Abstract
Background
We aimed to determine the major contributing component of metabolic syndrome (MetS) that results in an elevated small dense LDL cholesterol (sdLDL-C) concentration and sdLDL-C/LDL-C ratio.
Methods
Four hundred and forty-seven subjects (225 men; 222 women) with MetS were randomly selected from the Korean Metabolic Syndrome Research Initiatives-Seoul cohort study. Age- and sex-matched healthy controls (181 men; 179 women) were also randomly selected from the same cohort.
Results
A comparison of the median values of the sdLDL-C concentration between subgroups, divided according to whether subjects met or did not meet the criteria for each MetS component in patients with MetS, revealed a significant difference in the sdLDL-C concentration only between subgroups divided according to whether subjects met or did not meet the triglyceride (TG) criteria (P<0.05 for each gender). The TG level showed a good correlation with sdLDL-C concentration (correlation coefficients [r]=0.543 for men; 0.653 for women) and the sdLDL-C/LDL-C ratio (r=0.789 for men; 0.745 for women). Multiple linear regression analyses conducted for the MetS group concordantly identified TG as one of the most significant contributors to sdLDL-C concentration (β=0.1747±0.0105, P<0.0001) and the sdLDL-C/LDL-C ratio (β=6.9518±0.3011, P<0.0001).
Conclusions
Among five MetS components, only the abnormal TG level was a differentiating factor for sdLDL-C concentration and sdLDL-C/LDL-C ratio. These results were reproducible in both genders, with or without MetS.
Keywords: Hypertriglyceridemia, Small dense LDL, Metabolic syndrome
INTRODUCTION
Elevated LDL cholesterol (LDL-C) is a major cause of cardiovascular disease (CVD), and clinical trials have conclusively shown that LDL-C-lowering therapy reduces the risk of developing CVD [1,2]. For these reasons, the United States National Institutes of Health National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III continues to identify elevated LDL-C as the primary target of cholesterol-lowering therapy [3]. However, measuring LDL-C concentration alone was insufficient to identify all individuals with incident CVD since a substantial proportion of these events occur in patients with a normal LDL-C concentration [4]. This has led to a search for other factors that may be implicated in the pathogenesis of atherosclerosis and CVD.
Metabolic syndrome (MetS), a constellation of CVD risk factors relating to the concentration of certain lipids other than LDL-C (hypertriglyceridemia, low HDL cholesterol [HDL-C], and insulin resistance) and non-lipid factors (hypertension and abdominal obesity), has been proposed as a criterion that would be helpful in identifying those patients who are at high risk of CVD regardless of LDL-C level [5]. The ATP III report has identified MetS as a secondary target of therapy in the management of CVD, in addition to LDL-C-lowering therapy [3,6].
Small dense LDL (sdLDL), which is not a MetS criterion, is a distinct LDL subclass primarily identified through size separation using gradient gel electrophoresis [7]. sdLDL has gained attention because of its pathogenicity and correlation with metabolic disease. It has been shown to have a higher degree of penetration of the arterial wall, a lower binding affinity for LDL receptors, a prolonged plasma half-life, and a lower resistance to oxidative stress relative to large buoyant LDL [8,9]. Clinical studies have consistently demonstrated that the accumulation of sdLDL particles in the plasma is associated with an increased risk of CVD [10]. Furthermore, the measurement of sdLDL cholesterol (sdLDL-C) concentration was useful in the assessment of the presence of CVD [11,12] and its severity [13]. In addition, a recent publication by Arai et al. [14] demonstrated the utility of the sdLDL-C concentration as a predictive marker for CVD incidence.
Patients with MetS may not present with an elevated LDL-C concentration. However, a qualitative abnormality in LDL-C, such as sdLDL-C, is associated with MetS [15]. Nozue et al. [16] reported that the sdLDL-C concentration measured by using the heparin-Magnesium precipitation method was significantly higher in patients with coronary artery disease and MetS than in patients without MetS. Nakano et al. [17] and Sugino et al. [18] conducted cross-sectional studies using patients with MetS and healthy controls, and observed a higher concentration of sdLDL-C in patients with MetS. However, the component of MetS that is most closely associated with an elevated sdLDL-C concentration has not been identified.
In this study, we evaluated the association between sdLDL-C concentration or sdLDL-C/LDL-C ratio and metabolic parameters that included each component of MetS, and attempted to identify the major component of MetS contributing to an elevated sdLDL-C concentration.
METHODS
1. Study participants
Four hundred and forty-seven subjects (225 men; 222 women) with MetS were obtained from the Korean Metabolic Syndrome Research Initiatives-Seoul cohort study (2006-2010) [19] by using simple random sampling in subgroup with MetS. Age- and sex-matched healthy controls (181 men; 179 women) without MetS were also randomly selected from healthy subgroup of the same cohort. All subjects completed the lifestyle questionnaire and anthropometric survey, and serum samples for biochemical tests were collected in accordance with the protocols outlined by the Institutional Review Board of Severance Hospital, Yonsei University, Seoul, Korea. Serum samples were stored frozen below -80℃ until further analyses.
2. Diagnosis of MetS and definition of healthy status
MetS was diagnosed according to the NCEP ATP III definition of MetS, with the exception of two components, i.e., fasting glucose (fasting blood glucose >5.6 mmol/L) and waist circumference (waist circumference [WC]; >90 cm for mem; >85 cm for women), which had been modified for the Asian population [20]. Healthy population was defined as individuals without renal disease, hepatic disease, infectious diseases, or malignancy, as well as, history of familial lipid disorders or dyslipidemia-related diseases.
3. Biochemical tests
Frozen serum samples of the study participants were thawed and used for biochemical tests. Serum glucose concentrations were measured by using the hexokinase method (Roche Diagnostics, Mannheim, Germany) with a Hitachi 7600 clinical chemistry analyzer (Hitachi Ltd., Tokyo, Japan). Total cholesterol (TC) and triglyceride (TG) concentrations were determined by using enzymatic methods (Sekisui, Tokyo, Japan and Roche Diagnostics, respectively), and HDL-C and LDL-C were determined by using a direct enzymatic procedure (Sekisui) with a Hitachi 7600 analyzer. Serum sdLDL-C concentrations were measured by using a homogeneous enzymatic assay (Denka Seiken, Tokyo, Japan) with a Hitachi-7600 analyzer. Serum insulin concentration was determined by using an automated enzyme chemiluminescence immunoassay (DxI; Beckman Coulter, Brea, CA, USA). As a surrogate index of insulin resistance, homeostasis model assessment of insulin resistance (HOMA-IR) was calculated by using the formula of Matthews et al. [21] as follows: fasting plasma insulin (mIU/L)×fasting plasma glucose (mmol/L)/22.5.
