentary behavior variables and definitions are presented in Table 1.
Objective Measurement of Physical Activity and Sedentary Behavior
Children who completed the enhanced protocol wore an ActiGraph GT3X+ accelerometer for up to 7 days. The accelerometer was attached to a belt and worn around the waist with the monitor over the right hip during all waking hours. The Field Data Collectors (FDCs) asked parents/guardians and children to remove the monitor only when sleeping at night or when it might get wet (swimming, bathing, and showering). Wear during naps and brief exposure to water (sweat or splashes) was acceptable and encouraged.
The accelerometers were initialized to collect triaxial data at an 80-Hz sampling rate beginning at midnight of the day of the first home visit. Accelerometry data will be reduced to daily minutes of light and moderate-to-vigorous intensity PA, as well as daily minutes of sedentary behavior. Operational definitions of PA and sedentary behavior variables are presented in Table 2. Times spent in selected PA intensity categories will be determined by applying the age-specific accelerometry count cut-points used in the National Health and Nutrition Examination Survey (ranges presented in Table 2).14
Table 2.
Operational Definitions of Physical Activity and Sedentary Behavior Variables Derived from Accelerometry
| Variable | Definition |
|---|---|
| Total activity | Daily vector magnitude sum from 3 axes |
| Total physical activity (min/day) | Sum of all wear min w/ Actigraph count values >100 |
| Sedentary behavior (min/day) | Accumulated daily min w/ Actigraph count value ≤100 |
| Light intensity physical activity (min/day) | Accumulated daily min w/ Actigraph count range ≥101 to age-adjusted value (1,400-2,780) |
| Moderate-to-vigorous activity (MVPA) (min/day) | Accumulated daily min w/ Actigraph count values ≥age-adjusted cut-off (1,400-2,780) |
| Vigorous activity (min/day) | Accumulated daily min w/ Actigraph count values ≥age-adjusted cut-off (3,758-6,007) |
| MET-weighted MVPA (MET-min/day)a | Daily MET-weighted minutes of MVPA |
1 MET=3.5 mL O2 kg–1 min–1, which is the rate of energy expenditure at rest. MET-minutes (MET-min)=minutes spent in activity × MET level of the activity.
Personal, Family, and Home Influences on Youth Physical Activity
Studies have identified significant social cognitive and social environmental correlates of youth PA,15 which have been used to guide interventions to assist young people to maintain or increase PA.15,16 They may also serve as important mediators of the effects of CPPs to promote PA in youth. Important correlates identified in the literature include PA self-schema, parental support for PA, and parental rules related to PA and sedentary behavior.
Physical activity self-schema, self-identification as an active or fit person or one who exercises regularly, was assessed with a single item that asked each child to rate your level of PA compared to others of the same age and gender. Responses were recorded on a 5-point Likert scale with endpoints of much less than others to much more than others. This item was adapted from the Amherst Health and Activity Study.17
Parental support for PA was assessed as the weekly frequency with which a member of the child's household provided transportation so the child could participate in PA. This measure was taken from the International Life Sciences Institute national phone survey18 and the Amherst Health and Activity Study.17 The 1-week test–retest reliability for this measure has been shown to be high (r =0.81).19
Items on parental rules were adapted from the Activity Support Scale for Multiple Groups (ACTS-MG).20 The ACTS-MG has been shown to be a valid measure in several racial/ethnic populations.20–22 Parents were asked whether their child is allowed to play outside without adult supervision. Three additional items asked parents if they limited access to sedentary activities (e.g., is the child allowed to play video or computer games as much as he or she would like?). Parental responses were recorded on a 4-point Likert scale ranging from strongly disagree to strongly agree.
Neighborhood/Community Physical Environment
Numerous studies have demonstrated that attributes of the neighborhood environment (e.g., availability of PA facilities, safety) are correlated with PA in young people, though contrary evidence also exists.23–25 To measure children's perceptions of their neighborhood environments, 12 items selected from related studies17,26 were included. These items have been shown to have fair to acceptable test–retest reliability.27 All items were measured on a 4-point scale from disagree a lot to agree a lot. Availability of PA equipment in the home (e.g., basketball hoop, bicycle) also has been shown to positively influence child and adolescent PA.28 Parental reports of availability of equipment in the home and availability of equipment and facilities in the neighborhood were obtained using 11- and 13-item checklists modified from a previous study.29
Attributes of each child's street segment were documented through direct observation using five items from the Neighborhood Attribute Inventory.30,31 The items utilized in the HCS (e.g., measures of physical disorder, including the presence of litter) were chosen because they represent constructs important for PA and have acceptable to high reliability.32,33 To collect the data, an FDC drove a vehicle down the participant's street segment and documented specific attributes of the street segment.
