Abstract
Developmental anomalies and anatomic variations of the thyroid gland in the general population with no known thyroid dysfunction usually goes unnoticed. Only those patients with neck swellings, incidentally detected hypo or hyperthyroidism, and those with a maternal history of hypothyroidism undergo screening for the thyroid gland. Neck ultrasound and scintigraphic techniques are the imaging tools routinely used to identify these anomalies. We present interesting technetium (Pertechnetate and sestaMIBI) scintigraphic images of adults and children who presented to our department with thyroid dysfunction showing developmental anomalies of the thyroid.
Keywords: Developmental thyroid anomalies, TcO4 thyroid scan, Sestamibi thyroid scan
INTRODUCTION
Thyroid dysgenesis refers to structural anomalies of the thyroid gland. Thyroid agenesis or ectopia is responsible for 85% of congenital hypothyroidism.
Developmental anomalies and anatomic variations of the thyroid gland in the general population with no known thyroid dysfunction usually goes unnoticed. Only those patients with neck swellings, incidentally detected hypo or hyperthyroidism, and those with a maternal history of hypothyroidism undergo screening for the thyroid gland. Neck ultrasound and scintigraphic techniques are the imaging tools routinely used to identify these anomalies.
The thyroid gland is the first endocrine gland to develop, at approximately the 24th day of gestation. The gland originates as a proliferation of endodermal epithelial cells on the median surface of the developing pharyngeal floor [Figure 1]. The site of this initial development lies between two key structures, the tuberculum impar, and the copula and is known as the foramen caecum. It then migrates down from the foramen cecum at the posterior aspect of the tongue, to its permanent location anterior to the trachea by 7th week of life. This normal migration can be disrupted at any point, and thyroid tissue coming to rest in unusual locations within the neck.[1]
Figure 1.
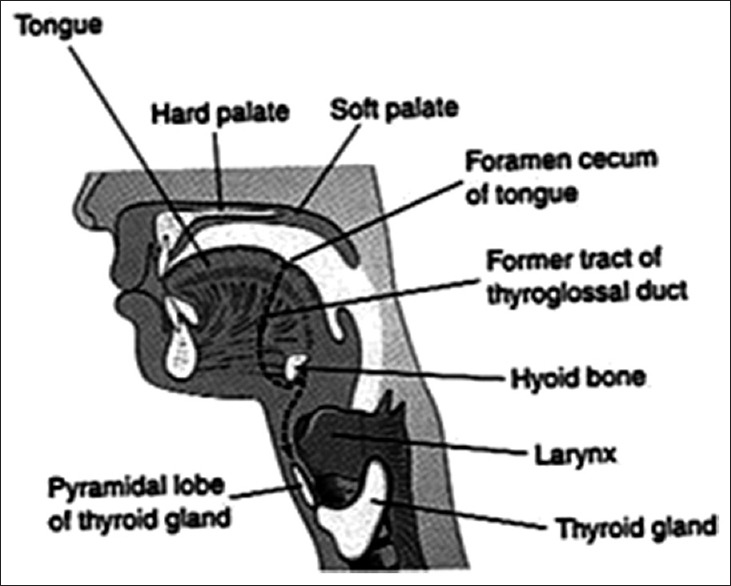
Illustration of path of descent and sites of ectopic thyroid remnants during embryonic development
MATERIALS AND METHODS
Images of 628 children and adults who had undergone Technetium pertechnetate/99mTcO4/sestaMIBI (MIBI) thyroid imaging for 75–370 Mega becquerel (MBq) of either 99mTcO4/99mTc MIBI was injected intravenously (dose adjusted to body weight in children, 1–5 MBq/kg). All hypothyroid patients on thyroxine replacement underwent MIBI thyroid study only; as thyroxine intake could mask the technetium trapping function of thyroid gland. 99mTcO4 planar neck images were acquired 15–30 min postinjection and 99mTc MIBI images were acquired 10–15 min postinjection. Single photon emission computed tomography along with computed tomography (SPECTCT) of the neck was performed only in selected cases.
Acquisition parameters
For 99mTc04/99mTc MIBI thyroid scan, an anterior image using 128 × 128 or 256 × 256 matrix was acquired using high-resolution parallel hole collimators for 100,000–200,000 counts or 5 min whichever occurs first. Localization markers were used in patients with neck nodules either at sternal notch or at the thyroid cartilage level.