4. Statistical analyses
Participants' characteristics were compared according to MetS status by using the Mann-Whitney'S U tests for continuous measures and chi-square tests for categorical measures. The median values of sdLDL-C concentration were compared between subgroups classified according to whether subjects met or did not meet the criteria for each MetS component. A correlation between the sdLDL-C concentration or sdLDL-C/LDL-C ratio and age or another metabolic parameter was examined. The strength of correlation was interpreted according to the size of correlation coefficient (r) as strong (0.8≤ |r<1), moderate (0.5≤|r|<0.8), or weak (0.1 ≤|r|<0.5). Multiple linear regression analysis by the "enter" procedure was performed to identify the independent variables associated with plasma sdLDL-C concentration. To perform this analysis, the criteria for MetS (WC, TG, HDL-C, systolic blood pressure, diastolic blood pressure [DBP], fasting glucose), age, and LDL-C were included in the model. All statistical analyses were conducted by using the Analyse-it Method Evaluation Edition version 2.22 software (Analyse-it Software Ltd., Leeds, UK), GraphPad Prism version 6.04 (GraphPad Software, La Jolla, CA, USA), or PASW Statistics 18.0.0 tool (IBM Corp., Armonk, NY, USA). P values <0.05 were considered statistically significant.
RESULTS
1. Characteristics of the study groups
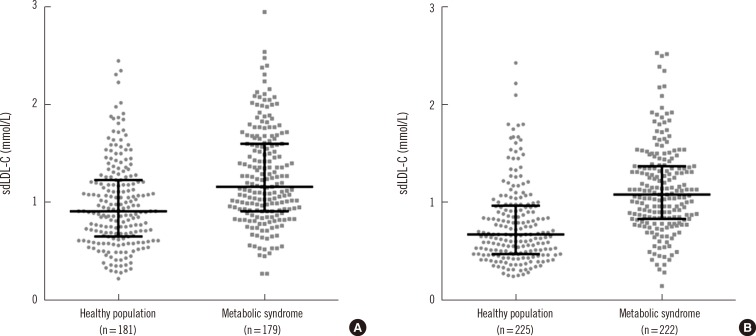
The characteristics of participants grouped by MetS status are summarized in Table 1. Subjects with MetS had a significantly higher sdLDL-C concentration and sdLDL-C/LDL-C ratio than healthy controls, in both men and women (Fig. 1). In addition, subjects presenting with MetS had a higher body mass index, fasting insulin level, HOMA-IR, and non-HDL-C concentration than healthy controls in both genders (Table 1). TC and LDL-C concentrations were higher in women with MetS than without MetS. Reference intervals for sdLDL-C, determined by using non-parametric methods (2.5 and 97.5 percentiles) in healthy controls, were 0.30-1.86 mmol/L for men and 0.27-1.61 mmol/L for women.
Table 1. Baseline characteristics of the study population.
| Characteristic | Men (n = 406) | Women (n = 401) | ||||
|---|---|---|---|---|---|---|
| Healthy population | MetS | P value | Healthy population | MetS | P value | |
| Number | 181 | 225 | - | 179 | 222 | - |
| Age (yr) | 46 (40-54) | 51 (43-57) | < 0.001 | 45 (38-53) | 56 (50-62) | < 0.001 |
| BMI (kg/m2) | 24.10 (22.38-25.68) | 26.56 (25.20-28.15) | < 0.001 | 21.91 (20.80-23.79) | 25.55 (24.25-27.48) | < 0.001 |
| WC (cm) | 84 (79-88) | 92 (90-96) | < 0.001 | 73 (69-77) | 84 (81-88) | < 0.001 |
| SBP (mm Hg) | 116 (111-122) | 128 (119-135) | < 0.001 | 109 (104-116) | 125 (116-137) | < 0.001 |
| DBP (mm Hg) | 77 (69-81) | 88 (82-93) | < 0.001 | 70 (65-78) | 82 (75-87) | < 0.001 |
| Fasting glucose (mmol/L) | 4.83 (4.55-5.05) | 5.61 (5.00-6.49) | < 0.001 | 4.66 (4.38-4.88) | 5.27 (4.83-6.44) | < 0.001 |
| Fasting insulin (mIU/L) | 4.1 (2.8-5.6) | 6.5 (4.8-8.7) | < 0.001 | 3.8 (2.5-4.8) | 5.3 (3.9-7.1) | < 0.001 |
| HOMA-IR | 0.894 (0.655-1.302) | 1.687 (1.184-2.369) | < 0.001 | 0.818 (0.524-1.039) | 1.302 (0.984-1.888) | < 0.001 |
| TC (mmol/L) | 4.82 (4.33-5.34) | 4.95 (4.33-5.59) | 0.123 | 4.74 (4.25-5.46) | 5.21 (4.61-5.78) | < 0.001 |
| TG (mmol/L) | 1.42 (1.01-2.02) | 2.43 (1.88-3.21) | < 0.001 | 0.95 (0.80-1.41) | 2.00 (1.73-2.52) | < 0.001 |
| HDL-C (mmol/L) | 1.27 (1.11-1.48) | 1.01 (0.93-1.17) | < 0.001 | 1.53 (1.32-1.79) | 1.17 (1.06-1.35) | < 0.001 |
| LDL-C (mmol/L) | 3.08 (2.69-3.50) | 3.08 (2.59-3.52) | 0.840 | 2.93 (2.43-3.55) | 3.32 (2.82-3.89) | < 0.001 |
| Non-HDL-C (mmol/L) | 3.52 (2.98-3.96) | 3.86 (3.26-4.53) | < 0.001 | 3.19 (2.69-3.91) | 3.94 (3.39-4.61) | < 0.001 |
| sdLDL-C (mmol/L) | 0.88 (0.62-1.20) | 1.16 (0.91-1.60) | < 0.001 | 0.64 (0.47-0.89) | 1.10 (0.85-1.39) | < 0.001 |
| sdLDL-C (mmol/L), 2.5-97.5 percentile | 0.30-1.86 | 0.49-2.31 | - | 0.27-1.61 | 0.39-2.22 | - |
| sdLDL-C/LDL-C (%) | 28.08 (21.74-37.00) | 39.29 (32.21-48.50) | < 0.001 | 21.37 (18.21-26.06) | 33.20 (26.93-40.07) | < 0.001 |
| LDL-C < 2.6 mmol/L | 20.40% | 24.40% | 0.3383* | 30.20% | 17.10% | 0.0020* |
| LDL-C > 4.14 mmol/L | 4.40% | 11.60% | 0.0099* | 11.20% | 17.60% | 0.0723* |
| sdLDL-C < 0.5 mmol/L | 13.80% | 2.70% | < 0.0001* | 31.80% | 6.30% | < 0.0001* |
| sdLDL-C > 1.0 mmol/L | 38.10% | 60.90% | < 0.0001* | 15.10% | 56.80% | < 0.0001* |
Values are presented as the median (interquartile range), with the exception of the frequency data.
