Abstract
Background
Descent of the lateral aspect of the brow is one of the earliest signs of aging. The purpose of this study was to describe an open surgical technique for lateral brow lifts, with the goal of achieving reliable, predictable, and long-lasting results.
Methods
An incision was made behind and parallel to the temporal hairline, and then extended deeper through the temporoparietal fascia to the level of the deep temporal fascia. Dissection was continued anteriorly on the surface of the deep temporal fascia and subperiosteally beyond the temporal crest, to the level of the superolateral orbital rim. Fixation of the lateral brow and tightening of the orbicularis oculi muscle was achieved with the placement of sutures that secured the tissue directly to the galea aponeurotica on the lateral aspect of the incision. An additional fixation was made between the temporoparietal fascia and the deep temporal fascia, as well as between the temporoparietal fascia and the galea aponeurotica. The excess skin in the temporal area was excised and the incision was closed.
Results
A total of 519 patients were included in the study. Satisfactory lateral brow elevation was obtained in most of the patients (94.41%). The following complications were observed: total relapse (n=8), partial relapse (n=21), neurapraxia of the frontal branch of the facial nerve (n=5), and limited alopecia in the temporal incision (n=9).
Conclusions
We consider this approach to be a safe and effective procedure, with long-lasting results.
Keywords: Eyebrow; Sutures; Rejuvenation; Surgery, plastic
INTRODUCTION
Descent or flattening of the lateral aspect of the brow is one of the earliest signs of aging [1]. The traditional coronal approach to brow correction is a highly effective technique, but it has been replaced to a great extent by various endoscopic methods. Although the use of endoscopy enabled the application of a more limited approach in brow lift techniques, a disadvantage of endoscopic procedures is the fact that they frequently result in undercorrection of the brow position [2]. More recently, various non-endoscopic surgical techniques have been described, involving different planes of dissection, incisions, and fixation points, in an attempt to elevate the lateral brow in patients with an otherwise normal brow position [3,4,5,6,7,8,9,10,11,12,13,14].
We describe and illustrate an open surgical technique that allows us to elevate and reshape the lateral aspect of the brow, as well as to suspend the orbicularis oculi muscle, with the goal of improving the overall lateral canthal area.
METHODS
A retrospective review was performed of patients who underwent lateral brow lift using the proposed technique at our center over a 10-year period. The study protocol was approved by the national research ethics committee and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. All the patients signed a consent form prior to undergoing surgical correction of the lateral brow position.
The inclusion criteria were: (1) age >18 years, (2) no previous invasive or non-invasive brow lift procedures, (3) no history of trauma in the area of the upper face, (4) at least two years of follow-up, and (5) the presence of preoperative and postoperative photos.
Preoperatively, we evaluated the eyebrow position, possible asymmetries, and different vectors of brow elevation, with the patient awake and in a standing position. Preoperative measurements of the distance between the peak of the eyebrow and the lateral canthus were made using a digital caliper, in order to serve as a reference during follow-up (Fig. 1). The results of the procedure, including the presence and duration of complications, were evaluated at one, three, and six months after the procedure, with subsequent annual follow-up. Patients were advised not to use neuromodulators or fillers during follow-up. Patients who returned for follow-up and had undergone treatment with neuromodulators or fillers were excluded from the study. Digital photographs were taken to document the preoperative brow position, surgical technique, and postoperative results.
Fig. 1. Preoperative measurements and anatomical landmarks.
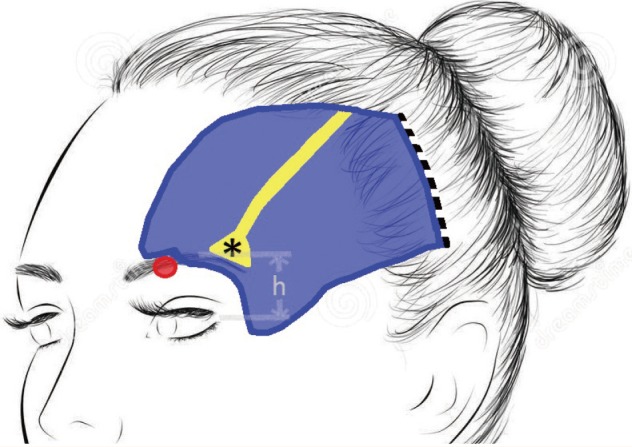
Preoperative measurements of the distance between the peak of the eyebrow and the lateral canthus (h) were made using a digital caliper to serve as a reference during follow-up. The skin incision (dashed black line) was placed 5-6 cm posterior to the temporal hairline. The area of dissection (blue area), the fascial adhesions in the temporal fusion line (yellow), and the area of the supraorbital notch (red circle) are illustrated. *, condensation of fibrous tissue between the periosteum and the superolateral orbital rim.
