Abstract
Purpose
Quantitative fluoroscopy is an emerging technology for assessing continuous inter-vertebral motion in the lumbar spine, but information on radiation dose is not yet available. The purposes of this study were to compare the radiation dose from quantitative fluoroscopy of the lumbar spine with lumbar spine radiographs, and identify opportunities for dose reduction in quantitative fluoroscopy.
Methods
Internationally reported dose area product (DAP) and effective dose data for lumbar spine radiographs were compared with the same for quantitative fluoroscopy and with data from a local hospital for functional radiographs (weight bearing AP, lateral, and/or flexion and extension) (n = 27). The effects of procedure time, age, weight, height and body mass index on the fluoroscopy dose were determined by multiple linear regression using SPSS v19 software (IBM Corp., Armonck, NY, USA).
Results and conclusion
The effective dose (and therefore the estimated risk) for quantitative fluoroscopy is 0.561 mSv which is lower than in most published data for lumbar spine radiography.
The dose area product (DAP) for sagittal (flexion + extension) quantitative fluoroscopy is 3.94 Gy cm2 which is lower than local data for two view (flexion and extension) functional radiographs (4.25 Gy cm2), and combined coronal and sagittal dose from quantitative fluoroscopy (6.13 Gy cm2) is lower than for four view functional radiography (7.34 Gy cm2).
Conversely DAP for coronal and sagittal quantitative fluoroscopy combined (6.13 Gy cm2) is higher than that published for both lumbar AP or lateral radiographs, with the exception of Nordic countries combined data.
Weight, procedure time and age were independently positively associated with total dose, and height (after adjusting for weight) was negatively associated, thus as height increased, the DAP decreased.
Keywords: Flexion-extension, Spine kinematics, Low back pain, Inter-vertebral, Continuous motion, Movement disorders
Introduction
Quantitative fluoroscopy (QF) of the lumbar spine allows inter-vertebral motion to be measured from fluoroscopic sequences where trunk motion is standardised for velocity and range. Sequences can be recorded using passive recumbent (i.e. no muscle or motor control) or active weight-bearing protocols in both the coronal and sagittal planes. Automated frame-to-frame image registration relies upon good digital image quality and provides continuous inter-vertebral rotational and translational data, giving more information about the function of the spine than AP, lateral, or flexion-extension (functional) radiographs.1,2
Functional radiographs have long been used for measuring spinal movement and for diagnosing instability.3 However, such measurements are unreliable due to errors from positioning, distortion and magnification, with mean test-retest errors of up to 4.9° 4 By contrast, QF is reported to be accurate to 0.32° for coronal, and 0.52° for sagittal plane inter-vertebral rotation5 with inter-observer errors below 1.5° for rotation and 1.5 mm for translation.6–9
QF technology is mainly limited to research, although a new system for clinical use has recently gained 510(K) clearance from the United States Food and Drug Administration (KineGraph VMA, Ortho Kinematics, Austin, Texas, USA).10 However, few authors have published radiation dose data and none have compared these to published data from radiographic images. The present study sought to provide this, with suggestions for further optimising radiation doses by analysis of the characteristics which contribute to dose.
The aim was to determine if quantitative fluoroscopic investigation of the lumbar spine imparts a similar dose-area product (DAP) and effective dose (ED) to lumbar spine radiographs. To determine this, published data for AP and lateral radiographs were interrogated. Because no published data exists for functional radiographs, local hospital data were used to represent this dose for comparison. A secondary aim was to determine which factors may contribute to a reduction of the dose from quantitative fluoroscopy.
Methods and materials
This was a retrospective study comparing the radiation dose from an on-going QF study with AP and lateral lumbar spine radiographs, functional radiographs, and other QF studies. The comparisons were Dose Area Product (DAP) measured in Gray multiplied by area (Gy cm2) and the estimated effective dose (ED) measured in miliSievert (mSv).
Published dose data
National and international surveys,11–15 and peer reviewed scientific literature reporting radiation doses of lumbar spine radiographs and quantitative fluoroscopy/cineradiography/video-fluoroscopy were examined.5,9,16–20 Literature was excluded if only entrance skin doses (ESD's) were reported leaving six references reporting DAP values and eight reporting effective dose. DAP and ED were extracted and compared to the dose from QF in this study.
