Abstract
Clear differences are present in men and women’s developmental course of substance use disorders. Whether these sex differences impact substance abuse treatment outcomes is less apparent. The present study investigated sex differences in demographic and intake characteristics and assessed sex, treatment condition, and interactive effects on three treatment outcomes: treatment retention, longest duration of abstinence (LDA), and percent negative samples submitted. Participants (N = 920) were randomized to contingency management (CM) for abstinence or standard care treatment in one of five clinical trials. In terms of pre-treatment characteristics, women reported lower educational achievement and more unemployment, were younger and more likely to submit a positive urine sample at intake, and experienced more problems in employment, drug, family, and psychiatric domains. Men reported more years of alcohol use and significantly higher alcohol and legal problem severity. Men and women stayed in treatment for similar durations of time and had similar abstinence outcomes. No significant sex by treatment condition interactions were present across the three outcomes. These results suggest treatment-seeking substance users in intensive-outpatient settings benefit equally well from CM interventions, regardless of sex.
Keywords: incentives, sex differences, gender, treatment outcome, treatment retention
Prevalence rates of substance use disorders are about double in men compared to women. In the National Epidemiologic Survey on Alcohol and Related Conditions sample, past year and lifetime rates of substance use disorders for men were 2.8% and 13.8%, respectively (Compton, Thomas, Stinson, & Grant, 2007). For women, these rates were significantly lower at 1.2% and 7.1%. Clinical course may vary by sex. Women tend to progress to disordered levels of use more quickly than men (Dawson, 1996; Hernandez-Avila, Rounsaville, & Kranzler, 2004; Lewis, Hoffman, & Nixon, 2014) and enter treatment at a younger age or more quickly relative to men (Bravo, Gual, Lligona, & Colom, 2013; Lewis & Nixon, 2014).
Sex differences in comorbidities are also present. Women with drug use disorders are more likely to meet criteria for lifetime bipolar and alcohol disorders, and less likely to meet criteria for dependent and narcissistic personality disorders, than men after adjusting for socio-demographic characteristics (Goldstein, Dawson, Chou, & Grant, 2012). Related, psychiatric symptoms appear to be worse among women than men presenting to treatment (e.g., Grella, Scott, Foss, Joshi, & Hser, 2003; Green, Polen, Dickinson, Lynch, & Bennett, 2002). Women with substance use disorders also tend to be more disadvantaged than their male counterparts, with lower education levels, more unemployment, and more family problems than their male counterparts (Brady & Ashley, 2005; Goldstein et al., 2012; Najavits & Lester, 2008).
Given the differences between sexes in the development and presentation of substance use disorders, increased attention has been given to the question of whether substance abuse treatment benefits both sexes equally. The data related to treatment outcomes, both in terms of treatment retention and abstinence outcomes, are mixed. While the bulk of studies find no differences in treatment retention (e.g., Devito, Babuscio, Nich, Ball, & Carroll, 2014; Green et al., 2002; Mertens & Weisner, 2000; Wong, Badger, Sigmon, & Higgins, 2002), others suggest that women have lower retention (Arfken, Klein, di Menza, & Schuster, 2001), are less likely to complete treatment (Arfken et al., 2001), and spend fewer days in treatment compared to men (Grella et al., 2003). Brady and Ashley (2005) examined treatment retention in a large nationally representative sample of patients with mixed substance disorders across multiple treatment settings, and both genders stayed in treatment for similar durations. Women were less likely to complete non-methadone outpatient treatment than men, but the relationship did not remain significant when controlling for confounds. Mertens and Weisner (2000) and Green et al. (2002) similarly found no sex differences in retention among outpatients with multiple substance use disorders.
Three studies evaluated gender differences in clinical trials of patients with cocaine use disorders specifically. Devito et al. (2014) and Kosten et al. (1993) conducted pharmacotherapy trials, and Wong et al. (2002) evaluated patients from behavioral trials. None of these studies (Devito et al., 2014; Kosten, Gawin, Kosten, & Rounsaville, 1993; Wong et al., 2002) found a significant main effect of sex on treatment retention, and no interaction effects of sex by treatment condition were present in the two studies that examined these effects (Devito et al., 2014; Wong et al., 2002).