School Influences on Youth Physical Activity
School PA policies and practices were assessed by questionnaire.34 PE teachers responded to questions about PE and fitness testing practices, recess policies, intramural clubs and sports programs, facilities for PA, and professional development. They also reported on the following school policies and practices:
time spent in PE, standards for PE, and physical fitness testing;
school recess requirements and the time spent each day in recess;
types of physical activities in intramural and interscholastic sports programs;
availability of and access to school facilities (e.g., gym, indoor track);
access to school PA facilities by local groups (e.g., recreation department); and
PA professional development opportunities offered to teachers (e.g., information about monitoring PA, fitness testing, and individual PA plans).
An objective of the study is to evaluate whether perceptions of one's environment impact the association between CPPs and children's PA and obesity-related outcomes. Children spend a great deal of time at school, and the school environment may influence the PA behavior of students. Therefore, children's perceptions of their school's PA environment were assessed using four questions in the self-administered PA component of the child survey, which was part of the household interview. Using a 4-point Likert scale, respondents rated their level of agreement/disagreement with the following questions:
My school has non-sports programs for students to be physically active (step team, dance, walk/run club, etc.).
My school has sports teams that you have to try out for.
My school has sports teams where everyone can participate (no try-outs).
I enjoy PE classes at my school.
Respondents had the option to indicate that the PE classes question was not applicable to them. Enjoyment of PE will be treated as a single item.35 The three school activities/sports items were summed to create a school PA index in which a higher score is indicative of a perceived PA-promoting school environment.
The features and quality of outdoor facilities at schools are important for increasing PA levels during school hours36–38 and for increasing use of school grounds outside of school hours.39 To assess the variety and quality of school ground features and amenities and to document evidence of unsociable behaviors (i.e., incivilities), CLs evaluated all outside areas at participating schools using a modified version of the PARA.40 Specifically, observers documented:
the presence or absence and quality of 11 features (e.g., baseball fields);
the presence or absence and quality of 11 amenities (e.g., lighting);
the presence or absence of ten incivilities (e.g., evidence of drug use); and
facility hours, capacity, and size; cost of facility use; and the presence or absence of signs with rules and hours of operation.
Staff Training and Quality Control
The FDCs were responsible for collecting data during a visit to a participating family's home. They were trained to administer the household interview as part of a weeklong in-person session. The training covered interview skills, use of the study's information management system (IMS) and information on each section of the household interview. FDCs completed practice interviews and were certified on all components prior to data collection. Times to complete the interview components were recorded through the IMS and reviewed weekly by the University of South Carolina (USC) Quality Control (QC) lead. Short and long times to complete were flagged, and the Battelle Survey Operations Center followed up with the FDCs. The USC QC team developed monthly summary tables for all PA variables data and reviewed them for out-of-range responses and general spread of the data. The QC team notified the Survey Operations team of any issues it identified, and refresher training for FDCs was delivered as needed. During the initial weeks of data collection, QC leads or staff observed FDCs and provided additional training as needed.
CLs were trained to conduct the PE teacher interview as part of their standardized training on conducting interviews with community personnel. For the PARA, CLs were trained and certified by an investigator at USC who served as the “gold standard.” During in-person training, CLs completed practice observations and certification observations at schools. All CLs were certified at an 80% agreement with the gold standard. During the initial months of data collection, all CLs were visited by a QC lead and observed for inter-rater reliability. All CLs showed >80% agreement with the QC lead during these observations. Additionally, PE teacher and PARA data were reviewed on a monthly basis by the USC QC lead for data completeness, out-of-range responses, and missingness.
Discussion
The protocol for measurement of PA variables in the HCS includes a unique method for assessment of child-level PA behavior. The HCS investigators developed a PA recall instrument for use in this study because the protocol required a focus on forms of PA participation that are typically targeted by CPPs designed to prevent obesity in children and youth. Accordingly, the primary method for assessing child PA involved the child (or a parent/guardian) responding yes or no to queries regarding the child's participation, during the previous seven days, in 14 specific forms of physical activities. For activities performed in the previous week, the child (or parent) reported additional information regarding frequency and intensity of participation. For any activities performed on the previous day, they provided additional contextual and duration information. It is anticipated that the data collected through administration of this protocol will be used in two major ways. First, it will be used to assess, among children in each community, the prevalence of participation in forms of PA. Second, it will be reduced to create metrics that reflect child-level PA behavior (Table 1). The validity of this new instrument has not been established previously. However, because the HCS enhanced protocol provides accelerometry data for approximately10% of participating children, it will be possible to examine the validity of the new self-report instrument versus objectively measured PA.
