Abstract
Aim:
Complementary and alternative medicine (CAM) is commonly used all over the world, and herbal medicines are the most preferred ways of CAM. The aim of this study was to determine the frequency of herbal medicine use among patients with chronic diseases.
Methodology:
A cross-sectional descriptive study was conducted from April 2014 to December 2014 among patients who had been diagnosed with diabetes mellitus (DM), hypertension (HT), and hyperlipidemia (HL) in Family Medicine Department of Dışkapı Yıldırım Beyazıt Training and Research Hospital, in Ankara. A questionnaire about herbal drug use was applied by face to face interview to the participants.
Results:
A total of 217 patients were included in this study. The mean age of the participants was 56.6 ± 9.7 years (55 male and 162 female). The rate of herbal medicine use was 29%. Herbal medicine use among female gender was significantly higher (P = 0.040). Conventional medication use was found to be lower among herbal medicine consumers. There was no relationship between herbal medicine use and type of chronic disease, living area, and occupation or education level. Most frequently used herbs were lemon (39.6%) and garlic (11.1%) for HT, cinnamon (12.7%) for DM, and walnut (6.3%) for HL.
Conclusions:
In this study, herbal medicine use was found to be higher among patients who had been diagnosed with chronic diseases. Therefore, physicians should be aware of herbal medicine usage of their patients and inform them about the effectivity and side effects of herbal medicines.
KEY WORDS: Diabetes, herbal medicines, hyperlipidemia, hypertension, phytotherapy
INTRODUCTION
Complementary and alternative medicine (CAM) is commonly used all over the world [1]. Herbal medicines are the most preferred ways of CAM [2]. In USA, 38% of the population use herbal medicines [3]. Soner et al. found that 48.8% of people use herbal medicine in Turkey [4]. People use herbal medicines to be healthier, prevent or treat diseases. Although herbal products are believed to be harmless among consumers, they might have side effects, and they have potential to cause drug interactions [5,6]. This is a particular concern in patients with chronic diseases who utilize polypharmacy.
Although Turkey has a long tradition of using herbal medicine, the data about the frequency of utilization of herbal medicine in chronic diseases are scarce [4,7-12]. Therefore, in this study, we aimed to determine the frequency of the use of herbal medicine among patients who had been diagnosed with diabetes mellitus (DM), hypertension (HT), and hyperlipidemia (HL) in family medicine department.
METHODOLOGY
A cross-sectional descriptive study was conducted among adult patients (n = 232) who had been followed with DM, HT, HL from April 2014 to December 2014 in Hasköy Outpatient Clinics of Family Medicine Department of Dışkapı Yıldırım Beyazıt Training and Research Hospital in Ankara. Eligible patients who gave informed consent were included in the study.
A face-to-face questionnaire was administered to the participants by the first author. The questionnaire included information about socio-demographic features, chronic diseases, conventional medications, and herbal medicine use. Compliance to conventional medicine use was defined as compliance and non-compliance whether the patients regularly had received their prescribed drugs according to the clinicians’ instructions. In addition, data about the name of the herbal medicine, the reasons for herbal use, belief about effectivity, knowledge about potential adverse effects, and by whom (e.g., families or friends, media or health care providers) its use was recommended were collected.
The study was approved by Local Ethical Committee of Dışkapı Yıldırım Beyazıt Training and Research Hospital.
Data Analysis
The data obtained from the study were analyzed using Statistical Package for Social Sciences version 15 for Windows. Descriptive statistics is presented as mean ± standard deviation, range, and frequency (% values). Chi-square test or Fisher’s exact test was used for categorical variables and Student’s t-test for normally distributed data with equal variances. A P < 0.05 considered as statistically significant.
RESULTS
A total of 217 patients were included in this study. The mean age of the participants was 56.6 ± 9.7 years. There were 55 male (25.4%) and 162 female (74.6%) patients. It was found that 96.2% of women were housewives and 63.6% of men were retired. There were 35 patients (16.1%) who had DM, 59 patients (27.2%) who had HT, 7 patients (3.2%) who had HL, and there were 116 patients (53.5%) who had more than one disease. Among those patients, 212 of them (97.7%) used conventional medicine and 122 of them (56.2%) went check-up regularly. The socio-demographic and clinical features of the study population are presented in Table 1.
Table 1.