Quantitative fluoroscopy
Ethical approval was obtained from the UK National Research Ethics Committee Southampton A (09/H0502/99). Recruitment of all participants and theirwritten informed consent were carried out by the principal researcher prior to screening. QF was undertaken in the recumbent coronal and sagittal planes, in a cross-sectional mixed gender study (n = 74) of in vivo lumbar spine biomechanics, and movement was controlled by a specially designed motorised motion table (Fig. 1). Data collection was undertaken by the principal researcher using a portable digital C-arm fluoroscope with a 30 cm Image Intensifier (Siemens Avantic, Germany), and a pulse rate of fifteen frames per second was selected to minimise movement blurring.
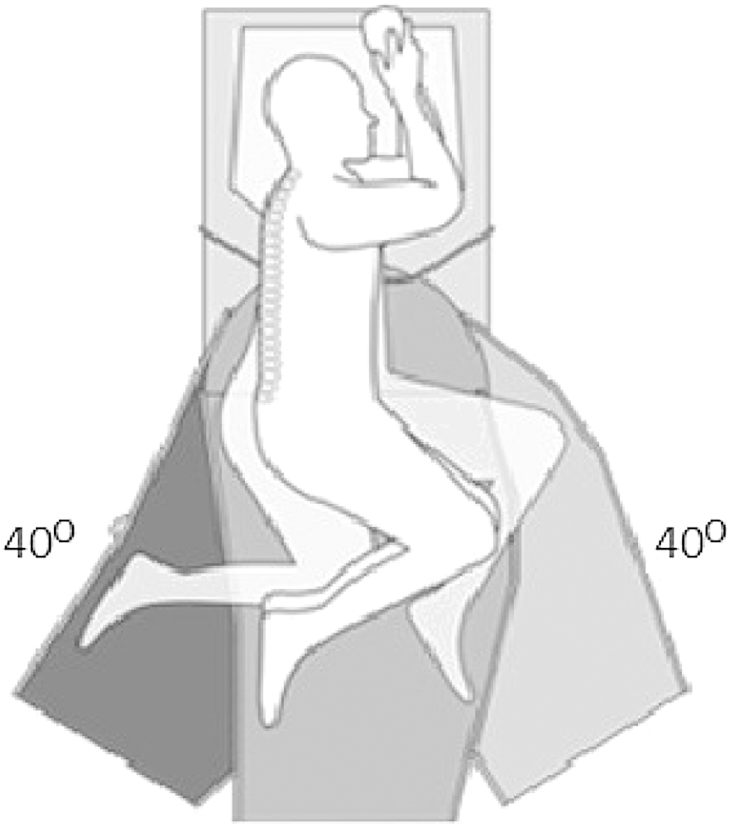
Figure 1.
Diagram of the passive motion table for QF of the lumbar spine. Patients lie in either a supine or lateral decubitus position with L3 centred to the fulcrum with knees bent to flatten the lumbar lordosis. The table swings through an arc of 40° each way.
DAP, procedure time, age, gender, height and weight of the participants was obtained. DAP was then converted to ED using PCXMC v2 software(stuk.fi) and 2007 ICRP 103 tissue weighting factors.21 For QF, The mean kVp was 67 for coronal and 79 for sagittal plane, and the mean focus skin distances (FSD) were 75 cm and 60 cm respectively.
Hospital radiographs
A local hospital database of referrals by spinal surgeons for functional radiographs was inspected. The search covered the previous 12-month period and the cumulative DAP was recorded for patients who had a four series examination (weight-bearing AP, lateral, flexion and extension) or a two series examination (weight-bearing flexion and extension). The collection of retrospective hospital dose data did not require ethical review; however hospital and radiology department R&D approvals were gained.
No identifying details were recorded and patients who had images that were repeated were excluded, as were those who only had supine AP and lateral lumbar radiographs. Examinations were undertaken by different practitioners using the same room equipped with a GE Medical Systems DEFINIUM 8000 System. ED was estimated using generalised conversion coefficients from the NRPB-R262 report22 (see Table 2).
Table 2.