Single photon emission computed tomography images were acquired on a GE Infinia Hawkeye dual head, variable angle gamma camera system. SPECT data were acquired over a 360° arc, using a body-contoured elliptical orbit, obtaining a minimum of 60 projections at 15–25 s/projection (average acquisition time: Around 20–25 min) The images were acquired into an 128 × 128 (16-bit) matrix, corrected for attenuation, and reconstructed using two-dimensional ordered subset expectation maximization iterative technique.
Thyroid agenesis/hemi agenesis
Congenital hypothyroidism from thyroid dysgenesis is a common disorder with a birth prevalence of 1 case in 4,000 live births.[2] It occurs when there is either complete (agenesis) [Figure 2a] or partial failure (hemiagenesis) [Figure 2b, 2c] of the development of thyroid gland. Isthmus is rarely absent. Although thyroid hypoplasia has recently been associated with mutations in the thyrotropin receptor, the cause of thyroid agenesis is unknown. Females are more commonly affected than males. It is thought to result from the failure of cells to migrate laterally leading to agenesis of a part of the thyroid.[3] Most cases of thyroid dysgenesis are sporadic. This disruption of the normal process of lobulation may be environmental or genetically driven as exemplified by studies on monozygotic twins and in families with thyroid ectopia.[4,5,6] Patients with Downs syndrome have an increased incidence of thyroid dysgenesis.[7] Several genes have been found to control thyroid descent, development, and morphogenesis. Three thyroid transcription factors, TTF1, TTF2, and Pax-8 are reported to be involved in thyroid developmental defects, but their role in thyroid hemiagenesis is still not clear.
Figure 2.
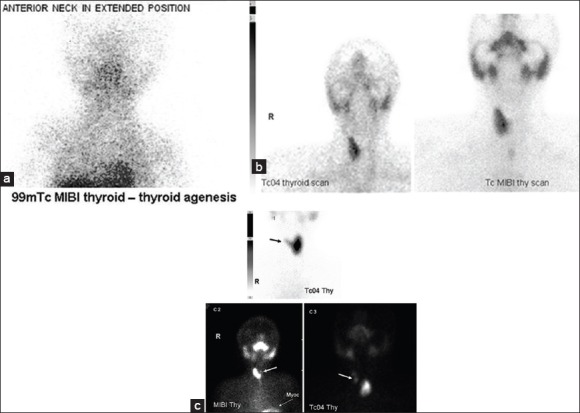
(a) 99mTc MIBI thyroid images showing agenesis (absence of both lobes) of thyroid gland in a hypothyroid child who is on tab thyroxine (b) thyroid hemiagenesis (absence of one of the lobes of thyroid) in a 26-year-old male, confirmed with MIBI thyroid image. (c) rudimentary left lobe with right lobe showing Graves disease (C1 image). (arrow), (c2) sestaMIBI thyroid image in a patient with Downs syndrome on tab thyroxine. Images show intact right lobe and rudimentary left lobe (arrow), (c3) TcO4 thyroid scan showing rudimentary right upper lobe (arrow) in presence of a normal sized left lobe thyroid (toxic nodule) in a 52-year-old lady
Developmental variations in thyroid lobes
A number of variations in the shape and size of the thyroid gland have been described. The mean length of the lateral lobes is described as 5 cm [Figure 3]. The left lobe is smaller than the right lobe. Harjeet et al.[8] described it as 4.04 cm for the right lobe and 3.82 cm for the left lobe.
Figure 3.