*The chi-square test was employed to compare frequency data. Other characteristics were analyzed using the Mann-Whitney's U test.
Abbreviations: MetS, metabolic syndrome; BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; HOMA-IR, homeostasis model of insulin resistance; TC, total cholesterol; TG, triglyceride; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol; sdLDL-C, small dense LDL cholesterol.
Fig. 1. Scattergrams of the small dense LDL cholesterol (sdLDL-C) concentrations in a healthy population versus male (A) and female (B) patients with metabolic syndrome. The lines depict the median values and and interquartile ranges of each group, which were significantly different (P<0.001) in both genders.
Subjects presenting with MetS included a higher percentage with high LDL-C (>4.14 mmol/L) as defined by the NCEP [3] than healthy men and women. However, the percentage with optimal LDL-C (<2.6 mmol/L) was lower in individuals with MetS than without MetS for women only. The proportion of subjects with a sdLDL-C concentration <0.5 mmol/L was significantly lower among both men and women with MetS than without MetS (Table 1). The proportion with sdLDL-C >1.0 mmol/L was higher in individuals with MetS than without MetS.
2. Differences in sdLDL-C concentration or sdLDL-C/LDL-C ratio in relation to the presence or absence of each MetS component
Fig. 1 shows that patients with MetS had higher sdLDL-C concentrations than healthy controls, in both men and women. When the median values of sdLDL-C concentration were compared between subgroups, divided according to whether subjects met or did not meet the criteria for each MetS component (Table 2), a significant difference in the sdLDL-C concentration was only found between subgroups divided according to TG criteria. There were no differences in sdLDL-C concentration in the presence or absence of other MetS components. A similar pattern was observed for healthy controls. Subjects who met the TG criteria showed a higher sdLDL-C concentration than those who did not. In addition, sdLDL-C concentration was significantly different between healthy controls who met the WC criteria and those who did not.
Table 2. Differences in the medians of the sdLDL-C concentration and sdLDL-C/LDL-C ratio between subgroups divided according to whether subjects met or did not meet the criteria for each metabolic syndrome component.
| Group | Men (n=406) | Women (n=401) | ||||||
|---|---|---|---|---|---|---|---|---|
| sdLDL-C (mmol/L) N of subjects |
sdLDL-C/LDL-C (%) N of subjects |
sdLDL-C (mmol/L) N of subjects |
sdLDL-C/LDL-C (%) N of subjects |
|||||
| Component- | Component+ | Component- | Component+ | Component- | Component+ | Component- | Component+ | |
| Metabolic syndrome | 1.16 (0.91-1.60) | 39.29 (32.21-48.50) | 1.10 (0.85-1.39) | 33.20 (26.93-40.07) | ||||
| 225 | 225 | 222 | 222 | |||||
| WC | 1.18 (0.92-1.59) 54 |
1.13 (0.91-1.63) 171 |
41.75 (35.87-51.98) 54 |
38.39 (31.02-47.36) 171 |
1.17 (0.88-1.37) 32 |
1.09 (0.85-1.39) 190 |
34.09 (29.39-40.56) 32 |
33.12 (26.45-40.07) 190 |
| TG | 0.75 (0.59-0.95)* 32 |
1.26 (0.99-1.68)* 193 |
25.95 (22.44-31.45)* 32 |
41.75 (35.3-51.02)* 193 |
0.86 (0.68-1.06)* 47 |
1.18 (0.91-1.50)* 175 |
25.67 (22.00-31.22)* 47 |
35.75 (29.82-42.33)* 175 |
| HDL-C | 1.18 (0.92-1.68) 105 |
1.16 (0.91-1.52) 120 |
38.39 (30.48-47.57) 105 |
40.24 (32.88-50.2) 120 |
1.15 (0.82-1.51) 66 |
1.08 (0.85-1.37) 156 |
33.54 (25.80-40.64) 66 |
33.12 (28.26-39.92) 156 |
| BP | 1.27 (0.91-1.65) 39 |
1.14 (0.91-1.59) 186 |
42.23 (33.76-49.22) 39 |
38.53 (31.95-48.29) 186 |
1.09 (0.89-1.46) 63 |
1.10 (0.82-1.36) 159 |
34.83 (28.68-41.90) 63 |
32.58 (25.58-39.92) 159 |
| FG | 1.19 (0.96-1.59) 143 |
1.09 (0.78-1.61) 82 |
39.45 (32.81-48.29) 143 |
39.10 (28.57-49.04) 82 |
1.10 (0.85-1.38) 135 |
1.08 (0.82-1.51) 87 |
32.79 (26.85-39.17) 135 |
33.91 (26.93-42.84) 87 |
| Healthy population | 0.88 (0.62-1.20) | 28.08 (21.74-37) | 0.64 (0.47-0.89) | 21.37 (18.21-26.06) | ||||
| 181 | 181 | 179 | 179 | |||||
| WC | 0.87 (0.61-1.19)* 158 |
1.08 (0.74-1.39)* 23 |
27.89 (21.44-36.9) 158 |
31.65 (26.62-43.73) 23 |
0.61 (0.47-0.85)* 146 |
0.78 (0.60-1.08)* 33 |
21.08 (18.12-26.06) 146 |
22.83 (19.70-25.98) 33 |
| TG | 0.72 (0.57-0.94)* 115 |
1.23 (0.98-1.53)* 66 |
23.28 (19.94-28.93)* 115 |
40.95 (32.04-51.09)* 66 |
0.60 (0.46-0.79)* 152 |
1.11 (0.92-1.53)* 27 |
20.58 (17.58-23.59)* 152 |
33.90 (28.33-37.48)* 27 |
| HDL-C | 0.85 (0.61-1.18) 156 |
1.07 (0.87-1.28) 25 |
27.46 (21.46-35.58)* 156 |
36.04 (31.18-47.88)* 25 |
0.62 (0.47-0.86) 145 |
0.71 (0.53-0.99) 34 |
21.07 (17.74-25.74) 145 |
22.54 (20.07-30.32) 34 |
| BP | 0.88 (0.61-1.19) 155 |
0.91 (0.69-1.37) 26 |
28.08 (21.56-37.00) 155 |
29.38 (21.74-37.32) 26 |
0.65 (0.48-0.90) 164 |
0.59 (0.40-0.84) 15 |
21.49 (18.51-26.10) 164 |
19.70 (16.67-23.55) 15 |
| FG | 0.88 (0.62-1.20) 178 |
0.94 (0.29-1.26) 3 |
28.18 (21.74-37.00) 178 |
24.93 (13.29-39.35) 3 |
0.64 (0.47-0.89) 179 |
- | 21.37 (18.21-26.06) 179 |
- |
BP component was considered positive when subjects met metabolic syndrome criteria for systolic blood pressure or diastolic blood pressure. Values are presented as the median (interquartile range).
sdLDL-C concentration (mmol/L) or sdLDL-C/LDL-C ratio (%) of those who have the component and not in each gender group were compared using the Mann-Whitney's U test, and P<0.05 are indicated by *.