DAP and effective (ED) radiation dose data for QF recumbent sagittal and coronal plane sequences and weight bearing AP, lateral, flexion and extension radiographs from a local hospital database.
| Coronal QF (n = 74) | Sagittal QF (n = 74) | Total QF (n = 74) | Radiographic views 4 series (weight-bearing AP, lateral, flexion and extension) (n = 15) | Radiographic views 2 series (weight-bearing flexion and extension) (n = 12) | |
|---|---|---|---|---|---|
| kVp Mean(SD) | 66.99 (4.25) | 79.09 (8.95) | 73.04 (9.26) | 90 | 90 |
| DAP Gy cm2 Mean (SD) | 2.19 (0.78) | 3.94 (0.86) | 6.13 (1.5) | 7.34 (4.4) | 4.25 (1.98) |
| ED mSv Mean (SD) | 0.321 (0.115) | 0.24 (0.529) | 0.561 (0.154) | – | 2.2 (2.1) |
| Procedure time (seconds). Mean (SD) | 36.08 (3.52) | 39.27 (4.55) | 75.35 (6.11) | – | – |
Statistical analysis
For QF, the relationships between DAP (outcome variable) and procedure time, age, gender, height, weight and body mass index (BMI) (predictor variables) were examined. A 2-sided 5% significance level was used. Initially, a least squares linear regression (IBM SPSS Statistics Version 19) of total dose was conducted to calculate unadjusted regression and correlation coefficients. Next, a multiple linear regression model including only height, weight and BMI determined whether all 3 variables independently predicted dose. Large changes in the standard errors of the regression coefficients from values seen in the unadjusted analyses were used to identify collinearity.
A variety of different models containing different combinations of these three predictor variables were also run, using adjusted R-squared values to help choose the best. From this, the best anthropometric variables were chosen and included with all the other remaining predictor variables in a single regression model. Variables that were not statistically significant were dropped from the analysis in order to obtain a parsimonious model. Adjusted regression (95% CI) and partial correlation coefficients of all statistically significant variables in the resultant model are presented.
Results
Demographics
Table 1 summarises the participant demographics for QF (n = 74) and functional radiographic studies (n = 27).
Table 1.
Demographics of participants imaged with QF versus local hospital data of weight-bearing lumbar radiographs (2 or 4 series) for instability.
| This QF study |
Local hospital |
|
|---|---|---|
| N = 74 | N = 27 | |
| Gender (%) | Male = 42 (57%) Female = 32 (43%) |
Male = 11 (41%) Female = 16 (59%) |
| Age years. Mean (SD) | 36.9 (8.49) | 63.2 (17.2) |
| Weight Kg. Mean (SD) | 74.97 (12.73) | – |
| Height m. mean (SD) | 1.716 (0.127) | – |
| BMI mean (SD) | 24.77 (2.57) | – |
QF and lumbar spine radiation doses
Data from the functional radiographs were separated into 2 view (n = 12) and 4-view series (n = 15). The mean kVp, DAP and effective doses, along with the same from QF, are summarised in Table 2. The mean age at which patients had functional radiography (63 years) was much higher than the participants in this study (37years). The age of the functional radiographic sample is indicative of the population in the local area, whereas the QF study participants were limited to an age range of 20–51 years.
Dose Area Product (DAP)
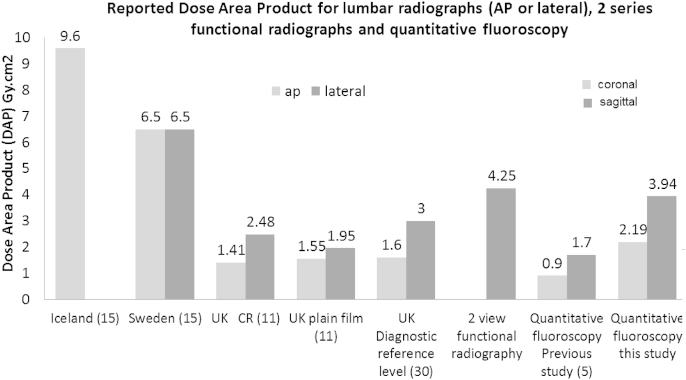
Fig. 2 shows the internationally published DAPs for lumbar spine radiographs compared to two series functional radiography, one previous QF lumbar spine study, and the mean DAP for coronal and sagittal QF in this study.
Figure 2.
The reported DAP of AP and lateral lumbar spine radiographs compared to quantitative fluoroscopy and local data for 2 view (flexion and extension) functional radiographs.
DAP data for separate coronal or sagittal QF studies (2.19 Gy cm2 (SD 0.78) 3.94 Gy cm2 (SD 0.86) respectively) were higher than UK dose reference levels AP (1.6 Gy cm2) and lateral (3 Gy cm2) lumbar radiographs, whereas sagittal QF was lower than local data for functional radiographs two view series (4.25 Gy cm2) and lower than data reported from Sweden (6.5 Gy cm2).