Surgical technique
The procedure was performed under local anesthesia, with or without intravenous sedation, or under general anesthesia. The hair was not cut or shaved. Taping the hair into bundles away from the incisions facilitated operative exposure. Infiltration consisting of 120 mL of 0.9% normal saline, 30 mL of 2% lidocaine, and 0.1 mL of 1:1,000 adrenaline was administered deep to the temporoparietal fascia laterally and subperiosteally medially to provide hydrodissection. Bitemporal curvilinear incisions of 7-8 cm were placed throughout the skin, well behind (5-6 cm) and parallel to the temporal hairline. The incisions did not extend medial to the superior temporal fusion line, thus avoiding any damage to the deep branch of the supraorbital nerve. The incision was extended deeper through the superficial temporal fascia to the level of the deep temporal fascia. Dissection was continued anteriorly, on the surface of the deep temporal fascia, to the temporal fusion line. Using a curved periosteal elevator, the fascia confluence (inferior and superior temporal line) was broken from the lateral aspect and the dissection was continued subperiosteally medially and towards the orbital rim, releasing the fibrous band that connects the orbital rim and the superficial temporal fascia deep to the lateral eyebrow (Fig. 1).
Once the tissue was mobilized, the lateral brow was elevated and fixation was achieved. For this purpose, three to four absorbable sutures (Vicryl 0, polyglactin 910) were placed (Fig. 2). Each suture was passed through the periosteum and fascia of the superolateral orbital rim, retracting the lateral eyebrow, reshaping it, and tightening the orbital portion of the orbicularis oculi muscle. The point of placement of each suture was altered from case to case in order to achieve the most aesthetically pleasing fixation of the brow. The sutures were secured laterally to the galea aponeurotica in the lateral margin of the incision, in a radial manner that determined the vector of elevation. The degree of tightening of each suture affected the extent of elevation as well as the shape of the brow. These stitches were left long enough in the hair-bearing temporal area of the scalp to facilitate their subsequent removal. One or two additional absorbable mattress sutures (Vicryl 2-0, polyglactin 910) were placed between the temporoparietal fascia and the immobile deep temporal fascia (Fig. 3). Finally, three to four absorbable sutures (Vicryl 2-0, polyglactin 910) were placed to anatomically restore the continuation of the temporoparietal fascia to the galea aponeurotica on the lateral margin of the incision. No drains were used. The excess skin in the temporal area was excised in a fusiform manner and the incision was closed with staples (Fig. 4). A head compression garment was maintained for 24 hours. Precise positioning and stable fixation were maintained with the aforementioned sutures. The initial sutures were removed two weeks postoperatively if any pinching of the skin was noted as healing progressed.
Fig. 2. Lateral eyebrow elevation and fixation with sutures.
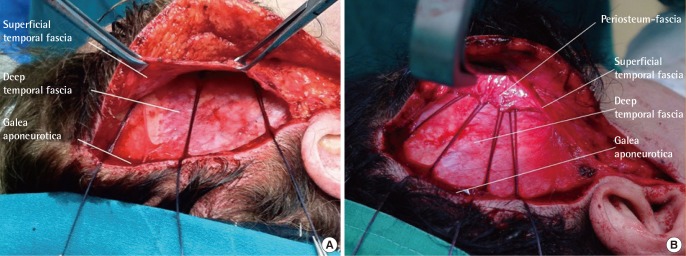
(A) Three absorbable sutures (Vicryl 0, polyglactin 910) were passed through the periosteum and fascia of the superolateral orbital rim and secured to the galea of the posterior edge of the lateral incision. They were left long enough in the hair-bearing temporal area of the scalp to facilitate their subsequent removal two weeks postoperatively if any pinching of the skin was observed as healing progressed. (B) A patient in whom four sutures (Vicryl 0, polyglactin 910) were placed in a radial manner, achieving a wider vector of elevation.
Fig. 3. "Key" sutures.