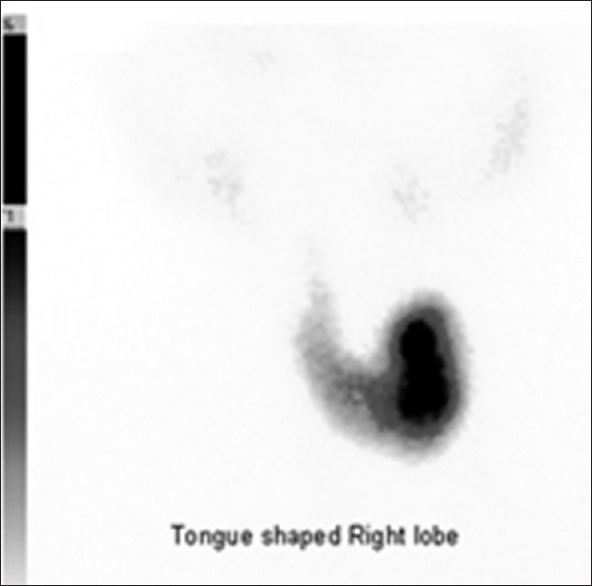
TcO4 thyroid scan performed on a 23-year-old female. Images show a tongue shaped developmental anomaly of right lobe of thyroid gland with contralateral Graves disease (left lobe)
Pyramidal lobe
It is an additional lobe of thyroid gland, in fact remnant of the thyroglossal duct which appears like a long pyramid or a conical shaped structure. It is also known as the Lalouette's pyramid[9] attached by its base to the superior border of the isthmus, usually at its junction with the left lobe. It rarely occurs in midline. Its apex is attached to the body of the hyoid bone by a fibrous band which sometimes contains muscular fibers, known as the levator glandulae thyroideae. Incidence of a pyramidal lobe in Indian population as per literature search is variable and many of them may largely remain unnoticed. Marshall[10] described the presence of pyramidal lobe in 43% of cases while Harjeet et al.[8] observed it in 28.9% of cadaveric specimens. It is usually attached either to the upper part of isthmus or one of the lateral lobes. It is reported that the maximum number of pyramidal lobes was attached to the left lobe (47.05%), as compared to the right lobe or the isthmus that is, 32.55% and 20.58% of cases respectively.[8,10] The pyramidal process develops out of the lower part of the thyroglossal duct by differentiation of the duct tissue into glandular tissue. The length of the pyramidal process depends on the position at which fragmentation of the thyroglossal duct first occurs.[11] Very rarely two pyramidal lobes may be attached by a single levator glandulae thyroideae muscle fibers [Figure 4]. Surgical importance of this lobe lies in the fact that as it is rarely present it may be left unresected during thyroidectomy which may lead to recurrence of hyperthyroidism or cancers.
Figure 4.
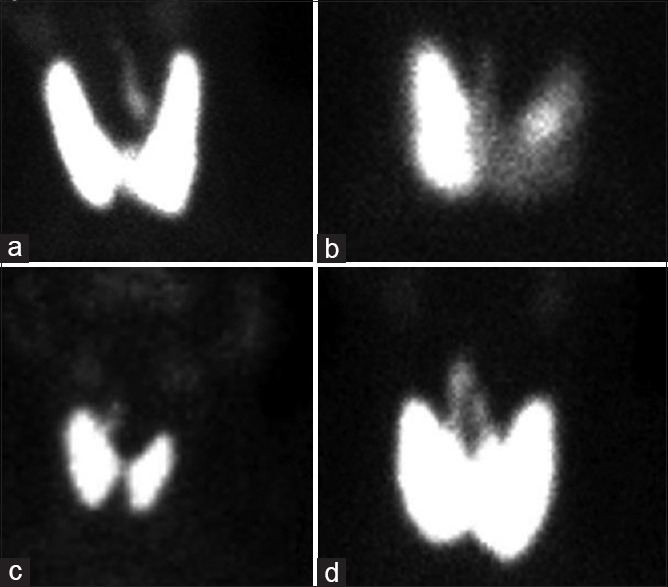
Variations in pyramidal lobe: (a) Arising from left lobe, (b) from isthmus, (c) from right lobe, (d) two pyramidal lobes joined by levator glandulae thyroideae (“inverted V”)
Along thyroglossal tract
The thyroid diverticulum grows in allometric proliferation becoming a solid cellular cord called the thyroglossal duct; its caudal end bifurcates and gives origin to the thyroid lobe and the isthmus. The presence of the thyroglossal tract is usually noticed as a cystic neck swelling i.e., congenital thyroglossal tract cysts accounting for approximately 70% of congenital neck abnormalities.[8,9] They are cysts of epithelial remnants of the thyroglossal tract and present characteristically as a midline neck mass at the level of the thyrohyoid membrane, closely associated with the hyoid bone [Figure 5e]. The tract usually atrophies and disappears by the 10th week of gestation. It may at times be paramedian in location. Portions of the tract and remnants of thyroid tissue associated with it may persist at any point between the tongue and the thyroid. Ectopic thyroid tissue may also be seen in the walls of thyroglossal cysts.
Figure 5.