Among the studies finding sex differences in treatment retention, Grella et al. (2003) examined outcomes among individuals in non-methadone programs and found that women spent fewer days in treatment compared to men for the index treatment episode. Arfken et al. (2001) similarly found that women seeking publically-funded treatment in non-methadone inpatient and outpatient settings were less likely to complete treatment (24% versus 46%) and had lower 30-day retention rates (62% versus 75%) compared to men. The opposite finding, that women have better treatment retention compared to men, has also been reported (Bravo et al., 2013; Choi, Adams, Morse, & MacMaster, 2015; Hser, Huang, Teruya, & Anglin, 2003; Hser, Huan, Teruya, & Anglin, 2004).
Type of substance use disorder may also play a role in treatment outcomes. Individuals with substance use problems evidence poorer treatment retention compared to those with alcohol use problems (Brady & Ashley, 2005), but this relationship held only for women and not men in one study (Choi et al., 2015). Others find that these sex effects may be specific to certain substances, such as heroin and cocaine (Arfken et al., 2001).
With respect to substance use outcomes, a mixed pattern of results also emerges. Some reports find equivalent outcomes for men and women (Hser et al., 2003; Garcia-Fernandez et al., 2011; Green, Polen, Lynch, Dickinson, & Bennett, 2004; Grella et al., 2003). Other studies suggest that women have poorer substance use outcomes (Aguiar, Neto, Lambaz, Chick, & Ferrinho, 2012; Archaryya & Zhang, 2003; Devito et al., 2014) and still others (Bravo et al., 2013; Weiss, Martinez-Raga, Griffin, Greenfield, & Hufford, 1997) find that women fare better in terms of reduced substance use or abstinence. Sex may interact with time in terms of treatment response in the first year beyond intake. Using a large mixed diagnosis treatment-seeking sample (N = 10,010) that included 96 inpatient, outpatient, residential, and methadone maintenance programs, Archaryya and Zhang (2003) found that women were significantly more likely to be classified as heavy or very heavy cocaine users at the 1-month in-treatment interview. However, these differences between men and women became smaller and nonsignificant over time through a 12-month follow-up.
Collectively, these studies indicate mixed results in terms of the impact of sex differences on treatment outcomes. The present study examined sex effects of substance abuse treatment in general, and as relates to contingency management (CM) interventions specifically, using a combined sample from five randomized clinical trials (Petry, Alessi, Marx, Austin, & Tardif, 2005; Petry, Barry, Alessi, Rounsaville, & Carroll, 2012; Petry, Weinstock, & Alessi, 2011; Petry et al., 2004; Petry et al., 2006). CM is a behavioral intervention that uses tangible incentives to motivate behavior change. It is efficacious in reducing substance use across a range of substances, including cocaine, opiates, alcohol, nicotine, and marijuana, generating short-term effect sizes in the medium range, especially when appropriate parameters are applied (Benishek et al., 2014; Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Prendergast, Podus, Finney, Greenwell, & Roll, 2006), and yielding the largest effect size of any psychosocial treatment for substance use disorders (Dutra et al., 2008). Meta-analyses (Benishek et al., 2014; Prendergast et al., 2006) suggest CM’s effects are sustained at least for short durations (e.g., 3-months) beyond the removal of the contingencies.
Of the above reports, two studies (Garcia-Fernandez et al., 2011; Wong et al., 2002) examined sex effects in trials involving CM and only one of these examined sex by treatment condition interactions (Wong et al., 2002). Wong et al. (2002) examined sex differences in 188 cocaine dependent outpatients randomized to community reinforcement approach and contingent incentives or a comparison condition. They found that men and women had similar retention rates, reported similar reductions in cocaine use, and submitted similar rates of cocaine positive urinalysis results during treatment with no interactive effects with treatment condition. However, across treatment conditions, women reported more frequent cocaine use at intake and continued to report more days of cocaine use at each assessment through a 12-month follow-up. Another study (Garcia-Fernandez et al., 2011) examined sex as a predictor of end-of-treatment point prevalence abstinence in 50 cocaine dependent outpatients participating in two randomized clinical trials involving community reinforcement approach plus vouchers. Sex was not a significant predictor of cocaine abstinence. These reports suggest no sex effect in CM trials; however, both studies used small samples and may not have been powered to detect sex or sex by treatment condition interactions if present.
This study therefore evaluated main and interactive effects of sex and treatment condition on substance use treatment outcomes using a sizable sample (N = 920). We hypothesized that women and men would differ on baseline characteristics including psychiatric symptoms but may respond equally well to treatment overall. We also evaluated whether sex interacts with treatment condition, such that women may benefit to a greater degree from CM interventions than men. This latter exploratory hypothesis is based on evidence that CM positively impacts psychiatric symptoms (Petry, Alessi, & Rash, 2013) and that women report greater psychiatric severity compared to men.
