To the editor
Thrombotic thrombocytopenic purpura (TTP) is an uncommon disorder caused by a congenital or acquired deficiency of ADAMTS13, a Von Willebrand Factor cleaving serine protease. Generally, the focus on treatment of TTP has been on management of acute episodes since these were almost invariably fatal prior to the advent of plasma exchange. With plasma exchange, mortality has decreased from >90% to approximately 15%. The increasing use of corticosteroids and Rituximab with plasma exchange has led to a decrease in the duration of plasma exchange needed to induce remission and hence plasma exchange-related complications. Recovery from TTP has generally been considered complete except for a significant risk of relapse, particularly within the first year after diagnosis. However, recent reports have suggested that survivors of TTP have a high incidence of hypertension, renal insufficiency, persistent cognitive deficits, depression, poorer quality of life and higher than expected mortality [1–3]. We conducted this retrospective cohort analysis to determine the prevalence of chronic kidney disease (CKD), hypertension, depression, stroke and other psychiatric and neurologic conditions during long term follow up in survivors of TTP.
We identified 100 consecutive with a clinical diagnosis of TTP of which 57 had documented ADAMTS13 activity <5%. The latter were included in the study cohort and were followed until death or date of last clinical contact. Clinical and laboratory data as well as information concerning clinical outcomes including death, relapse, CKD (serum creatinine > 2 mg/dl or greater than 1.5 times baseline persisting for at least 3 months), hypertension (two blood pressure measurements greater than 140/90 mmHg or the initiation of anti-hypertensive therapy), diabetes mellitus (single hemoglobin A1C value of > 6.5%), stroke (new neurologic deficits persisting for > 7 days with a documented cerebrovascular event on brain MRI), depression (started on antidepressant medications and a psychiatrist or primary care physician documented a diagnosis of major depression) were extracted from the electronic medical record. A one way chi-squared test was used to compare period prevalence of the study outcomes with expected rates in the reference United States population obtained from 6 cycles of the National Health and Nutrition Examination Survey (NHANES) data (2001–2012) adjusted for age and sex. All analyses were performed using SPSS version 20 (IBM corp., USA) and significance was set at a p-value of 0.05.
The median patient age was 45 years (range 16–79 years) and 38 (66.7%) were female. Additional information on patient characteristics is provided in the supporting information. All patients were treated with plasma exchange and 48(84%) received concurrent corticosteroids. Patients were followed for a median period of 59 months (range 10–117 months). Four (7%) patients died during an acute episode of TTP and 11(19.3%) suffered relapses. At initial presentation, 10 (19.4%) of survivors (n=53) had a preexisting diagnosis of hypertension, 3 (5.6%) had CKD, 4 (7.5%) had major depression, and 4 (7.5%) had a diagnosis of stroke (patients with stroke during the course an acute TTP episode were included). Over the follow up period, the number of patients affected by hypertension increased to 20 (39.6%), stroke to 7 (13.2 %), CKD to 10 (18.8%) and depression needing pharmacologic treatment to 10 (18.8%).
The period prevalence of hypertension (39.6% versus 29.8%, p=0.044), stroke (13.2% versus 1.81%, p=0.007), and depression requiring pharmacologc treatment (18.8% versus 6.1, p=0.016) were significantly higher in TTP survivors compared with an age and sex matched reference US population. The prevalence of CKD (18.8% versus 16.8%, p=0.077) was not significantly higher than that of the reference population. We also noted a significant rate of other mental health disorders such as anxiety (n=9), bipolar disorder (n=1), and conversion disorder (n=1). Figure 1 shows the rates of these morbidities in TTP survivors compared with the reference population.
Figure 1.