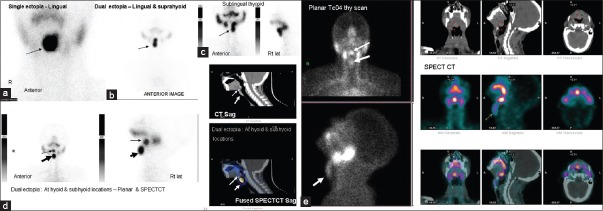
99mTcO4 thyroid images showing different sites of ectopic thyroid tissue, (a) single ectopia at lingual location, (b) dual ectopia-at lingual and suprahyoid location with thyroid tissue along thyroglossal tract, (c) sublingual thyroid, (d) dual ectopia at hyoid and subhyoid location (planar and single photon emission computed tomography [SPECTCT] images) (e) planar TcO4 thyroid scan and SPECTCT images showing lingual thyroid (thin arrow) and thyroid tissue along thyroglossal tract (bold arrow) in the same patient, confirmed with SPECTCT images.
Ectopic locations of thyroid gland
With respect to this embryologic course ectopic thyroid tissue/gland can be categorized into any of the four typical locations: (i) The base of the tongue, (ii) adjacent to the hyoid bone, (iii) the midline infrahyoid portion of the neck, and rarely, (iv) the lateral part of the neck.[10,11,12] By far the most common location in 90% cases is at foramen caecum resulting in lingual thyroid.[10] This may present as an asymptomatic swelling at base of tongue or may manifest either as dysphagia, dysphonia or dyspnea. The differential diagnosis includes metastatic thyroid carcinoma, branchial cleft cyst, lymphatic malformation, abscess, saccular cyst, epidermoid cyst, and squamous cell carcinoma. The relationship of a mass to landmarks such as the foramen cecum, hyoid bone, strap muscles, thyrohyoid membrane, and thyroid cartilage can help to differentiate a thyroglossal duct cyst and ectopic thyroid tissue from other anterior neck masses when the embryologic thyroid course is considered. Managing ectopic thyroid tissue depends on the size of the lesion, symptoms, age, thyroid functioning status and complications like bleeding from the lesion, ulceration and malignancy.
Images [Figure 5] show absence of native thyroid gland with single ectopia-lingual thyroid marked with thin arrow (a), dual ectopia at lingual and suprahyoid locations (b), at sublingual location (c), another dual ectopia at hyoid (thin arrow) and subhyoid locations, bold arrow (d), lastly at lingual and along thyroglossal tract (e).
Thyrothymic thyroid rests
These are bits or deposits of ectopic thyroid tissue, which lie below the thyroid gland level and arise in the thyrothymic tract. They can occur unilaterally [Figure 6a] or may be bilateral in occurrence and are of variable size, although most of them may be very small. At times they can be very large leading to obstructive symptoms like dyspnea or dysphagia. These may occur either as entirely separate nodules [Figure 6b] or as prolongations [Figure 6c and 6d] from the thyroid lobe, and might be of clinical importance during thyroid or parathyroid surgery.[13] They tend to be attached by thin sheets of thyroid or fibrous tissue to the main body of thyroid gland, but 20% have no attachment at all and can migrate to mediastinum and present as intrathoracic mass.
Figure 6.
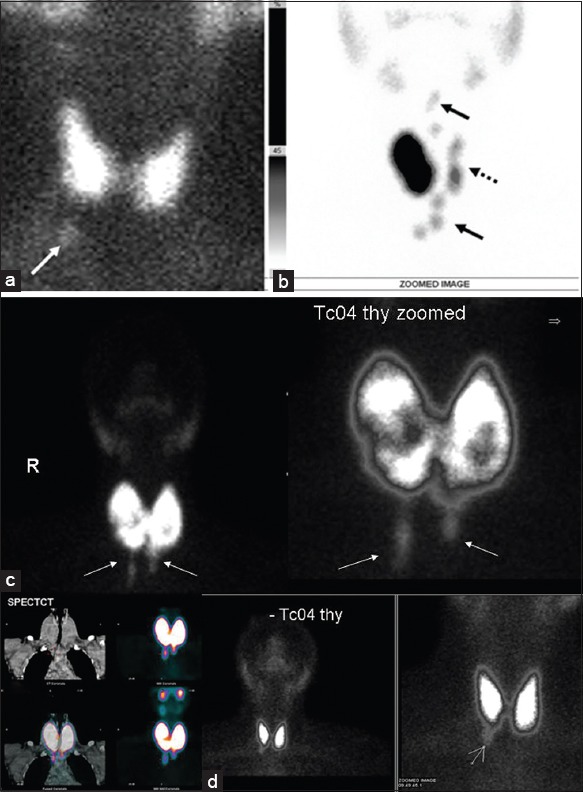
(a) Images of thyrothymic thyroid rests: Shows bits or deposits of ectopic thyroid tissue, which lie below the thyroid gland level and arise in the thyrothymic tract. They may be variable in size; unilateral (a) or may be bilateral, although most of them may be very small. These may occur either as entirely separate nodules (b) these ectopic thyroid tissue may occur as bilateral or unilateral prolongations (c and d) arising from either one or both thyroid lobes (arrow) and might be of clinical importance during thyroid or parathyroid surgery. They tend to be attached by thin sheets of thyroid or fibrous tissue to the main body of thyroid gland, but 20% have no attachment at all and can migrate to mediastinum and present as intra thoracic mass