One or two additional absorbable mattress sutures (Vicryl 2-0, polyglactin 910) were placed between the temporoparietal fascia and the immobile deep temporal fascia. These are considered "key" sutures, as they bear the entire strain of the temporofrontal compound flap.
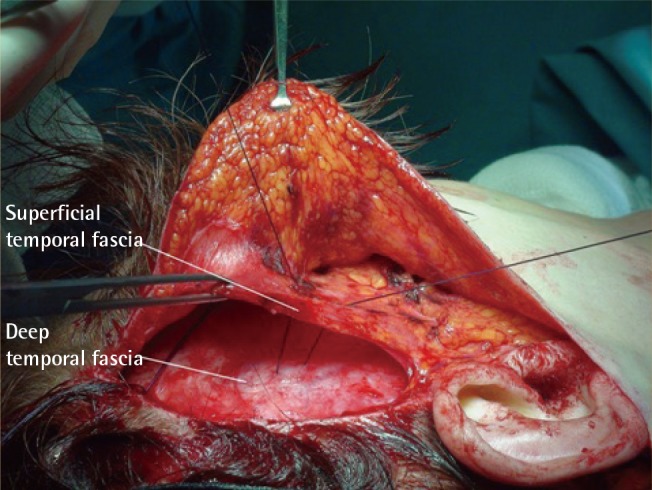
Fig. 4. Temporal skin excision.

The excess skin in the temporal area was excised in a fusiform manner and the incision was closed with staples. The sutures that were left long enough (asterisk), are visible through the skin incision in the hair-bearing temporal area of the scalp.
RESULTS
A total of 519 patients were enrolled in this study (Table 1), of whom 471 were female and 48 were male (Figs. 5, 6, 7, 8, 9). The mean age of the patients was 57.3±11.2 years. The mean follow-up was 4.08±2.38 years. In 318 of the 519 patients (61.27%), the procedure was performed in combination with a face lift and superior and inferior blepharoplasty; in 124 of the 519 patients (23.89%), the procedure was combined with upper blepharoplasty; and in 78 of the 519 cases (15.02%), the procedure was performed in isolation. However, these 78 patients had previously undergone upper blepharoplasty. We are of the opinion that the brow position was not affected by the associated blepharoplasty procedure.
Table 1. Patients excluded from the study due to exclusion criteria during the follow-up period.
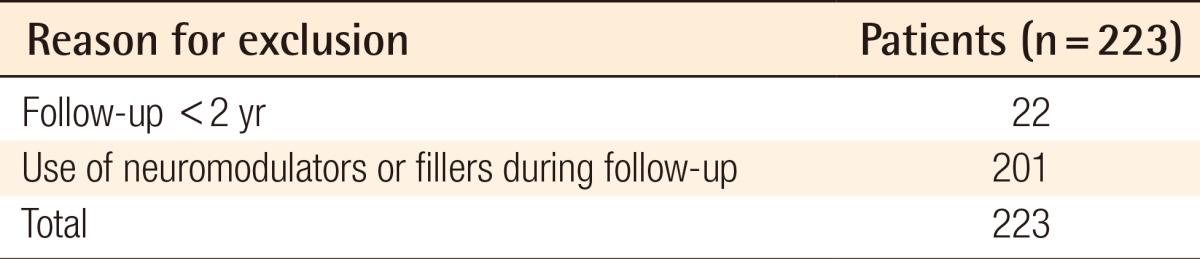
Fig. 5. Lateral brow lift with upper and lower blepharoplasty.
(A) Preoperative view. (B) Postoperative view after four years and three months.
Fig. 6. Lateral brow lift with upper and lower blepharoplasty.
(A) Preoperative view. (B) Postoperative view after six months.
Fig. 7. Lateral brow lift with facelift and upper and lower blepharoplasty.
(A) Preoperative view. (B) Postoperative view after seven years and one month.
Fig. 8. Lateral brow lift with upper and lower blepharoplasty.
(A) Preoperative view. (B) Postoperative view after one month.
Fig. 9. Lateral brow lift with upper blepharoplasty.
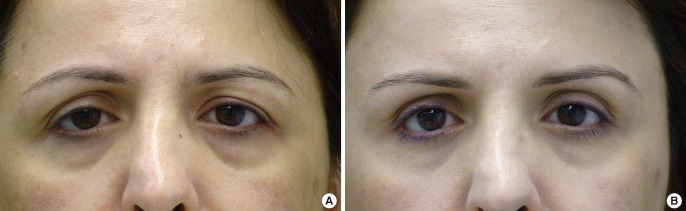
(A) Preoperative view. (B) Postoperative view after three years and five months.