Abbreviations: BP, blood pressure; FG, fasting glucose; see Table 1.
The ratio of sdLDL-C/LDL-C was also significantly increased in subjects who met the TG criteria, regardless of gender or disease status (Table 2). However, the presence or absence of the WC component did not significantly alter this ratio. A difference in the sdLDL-C/LDL-C ratio was observed between healthy men who met the HDL-C criteria and those who did not.
3. Association of the sdLDL-C concentration with other metabolic parameters
Among those univariate correlations analysis in all subjects; TC, LDL-C, and TG each showed moderate correlation with sdLDL-C concentration (r=0.738, 0.508, and 0.543, respectively, for men; 0.748, 0.692, and 0.653, respectively, for women), whereas only TG showed moderate correlation with sdLDL-C/LDL-C ratio (r=0.789 for men; 0.745 for women).
When subpopulations divided according to MetS status were analyzed, in the healthy group, TC, LDL-C, and TG each showed moderate correlation with sdLDL-C concentration (r=0.665, 0.574, and 0.659 for TC, LDL-C, and TG, respectively), whereas only TG showed moderate correlation with sdLDL-C/LDL-C ratio (r=0.749). In the MetS group, the strength of the correlation between TG and sdLDL-C concentration was diminished (r=0.403), while other factors retained moderate correlation with sdLDL-C (r=0.589 for TC; 0.752 for LDL-C). However, only TG showed moderate correlation with sdLDL-C/LDL-C ratio (r=0.767).
To elucidate each factor's quantitative contribution to the sdLDL-C concentration and the sdLDL-C/LDL-C ratio, multiple linear regression analysis using anthropometric and metabolic parameters was conducted for the whole study population (Table 3). The most significant determinant of plasma sdLDL-C concentration was LDL-C, followed by TG concentration, and fasting glucose level; WC in men and age in women apparently had an additive effect on sdLDL-C concentration. For the sdLDL-C/LDL-C ratio, TG concentration was the most significant contributing factor in both genders.
Table 3. Associations of the sdLDL-C concentration and sdLDL-C/LDL-C ratio with metabolic variables in each gender determined by multiple linear regression analysis.
| Parameter | Men (n = 406) | Women (n=401) | ||||||
|---|---|---|---|---|---|---|---|---|
| sdLDL-C (mmol/L) | sdLDL-C/LDL-C (%) | sdLDL-C (mmol/L) | sdLDL-C/LDL-C (%) | |||||
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Age (yr) | 0.0006±0.0016 | 0.7126 | 0.0363±0.0456 | 0.4259 | 0.0042±0.0012 | 0.0007* | 0.1638±0.0379 | <0.0001* |
| WC (cm) | 0.0078±0.0022 | 0.0005* | 0.2501±0.0644 | 0.0001* | 0.0004±0.0018 | 0.8129 | 0.0269±0.0535 | 0.6150 |
| SBP (mm Hg) | -0.0029±0.0017 | 0.0873 | -0.1066±0.0490 | 0.0303* | -0.0001±0.0012 | 0.9223 | -0.0007±0.0363 | 0.9836 |
| DBP (mm Hg) | 0.0036±0.0020 | 0.0713 | 0.0969±0.0588 | 0.1000 | 0.0013±0.0016 | 0.4366 | 0.0502±0.0497 | 0.3131 |
| Fasting glucose (mmol/L) | 0.0198±0.0099 | 0.0467* | 0.4983±0.2903 | 0.0868 | 0.0215±0.0068 | 0.0017* | 0.4732±0.2069 | 0.0227* |
| TG (mmol/L) | 0.1776±0.0112 | <0.0001* | 7.4390±0.3270 | <0.0001* | 0.2420±0.0143 | <0.0001* | 7.3739±0.4339 | <0.0001* |
| HDL-C (mmol/L) | 0.0430±0.0617 | 0.4864 | 3.3684±1.8020 | 0.0623 | 0.0441±0.0404 | 0.2767 | -0.0022±1.2312 | 0.9986 |
| LDL-C (mmol/L) | 0.3911±0.0204 | <0.0001* | 0.3981±0.5957 | 0.5043 | 0.3005±0.0137 | <0.0001* | -0.1538±0.4164 | 0.7122 |
The components of metabolic syndrome (WC, TG, HDL-C, SBP, DBP, fasting glucose), age, and LDL-C were included in the multiple linear regression analysis with an "enter" procedure, and P values <0.05 are indicated by *.
Abbreviations: See Table 1.
LDL-C, TG, fasting glucose and WC were common significant determinants of plasma sdLDL-C in both MetS and healthy subjects (Table 4). However, the effect of LDL-C was no longer observed when sdLDL-C/LDL-C ratio was used as the dependent factor. The regression coefficients of TG for sdLDL-C concentration and sdLDL-C/LDL-C ratio in the healthy group (0.2706 and 9.1815, respectively) were noticeably higher than in the MetS group (0.1747 and 6.9518, respectively), consistent with the diminished strength of correlation between TG and sdLDL-C concentration in the MetS group. While the association between DBP and sdLDL-C concentration or sdLDL-C/LDL-C ratio was only significant in the MetS group, HDL-C concentration showed significant association with sdLDL-C concentration and sdLDL-C/LDL-C ratio in the healthy population only (Table 4).