Methods
Study Design
This study reports results of secondary analyses from five randomized clinical trials (Petry et al., 2004; Petry et al., 2005. Petry et al., 2006; Petry et al., 2011; Petry et al., 2012) comparing CM interventions to standard care (SC) treatment. In all primary trials, participants randomized to CM achieved better treatment outcomes relative to those randomized to SC. The studies assessed the same primary outcomes and assessment measures, were conducted in community clinics, and targeted similar populations (i.e., treatment seeking individuals with substance use disorders). These similarities in methods and design provide a rationale for combining samples, thus providing sufficient power to detect sex effects in secondary analyses if they exist.
Participants
The sample consisted of 920 substance users initiating treatment at 7 community clinics that provided intensive outpatient treatment and who participated in one of five randomized clinical trials (Petry et al., 2004; Petry et al., 2005. Petry et al., 2006; Petry et al., 2011; Petry et al., 2012). The clinics were all located in the New England region and were non-profit community-based clinics that served primarily indigent and uninsured patients. Studies used similar inclusion and exclusion criteria, assessment and outcome measures, follow-up structure, and procedures, which facilitated combining them for secondary analyses. Participants were aged 18 years or older, English-speaking, and met diagnostic criteria for past year substance abuse or dependence (American Psychiatric Association, 1994), with the vast majority cocaine dependent, and most with polysubstance use problems (Table 1). Exclusion criteria included uncontrolled, severe psychiatric problems, inability to understand study procedures, and being in recovery for pathological gambling. Those with severe psychiatric illnesses who were reasonably stable (e.g., not actively suicidal) were not excluded from participation if they met other study criteria. Study procedures were approved by the university Institutional Review Board, and all patients provided written informed consent.
Table 1.
Demographic and Clinical Characteristics of Men and Women Receiving Substance Abuse Treatment
| Men (n = 451) | Women (n = 469) | p-value | |
|---|---|---|---|
| Study, % (n) | .013 | ||
| Petry et al. (2004) | 12 (53) | 14 (67) | |
| Petry et al. (2005) | 14 (65) | 16 (77) | |
| Petry et al. (2006) | 11 (48) | 8 (36) | |
| Petry et al. (2011) | 30 (136) | 22 (103) | |
| Petry et al. (2012) | 33 (149) | 40 (186) | |
| CM condition | 57 (257) | 61 (284) | .271 |
| Race, % (n) | .039 | ||
| African American | 44 (200) | 53 (247) | |
| Caucasian | 40 (181) | 35 (163) | |
| Other | 16 (70) | 13 (59) | |
| Marital status, % (n) | .562 | ||
| Never married | 56 (253) | 57 (266) | |
| Married, remarried, cohabitating | 18 (80) | 15 (70) | |
| Separated/divorced | 25 (111) | 26 (122) | |
| Widowed | 2 (7) | 2 (11) | |
| Employment status, % (n) | <.001 | ||
| Full time | 53 (237) | 31 (143) | |
| Part-time | 20 (92) | 26 (124) | |
| Unemployed | 15 (68) | 35 (162) | |
| Retired/disability | 7 (32) | 6 (29) | |
| Student/controlled environment | 2 (22) | 1 (11) | |
| Intake positive sample, % (n) | 20 (92) | 29 (134) | .004 |
| Cocaine dependent, % (n) | 83 (376) | 87 (407) | .146 |
| Alcohol dependent, % (n) | 56 (251) | 52 (242) | .218 |
| Opiate dependent, % (n) | 28 (122) | 26 (122) | .641 |
| Age | 37.93 (9.60) | 35.60 (8.50) | <.001 |
| Years education | 12.09 (1.93) | 11.76 (2.02) | .011 |
| Years cocaine use | 10.01 (8.38) | 9.61 (7.26) | .437 |
| Years alcohol use | 15.74 (11.03) | 11.86 (9.76) | <.001 |
| Years heroin use (among users) | 7.49 (8.10) | 7.42 (6.86) | .938 |
| ASI scores | |||
| Medical | 0.23 (0.34) | 0.27 (0.36) | .073 |
| Employment | 0.69 (0.29) | 0.78 (0.26) | <.001 |
| Alcohol | 0.24 (0.24) | 0.20 (024) | .016 |
| Drug | 0.15 (0.10) | 0.17 (0.10) | .025 |
| Legal | 0.15 (0.22) | 0.12 (0.20) | .021 |
| Family/social | 0.16 (0.20) | 0.20 (0.23) | .030 |
| Psychiatric | 0.25 (0.23) | 0.30 (0.24) | .001 |
Notes. ASI = Addiction Severity Index. CM = contingency management. Values are means and standard deviations unless otherwise noted.