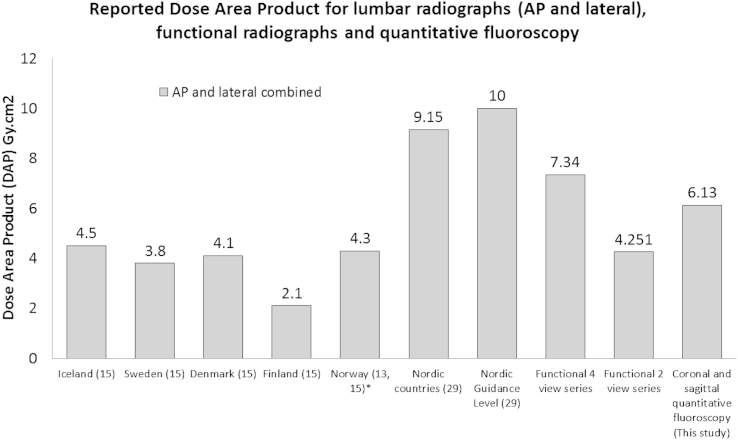
When combined (coronal and sagittal, Fig. 3), DAP for QF (6.13 Gy cm2) was smaller than combined Nordic countries (9.15 Gy cm2) and the Nordic guidance level (10 Gy cm2). Conversely DAP for QF was higher than individual Nordic countries data; however data for the latter were reported 10 years later than the combined data, which may reflect updates in practice and equipment. Combined QF is lower than four view functional radiography (7.34 Gy cm2) which is the examination it is comparable with in the USA.23
Figure 3.
The reported DAP of combined lumbar spine radiographs (AP + lateral) compared to quantitative fluoroscopy and local data for functional radiographs. *Data for Norway has been reported as 4.2 Gy cm2 and 4.4 Gy cm2 in two separate references. The average of 4.3 Gy cm2 is shown here.
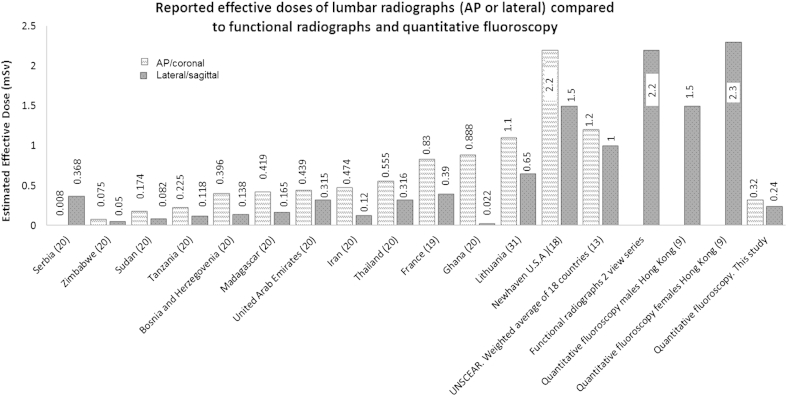
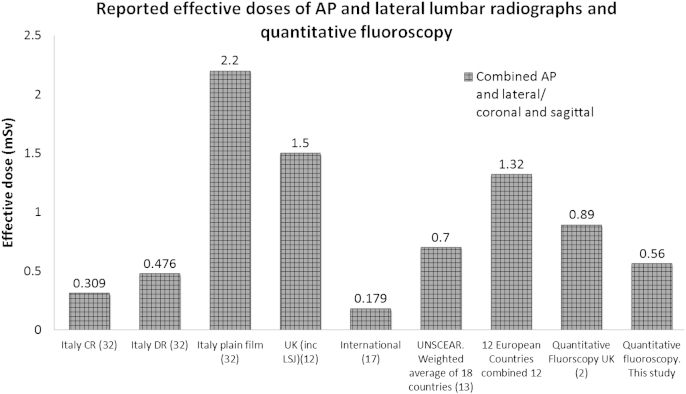
Comparison of effective dose (ED)
Fig. 4 shows that the effective doses for QF coronal (0.32 mSv) or sagittal (0.24 mSv) were less than the estimated ED for 2 view functional radiographs (2.2 mSv) and the weighted average for AP and lateral lumbar spine radiographs across 18 countries (1.2 mSv and 1 mSv respectively)13. In comparison with individual countries, ED for coronal QF was less than that reported for AP lumbar spine radiographs in 9/12 regions, and for sagittal QF the ED was less in 5/12 regions.
Figure 4.