Table 4. Associations of the sdLDL-C concentration and sdLDL-C/LDL-C ratio with metabolic variables in patients with metabolic syndrome and healthy controls.
| Parameter | MetS (n=447) | Healthy population (n=360) | ||||||
|---|---|---|---|---|---|---|---|---|
| sdLDL-C (mmol/L) | sdLDL-C/LDL-C (%) | sdLDL-C (mmol/L) | sdLDL-C/LDL-C (%) | |||||
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Age (yr) | 0.0025 ± 0.0016 | 0.1183 | 0.0698 ± 0.0455 | 0.1257 | 0.0022 ± 0.0013 | 0.0764 | 0.0780 ± 0.0406 | 0.0557 |
| WC (cm) | 0.0045 ± 0.0019 | 0.0226* | 0.1200 ± 0.0561 | 0.0329* | 0.0055 ± 0.0018 | 0.0020* | 0.2161 ± 0.0571 | 0.0002* |
| SBP (mm Hg) | -0.0024 ± 0.0013 | 0.0729 | -0.0653 ± 0.0388 | 0.0927 | 0.0003 ± 0.0016 | 0.8678 | -0.0255 ± 0.0521 | 0.6241 |
| DBP (mm Hg) | 0.0047 ± 0.0018 | 0.0102* | 0.1303 ± 0.0521 | 0.0127* | -0.0006 ± 0.0018 | 0.7561 | 0.0102 ± 0.0585 | 0.8612 |
| Fasting glucose (mmol/L) | 0.0172 ± 0.0068 | 0.0121* | 0.4015 ± 0.1966 | 0.0418* | 0.0990 ± 0.0277 | 0.0004* | 3.0126 ± 0.8919 | 0.0008* |
| TG (mmol/L) | 0.1747 ± 0.0105 | < 0.0001* | 6.9518 ± 0.3011 | < 0.0001* | 0.2706 ± 0.0157 | < 0.0001* | 9.1815 ± 0.5049 | < 0.0001* |
| HDL-C (mmol/L) | 0.0077 ± 0.0634 | 0.9030 | 0.4235 ± 1.8250 | 0.8166 | 0.0935 ± 0.0425 | 0.0287* | 3.0332 ± 1.3720 | 0.0277* |
| LDL-C (mmol/L) | 0.3830 ± 0.0167 | < 0.0001* | -0.0060 ± 0.4802 | 0.9900 | 0.2510 ± 0.0160 | < 0.0001* | -0.6816 ± 0.5151 | 0.1866 |
The components of metabolic syndrome (WC, TG, HDL-C, SBP, DBP, fasting glucose), age, and LDL-C were included in the multiple linear regression analysis with an "enter" procedure, and P values <0.05 are indicated by *.
Abbreviations: See Table 1.
DISCUSSION
In this study, we evaluated sdLDL-C concentration in both healthy subjects and patients with MetS. The study population was subdivided according to the presence or absence of each MetS component, and the concentration of sdLDL-C and the sdLDL-C/LDL-C ratio in each subgroup were compared. We found that the sdLDL-C concentration and sdLDL-C/LDL-C ratio were higher in patients with MetS who met TG component criteria compared with those who did not (Table 2), while the other MetS components were not associated with an elevated sdLDL-C concentration. The findings were reproducible in both genders and also in the healthy population, with an exception that additional effect of WC or HDL-C on the concentration of sdLDL-C or sdLDL-C/LDL-C ratio was found in healthy group. A possible explanation of this phenomenon is a larger effect of TG on sdLDL-C compared with that of WC or HDL-C, which would be sufficient to make a statistically significant difference even in patients with MetS whose baseline for sdLDL-C is higher than that of healthy population.
In correlation and multiple linear regression analyses, the TG concentration was a significant determinant of sdLDL-C concentration (Tables 3 and 4), in line with the previous studies on the association between sdLDL-C and TG concentrations [17,18,22]. However, to the best of our knowledge, none of these studies analyzed differences in sdLDL-C concentration according to the presence or absence of each MetS component as done in this study. A previous cross-sectional study on the relationship between sdLDL particle number, measured by nuclear magnetic resonance, and each MetS component also showed that only TG and HDL-C concentrations were strongly correlated with sdLDL particle number [15].
The precise mechanism underlying the association between TG and sdLDL-C concentrations has not yet been elucidated. It has been speculated that, when the TG concentration is normal, cholesteryl ester transfer protein preferentially mediates the transfer of HDL cholesteryl esters to LDL particles [23,24]. In hypertriglyceridemia, the large very low-density lipoprotein (VLDL) particles are preferred acceptors of HDL-derived cholesteryl esters owing to their increased numbers [23,24]. Under these conditions, there are high net transfer rates of cholesteryl esters from HDL to VLDL, and of TG from VLDL to both LDL and HDL. The TG-enriched LDL particles are targets for hepatic lipase activity that hydrolyzes phospholipid and TG, leading to the formation of sdLDL particles [23,24].
TG concentration is an independent risk factor in the development of CVD [25,26,27]. While the number of TG-rich lipoprotein particles or level of TG-rich lipoprotein cholesterol could contribute to the development of atherosclerosis in hypertriglyceridemia, alterations in other lipoprotein phenotypes induced by hypertriglyceridemia could also be important factors in this process [28]. An increased number of remnant-like lipoproteins and sdLDL particles were simultaneously present in fasting hypertriglyceridemia or postprandial lipidemia, and in both cases, highly atherogenic [28]. In the present study, the TG concentration showed relatively strong correlation with sdLDL-C concentration, and is considered a significant determinant of sdLDL-C concentration (Table 3). And the association between sLDL-C/LDL-C ratio, which may rise due to increased sdLDL without an increase of LDL, and TG was even stronger than that between sdLDL-C concentration and TG (Table 4), as reported previously [18]. These findings suggest that the atherogenic effect of hypertriglyceridemia partially results from an increased sdLDL. However, more studies are needed to elucidate the primary mechanism that leads to the atherogenic effect mediated by TG.
To our surprise, the correlation of TG with sdLDL-C previously was weakened in the MetS group compared with the healthy group, and the contribution of TG to the sdLDL-C previously was consistently diminished in the MetS group (Table 4). When each group was subdivided according to whether they had hypertriglyceridemia (TG>1.7 mmol/L) or not, the regression coefficient of TG for sdLDL-C previously was weakened by the presence of hypertriglyceridemia in both the MetS and healthy groups (Supplemental Data Table S1). This implies that a more complicated mechanism of lipid metabolism contributed to the sdLDL-C concentration in MetS or hypertriglyceridemia compared with the healthy group, particularly having a normal TG concentration.