Procedures
At an initial assessment, participants completed a demographic survey, a diagnostic criteria checklist based on the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1996), and the Addiction Severity Index (ASI; McLellan et al., 1985). The ASI produces composite scores ranging 0.00-1.00 on seven domains: medical, employment, alcohol, drug, legal, family/social, and psychiatric. Higher scores indicate greater problem severity in each domain. Following the intake interview, eligible participants were randomized to treatment condition, described below.
Treatments
All participants received either SC intensive outpatient substance abuse treatment as delivered by the community clinics or the same SC plus CM.
Standard care (SC)
SC was similar across studies and clinics and consisted of intensive outpatient group therapy sessions (up to 5 hr/day) 3-5 times per week for up to 6 weeks. Intensity then gradually tapered in frequency for up to 12 weeks. Aftercare involved one group session per week for up to 12 months. Therapy topics included 12-step treatment, HIV/AIDS education, relapse prevention, and life skills training. In addition to the intensive outpatient therapy as delivered by the clinics, participants submitted up to 24 breath and urine samples during the 12-week study intervention period. Research staff collected and screened samples and encouraged participants to discuss results with clinic staff if they tested positive. However, all data, including breath and urine sample results were considered confidential and were not shared with non-study staff.
Contingency Management (CM)
Participants in CM conditions received the same SC, as described above. In addition, these participants earned reinforcement for achievement of verified target behaviors. The target behaviors differed across study and included abstinence, attendance at treatment sessions, and/or completion of treatment goal-related activities. Magnitude of available reinforcement (range = $80-$874), reinforcement delivery system (prizes versus vouchers), and format (group versus individual) also varied across CM conditions. The primary aims of each study are described briefly below and readers are referred to the original reports for additional details related to study design and treatment conditions. Petry et al. (2004) examined the efficacy of low magnitude CM ($80) or a higher magnitude CM ($240) relative to the SC condition. Petry et al. (2005) varied the delivery system, comparing prize CM versus voucher CM to the SC condition. The Petry et al. (2006) study compared CM for abstinence or CM for goal-related activities to a SC condition. Petry et al. (2011) had only one CM condition, CM delivered in a group setting, which was compared to the SC condition. The Petry et al. (2012) study had two subcomponents based on the participants’ initial urine sample toxicology results. Participants testing negative for cocaine at intake were randomized to CM for abstinence, CM for attendance, or SC. Participants who were cocaine positive at intake were randomized to different magnitude CM for abstinence conditions or the SC condition. For the purposes of these analyses and to enhance uniformity among the CM conditions, we combined all CM conditions targeting abstinence because these conditions improved outcomes relative to SC in all studies and did not differ from one another. Thus, those conditions not targeting abstinence, the 47 individuals randomized to the CM for activities condition in Petry et al. (2006) study and the 107 participants randomized to the CM for attendance condition in Petry et al. (2012) study, were excluded. The remaining sample consisted of 920 participants for analyses.
Data Analysis
We compared men versus women for differences in intake and demographic characteristics using chi-square tests of independence for nominal variables and independent t-tests for continuous variables. We used corrected t values and degrees of freedom when heterogeneous variances were present. Parametric tests were reported given the large sample size and the robust nature of these tests under these conditions (Lumley, Diehr, Emerson, & Chen, 2002).
Primary outcomes included treatment retention (range = 0-12 weeks), longest duration of abstinence (LDA), and percent of negative samples submitted. LDA represents the longest period of abstinence uninterrupted by positive or unexcused samples (range = 0-12 weeks). The percent of negative samples submitted was calculated with the total number of samples submitted in the denominator and the number of negative samples in the numerator (range = 0-100%). In order to receive reinforcement in all the CM conditions, participants’ samples were required to test negative for cocaine, alcohol, and opioids for the Petry (2004, 2005, 2006, 2012) studies. Samples in the Petry et al. (2011) study also had to test negative for methamphetamine. Samples that tested positive for one or more of the targeted substances interrupted the string of abstinence for LDA and were considered positive for the calculation of the percent of negative samples submitted.