Reported effective dose for lumbar spine radiographs (AP or lateral) compared to quantitative fluoroscopy.
ED data for lumbar radiographs (Figs. 4 and 5) comes from international sources where there is greater variation in the number of radiographs that make up the series. Additionally these studies did not quote their conversion coefficients which may have influenced the resultant estimation; hence a margin of error is expected when interpreting these comparisons.
Figure 5.
The effective dose of combined lumbar spine radiographic series compared to quantitative fluoroscopy and local data for functional radiographs.
One previous QF study undertaken in Hong Kong9 reported an ED of 1.5 mSv for males and 2.3 mSv for females. No other exposure factors were reported but these estimates are between 1 and 2 mSv higher than the EDs in this study.
Fig. 5 shows the reported EDs for AP and lateral radiographs combined, a previous report from QF in 2011,2 and QF in this study. The EDs from this study are lower than the QF data reported in 2011 where the imaging technique was similar but the sample size was smaller. When combined the ED for QF is again lower than the averages of 18 countries.13
Relationship of patient characteristics to QF dose
Inspection of the histogram and the result from the Kolmogorov–Smirnov test (p = 0.30) suggested that it was reasonable to assume that total dose was normally distributed. Unadjusted regression and correlation coefficients relating potential predictors to DAP are shown in Table 3. All variables were significantly associated with total dose. The regression model of total dose against height, weight and BMI displayed substantial collinearity so not all could be included. A model containing weight and height together had a larger adjusted R squared (69%) than BMI alone (56%), and slightly larger adjusted R squared than BMI and height together (67%) and BMI and weight together (68%). Thus BMI was dropped from subsequent models. The effect of gender on total dose appears to be explained by height and weight differences. The remaining statistically significant variables are shown in Table 3. Increased average total dose was associated with greater age, longer procedure time, increased weight and smaller height (after weight is taken into account). The partial correlation coefficients suggest that, of the predictors of total dose, the association is greatest for weight. The adjusted R squared for this final model was 82%.
Table 3.
Linear regression analyses of total absorbed dose on potential predictor.
| Predictor | Unadjusted regression coefficient (95% CI) p-value | Correlation | Adjusted regression coefficient for parsimonious model (95% CI) p-value | Partial correlation |
|---|---|---|---|---|
| Age (years) | 6.03 (2.14, 9.92) p = 0.003 | 0.34 | 3.64 (1.79, 5.49) p < 0.001 | 0.43 |
| Procedure time (min) | 9.30 (3.98, 14.62) p < 0.001 | 0.38 | 8.47 (5.96, 10.97) p < 0.001 | 0.63 |
| Weight (kgs) | 9.56 (7.90, 11.22) p < 0.001 | 0.80 | 11.83 (9.77, 13.90) p < 0.001 | 0.81 |
| BMI (Kgs/m2) | 43.62 (34.67, 52.57) p < 0.001 | 0.75 | A | |
| Height (m) | 829.46 (508.06, 1150.87) p < 0.001 | 0.52 | −543.24 (−814.5, −271.97) p < 0.001 | −0.43 |
| Sex (M relative to F) | 149.15 (87.98, 210.32) p < 0.001 | NA | B |
Regression coefficients represent mean change in total dose (cGy cm2) per unit increase in predictor.
NA – sex is a nominal variable so Pearson's correlation not presented.
A – BMI excluded because of collinearity with weight and height.
B – Effect of sex explained by height, weight and other variables when added to the model (p = 0.87).
Discussion
There is large variation in methods and reporting of dosage data in existing literature which is reflected in the conflicting results presented here. However we can confidently say that the mean effective dose for QF in this study was less than 1 mSv. When undertaking research involving ionising radiation the risk to the individual versus societal benefit must be considered. A dose of less than 1 mSv places this research in the International Commission for Radiological Protections (ICRP) category of ‘IIa Intermediate’ which means the risk to the individual is minor and the benefit to society is intermediate to moderate.24 Alternatively stated, the risk of inducing cancer from 1 mSv is 1:20 00025 which is in addition to the lifetime risk of 1:3 .26 The mean background radiation dose received annually in the UK is 2.7 mSv27 thus the mean effective dose of 0.561 mSv from QF is equivalent to approximately 11 weeks' background radiation.