WC is regarded as a key component of MetS, as central obesity could drive all the pathophysiologic conditions constituting the other criteria of this syndrome [29]. Obesity itself also results in an increase in the formation of sdLDL by inducing changes in lipoprotein metabolism [30,31]. In the present study, healthy individuals who had an abnormal WC showed an increased sdLDL-C concentration; this tendency was not observed in patients with MetS (Table 2). Multiple linear regression analysis revealed this relationship as concordantly significant in both groups (Table 4), but relatively small contributions of WC to sdLDL-C concentration were noted (regression coefficients: 0.0055±0.0018 and 0.0045±0.0019, in the healthy and MetS group, respectively). While obesity is the major driving force of the other components of MetS, insulin resistance and compensatory hyperinsulinemia could predispose individuals to conditions related to CVD [32], and the insulin resistance correlates well with sdLDL-C concentration [33]. In the present study using HOMA-IR as an indicator of insulin resistance, weak correlation between insulin resistance and both sdLDL-C concentration and sdLDL-C/LDL-C ratio was observed (r=0.366 and 0.315, respectively). And the strength of correlation was weakened in the MetS group compared with the healthy population (Supplemental Data Figure S1).
Low HDL-C concentration, in conjunction with hypertriglyceridemia and presence of sdLDL, constitutes the so-called atherogenic lipoprotein phenotype [34]. However, in the present study, while HDL-C concentration significantly contributed to LDL-C concentration and sdLDL-C/LDL-C ratio in the healthy population, it did not do so in patients with MetS (Table 4), opposite to the reported correlation between sdLDL particle number and HDL-C concentration in MetS [15]. As there seem to be different contributions of HDL subfractions to sdLDL-C, HDL2-C being more closely correlated with sdLDL-C than total HDL-C or HDL3-C [35], further studies utilizing HDL-C subfractions are needed to elucidate their association with sdLDL-C level or sdLDL-C/LDL-C ratio in patients with MetS.
In the Framingham Heart Study, hypertension and sdLDL particle number were significantly correlated in the MetS group [15]. In line with this report, both the sdLDL-C concentration and sdLDL-C/LDL-C ratio were significantly associated with DBP in the MetS group (Table 4). However, these associations were not observed in the healthy population. A study comparing LDL subfraction patterns of normotensive and hypertensive individuals without MetS also concluded that hypertension per se did not increase the proportion of sdLDL particles in this population [36]. Taken together, hypertension is the only factor among components of MetS that is more closely associated to sdLDL-C concentration in MetS than in healthy population. Thus there might be a different contribution of hypertension to the formation of sdLDL in MetS.
When the total number of MetS components was regarded as a simple tentative surrogate marker for the severity of MetS, it was found to be well associated with the number of sdLDL particles [15]. In our study, the sdLDL-C concentration and sdLDL-C/LDL-C ratio were concordantly elevated with the increasing number of MetS components, although the sdLDL-C concentration was not significantly different between MetS patients who had four and five MetS components (Supplemental Data Figure S2).
This study has several limitations. As the study population was selected from a cohort to give nearly equal numbers in the subgroups, the natural distribution of metabolic parameters in the general population was abolished. Furthermore, because of differences in measurement methods and the ethnicity of the study population, our results are not directly comparable with those of previous studies [37].
In conclusion, among five MetS components, abnormal TG concentration was the only factor associated with sdLDL-C concentration and sdLDL-C/LDL-C ratio in both genders with or without MetS. In addition, TG concentration showed the strongest correlation with sdLDL-C concentration and sdLDL-C/LDL-C ratio among the five MetS components. Therefore, hypertriglyceridemia is a major factor associated with elevated concentrations of sdLDL-C in patients with MetS. Our results support the hypothesis that the atherogenic effect of hypertriglyceridemia is mediated by increased sdLDL-C; further studies are required to elucidate the underlying mechanism.
Acknowledgments
This study was supported by generous donation of sdLDL-C kits by the Hanlab and Denka Seiken companies and also by grant 10526 from the Seoul City Research and Business Development Program, Korea.
Footnotes
Authors' Disclosures of Potential Conflicts of Interest: No potential conflicts of interest relevant to this article were reported.
Supplementary Material
Supplemental Data Table S1. Associations of sdLDL-C with metabolic variables in the presence of either metabolic syndrome or hypertriglyceridemia (TG >1.7 mmol/L) determined by multiple linear regression analysis.
| Parameter | MetS (n = 447) | Healthy population (n = 360) | ||||||
|---|---|---|---|---|---|---|---|---|
| Normal TG (n = 80) | Hypertriglyceridemia (n = 367) | Normal TG (n = 267) | Hypertriglyceridemia (n = 93) | |||||
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Age (yr) | 0.0025±0.0029 | 0.3903 | 0.0031±0.0018 | 0.0781 | 0.0020±0.0012 | 0.0827 | 0.0072±0.0038 | 0.0629 |
| WC (cm) | 0.0024±0.0034 | 0.4911 | 0.0051±0.0022 | 0.0212 | 0.0043±0.0016 | 0.0083* | 0.0098±0.0051 | 0.0574 |
| SBP (mm Hg) | -0.0002±0.0023 | 0.9372 | -0.0025±0.0015 | 0.0997 | 0.0000±0.0015 | 0.9871 | 0.0018±0.0042 | 0.6715 |
| DBP (mm Hg) | -0.0015±0.0033 | 0.6594 | 0.0060±0.0020 | 0.0031* | -0.0011±0.0017 | 0.5153 | 0.0040±0.0049 | 0.4190 |
| Fasting glucose (mmol/L) | 0.0283±0.0113 | 0.0147* | 0.0216±0.0078 | 0.0061* | 0.0656±0.0259 | 0.0119* | 0.1134±0.0756 | 0.1373 |
| TG (mmol/L) | 0.2148±0.0822 | 0.0109* | 0.1526±0.0121 | <0.0001* | 0.2665±0.0368 | <0.0001* | 0.2128±0.0382 | <0.0001* |
| HDL-C (mmol/L) | 0.1233±0.0966 | 0.2060 | -0.0261±0.0731 | 0.7208 | 0.0878±0.0370 | 0.0183* | 0.2492±0.1488 | 0.0977 |
| LDL-C (mmol/L) | 0.2792±0.0300 | <0.0001* | 0.3860±0.0191 | <0.0001* | 0.2490±0.0152 | <0.0001* | 0.2511±0.0422 | <0.0001* |
The components of MetS (WC, TG, HDL-C, SBP, DBP, FG), age, and LDL-C were included in the multiple linear regression analysis with an "enter" procedure, and P values <0.05 are indicated by *.
Abbreviations: MetS, metabolic syndrome; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol.