Long-lasting lateral eyebrow lift was obtained in most patients (94.41%), with correct eyebrow movement. We observed total recurrence of brow ptosis in eight of the 519 patients (1.54%), and partial recurrence in 21 of the 519 patients (4.04%). No cases of excessive elevation of the eyebrows were observed.
Neurapraxia of the frontal branch of the facial nerve was observed in five patients (1.34%), all of whom recovered spontaneously after three to six months (Table 2).
Table 2. Complications.
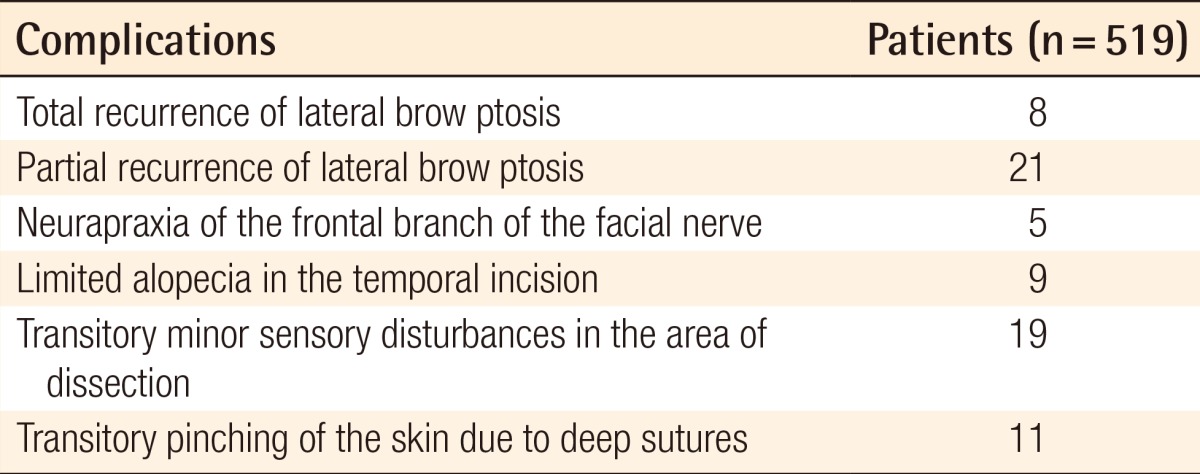
In nine patients (1.73%), limited (0.5-1 cm in width) alopecia in the incision site was observed. It was treated with excision and direct closure under local anesthesia. We are of the opinion that this limited alopecia was not related to the skin excision in the temporal area, as the closure of the skin was achieved with no tension at all.
Mild postoperative tension-related pain was present in most patients and was easily treated with simple analgesics. Sensory disturbances were minor, both in the area of dissection and posterior to the incision, and subsided in several weeks. No cases of permanent numbness in the areas innervated by the deep branch of the supraorbital nerve were observed postoperatively. No cases of hematoma, seroma, or infection were observed.
In 11 patients (2.11%), the long sutures were removed because of pinching of the skin. However, this was not due to failure of the technique, as the removal of these stitches did not affect the brow lift and immediately resolved the pinching of the skin.
DISCUSSION
The transcoronal brow lift is a versatile technique that rejuvenates the entire upper third of the face [15]. Alopecia in the incision line, permanent numbness, elevation of the hairline, possible neuroma formation, and prolonged recovery time [16] have motivated the replacement of this technique by less invasive procedures, either in the form of endoscopic procedures or limited-incision open approaches.
The use of endoscopy in brow rejuvenation generally produces good and predictable results [2,17,18]. Nevertheless, the increased cost of the endoscopic equipment and the prolonged time of the procedure have led surgeons to seek alternatives.
However, direct brow lifting leaves visible scars, whereas transpalpebral brow lifting achieves a limited amount of lifting and has high rates of relapse [15].
Furthermore, the use of subcutaneous thread lifts has specific indications [19], and the use of botulin toxin is not predictable in terms of the amount of lift and is only effective for several months.