The present analyses examined the main effects of sex and treatment condition and their interaction. CM conditions were collapsed and represented by a dichotomous variable indicating randomization to SC or any abstinence CM condition. We examined these effects using analyses of covariance, with the three primary outcomes (treatment retention, LDA, percent negative samples) entered as dependent variables. Covariates included study, age, intake toxicology result, employment status, and ASI drug and medical scores. The ASI drug score was missing for one individual and was replaced with the overall mean prior to analysis. The selected covariates either differed significantly between groups and were related to outcomes, or in the case of ASI medical score and employment status, were judged to be important potential barriers to treatment engagement. Other variables that differed between men and women (see Table 1) were excluded as covariates due to lack of correlation with the outcome variables. For the ANCOVA analyses, we used an alpha of .01 or less for significance to correct for multiple testing. Data analyses were conducted using SPSS (version 21).
Results
Table 1 presents demographic and intake characteristics by sex. The sex distribution differed across studies, with more women participating in the Petry et al. (2012) study than the others. A higher percentage of women (53%) were African American compared to men (44%). Employment status also differed significantly, with more women unemployed (35% for women versus 15% for men) and fewer reporting full-time employment (31% for women versus 53% for men). More women submitted samples positive for alcohol, stimulants, or opioids at their intake visit (29% versus 20% in men). Men were older, had more years of education, more years of alcohol use, and reported greater problem severity in alcohol and legal domains on the ASI. Women reported more severe problems with employment, drug, family/social, and psychiatric issues on the ASI. No differences between men and women were present for marital status, years of cocaine or heroin use, percent meeting dependence diagnoses, ASI medical scores, or percent randomized to CM.
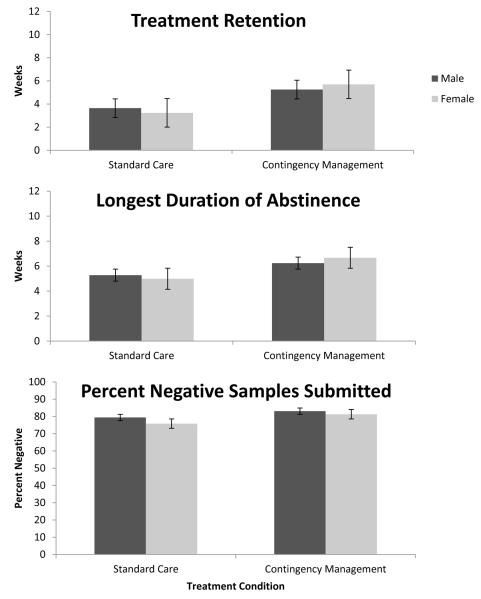
In terms of treatment outcomes, study and intake toxicology result were significantly associated with retention, ps < .01 (data not shown, available from authors). After controlling for covariates, the main effect of treatment condition was significant, F(1, 909) = 25.78, p < .001, η2 = .028; participants assigned to CM (M = 6.45, SE = 0.17) stayed in treatment about 1 week longer than those randomized to SC (M = 5.13, SE = 0.20). Sex was not significantly associated with retention, F(1, 909) = 0.08, p = .78, η2 < .001, nor was the interaction of sex and treatment condition, F(1, 909) =1.91, p = .17, η2 = .002.
For LDA, a similar pattern emerged for the main and interaction effects. Significant effects were found for age, intake toxicology result, and ASI drug score, ps < .01 (data not shown; available from author) and treatment condition, F(1, 909) = 65.65, p < .001, η2 = .067. Participants randomized to CM (M = 5.47, SE = 0.16) achieved about 2 additional weeks of abstinence on average relative to those in SC treatment (M = 3.44, SE = 0.19). Again, no effects were present for sex, F(1, 909) = 0.01, p = .92, η2 < .001, or the sex by treatment condition interaction F(1, 909) = 2.82, p = .09, η2 = .003.
Percent negative samples submitted was related to intake toxicology result and ASI drug scores, ps < .01 (data not shown; available from authors), as well as treatment condition, F(1, 909) = 8.44, p = .004, η2 = .009. CM participants (M = 82.20%, SE = 1.00) submitted higher percentages of negative samples compared to those in SC (M = 77.66%, SE = 1.19). For this outcome, neither the main effect of sex, F(1, 909) = 2.71, p = .10, η2 = .003, nor the interaction were significant, F(1, 909) = 0.33, p = .56, η2 < .001. Men (M = 81.26%, SE = 1.13) achieved a similar percentage of negative samples submitted compared to women (M = 78.59%, SE = 1.12).