Scatterplots showing the correlation between the plasma concentration of small dense LDL cholesterol (sdLDL-C) (A) or the sdLDL-C/LDL-C ratio (B) and the homeostasis model assessment of insulin resistance (HOMA-IR) in patients with MetS (●) and healthy population (◦). Linear regression curve for the two variables are indicated in solid line (for patients with MetS) or dashed line (for healthy population).
Progressive increase in the small dense LDL cholesterol (sdLDL-C) concentration in men (A) and women (B), and the sdLDL-C/LDL-C ratio in men (C) and women (D), as a function of the number of metabolic syndrome components (P for trend < 0.001, for all).
References
- 1.Smith SC, Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel on Detection, Evaluation, Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Kannel WB. Range of serum cholesterol values in the population developing coronary artery disease. Am J Cardiol. 1995;76:69C–77C. doi: 10.1016/s0002-9149(99)80474-3. [DOI] [PubMed] [Google Scholar]
- 5.Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004;89:2595–2600. doi: 10.1210/jc.2004-0372. [DOI] [PubMed] [Google Scholar]
- 6.Kahn R. Metabolic syndrome: is it a syndrome? Does it matter? Circulation. 2007;115:1806–1810. doi: 10.1161/CIRCULATIONAHA.106.658336. [DOI] [PubMed] [Google Scholar]
- 7.Krauss RM. Identification of multiple subclasses of plasma low density lipoproteins in normal humans. J Lipid Res. 1982;23:97–104. [PubMed] [Google Scholar]
- 8.Björnheden T, Babyi A, Bondjers G, Wiklund O. Accumulation of lipoprotein fractions and subfractions in the arterial wall, determined in an in vitro perfusion system. Atherosclerosis. 1996;123:43–56. doi: 10.1016/0021-9150(95)05770-6. [DOI] [PubMed] [Google Scholar]
- 9.Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43:1363–1379. doi: 10.1194/jlr.r200004-jlr200. [DOI] [PubMed] [Google Scholar]
- 10.Rizzo M, Pernice V, Frasheri A, Di Lorenzo G, Rini GB, Spinas GA, et al. Small, dense low-density lipoproteins (LDL) are predictors of cardio- and cerebro-vascular events in subjects with the metabolic syndrome. Clin Endocrinol (Oxf) 2009;70:870–875. doi: 10.1111/j.1365-2265.2008.03407.x. [DOI] [PubMed] [Google Scholar]
- 11.Hirano T, Ito Y, Koba S, Toyoda M, Ikejiri A, Saegusa H, et al. Clinical significance of small dense low-density lipoprotein cholesterol levels determined by the simple precipitation method. Arterioscler Thromb Vasc Biol. 2004;24:558–563. doi: 10.1161/01.ATV.0000117179.92263.08. [DOI] [PubMed] [Google Scholar]
- 12.Ai M, Otokozawa S, Asztalos BF, Ito Y, Nakajima K, White CC, et al. Small dense LDL cholesterol and coronary heart disease: results from the Framingham Offspring Study. Clin Chem. 2010;56:967–976. doi: 10.1373/clinchem.2009.137489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shoji T, Hatsuda S, Tsuchikura S, Shinohara K, Kimoto E, Koyama H, et al. Small dense low-density lipoprotein cholesterol concentration and carotid atherosclerosis. Atherosclerosis. 2009;202:582–588. doi: 10.1016/j.atherosclerosis.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 14.Arai H, Kokubo Y, Watanabe M, Sawamura T, Ito Y, Minagawa A, et al. Small dense low-density lipoproteins cholesterol can predict incident cardiovascular disease in an urban Japanese cohort: the Suita study. J Atheroscler Thromb. 2013;20:195–203. doi: 10.5551/jat.14936. [DOI] [PubMed] [Google Scholar]
- 15.Kathiresan S, Otvos JD, Sullivan LM, Keyes MJ, Schaefer EJ, Wilson PW, et al. Increased small low-density lipoprotein particle number: a prominent feature of the metabolic syndrome in the Framingham Heart Study. Circulation. 2006;113:20–29. doi: 10.1161/CIRCULATIONAHA.105.567107. [DOI] [PubMed] [Google Scholar]
- 16.Nozue T, Michishita I, Ishibashi Y, Ito S, Iwaki T, Mizuguchi I, et al. Small dense low-density lipoprotein cholesterol is a useful marker of metabolic syndrome in patients with coronary artery disease. J Atheroscler Thromb. 2007;14:202–207. doi: 10.5551/jat.e507. [DOI] [PubMed] [Google Scholar]
- 17.Nakano S, Kuboki K, Matsumoto T, Nishimura C, Yoshino G. Small, dense LDL and high-sensitivity C-reactive protein (hs-CRP) in metabolic syndrome with type 2 diabetes mellitus. J Atheroscler Thromb. 2010;17:410–415. doi: 10.5551/jat.1891. [DOI] [PubMed] [Google Scholar]
- 18.Sugino I, Kuboki K, Matsumoto T, Murakami E, Nishimura C, Yoshino G. Influence of fatty liver on plasma small, dense LDL- cholesterol in subjects with and without metabolic syndrome. J Atheroscler Thromb. 2011;18:1–7. doi: 10.5551/jat.5447. [DOI] [PubMed] [Google Scholar]
- 19.Lee M, Jang Y, Kim K, Cho H, Jee SH, Park Y, et al. Relationship between HDL3 subclasses and waist circumferences on the prevalence of metabolic syndrome: KMSRI-Seoul Study. Atherosclerosis. 2010;213:288–293. doi: 10.1016/j.atherosclerosis.2010.07.056. [DOI] [PubMed] [Google Scholar]
- 20.Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–1186. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 21.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 22.Srisawasdi P, Chaloeysup S, Teerajetgul Y, Pocathikorn A, Sukasem C, Vanavanan S, et al. Estimation of plasma small dense LDL cholesterol from classic lipid measures. Am J Clin Pathol. 2011;136:20–29. doi: 10.1309/AJCPLHJBGG9L3ILS. [DOI] [PubMed] [Google Scholar]
- 23.Kolovou GD, Anagnostopoulou KK, Kostakou PM, Mikhailidis D. Cholesterol ester transfer protein (CETP), postprandial lipemia and hypolipidemic drugs. Curr Med Chem. 2009;16:4345–4360. doi: 10.2174/092986709789712853. [DOI] [PubMed] [Google Scholar]