CONCLUSION
The actual incidence of these variations in the development of the thyroid gland is unknown. Mere clinical examination in euthyroid subjects is, of course, unreliable to identify these anomalies. Thyroid hemiagenesis and the presence of the pyramidal lobe are usually incidentally discovered in patients with other thyroid disorders when thyroid ultrasound or scintigraphy is performed. Neck ultrasound and thyroid scintigraphy are the only methods that can objectively localize these anomalies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Moore KL, Persaud TV, Torchia MG. The developing human: Clinically oriented embryology. 9th ed. Philadelphia, PA: Elsevier/Saunders; 2013. pp. 16–23. [Google Scholar]
- 2.Deladoëy J, Bélanger N, Van Vliet G. Random variability in congenital hypothyroidism from thyroid dysgenesis over 16 years in Québec. J Clin Endocrinol Metab. 2007;92:3158–61. doi: 10.1210/jc.2007-0527. [DOI] [PubMed] [Google Scholar]
- 3.Greening WP, Sarker SK, Osborne MP. Hemiagenesis of the thyroid gland. Br J Surg. 1980;67:446–8. doi: 10.1002/bjs.1800670621. [DOI] [PubMed] [Google Scholar]
- 4.McLean R, Howard N, Murray IP. Thyroid dysgenesis in monozygotic twins: Variants identified by scintigraphy. Eur J Nucl Med. 1985;10:346–8. doi: 10.1007/BF00251309. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg T, Gilboa Y. Familial thyroid ectopy and hemiagenesis. Arch Dis Child. 1980;55:639–41. doi: 10.1136/adc.55.8.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Léger J, Marinovic D, Garel C, Bonaïti-Pellié C, Polak M, Czernichow P. Thyroid developmental anomalies in first degree relatives of children with congenital hypothyroidism. J Clin Endocrinol Metab. 2002;87:575–80. doi: 10.1210/jcem.87.2.8268. [DOI] [PubMed] [Google Scholar]
- 7.Fort P, Lifshitz F, Bellisario R, Davis J, Lanes R, Pugliese M, et al. Abnormalities of thyroid function in infants with Down syndrome. J Pediatr. 1984;104:545–9. doi: 10.1016/s0022-3476(84)80544-2. [DOI] [PubMed] [Google Scholar]
- 8.Harjeet A, Sahni D, Jit I, Aggarwal AK. Shape, measurements and weight of the thyroid gland in northwest Indians. Surg Radiol Anat. 2004;26:91–5. doi: 10.1007/s00276-003-0194-y. [DOI] [PubMed] [Google Scholar]
- 9.Sauk JJ., Jr Ectopic lingual thyroid. J Pathol. 1970;102:239–43. doi: 10.1002/path.1711020408. [DOI] [PubMed] [Google Scholar]
- 10.Marshall CF. Variations in the form of the thyroid gland in man. J Anat Physiol. 1895;29(Pt 2):234–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Braun EM, Windisch G, Wolf G, Hausleitner L, Anderhuber F. The pyramidal lobe: Clinical anatomy and its importance in thyroid surgery. Surg Radiol Anat. 2007;29:21–7. doi: 10.1007/s00276-006-0165-1. [DOI] [PubMed] [Google Scholar]
- 12.Zander DA, Smoker WR. Imaging of ectopic thyroid tissue and thyroglossal duct cysts. Radiographics. 2014;34:37–50. doi: 10.1148/rg.341135055. [DOI] [PubMed] [Google Scholar]
- 13.Sackett WR, Reeve TS, Barraclough B, Delbridge L. Thyrothymic thyroid rests: Incidence and relationship to the thyroid gland. J Am Coll Surg. 2002;195:635–40. doi: 10.1016/s1072-7515(02)01319-4. [DOI] [PubMed] [Google Scholar]