Discussion
These secondary analyses examined sex differences in treatment outcomes in a large sample of individuals seeking intensive-outpatient treatment for substance use disorders at community clinics throughout New England. Consistent with prior reports (Arfken et al., 2001; Green et al., 2002; Grella et al., 2003; Mertens & Weisner, 2000), women evidenced higher problem severity across a number of domains at intake. Despite these differences, men and women responded equally well to intensive outpatient treatment in general, and to CM specifically, across three treatment outcomes: treatment retention, longest duration of abstinence, and the percent of negative samples submitted. Patients randomized to CM achieved better treatment outcomes across all three measures compared to standard care alone. These results match those of Wong et al. (2002) and Garcia-Fernadez et al. (2011) who found no significant main effects of sex on primary treatment outcomes. Contrary to our hypothesis, no interaction effects of sex and treatment condition were present for any of the three outcomes. These results and those of Wong et al. (2002) suggest men and women similarly benefit from CM in these samples.
Our findings add to the extant literature (e.g., Brady & Ashley, 2005; Devito et al., 2014; Mertens & Weisner, 2000; Wong et al., 2002) indicating that men and women stay in outpatient treatment for similar durations of time. Despite greater problem severity across multiple domains that could impact continued treatment participation including lower education and greater family, employment and psychiatric concerns (e.g., Arfken et al., 2001; Green et al., 2002; Grella et al., 2003; Mertens & Weisner, 2000), women tend to stay in outpatient treatment as long as men once they initiate care. Our results indicated that men and women have similar abstinence outcomes as well.
Women in our sample and another (Wong et al., 2002) were more likely to submit positive urine or breath samples at intake. Intake toxicology results are strong predictors of treatment retention and abstinence outcomes and indicative for more severe and persistent substance use problems (Stitzer et al., 2007); however, few studies examining differences in intake characteristics of men and women report results of initial urine toxicology samples. In future studies, it will be important to assess sex effects on treatment outcome after controlling for this well-known predictor of outcome, as done in this study. Despite this indication of more severe baseline substance use, women still achieved similar retention and abstinence outcomes during treatment.
Consistent with prior studies (Green et al., 2002; Grella et al. 2003; Hser et al., 2003; Wong et al., 2002), women also reported higher rates of unemployment and lower education levels. ASI scores indicated greater severity of problems for women in the employment, drug, family/social, and psychiatric domains. Men had more severe scores for alcohol and legal domains. More severe legal issues and criminal justice involvement have been reported elsewhere (Arfken et al., 2001; Grella et al., 2003; Mertens & Weisner, 2000) for men seeking treatment for substance use disorders. On the other hand, psychiatric and family problems are more commonly documented among women (Arfken et al., 2001; Green et al., 2002; Grella et al., 2003; Mertens & Weisner, 2000).
This study’s use of a large, heterogeneous sample, broad inclusion criteria, limited exclusion criteria, and use of multiple studies, community-based clinics, and CM protocols, supports the generalizability of these findings. Another strength of this report is the use of objective indices of substance use in determining treatment outcome. Prior studies (Aguiar et al., 2012; Archaryya et al., 2003; Green et al., 2002; Grella et al., 2003) have relied primarily on self-reported abstinence, with some exceptions (Hser et al., 2003; Wong et al., 2002), and there is some evidence that women and men differ in the reliability of their self-report of substance use (Magura, Nwakeze, Rosenblum, & Joseph, 2000).
Given the nature of secondary analyses, some variables potentially important to treatment response, such as childcare responsibilities, perceptions about treatment, and subjective indicators of response to treatment (e.g., treatment satisfaction), were not assessed. Future studies examining these constructs may provide greater insight of the associations with sex differences in treatment outcomes. Additionally, this study did not evaluate sex differences in long-term substance use outcomes, nor did it address barriers to treatment initiation. Another limitation is that these data were collected over a period of a decade (Petry et al., 2004; Petry et al., 2005. Petry et al., 2006; Petry et al., 2011; Petry et al., 2012), and individuals seeking treatment for substance use disorders may have changed over time. Future studies may be needed to assess sex differences as the treatment seeking population, as well as treatment settings and care provided, continue to shift in response to changing needs.
Despite these limitations, this study adds to the existing literature on sex differences in response to substance abuse treatment in general and in response to CM. Women present with more severe psychosocial problems when initiating treatment, but men and women stay in treatment for similar durations and achieve similar abstinence outcomes while in treatment. Both men and women responded equally well to CM treatments. Men and women in this study present to treatment with very different challenges and problem areas. Future research might investigate whether treatments that attend to sex-specific needs, e.g., education, unemployment, and comorbidity needs in women, and legal concerns in men, would enhance treatment response for both sexes.