Several authors have described non-endoscopic limited-incision open methods to elevate or stabilize the position of a ptotic lateral brow. These techniques vary with respect to incision length and location, plane of dissection, and method of fixation. Skin-only temporal brow lifts [10] lack a second deeper layer of dissection and advancement for suspension. Biplanar techniques involve a coronal incision [20]. In other multiplanar dissection techniques, the second plane of dissection is subcutaneous [14], becomes subcutaneous far anterior to the skin incision [21], or is dissected in the midface only [22].
Ptosis of the lateral third of the eyebrow occurs earlier and is more conspicuous than ptosis of the medial area [1,23,24]. Frontalis muscle fibers interdigitate downward with the orbicularis oculi muscle. Consequently, as the brow becomes ptotic, the orbicularis oculi muscle, along with the overlying skin, also droops.
The technique described in this report corrects lateral brow ptosis, reshapes the brow, and allows fixation as well as expansion and repositioning of the superolateral periorbita. Thus, a significant improvement in the overall lateral canthal area is achieved. This technique avoids extensive incisions, bleeding, permanent anesthesia, and large scars, and does not require the use of expensive equipment such as an endoscope or sophisticated devices for fixation. The incisions are well hidden in the hair-bearing temporal scalp, and are kept lateral to the superior temporal fusion line, thus avoiding any damage to the deep branch of the supraorbital nerve. The technique has stable results, as the entire support is made between inelastic aponeurotic layers [25]. The plane of dissection protects the frontal branch of the facial nerve, as the nerve is always kept above the plane of dissection, in more superficial layers. The use of a retractor with integrated cold light facilitates the dissection and identification of all anatomical structures, as well as providing good visibility and control if any bleeding occurs. Usually, complete release of the periosteum in the superolateral orbital rim is required, along with identification and protection of the supraorbital nerve, to allow the tissue to move more freely.
In our proposed technique, we applied more vectors of brow elevation, than have been applied in previously described procedures, using three to four initial sutures. The initial three to four absorbable sutures offer direct and precise traction of the tissue that is captured in the suture bite. Depending on the case, the point of placement of each suture may be altered in order to achieve the most aesthetically pleasing shaping and lifting of the brow. The next two sutures, which are placed between the temporoparietal fascia and the deep temporal fascia, are considered "key" sutures, as they take the entire strain of the temporofrontal compound flap. Finally, the edge of the temporoparietal fascia is sutured with the galea aponeurotica. This multi-point suture fixation ensures long-lasting results and is a major advantage of this technique.
The excess skin in the temporal area is excised in a fusiform manner, aiming to achieve a no-tension skin closure with staples, thus avoiding problems with alopecia in the suture line.
No complications were recorded that were directly related to this fixation technique. We relied on adequate undermining and release of the soft tissue, the upward and lateral traction of the undermined tissues, and the stable fixation of the elevated frontotemporal compound flap at multiple points. We have observed satisfactory and long-lasting results in the patients who were treated with this technique.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Knize DM. An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg. 1996;97:1321–1333. doi: 10.1097/00006534-199606000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Chiu ES, Baker DC. Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg. 2003;112:628–633. doi: 10.1097/01.PRS.0000071042.11435.2E. [DOI] [PubMed] [Google Scholar]
- 3.Gleason MC. Brow lifting through a temporal scalp approach. Plast Reconstr Surg. 1973;52:141–144. doi: 10.1097/00006534-197308000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001;108:1409–1424. doi: 10.1097/00006534-200110000-00048. [DOI] [PubMed] [Google Scholar]