- 24.Barter PJ, Brewer HB, Jr, Chapman MJ, Hennekens CH, Rader DJ, Tall AR. Cholesteryl ester transfer protein: a novel target for raising HDL and inhibiting atherosclerosis. Arterioscler Thromb Vasc Biol. 2003;23:160–167. doi: 10.1161/01.atv.0000054658.91146.64. [DOI] [PubMed] [Google Scholar]
- 25.Tirosh A, Rudich A, Shochat T, Tekes-Manova D, Israeli E, Henkin Y, et al. Changes in triglyceride levels and risk for coronary heart disease in young men. Ann Intern Med. 2007;147:377–385. doi: 10.7326/0003-4819-147-6-200709180-00007. [DOI] [PubMed] [Google Scholar]
- 26.Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007;298:309–316. doi: 10.1001/jama.298.3.309. [DOI] [PubMed] [Google Scholar]
- 27.Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298:299–308. doi: 10.1001/jama.298.3.299. [DOI] [PubMed] [Google Scholar]
- 28.Stalenhoef AF, Graaf J. Association of fasting and nonfasting serum triglycerides with cardiovascular disease and the role of remnant-like lipoproteins and small dense LDL. Curr Opin Lipidol. 2008;19:355–361. doi: 10.1097/MOL.0b013e328304b63c. [DOI] [PubMed] [Google Scholar]
- 29.Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. 2013;5:1218–1240. doi: 10.3390/nu5041218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hokanson JE, Krauss RM, Albers JJ, Austin MA, Brunzell JD. LDL physical and chemical properties in familial combined hyperlipidemia. Arterioscler Thromb Vasc Biol. 1995;15:452–459. doi: 10.1161/01.atv.15.4.452. [DOI] [PubMed] [Google Scholar]
- 31.Capell WH, Zambon A, Austin MA, Brunzell JD, Hokanson JE. Compositional differences of LDL particles in normal subjects with LDL subclass phenotype A and LDL subclass phenotype B. Arterioscler Thromb Vasc Biol. 1996;16:1040–1046. doi: 10.1161/01.atv.16.8.1040. [DOI] [PubMed] [Google Scholar]
- 32.Reaven GM. Role of insulin resistance in human disease (syndrome X): an expanded definition. Annu Rev Med. 1993;44:121–131. doi: 10.1146/annurev.me.44.020193.001005. [DOI] [PubMed] [Google Scholar]
- 33.Toth P. Insulin resistance, small LDL particles, and risk for atherosclerotic disease. Curr Vasc Pharmacol. 2014;12:653–657. doi: 10.2174/15701611113119990125. [DOI] [PubMed] [Google Scholar]
- 34.Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82:495–506. doi: 10.1161/01.cir.82.2.495. [DOI] [PubMed] [Google Scholar]
- 35.Maeda S, Nakanishi S, Yoneda M, Awaya T, Yamane K, Hirano T, et al. Associations between small dense LDL, HDL subfractions (HDL2, HDL3) and risk of atherosclerosis in Japanese-Americans. J Atheroscler Thromb. 2012;19:444–452. doi: 10.5551/jat.11445. [DOI] [PubMed] [Google Scholar]
- 36.Kim YK, Seo HS, Lee EM, Na JO, Choi CU, Lim HE, et al. Association of hypertension with small, dense low-density lipoprotein in patients without metabolic syndrome. J Hum Hypertens. 2012;26:670–676. doi: 10.1038/jhh.2011.86. [DOI] [PubMed] [Google Scholar]
- 37.Cho Y, Kim Y, Kim JH, Jee SH, Han K. The plasma small dense LDL-cholesterol calculation formula proposed by Srisawasdi et al is not applicable to Koreans who are healthy or have metabolic syndrome. Am J Clin Pathol. 2012;138:754–755. doi: 10.1309/ajcpkkogej86lgju. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Data Table S1. Associations of sdLDL-C with metabolic variables in the presence of either metabolic syndrome or hypertriglyceridemia (TG >1.7 mmol/L) determined by multiple linear regression analysis.
| Parameter | MetS (n = 447) | Healthy population (n = 360) | ||||||
|---|---|---|---|---|---|---|---|---|
| Normal TG (n = 80) | Hypertriglyceridemia (n = 367) | Normal TG (n = 267) | Hypertriglyceridemia (n = 93) | |||||
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Age (yr) | 0.0025±0.0029 | 0.3903 | 0.0031±0.0018 | 0.0781 | 0.0020±0.0012 | 0.0827 | 0.0072±0.0038 | 0.0629 |
| WC (cm) | 0.0024±0.0034 | 0.4911 | 0.0051±0.0022 | 0.0212 | 0.0043±0.0016 | 0.0083* | 0.0098±0.0051 | 0.0574 |
| SBP (mm Hg) | -0.0002±0.0023 | 0.9372 | -0.0025±0.0015 | 0.0997 | 0.0000±0.0015 | 0.9871 | 0.0018±0.0042 | 0.6715 |
| DBP (mm Hg) | -0.0015±0.0033 | 0.6594 | 0.0060±0.0020 | 0.0031* | -0.0011±0.0017 | 0.5153 | 0.0040±0.0049 | 0.4190 |
| Fasting glucose (mmol/L) | 0.0283±0.0113 | 0.0147* | 0.0216±0.0078 | 0.0061* | 0.0656±0.0259 | 0.0119* | 0.1134±0.0756 | 0.1373 |
| TG (mmol/L) | 0.2148±0.0822 | 0.0109* | 0.1526±0.0121 | <0.0001* | 0.2665±0.0368 | <0.0001* | 0.2128±0.0382 | <0.0001* |
| HDL-C (mmol/L) | 0.1233±0.0966 | 0.2060 | -0.0261±0.0731 | 0.7208 | 0.0878±0.0370 | 0.0183* | 0.2492±0.1488 | 0.0977 |
| LDL-C (mmol/L) | 0.2792±0.0300 | <0.0001* | 0.3860±0.0191 | <0.0001* | 0.2490±0.0152 | <0.0001* | 0.2511±0.0422 | <0.0001* |
The components of MetS (WC, TG, HDL-C, SBP, DBP, FG), age, and LDL-C were included in the multiple linear regression analysis with an "enter" procedure, and P values <0.05 are indicated by *.
Abbreviations: MetS, metabolic syndrome; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol.
Scatterplots showing the correlation between the plasma concentration of small dense LDL cholesterol (sdLDL-C) (A) or the sdLDL-C/LDL-C ratio (B) and the homeostasis model assessment of insulin resistance (HOMA-IR) in patients with MetS (●) and healthy population (◦). Linear regression curve for the two variables are indicated in solid line (for patients with MetS) or dashed line (for healthy population).
Progressive increase in the small dense LDL cholesterol (sdLDL-C) concentration in men (A) and women (B), and the sdLDL-C/LDL-C ratio in men (C) and women (D), as a function of the number of metabolic syndrome components (P for trend < 0.001, for all).