The HCS PA protocol also draws heavily on instruments that have been used successfully in previous large-scale studies of PA behavior in youth.41,42 These include several measures of school and neighborhood characteristics that are related to children's PA. The school and neighborhood constructs were included in the protocol because of their hypothesized roles as potential mediators and moderators of the effects of community policies and programs on child PA. Through a combination of interviews with school personnel, self-reports by children and parents, and objective assessments of the built environments of the school and neighborhood, the HCS protocol provides a comprehensive assessment of key school and community characteristics.
In summary, the HCS PA protocol includes important strengths and some limitations. A major strength is the selection of measures that collectively allow testing of study hypotheses in a manner that is consistent with the conceptual framework that guided design of the study. However, resource limitations and the need to avoid excessive staff and participant burden precluded inclusion of some potentially useful measures. Among the various child-level social cognitive variables that have been associated with PA, only measures of PA self-schema, parental social support, and parental rules were included in the HCS protocol. Objective assessments of the built environment are limited to observations of school grounds and residential street segments and do not include observations of parks or other community PA resources. However, it is an important strength that the enhanced protocol includes accelerometry, which will provide the basis for comparison of the HCS sample with national norms and with findings of other large-scale studies in which accelerometry has been used as an objective measure of PA.
Supplementary Material
Acknowledgments
The Healthy Communities Study was funded with federal funds from the National Heart, Lung, and Blood Institute, in collaboration with the Eunice Kennedy Shriver National Institute of Child Health and Development, National Institute of Diabetes and Digestive and Kidney Disorders, National Cancer Institute, and NIH Office of Behavioral and Social Sciences Research; DHHS, under Contract No. HHSN268201000041C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Wuest DA, Bucher CA. Historical foundations of physical education and sport. In: Wuest DA, Bucher CA, editors. Foundations of Physical Education and Sport. WCB McGraw-Hill; Boston: 1999. pp. 146–93. [Google Scholar]
- 2.Reiff GG, Dixon W, Jacoby D, Ye G, Spain CG, Hunsicker P. The President's Council on Physical Fitness and Sports National School Population Fitness Survey. University of Michigan; Ann Arbor, MI: 1986. [Google Scholar]
- 3.U.S. DHHS. Physical Activity Guidelines for Americans. 2008 www.health.gov/paguidelines/
- 4.U.S. DHHS. Physical Activity Guidelines Advisory Committee Report, 2008. U.S. DHHS; Washington, DC: 2008. [Google Scholar]
- 5.Pate RR, O'Neill JR, Liese AD, et al. Factors associated with development of excessive fatness in children and adolescents: A review of prospective studies. Obes Rev. 2013;14(8):645–658. doi: 10.1111/obr.12035. http://dx.doi.org/10.1111/obr.12035. [DOI] [PubMed] [Google Scholar]
- 6.Blaak EE, Westerterp KR, Baror O, Wouters LJM, Saris WHM. Total energy expenditure and spontaneous activity in relation to training in obese boys. Am J Clin Nutr. 1992;55(4):777–782. doi: 10.1093/ajcn/55.4.777. [DOI] [PubMed] [Google Scholar]
- 7.IOM. Early Childhood Obesity Prevention Policies. The National Academies Press; Washington, DC: 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.IOM. Preventing Childhood Obesity: Health in the Balance. The National Academies Press; Washington, D.C.: 2005. [PubMed] [Google Scholar]
- 9.IOM. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. The National Academies Press; Washington, DC: 2012. [PubMed] [Google Scholar]
- 10.Physical Activity Guidelines for Americans Midcourse Report Subcommittee, President's Council on Fitness, Sports and Nutrition . Physical Activity Guidelines for Americans Midcourse Report: Strategies to Increase Physical Activity Among Youth. U.S. DHHS; Washington, DC: 2012. [Google Scholar]