The socio-demographic and clinical features of the study population
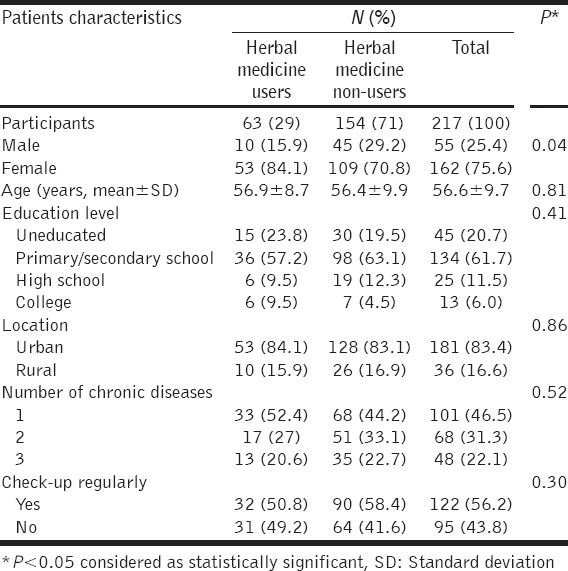
The number of herbal medicine users was 63. Herbal medicine use was found to be significantly higher among female gender (P = 0.04). Conventional medication use was found to be lower among herbal medicine consumers (97.3% vs. 99.4%).
Herbal medicines were commonly recommended to the users by their families or friends (61.9%), by media (27%), and by health care providers (11.1%), respectively. Herbal medicines were merely recommended by professional health care providers (7.9% by physicians, 3.2% by pharmacists).
Among those herbal medicine users, 68.3% thought that herbal medicines had a good effect, 11.1% had a minor effect, and 20.6% had no effect on their medical conditions. A total of 54 herbal medicine users (85.7%) thought that herbal medicines had no adverse effects, 7 (11.1%) thought they might have adverse effects, 2 (3.2%) had no idea.
The most common reasons of herbal medicine use were to increase the effectiveness of the conventional medications (39.7%), to believe that they were harmless (33.3%), to find them more effective (25.6%), and cheaper (1.6%) than the conventional drugs.
Most frequently used herbs were lemon (39.6%) and garlic (11.1%) for HT, cinnamon (12.7%) for DM, and walnut (6.3%) for HL. Four patients (6.3%) were using herbal mixtures without knowing the ingredients. Patients mostly use roots, leaves, fruits or seeds of plants which can be found easily.
DISCUSSION
DM, HT, and HL are the most prevalent chronic diseases in the world. According to TURDEP-2 and TEKHARF studies, the prevalence of DM is 16.6%, the prevalence of HT is 31.6%, and the prevalence of HL is 37.3% in Turkey [13,14].
Recent studies support the popularity and increasing use of CAM by individuals in western countries as well as in Turkey [2,4,9,10]. We found approximately one-third of our patients had used herbal medicine for the treatment of chronic diseases. The differences in the reported rates of herbal medicine use might depend on socio-demographic features of study population even in the same country. Biçen et al. reported 53% herbal medicine use for HT in a study population similar to our study population (most of the individuals were female, mean age was 57.6 years, and education level was low) [11]. Soner et al. found 48.8% herbal use in a population mostly consisted of female inpatients with the median age 37.0 years and with higher education levels [4]. However, Gücük et al. reported lower rates (16%) herbs use in cardiovascular disease among male predominant patients with the mean age of 49 ± 13 years [7].
The proposed reasons of the prevalent use of herbal medicines were insufficient controlling in the market, ease of reaching to the products, and over advertising of those products by media [15].
It was shown that women are more prone to use herbal medicines [3,4,7]. Our findings were also compatible with those previous reports. Hence, most of the women were housewives (96.2%) in our study population. The television programs, especially for women may be the possible explanation for this cause. Herbal medicines are mentioned a lot on these kinds of programs.
In contrast to the studies [3,4,7], we did not find a relationship between herbal medicine use and education level. Previous studies found that people who had high education level were more likely to use herbal medicines.
It is known that compliance to conventional drugs in chronic diseases is low [16]. Although the effectiveness of the herbal medicines in the treatment of chronic diseases has not been clearly documented, we found that non-compliance with conventional medication was found to be higher in herbal medicine users. This preference has potential to jeopardize the patients’ health. Furthermore, we found that most of the patients believed that herbal medicine was effective (68.3% good effect, 11.1% minor effect) and had no adverse effects (85.7%). Although there were 7 patients (11.1%) who thought herbal medicines might have adverse effects, we did not ask their experiences about adverse effects. Unfortunately, we did not collect data about the impact of those medications on our patients’ medical conditions (e.g., blood pressure, hemoglobin A1c levels or lipid profiles). Soner et al. found that 53.2% of the study population believed that herbal medicines were not harmful, had less side effects or completely safe; they also found that 11.3% of the herbal medicine users had adverse effects such as palpitation, abdominal pain or hot flushing [4].