- 5.Gasperoni C, Salgarello M, Gargani G. Subperiosteal lateral browlift and its relationship to upper blepharoplasty. Aesthetic Plast Surg. 1993;17:243–246. doi: 10.1007/BF00636269. [DOI] [PubMed] [Google Scholar]
- 6.Dempsey PD, Oneal RM, Izenberg PH. Subperiosteal brow and midface lifts. Aesthetic Plast Surg. 1995;19:59–68. doi: 10.1007/BF00209312. [DOI] [PubMed] [Google Scholar]
- 7.Byrd HS, Andochick SE. The deep temporal lift: a multiplanar, lateral brow, temporal, and upper face lift. Plast Reconstr Surg. 1996;97:928–937. doi: 10.1097/00006534-199604001-00007. [DOI] [PubMed] [Google Scholar]
- 8.Knize DM. Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg. 1996;97:1334–1342. doi: 10.1097/00006534-199606000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Lassus C. Elevation of the lateral brow without the help of an endoscope. Aesthetic Plast Surg. 1999;23:23–27. doi: 10.1007/s002669900237. [DOI] [PubMed] [Google Scholar]
- 10.Miller TA, Rudkin G, Honig M, et al. Lateral subcutaneous brow lift and interbrow muscle resection: clinical experience and anatomic studies. Plast Reconstr Surg. 2000;105:1120–1127. doi: 10.1097/00006534-200003000-00044. [DOI] [PubMed] [Google Scholar]
- 11.Strauch B, Baum T. Correction of lateral brow ptosis: a nonendoscopic subgaleal approach. Plast Reconstr Surg. 2002;109:1164–1167. doi: 10.1097/00006534-200203000-00059. [DOI] [PubMed] [Google Scholar]
- 12.Tuccillo F, Jacovella P, Zimman O, et al. An alternative approach to brow lift fixation: temporoparietalis fascia, galeal, and periosteal imbrication. Plast Reconstr Surg. 2007;119:692–702. doi: 10.1097/01.prs.0000246526.59290.57. [DOI] [PubMed] [Google Scholar]
- 13.Marshak H, Morrow AA, Morrow DM. Biplanar temple lift for lateral brow ptosis: comparison with uniplanar dissection technique. Aesthetic Plast Surg. 2008;32:517–522. doi: 10.1007/s00266-008-9131-0. [DOI] [PubMed] [Google Scholar]
- 14.Centurion P, Romero C. Lateral brow lift: a surgical proposal. Aesthetic Plast Surg. 2010;34:745–757. doi: 10.1007/s00266-010-9537-3. [DOI] [PubMed] [Google Scholar]
- 15.Nahai F. Clinical decision-making in brow lift. In: Nahai F, editor. The art of aesthetic surgery: principles & techniques. St. Louis: Quality Medical Pub.; 2005. pp. 536–550. [Google Scholar]
- 16.Elkwood A, Matarasso A, Rankin M, et al. National plastic surgery survey: brow lifting techniques and complications. Plast Reconstr Surg. 2001;108:2143–2150. doi: 10.1097/00006534-200112000-00056. [DOI] [PubMed] [Google Scholar]
- 17.Foustanos A, Zavrides H. An alternative fixation technique for the endoscopic brow lift. Ann Plast Surg. 2006;56:599–604. doi: 10.1097/01.sap.0000203317.50871.5c. [DOI] [PubMed] [Google Scholar]
- 18.de la Fuente A, Santamaria AB. Endoscopic forehead lift: is it effective? Aesthet Surg J. 2002;22:113–120. doi: 10.1067/maj.2002.122939. [DOI] [PubMed] [Google Scholar]
- 19.Sulamanidze M, Sulamanidze G. APTOS suture lifting methods: 10 years of experience. Clin Plast Surg. 2009;36:281–306. doi: 10.1016/j.cps.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Ramirez OM. Endoscopically assisted biplanar forehead lift. Plast Reconstr Surg. 1995;96:323–333. doi: 10.1097/00006534-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Fogli AL. Temporal lift by galeapexy: a review of 270 cases. Aesthetic Plast Surg. 2003;27:159–165. doi: 10.1007/s00266-003-0062-5. [DOI] [PubMed] [Google Scholar]
- 22.de la Fuente A, Honig JF. Video-assisted endoscopic transtemporal multilayer upper midface lift (MUM-Lift) J Craniofac Surg. 2005;16:267–276. doi: 10.1097/00001665-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Lemke BN, Stasior OG. The anatomy of eyebrow ptosis. Arch Ophthalmol. 1982;100:981–986. doi: 10.1001/archopht.1982.01030030989019. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan PK, Salomon JA, Woo AS, et al. The importance of the retaining ligamentous attachments of the forehead for selective eyebrow reshaping and forehead rejuvenation. Plast Reconstr Surg. 2006;117:95–104. doi: 10.1097/01.prs.0000185862.37301.32. [DOI] [PubMed] [Google Scholar]
- 25.Psillakis JM, Rumley TO, Camargos A. Subperiosteal approach as an improved concept for correction of the aging face. Plast Reconstr Surg. 1988;82:383–394. doi: 10.1097/00006534-198809000-00001. [DOI] [PubMed] [Google Scholar]