When considering risks to health from radiation, epidemiological evidence currently states that there is insufficient statistical power to detect excess carcinomas for doses below 100 mSv,28 although a more recent editorial summarised the evidence on the health effects of low level radiation29 and agreed that it remains prudent to stay within the linear no threshold (LNT) model and adhere to the ALARA principle because it is possible for a single radiation track to cause significant DNA changes.30
Considering dose reduction strategies for QF, patient weight appears to be the strongest predictor, followed by procedure time. It is interesting to note the statistically significant correlation between age and dose which cannot be explained by other factors in the model. The negative association between height and total dose after adjusting for weight can be explained by the fixed field of radiation exposure during the procedure. That is, people of the same weight but greater height will have less of their bodies within the field.
Implications for clinical practice
Quantitative fluoroscopy has advanced our understanding of the biomechanics of the spine and it can be used with any portable image intensifier, a motion platform, and bespoke tracking software. This technique is currently being adopted in some centres in the USA23 and could be used to replace functional radiographs without adding to the medical radiation burden. However QF has an examination time of 15 min for one plane of motion which is longer than functional radiographs. Hence departments would need to consider the extra information gained in light of the increased examination time.
Quantitative fluoroscopy ensures that trunk movement is highly standardised to reduce inter and intra subject variation, hence all participants were bent to 40°, rather than their maximum voluntary trunk bend. Adopting the standardisation of trunk movement in functional radiography would advance upon the current technique by reducing inter and intra subject variation. However not bending to the maximum may not stress inter-vertebral segments sufficiently to establish a diagnosis of radiological instability, thus if standardisation of trunk motion was to be adopted, revised normative values would also be required.
Limitations
Studies reporting effective dose did not give details of their standard radiographic series or conversion coefficients so these comparisons are provided as an overview. The ED for 2 series functional radiographs was estimated using generalised coefficients22 because of the limited retrospective data available, however it is acknowledged that they are less accurate than those used for QF. Additionally the sample size for functional radiography is small and limited to one site; hence it is unlikely to be representative of the dose received from functional radiographs, it is presented here as an introduction and a suggestion that further research could examine radiation doses received from functional radiographs.
It is acknowledged that comparing QF (dynamic) with published AP and lateral (static) lumbar radiographs is not ideal, as the image quality and clinical indications differ. However it is necessary to show that new and emerging medical technologies are at least equal to, if not superior to, existing examinations and thus the nearest proxy data for radiation dosage was used.
The effective doses for QF in this study were calculated using Monte Carlo simulation software (PCXMC) and used the latest tissue weighting factors21 with an assumed constant field size of 30 cm × 30 cm. In practice, collimation was used throughout ensuring the field size was smaller than this and thus the EDs reported here are likely to be overestimated.
Options for further dose reduction
QF reduces the intra- and inter-subject variation in lumbar spine kinematics which allows for better comparisons of populations. Linear regression/correlation showed that QF procedure time had a significant correlation with DAP. Therefore, since range and velocity are controlled, increasing the velocity of the trunk motion should lead to a reduction in procedure time and thus a reduction in dose. However this needs to be carefully balanced against motion blurring which would render the objective automated tracking templates ineffective.
Another way to reduce dose from QF would be to reduce the pulse rate. The method currently in use employs a rate of 15 fps however the system in use in the USA employs a pulse rate of 8 fps. If the motion output is equally accurate and reproducible with the pulse rate halved, then it could be safely reduced.
As patients' weight increases so too does the amount of scatter which degrades the image quality upon which the QF tracking algorithms depend. One way of reducing the collective dose to patients undergoing QF would be to impose a maximum weight limit. In some diagnostic centres maximum weight limits are already imposed for CT and MRI although this is mainly for logistical reasons. However when undertaking QF, tracking algorithms are likely to fail if image quality is poor hence in larger participants there would be no benefit to those who exceed a certain weight limit if the tracking algorithms fail. However, further analysis would be needed to determine what that weight limit may be. In the present study a BMI limit of 30 was imposed due to the maximum output capacity of the mobile C arm.
Conclusion
Quantitative fluoroscopy of the lumbar spine has a similar radiation dose to AP, lateral and functional radiographs. Because QF can provide more reliable and comprehensive information about inter-vertebral motion, which improves the clinical decisions about the functional integrity of the spine, this technique could be used as a replacement for functional radiographs without an increase in radiation dose.
However QF requires careful standardisation of patient movement and bespoke tracking algorithms which are essential for accuracy and reliability. Hence its wider adoption within clinical departments will require careful management. However this technique has already been adopted in the U.S.A. and work is underway to improve its accessibility in the U.K.
