Abstract
Due to the possibility to examine at the patient bedside or incubator, ultrasound imaging of the central nervous system, particularly through the anterior fontanelle, is the most common diagnostic examination performed in neonates and infants with neurological problems. Despite its common application, this method has certain limitations. These limitations are associated with cross-sections of the cerebral structures that can be obtained when examining through the anterior fontanelle. The aim of the paper was to assess the usefulness of three dimensional sonography of the central nervous system in neonates and infants in the assessment of intracranial bleeding and its consequences when examined through the anterior fontanelle. The study enrolled 283 patients treated at the Pediatric Teaching Hospital at the Medical University of Lublin in whom a transfontanelle cerebral examination was indicated. The two- and three-dimensional ultrasound examinations of the central nervous system were conducted in 283 patients aged from 1 day to 18 months (mean age: 2 months). 254 three-dimensional examinations were of diagnostic value. The number of detected pathological lesions was higher in a statistically significant way (p = 0.007) in the three-dimensional ultrasound examination. In the authors’ own studies, the highest sensitivity and statistically significant superiority of the three-dimensional method over the two-dimensional one referred to detecting intraventricular or intracerebral hemorrhages. Novel techniques of ultrasound imaging, including the three-dimensional one, have undoubtedly increased the diagnostic possibilities of sonography and, at the same time, retained all its advantages.
Keywords: central nervous system ultrasound, anterior fontanelle, three-dimensional ultrasound, intraventricular hemorrhage, infants
Abstract
Ultrasonografia centralnego układu nerwowego, a szczególnie obrazowanie przez ciemiączko przednie, ze względu na możliwość wykonania badania przy łóżku pacjenta lub też w inkubatorze jest najczęściej stosowaną metodą diagnostyczną u noworodków i niemowląt z problemami neurologicznymi. Jednak pomimo powszechnego zastosowania metoda ta ma pewne ograniczenia. Są nimi płaszczyzny przekroju struktur mózgowia możliwe do uzyskania w obrazowaniu przez ciemiączko przednie. Celem pracy jest ocena przydatności ultrasonografii trójwymiarowej centralnego układu nerwowego u noworodków i niemowląt w ocenie krwawienia wewnątrzczaszkowego i jego następstw w badaniu przez ciemiączko przednie. Badaniami objęto 283 pacjentów leczonych w Dziecięcym Szpitalu Klinicznym Uniwersytetu Medycznego w Lublinie, u których istniały wskazania do badania przezciemiączkowego mózgu. Badanie ultrasonograficzne centralnego układu nerwowego w opcji dwu- i trójwymiarowej przeprowadzono u 283 pacjentów w wieku od 1 dnia do 18 miesięcy (średnio 2 miesiące). W badaniu ultrasonograficznym trójwymiarowym otrzymano 254 wyniki badań mające wartość diagnostyczną. Liczba zmian patologicznych wykrywanych w badaniu ultrasonograficznym była znamiennie statystycznie większa (p = 0,007) w badaniu ultrasonograficznym trójwymiarowym. W badaniach własnych największa czułość i istotna statystycznie przewaga metody trójwymiarowej nad dwuwymiarową dotyczyła krwawień do układu komorowego i krwawień wewnątrzmózgowych. Nowe techniki badania ultrasonograficznego, a wśród nich trójwymiarowego, niewątpliwie zwiększyły możliwości diagnostyczne ultrasonografii, zachowując przy tym wszystkie jej zalety.
Introduction
Ultrasound imaging (US) of the central nervous system (CNS), particularly through the anterior fontanelle, is the most common diagnostic examination performed in neonates and infants with significant perinatal history, prematurity, low birth weight, symptoms of infections, neurological disorders or disorders in the coagulation system(1).
Sonography is a non-invasive method of imaging enabling diagnosis at the patient's bedside or incubator. Thus, it does not necessitate transportation to a different ward or to a different hospital, as it may happen in the case of computed tomography (CT) or, a less available, magnetic resonance imaging (MRI). The US examination is also several times cheaper than the methods mentioned above(2). Due to its numerous advantages, sonography became the most frequently selected method for the assessment of the CNS in obstetric and neonatal departments.
The most common pathologies in the CNS diagnosed by means of US examinations are: intracerebral or intraventricular hemorrhages, ventricular extension, periventricular leukomalacia, vascular malformations and other developmental anomalies of the CNS, more rarely – brain tumors(2, 3). However, despite its common application, this method has certain limitations. They are connected with cross-sections of the cerebral structures that can be obtained when examining through the anterior fontanelle(4). Obtaining optimal slices for establishing a correct diagnosis (such as oblique and axial views) is sometimes hindered or even impossible.
Three-dimensional (3D) imaging allows for jumping over the shadows of conventional two-dimensional (2D) sonography – the examined structure is presented in three perpendicular planes.