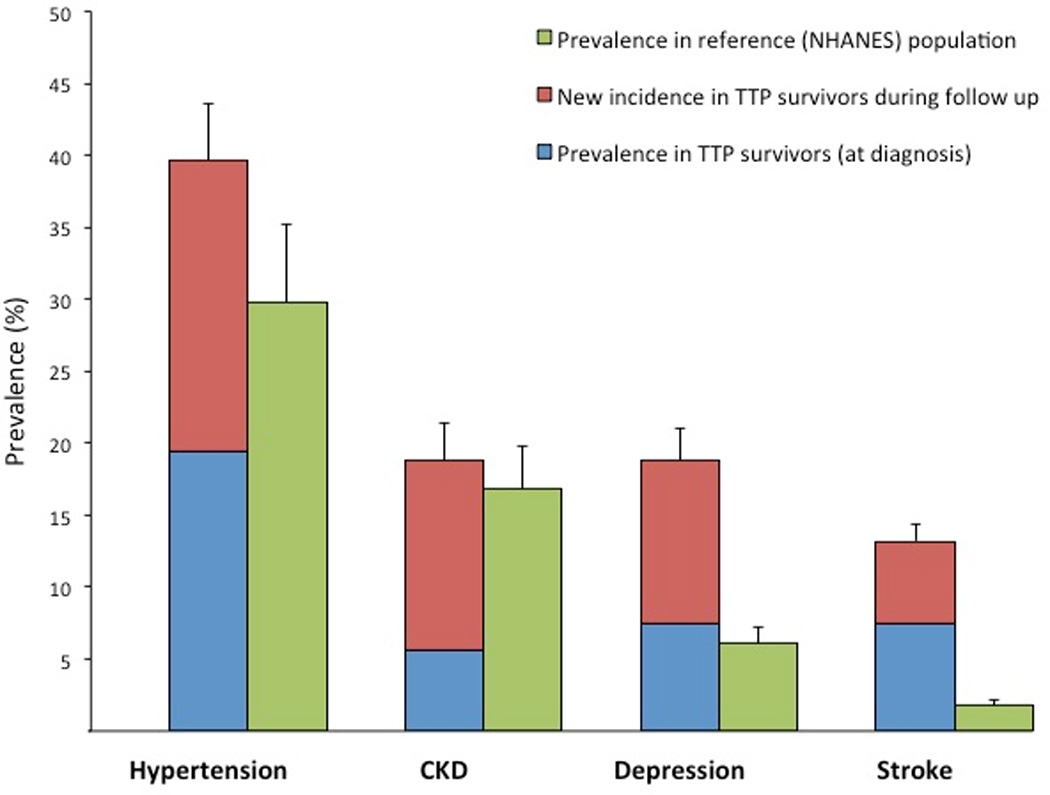
Prevalence of morbidity outcomes in TTP survivors over a median follow up of 59 months compared with reference United States population (data from NHANES database).
Other recent studies suggest that TTP survivors are a vulnerable population with higher rates of chronic morbidities such as hypertension, renal insufficiency, depression, systemic lupus, obesity and overall and poor quality of life. In a recent cohort study of 57 survivors of TTP, Deford et al described higher than expected rates of hypertension (40%), major depression (19%) and SLE (12%) [1]. Similar to our findings, other investigators have reported higher rates of depression and psychiatric illnesses as well as increased rates of fatigue and problems with concentration and memory [2,3].
There are several possible explanations for these findings. First, microvascular ischemia during acute episodes of TTP may cause persistent organ damage. Second, although the course of ADAMTS13 activity after recovery from TTP is poorly understood, persistently low activity may play a role in microvascular thrombosis by increasing levels of ultra-large Von Willebrand factor multimers and enhanced platelet aggregation. Lower ADAMTS13 activity has been documented in patients with ischemic cerebrovascular accidents, myocardial infarction, and hypertensive crises [4,5] The high prevalence of depression and psychiatric morbidities may, in part, be attributable to the psychological effects and sequelae of a life-threatening illness, a phenomenon that well documented in intensive care unit survivors [6].
In conclusion, we demonstrate that survivors of TTP have high rates of chronic morbidities such as hypertension, depression, stroke and chronic renal disease that limit quality of life, and ultimately survival. This highlights the need for continued follow up to address these negative health consequences in a timely manner. Further studies into the pathogenesis of these outcomes, including the role of ADAMTS13 and VWF, are warranted.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to recognize the contributions of the clinicians who cared for these patients. This work was supported in part by NIH HL123416 (to KRM).
REFERENCES
- 1.Deford CC, Reese JA, Schwartz LH, et al. Multiple major morbidities and increased mortality during long-term follow-up after recovery from thrombotic thrombocytopenic purpura. Blood. 2013;122:2023–2029. doi: 10.1182/blood-2013-04-496752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falter T, Alber KJ, Scharrer I. Long term outcome and sequelae in patients after acute thrombotic thrombocytopenic purpura episodes. Hamostaseologie. 2013;33:113–120. doi: 10.5482/HAMO-12-11-0019. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy AS, Lewis QF, Scott JG, et al. Cognitive deficits after recovery from thrombotic thrombocytopenic purpura. Transfusion. 2009;49:1092–1101. doi: 10.1111/j.1537-2995.2009.02101.x. [DOI] [PubMed] [Google Scholar]
- 4.De Meyer SF, Stoll G, Wagner DD, Kleinschnitz C. von Willebrand factor: an emerging target in stroke therapy. Stroke. 2012;43:599–606. doi: 10.1161/STROKEAHA.111.628867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsukawa M, Kaikita K, Soejima K, et al. Serial changes in von Willebrand factor-cleaving protease (ADAMTS13) and prognosis after acute myocardial infarction. Am J Cardiol. 2007;100:758–763. doi: 10.1016/j.amjcard.2007.03.095. [DOI] [PubMed] [Google Scholar]
- 6.Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2:369–379. doi: 10.1016/S2213-2600(14)70051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