In addition, we found that herbal medicines were merely recommended by professional health care providers (7.9% by physicians, 3.2% by pharmacists). Family and friends or media were the main sources of information as seen in previous studies [4,7,11,17]. This is another important point, which could lead to negative outcomes in the treatment. The potential side-effect and outcome influence may be brought about by combinated use of herbal medicine and conventional drugs, and these circumstances are always difficult to predict because elucidating the exact mechanism of each extract of an herb that affects drug’s pharmacokinetic is still incomplete. Hence, adverse drug reactions, toxicities, and treatment failure are more likely to occur when drugs are consumed with herbs [18]. To date, an increasing number of studies in evaluating herbal medicine-drug interaction have been reported, and many herbal drugs and products interactions and side effects are well-known [5,19,20]. For example, concomitant use of danshen (Salvia miltiorrhiza) and warfarin may exaggerate the anticoagulant effect of warfarin and possibly cause bleeding [21]. Korean/Asian ginseng (Panax ginseng) and American ginseng (Panax quinquefolius) have antidiabetic effects [22-24] using ginseng concurrently with oral hypoglycemic agents or insulin injections may increase the risk of hypoglycemia [25]. Therefore, herbs should be used with the control of a professional health-care provider. We do not know the attitudes of the health care professionals for herbal medicines in Turkey which should be further evaluated.
Although 20.6% of the herbal medicine users thought that herbal medicine was ineffective for their treatment, and 11.1% of them believed that herbal medicines might have had adverse effects, interestingly they continued to use herbal medicines. Efe et al. found that 45.3% of the patients believed that herbal medicines were effective for HT [17].
Patients mostly use roots, leaves, fruits or seeds of plants which can be found easily, according to our study. Studies on this subject are limited in order to compare our results. Efe et al. found that 74.7% of patients used CAM (mostly herbal medicines) for HT and lemon was the most preferred one [17]. The results are consistent with our study. Although lemon was the most preferred one for HT, its effectiveness for decreasing blood pressure was not shown before certainly [26].
According to our knowledge, this is the first study in Turkey about herbal medicine use among three, most prevalent chronic diseases. However, our study also has limitations. First of all, this is a local study and the number of participants is limited. The sample is not likely to be representative of the entire population. Second, the source of information was subjective and according to the declaration of patients.
CONCLUSION
In this study, herbal medicine use was found to be higher among patients with chronic diseases and most of the patients used herbal medicine without professional recommendations. There were also patients who prefer to use herbal medicines instead of their prescribed drugs. Therefore, physicians should be aware of herbal medicine usage of their patients and inform them about the effectivity and side effects of herbal medicines.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wu CH, Wang CC, Kennedy J. Changes in herb and dietary supplement use in the U.S. adult population: A comparison of the 2002 and 2007 National health interview surveys. Clin Ther. 2011;33:1749–58. doi: 10.1016/j.clinthera.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 2.Fox P, Coughlan B, Butler M, Kelleher C. Complementary alternative medicine (CAM) use in Ireland: A secondary analysis of SLAN data. Complement Ther Med. 2010;18:95–103. doi: 10.1016/j.ctim.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Barnes PM, Bloom B, Nahi RL. Complementary and alternative medicine use among adults and children: United States 2007. Natl Health Stat Rep. 2008;12:1–23. [PubMed] [Google Scholar]
- 4.Soner BC, Şahin AS, Şahin TK. A survey of Turkish hospital patients'use of herbal medicine. Eur J Integrat Med. 2013:547–52. [Google Scholar]
- 5.Cvijovic K, Boon H, Barnes J, Brulotte J, Jaegar W, Murty M, et al. A tool for rapid identification of potential herbal medicine-drug interactions. Can Pharm J. 2009;142:1–2. [Google Scholar]