Figure 1.
Mean treatment retention (0-12 weeks), longest duration of abstinence (LDA; 0-12 weeks), and percent of negative samples (0-100%) by sex and treatment condition. Values are adjusted means and standard errors. Significant main effects of treatment condition were present for all three outcomes (p < .001). Main effects of sex and the interaction of sex by treatment condition were not statistically significant for any of the outcomes. Main effects of treatment condition were significant for all three outcomes.
Acknowledgements
Funding for this research and report preparation was provided by National Institutes of Health grants: P30-DA023918, R01-DA027615, R21-DA031897, R01-DA018883, P50-DA09241, P60-AA03510, R01-DA024667, R01-HD075630, R01-AA021446, DP3-DK097705, M01-RR06192.
Footnotes
Disclosures
All authors contributed to the manuscript and have read and approved the final manuscript.
The authors report no conflicts of interest.
References
- Acharyya S, Zhang H. Assessing sex differences on treatment effectiveness from the Drug Abuse Treatment Outcome Study (DATOS) American Journal of Drug & Alcohol Abuse. 2003;29:415–444. doi: 10.1081/ada-120020524. [DOI] [PubMed] [Google Scholar]
- Aguiar P, Neto D, Lambaz R, Chick J, Ferrinho P. Prognostic factors during outpatient treatment for alcohol dependence: Cohort study with 6 months of treatment follow-up. Alcohol & Alcoholism. 2012;47:702–710. doi: 10.1093/alcalc/ags097. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual for mental disorders. 4th ed Author; Washington, DC: 1994. [Google Scholar]
- Arfken CL, Klein C, di Menza S, Schuster CR. Gender differences in problem severity at assessment and treatment retention. Journal of Substance Abuse Treatment. 2001;20:53–57. doi: 10.1016/s0740-5472(00)00155-0. [DOI] [PubMed] [Google Scholar]
- Benishek LA, Dugosh KL, Kirby KC, Matejkowski J, Clements NT, Seymour BL, Festinger DS. Prize-based contingency management for the treatment of substance abusers: A meta-analysis. Addiction. 2014;109:1426–1436. doi: 10.1111/add.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady TM, Ashley OS. Women in substance abuse treatment: Results from the Alcohol and Drug Services Study (ADSS) (DHHS Publication No. SMA 04-3968, Analytic Series A-26) Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2005. [Google Scholar]
- Bravo F, Gual A, Lligoña A, Colom J. Gender differences in the long-term outcome of alcohol dependence treatments: An analysis of twenty-year prospective follow up. Drug & Alcohol Review. 2013;32:381–388. doi: 10.1111/dar.12023. [DOI] [PubMed] [Google Scholar]
- Choi S, Adams SM, Morse SA, MacMaster S. Gender differences in treatment retention among individuals with co-occurring substance abuse and mental health disorders. Substance Use & Misuse. 2015 doi: 10.3109/10826084.2014.997828. Advance online publication. doi: 10.3109/10826084.2014.997828. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Dawson DA. Gender differences in the probability of alcohol treatment. Journal of Substance Abuse. 1996;8:211–225. doi: 10.1016/s0899-3289(96)90260-6. [DOI] [PubMed] [Google Scholar]
- DeVito EE, Babuscio TA, Nich C, Ball SA, Carroll KM. Gender differences in clinical outcomes for cocaine dependence: Randomized clinical trials of behavioral therapy and disulfiram. Drug & Alcohol Dependence. 2014;145:156–67. doi: 10.1016/j.drugalcdep.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165:179–87. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbin M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders- Clinician version. American Psychiatric Press; Washington, DC: 1996. [Google Scholar]
- Garcia-Fernandez G, Secedas-Villa R, Garcia-Rodriguez O, Alvarez-Lopez H, Sanchez-Hervas E, Fernandez-Hermida JR, Fernandez-Artamendi S. Individual characteristics and response to contingency management treatment for cocaine addiction. Psicothema. 2011;23:114–118. [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, Grant BF. Sex differences in prevalence and comorbidity of alcohol and drug use disorders: Results from wave 2 of the National Epidemiologic Study on Alcohol and Related Conditions. Journal of Studies on Alcohol & Drugs. 2012;73:938–950. doi: 10.15288/jsad.2012.73.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Polen MR, Dickinson DM, Lynch FL, Bennett MD. Gender differences in predictors of initiation, retention, and completion in an HMO-based substance abuse treatment program. Journal of Substance Abuse Treatment. 2002;23:285–295. doi: 10.1016/s0740-5472(02)00278-7. [DOI] [PubMed] [Google Scholar]