Finally, caution is advised when referring to published studies comparing radiation dose because of the variation in methods used to both obtain the image, and calculate effective dose. It is therefore recommended that this paper should only be used to compare the order of magnitude of the radiation dose between QF and other lumbar spine radiography.
Role of the funding source
Funding for this study was received from the National Institute for Health Research (CATCDRF09) under the Clinical Academic Training Doctoral Research Fellowship scheme. This article presents independent research. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
This study is registered on the UK Clinical Research Network: Portfolio database, UKCRN Study ID: 11478.
Conflict of interest
None.
Acknowledgements
The authors wish to acknowledge the contributions of the participants, Alex Breen for software development and support, Linda Bruce for her help with recruitment, and the Radiology department at Poole Hospital Foundation Trust UK for their help in providing data.
Contributor Information
F.E. Mellor, Email: imrci.fmellor@aecc.ac.uk, mellorfiona@gmail.com.
P. Thomas, Email: PThomas@bournemouth.ac.uk.
A. Breen, Email: imrci.abreen@aecc.ac.uk.
References
- 1.Mellor F.E., Muggleton J.M., Bagust J., Mason W.M.A., Thomas P.W., Breen A.C. Midlumbar lateral flexion stability measured in healthy volunteers by in-vivo fluoroscopy. Spine. 2009;34(22):E811–E817. doi: 10.1097/BRS.0b013e3181b1feba. [DOI] [PubMed] [Google Scholar]
- 2.Breen A.C., Teyhen D.S., Mellor F.E., Breen A.C., Wong K., Deitz A. Measurement of inter-vertebral motion using quantitative fluoroscopy: report of an international forum and proposal for use in the assessment of degenerative disc disease in the lumbar spine. Adv Orthop. 2012:1–10. doi: 10.1155/2012/802350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leone A., Cassar-Pullicino V., Gugliemli G., Bonomo L. Degenerative lumbar intervertebral instability: what is it and how does imaging contribute? Skelet Radiol. 2009;38(6):529–533. doi: 10.1007/s00256-009-0646-5. [DOI] [PubMed] [Google Scholar]
- 4.Mayer R.S., Chen I.H., Lavender S.A., Trafimow J.H., Andersson G.B. Variance in the measurement of sagittal lumbar spine range of motion among examiners, subjects, and instruments. Spine. 1995;20(13):1489–1493. doi: 10.1097/00007632-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Breen A., Muggleton J., Mellor F. An objective spinal motion imaging assessment (OSMIA): reliability, accuracy and exposure data. BMC Musculoskelet Disord. 2006;7(1):1–10. doi: 10.1186/1471-2474-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmadi A., Maroufi N., Behtash H., Zekavat H., Parnianpour M. Kinematic analysis of dynamic lumbar motion in patients with lumbar segmental instability using digital videofluoroscopy. Eur Spine J. 2009;18(11):1677–1685. doi: 10.1007/s00586-009-1147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auerbach J.D., Wills B.P.D., McIntosh T.C., Balderston R.A. Evaluation of spinal kinematics following lumbar total disc replacement and circumferential fusion using in vivo fluoroscopy. Spine. 2007;32(5):527–536. doi: 10.1097/01.brs.0000256915.90236.17. [DOI] [PubMed] [Google Scholar]
- 8.Cholewicki J., McGill S.M., Wells R.P., Vernon H. Method for measuring vertebral kinematics from videofluoroscopy. Clin Biomech. 1991;6:73–78. doi: 10.1016/0268-0033(91)90002-8. [DOI] [PubMed] [Google Scholar]
- 9.Lee S., Wong K., Chan M., Yeung H., Chiu J., Leong J. Development and validation of a new technique for assessing lumbar spine motion. Spine. 2002;27(8):E215–E220. doi: 10.1097/00007632-200204150-00022. [DOI] [PubMed] [Google Scholar]
- 10.Ortho-Kinematics . 2009. Revolutionizing spine motion analysis.http://orthokinematics.com/ [07.03.2012]; Available from: [Google Scholar]
- 11.Hart D., Hillier M.A., Wall B.F. 2005. Doses to patients from medical X-ray examinations in the UK. Review: National Radiation Protection Board (NRPB) [DOI] [PubMed] [Google Scholar]