- 11.Arteaga SS, Loria C, Carwford PB, et al. The Healthy Communities Study: Its rationale, aims, and approach. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.029. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John LV, Gregoriou M, Pate RR, et al. Operational implementation of the Healthy Communities Study: How communities shape children's health. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.019. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fawcett SB, Collie-Akers VL, Schultz JA, Kelley M. Measuring community programs and policies and their intensity in the Healthy Communities Study. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.027. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. http://dx.doi.org/10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 15.Van Der Horst K, Paw MJ, Twisk JW, Van Mechelen W. A brief review on correlates of physical activity and sedentariness in youth. Med Sci Sports Exerc. 2007;39(8):1241–1250. doi: 10.1249/mss.0b013e318059bf35. http://dx.doi.org/10.1249/mss.0b013e318059bf35. [DOI] [PubMed] [Google Scholar]
- 16.O'Dwyer MV, Fairclough SJ, Knowles Z, Stratton G. Effect of a family-focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act. 2012;9:117. doi: 10.1186/1479-5868-9-117. http://dx.doi.org/10.1186/1479-5868-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sallis JF, Taylor WC, Dowda M, Freedson PS, Pate RR. Correlates of vigorous physical activity for children in grades 1 through 12: Comparing parent-reported and objectively measured physical activity. Pediatr Exerc Sci. 2002;14(1):30–44. [Google Scholar]
- 18.Sallis JF, Prochaska JJ, Taylor WC, Hill JO, Geraci JC. Correlates of physical activity in a national sample of girls and boys in grades 4 through 12. Health Psychol. 1999;18(4):410–415. doi: 10.1037//0278-6133.18.4.410. http://dx.doi.org/10.1037/0278-6133.18.4.410. [DOI] [PubMed] [Google Scholar]
- 19.Trost SG, Sallis JF, Pate RR, Freedson PS, Taylor WC, Dowda M. Evaluating a model of parental influence on youth physical activity. Am J Prev Med. 2003;25(4):277–282. doi: 10.1016/s0749-3797(03)00217-4. http://dx.doi.org/10.1016/S0749-3797(03)00217-4. [DOI] [PubMed] [Google Scholar]
- 20.Davison KK, Li K, Baskin ML, Cox T, Affuso O. Measuring parental support for children's physical activity in white and African American parents: The Activity Support Scale for Multiple Groups (ACTS-MG). Prev Med. 2011;52(1):39–43. doi: 10.1016/j.ypmed.2010.11.008. http://dx.doi.org/10.1016/j.ypmed.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davison KK, Cutting TM, Birch LL. Parents' activity-related parenting practices predict girls' physical activity. Med Sci Sports Exerc. 2003;35(9):1589–1595. doi: 10.1249/01.MSS.0000084524.19408.0C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davison KK, Jago R. Change in parent and peer support across ages 9 to 15 yr and adolescent girls' physical activity. Med Sci Sports Exerc. 2009;41(9):1816–1825. doi: 10.1249/MSS.0b013e3181a278e2. http://dx.doi.org/10.1249/MSS.0b013e3181a278e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferdinand O, Sen B, Rahurkar S, Engler S, Menachemi N. The relationship between built environments and physical activity: A systematic review. Am J Public Health. 2012;102(10):e7–e13. doi: 10.2105/AJPH.2012.300740. http://dx.doi.org/10.2105/AJPH.2012.300740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster S, Giles-Corti B. The built environment, neighborhood crime and constrained physical activity: An exploration of inconsistent findings. Prev Med. 2008;47(3):241–251. doi: 10.1016/j.ypmed.2008.03.017. http://dx.doi.org/10.1016/j.ypmed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 26.Cohen DA, Ashwood S, Scott M, et al. Proximity to school and physical activity among middle school girls: The Trial of Activity for Adolescent Girls study. J Phys Act Health. 2006;3(Suppl 1):S129–S138. doi: 10.1123/jpah.3.s1.s129. [DOI] [PubMed] [Google Scholar]