- Green CA, Polen MR, Lynch FL, Dickinson DM, Bennett MD. Gender differences in outcomes in an HMO-based substance abuse treatment program. Journal of Addictive Diseases. 2004;23:47–70. doi: 10.1300/J069v23n02_04. [DOI] [PubMed] [Google Scholar]
- Grella CE, Scott CK, Foss MA, Joshi V, Hser Y-I. Gender differences in drug treatment outcomes among participants in the Chicago Target Cities Study. Evaluation & Program Planning. 2003;26:297–310. [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug & Alcohol Dependence. 2004;74:265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Huang Y-C, Teruya C, Anglin MD. Gender comparisons of drug abuse treatment outcomes and predictors. Drug & Alcohol Dependence. 2003;72:255–264. doi: 10.1016/j.drugalcdep.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Huang Y-C, Teruya C, Anglin MD. Gender differences in treatment outcomes over a 3-year period: A path model analysis. Journal of Drug Issues. 2004;34:419–439. [Google Scholar]
- Kosten TA, Gawin FH, Kosten TR, Rounsaville BJ. Gender differences in cocaine use and treatment response. Journal of Substance Abuse Treatment. 1993;10:63–66. doi: 10.1016/0740-5472(93)90100-g. [DOI] [PubMed] [Google Scholar]
- Lewis B, Hoffman LA, Nixon SJ. Sex differences in drug use among polysubstance users. Drug & Alcohol Dependence. 2014;145:127–133. doi: 10.1016/j.drugalcdep.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis B, Nixon SJ. Characterizing gender differences in treatment seekers. Alcohol: Clinical & Experimental Research. 2014;38:275–284. doi: 10.1111/acer.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health datasets. Annual Review of Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- Lussier J, Heil S, Mongeon J, Badger G, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Magura S, Nwakeze PC, Rosenblum A, Joseph H. Substance misuse and related infectious diseases in a soup kitchen population. Substance Use & Misuse. 2000;35:551–583. doi: 10.3109/10826080009147472. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffity J, Evans F, Barr HL, O’Brien CP. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous and Mental Diseases. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Weisner CM. Predictors of substance abuse treatment retention among women and men in an HMO. Alcoholism: Clinical & Experimental Research. 2000;24:1525–1533. [PubMed] [Google Scholar]
- Najavits LM, Lester KM. Gender differences in cocaine dependence. Drug & Alcohol Dependence. 2008;97:190–194. doi: 10.1016/j.drugalcdep.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierra S. Contingency management treatments: Reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology. 2006;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardif M. Vouchers versus prizes: Contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Rash CJ. Contingency management treatments decrease psychiatric symptoms. Journal of Consulting and Clinical Psychology. 2013;81:926–931. doi: 10.1037/a0032499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Barry D, Alessi SM, Rounsaville BJ, Carroll KM. A randomized trial adapting contingency management targets based on initial abstinence status of cocaine-dependent patients. Journal of Consulting and Clinical Psychology. 2012;80:276–85. doi: 10.1037/a0026883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treating cocaine users: How low can we go, and with whom? Addiction. 2004;99:349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Alessi SM. A randomized trial of contingency management delivered in the context of group counseling. Journal of Consulting and Clinical Psychology. 2011;79:686–696. doi: 10.1037/a0024813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Petry N, Peirce J, Kirby K, Killeen T, Roll J, Li R. Effectiveness of abstinence-based incentives: Interaction with intake stimulant test results. Journal of Consulting & Clinical Psychology. 2007;75:805–11. doi: 10.1037/0022-006X.75.5.805. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Martinez-Raga J, Griffin ML, Greenfield SF, Hufford C. Gender differences in cocaine dependent patients: A 6 month follow-up study. Drug & Alcohol Dependence. 1997;44:35–40. doi: 10.1016/s0376-8716(96)01319-1. [DOI] [PubMed] [Google Scholar]
- Wong CJ, Badger GJ, Sigmon SC, Higgins ST. Examining possible gender differences among cocaine-dependent outpatients. Experimental & Clinical Psychopharmacology. 2002;10:316–323. doi: 10.1037//1064-1297.10.3.316. [DOI] [PubMed] [Google Scholar]