- 12.Hart D., Wall B.F., Hillier M.C., Shrimpton P.C. Health Protection Agency (HPA); Chilton. Didcot. U.K.: 2008. Frequency and collective dose for medical and dental examinations in the UK; p. 19. [Google Scholar]
- 13.UNSCEAR . United Nations; New York: 2010. Sources and effects of ionising radiation. Report to the general assembly with scientific annexes. [Google Scholar]
- 14.FDA. Food and Drug Administration . 2010. Nationwide Evaluation of X-Ray Trends (NEXT)http://www.fda.gov/Radiation-EmittingProducts/RadiationSafety/NationwideEvaluationofX-RayTrendsNEXT/default.htm [cited 1.2.2012]; Available from: [Google Scholar]
- 15.Gron P., Olerud H.M., Einarsson G., Leitz W., Servomaa A., Schoultz B.W. A Nordic survey of patient doses in diagnostic radiology. Eur Radiol. 2000;10(12):1988–1992. doi: 10.1007/s003300000535. [DOI] [PubMed] [Google Scholar]
- 16.Almen A., Tingberg A., Mattsson S., Besjakov J., Kheddache S., Lanhede B. The influence of different technique factors on image quality of lumbar spine radiographs as evaluated by established CEC image criteria. Br J Radiol. 2000;73(875):1192–1199. doi: 10.1259/bjr.73.875.11144797. [DOI] [PubMed] [Google Scholar]
- 17.Mettler F.A., Huda W., Yoshizumi T.T., Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog1. Radiology. 2008;248(1):254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 18.Simpson A.K., Whang P.G., Jonisch A., Haims A., Grauer J.N. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech. 2008 Aug;21(6):409–412. doi: 10.1097/BSD.0b013e3181568656. [DOI] [PubMed] [Google Scholar]
- 19.Scanff P., Donadieu J., Pirard P., Aubert B. Population exposure to ionizing radiation from medical examinations in France. Br J Radiol. 2008;81(963):204–213. doi: 10.1259/bjr/24344062. [DOI] [PubMed] [Google Scholar]
- 20.Muhogora W.E., Ahmed N.A., Almosabihi A., Alsuwaidi J.S., Beganovic A., Ciraj-Bjelac O. Patient doses in radiographic examinations in 12 countries in asia, africa, and eastern europe: Initial results from IAEA projects. Am J Roentgenol. 2008;190(6):1453–1461. doi: 10.2214/AJR.07.3039. [DOI] [PubMed] [Google Scholar]
- 21.ICRP . Vol. 103. 2007. (The 2007 Recommendations of the International Commission on Radiological Protection). [Google Scholar]
- 22.Hart D., Jones D.G., Wall B.F. NRPB; Chilton: 1994. Estimation of effective dose in diagnostic radiology from entrance surface dose and dose-area product measurements. NRPB R262. [Google Scholar]
- 23.Ortho-Kinematics . 2012. Orthokinematics revolutionizing spine motion analysis.http://www.orthokinematics.com/index.php/physician/technology_overview [cited 30.08.2013]; Available from: [Google Scholar]
- 24.International Commission on Radiation Protection Radiological protection in biomedical research. Ann ICRP. 1991;22(3) [PubMed] [Google Scholar]
- 25.Health Protection Agency (HPA) 2008. Typical effective doses, equivalent periods of natural background radiation and lifetime fatal cancer risks from diagnostic medical exposures.http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733826941 [cited 13.03.2013]; Available from: [Google Scholar]
- 26.Sasieni P.D., Shelton J., Ormiston-SMith N., Thomas C.S., Silcocks P.B. What is the lifetime risk of developing cancer? the effect of adjusting for multiple primaries. Br J Cancer. 2011;105(3):460–465. doi: 10.1038/bjc.2011.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Health Protection Agency. Dose comparisons for ionising radiation. [cited 30.07.2013]; Available from:: http://www.hpa.org.uk/Topics/Radiation/UnderstandingRadiation/UnderstandingRadiationTopics/DoseComparisonsForIonisingRadiation/.
- 28.Tubiana M., Feinendegen L.E., Yang C., Kaminski J.M. The linear no-threshold relationship is inconsistent with radiation biologic and experimental data. Radiology. 2009;251(1):13–22. doi: 10.1148/radiol.2511080671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zeeb H. Health effects of low-level radiation: any news? J Radiol Prot. 2012;32:E111–E113. doi: 10.1088/0952-4746/32/3/E02. [DOI] [PubMed] [Google Scholar]
- 30.Harbron R.W. Cancer risks from low dose exposure to ionising radiation - is the linear no-threshold model still relevant? Radiography. 2012;18:28–33. [Google Scholar]