- 6.Lin SS, Tsai CL, Tu CY, Hsieh CL. Reducing drug-herb interaction risk with a computerized reminder system. Ther Clin Risk Manag. 2015;11:247–53. doi: 10.2147/TCRM.S78124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gücük Ipek E, Güray Y, Demirkan B, Güray U, Kafes H, Basyigit F. The prevalence of alternative herbal medicine and nutritional complementary product intake in patients admitted to out-patient cardiology departments. Turk Kardiyol Dern Ars. 2013;41:218–24. doi: 10.5543/tkda.2013.15146. [DOI] [PubMed] [Google Scholar]
- 8.Keskin A, BIlge U. Mental disorders frequency alternative and complementary medicine usage among patients with hypertension and type 2 diabetes mellitus. Niger J Clin Pract. 2014;17:717–22. doi: 10.4103/1119-3077.144384. [DOI] [PubMed] [Google Scholar]
- 9.Koc Z, Avci IA, Saglam Z. The use of complementary and alternative medicine by older patients that have chronic diseases. Health Med. 2012;6:413–22. [Google Scholar]
- 10.Aydın S, Bozkaya AO, Mazıcıoğlu M, Gemalmaz A, Özçakır A, Öztürk A. What influences herbal medicine use?Prevalence and related factors. Turk J Med Sci. 2008;38:455–63. [Google Scholar]
- 11.Biçen C, Elver Ö, Erdem E, Kaya C, Karataş A, Dilek M, et al. Herbal product use in hypertension patients. J Exp Clin Med. 2012;29:109–12. [Google Scholar]
- 12.Toprak D, Demir S. Treatment choices of hypertensive patients in Turkey. Behav Med. 2007;33:5–10. doi: 10.3200/BMED.33.1.5-10. [DOI] [PubMed] [Google Scholar]
- 13.Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–80. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yumuk VD. Prevalence of obesity in Turkey. Obes Rev. 2005;6:9–10. doi: 10.1111/j.1467-789X.2005.00172.x. [DOI] [PubMed] [Google Scholar]
- 15.Krasuski RA, Michaelis K, Eckart RE. The cardiovascular patient's perceptions of complementary and alternative medicine. Clin Cardiol. 2006;29:161–4. doi: 10.1002/clc.4960290407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hacıhasanoğlu R. Treatment compliance affecting factors in hypertension. TAF Prev Med Bull. 2009;8:167–72. [Google Scholar]
- 17.Efe D, Akca NK, Kiper S, Aydin G, Gumus K. Supportive methods used by individuals with hypertension to decrease blood pressure. Spatula DD. 2012;2:201–12. [Google Scholar]
- 18.Chen XW, Sneed KB, Pan SY, Cao C, Kanwar JR, Chew H, et al. Herb-drug interactions and mechanistic and clinical considerations. Curr Drug Metab. 2012;13:640–51. doi: 10.2174/1389200211209050640. [DOI] [PubMed] [Google Scholar]
- 19.Brantley SJ, Argikar AA, Lin YS, Nagar S, Paine MF. Herb-drug interactions: Challenges and opportunities for improved predictions. Drug Metab Dispos. 2014;42:301–17. doi: 10.1124/dmd.113.055236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu MZ, Zhang YL, Zeng MZ, He FZ, Luo ZY, Luo JQ, et al. Pharmacogenomics and herb-drug interactions: Merge of future and tradition. Evid Based Complement Alternat Med 2015. 2015:321091. doi: 10.1155/2015/321091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai HH, Lin HW, Lu YH, Chen YL, Mahady GB. A review of potential harmful interactions between anticoagulant/antiplatelet agents and Chinese herbal medicines. PLoS One. 2013;8:e64255. doi: 10.1371/journal.pone.0064255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeon WJ, Oh JS, Park MS, Ji GE. Anti-hyperglycemic effect of fermented ginseng in type 2 diabetes mellitus mouse model. Phytother Res. 2013;27:166–72. doi: 10.1002/ptr.4706. [DOI] [PubMed] [Google Scholar]
- 23.Xie JT, Mchendale S, Yuan CS. Ginseng and diabetes. Am J Chin Med. 2005;33:397–404. doi: 10.1142/S0192415X05003004. [DOI] [PubMed] [Google Scholar]
- 24.Sen S, Querques MA, Chakrabarti S. North American Ginseng (Panax quinquefolius) prevents hyperglycemia and associated pancreatic abnormalities in diabetes. J Med Food. 2013;16:587–92. doi: 10.1089/jmf.2012.0192. [DOI] [PubMed] [Google Scholar]
- 25.Kim DH. Chemical diversity of Panax ginseng, panax quinquifolium, and Panax notoginseng. J Ginseng Res. 2012;36:1–15. doi: 10.5142/jgr.2012.36.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kato Y, Domoto T, Hiramitsu M, Katagiri T, Sato K, Miyake Y, et al. Effect on blood pressure of daily lemon ingestion and walking. J Nutr Metab 2014. 2014:912684. doi: 10.1155/2014/912684. [DOI] [PMC free article] [PubMed] [Google Scholar]