- 27.Evenson KR, Birnbaum AS, Bedimo-Rung AL, et al. Girls' perception of physical environmental factors and transportation: Reliability and association with physical activity and active transport to school. Int J Behav Nutr Phys Act. 2006;3:28. doi: 10.1186/1479-5868-3-28. http://dx.doi.org/10.1186/1479-5868-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaushal N, Rhodes RE. The home physical environment and its relationship with physical activity and sedentary behavior: A systematic review. Prev Med. 2014;67C:221–237. doi: 10.1016/j.ypmed.2014.07.026. http://dx.doi.org/10.1016/j.ypmed.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 29.Dowda M, Pfeiffer KA, Brown WH, Mitchell JA, Byun W, Pate RR. Parental and environmental correlates of physical activity of children attending preschool. Arch Pediatr Adolesc Med. 2011;165(10):939–944. doi: 10.1001/archpediatrics.2011.84. http://dx.doi.org/10.1001/archpediatrics.2011.84. [DOI] [PubMed] [Google Scholar]
- 30.Caughy MO, O'Campo PJ, Patterson J. A brief observational measure for urban neighborhoods. Health Place. 2001;7(3):225–236. doi: 10.1016/s1353-8292(01)00012-0. http://dx.doi.org/10.1016/S1353-8292(01)00012-0. [DOI] [PubMed] [Google Scholar]
- 31.Laraia BA, Messer L, Kaufman JS, et al. Direct observation of neighborhood attributes in an urban area of the US south: Characterizing the social context of pregnancy. Int J Health Geogr. 2006;5:11. doi: 10.1186/1476-072X-5-11. http://dx.doi.org/10.1186/1476-072X-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Evenson KR, Sotres-Alvarez D, Herring AH, Messer L, Laraia BA, Rodriguez DA. Assessing urban and rural neighborhood characteristics using audit and GIS data: Derivation and reliability of constructs. Int J Behav Nutr Phys Act. 2009;6:44. doi: 10.1186/1479-5868-6-44. http://dx.doi.org/10.1186/1479-5868-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laraia B, Messer L, Evenson K, Kaufman JS. Neighborhood factors associated with physical activity and adequacy of weight gain during pregnancy. J Urban Health. 2007;84(6):793–806. doi: 10.1007/s11524-007-9217-z. http://dx.doi.org/10.1007/s11524-007-9217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CDC. SHPPS Physical Education District Questionnaire. 2006 www.cdc.gov/HealthyYouth/shpps/2006/questionnaires/pdf/physedd2006questionnaire.pdf.
- 35.Barr-Anderson DJ, Neumark-Sztainer D, Schmitz KH, et al. But I like PE: Factors associated with enjoyment of physical education class in middle school girls. Res Q Exerc Sport. 2008;79(1):18–27. doi: 10.1080/02701367.2008.10599456. http://dx.doi.org/10.1080/02701367.2008.10599456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haug E, Torsheim T, Sallis JF, Samdal O. The characteristics of the outdoor school environment associated with physical activity. Health Educ Res. 2010;25(2):248–256. doi: 10.1093/her/cyn050. http://dx.doi.org/10.1093/her/cyn050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sallis JF, Conway TL, Prochaska JJ, McKenzie TL, Marshall SJ, Brown M. The association of school environments with youth physical activity. Am J Public Health. 2001;91(4):618–620. doi: 10.2105/ajph.91.4.618. http://dx.doi.org/10.2105/AJPH.91.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nichol ME, Pickett W, Janssen I. Associations between school recreational environments and physical activity. J Sch Health. 2009;79(6):247–254. doi: 10.1111/j.1746-1561.2009.00406.x. http://dx.doi.org/10.1111/j.1746-1561.2009.00406.x. [DOI] [PubMed] [Google Scholar]
- 39.Colabianchi N, Maslow AL, Swayampakala K. Features and amenities of school playgrounds: A direct observation study of utilization and physical activity levels outside of school time. Int J Behav Nutr Phys Act. 2011;8:32. doi: 10.1186/1479-5868-8-32. http://dx.doi.org/10.1186/1479-5868-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee RE, Booth KM, Reese-Smith JY, Regan G, Howard HH. The Physical Activity Resource Assessment (PARA) instrument: Evaluating features, amenities and incivilities of physical activity resources in urban neighborhoods. Int J Behav Nutr Phys Act. 2005;2:13. doi: 10.1186/1479-5868-2-13. http://dx.doi.org/10.1186/1479-5868-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Webber LS, Catellier DJ, Lytle LA, et al. Promoting physical activity in middle-school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008;34(3):173–184. doi: 10.1016/j.amepre.2007.11.018. http://dx.doi.org/10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Borrud L, Chiappa MM, Burt VL, et al. National Health and Nutrition Examination Survey: National Youth Fitness Survey plan, operations, and analysis, 2012. Vital Health Stat 2. 2014;163:1–24. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.