A 3D ultrasound examination is less time-consuming than the conventional one. A single acquisition is automatic and does not last longer than several seconds. This is of particular relevance in the diagnosis of patients in a severe condition and patients in incubators who are susceptible to hypothermia.
The three-dimensional data acquired during the examination may be subsequently edited and processed so as to obtain the best visualization of the required structures or pathological lesions. It takes place in the monitor of the ultrasound equipment or at an additional diagnostic workstation, without the presence of the patient. It is also possible to conduct volume measurements based on genuine volumetric data(5–9).
The processing of three-dimensional data (postprocessing) is the most time-consuming part of a three-dimensional ultrasound examination.
Nevertheless, modern 3D sonography is not flawless – it is strictly dependent on the quality of the initial two-dimensional image, which means that the conditions of the examination, and bad quality of the 2D image, cannot be corrected. Some artefacts (resolution, enhancement, propagation or motion) which appear in the 2D image are transmitted into the 3D image. Furthermore, a loss of resolution must be taken into account in reconstructed images. Nonetheless, together with the appearance of more modern ultrasound systems, even this flaw is gradually being eliminated(3, 6).
Aim of the paper
The aim of this study was to determine the usefulness of 3D sonography of the CNS in neonates and infants in the assessment of intracranial bleeding and its aftereffects when examined through the anterior fontanelle.
It was attempted to answer the following questions:
What is the value of 3D sonography of the CNS compared to 2D US in intracranial hemorrhage assessment?
What information associated with hemorrhage and its aftereffects may be provided by 3D US examination when compared to brain CT?
Material and methods
The study enrolled 283 patients treated at the Pediatric Teaching Hospital at the Medical University of Lublin in whom a transfontanelle cerebral examination was indicated. The study was performed between 8 January 2007 and 29 October 2007 on patients aged from 1 day to 18 months (mean age: 2 months).
The examinations were performed by means of Philips iU22 system with a C8-5 transducer and subsequently, a 3D assessment was performed with the use of 3D9-3V endovaginal probe.
During both examinations of the CNS structures, the following were assessed:
size and shape of the ventricular system;
choroid plexuses of the lateral ventricles;
echogenicity of the cerebral structures;
presence of focal lesions and hemorrhages including their size and localization;
pericerebral fluid spaces;
in patients with a valve – the ventriculoperitoneal shunt placement.
The acquired 3D images and data were stored in the memory of the ultrasound system and subsequently, they were placed on the DICOM archive server at a remote station. It was not only used for storing and playback of the images, but also for postprocessing and analysis of the three-dimensional data.
Twenty-three patients also underwent computed tomography of the brain.
The statistical analysis of the obtained results was conducted with the use of Statistica 6.0 PL software. The outcomes were presented as:
arithmetic means ± standard deviation (SD) for variables with normal distribution;
median, minimal (min.) and maximal (max.) values of the statistical series for variables with non-normal distribution.
The agreement of individual variables in the populations with normal distribution was checked by means of the Shapiro-Wilk test. Because the analyzed variables did not have the normal distribution, non-parametric tests were applied in further analysis.
The results were considered statistically significant at the level of p = 0.05.
Results
2D and 3D ultrasound examinations of the CNS
2D and 3D ultrasound examinations of the CNS were performed on 283 patients; 254 three-dimensional US examinations were of diagnostic value.
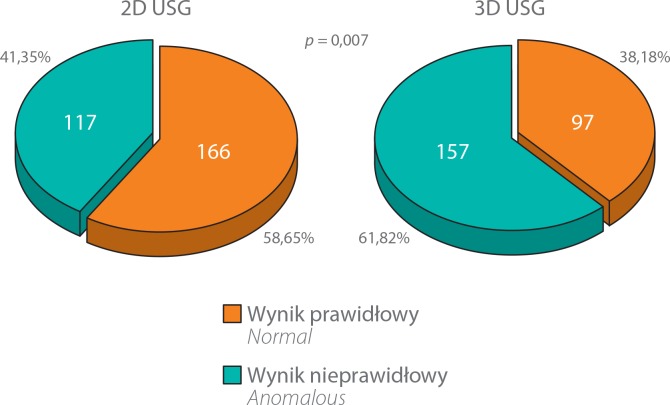
The number of detected pathological lesions was higher in a statistically significant way (p = 0.007) in the 3D ultra-sound examination. These data are presented in fig. 1.
Fig. 1.
Comparison of the sensitivity of 2D and 3D sonography in detecting pathological lesions
In 214 of 254 (84.25%) patients, the agreement between the diagnoses established with both methods was demonstrated. In 40 (15.75%) patients the diagnoses in 3D sonography were considerably different (p = 0.007) than t hose obt ained in a 2D exa mination. In 171 (67. 32%) cases, the results of both examinations were the same.
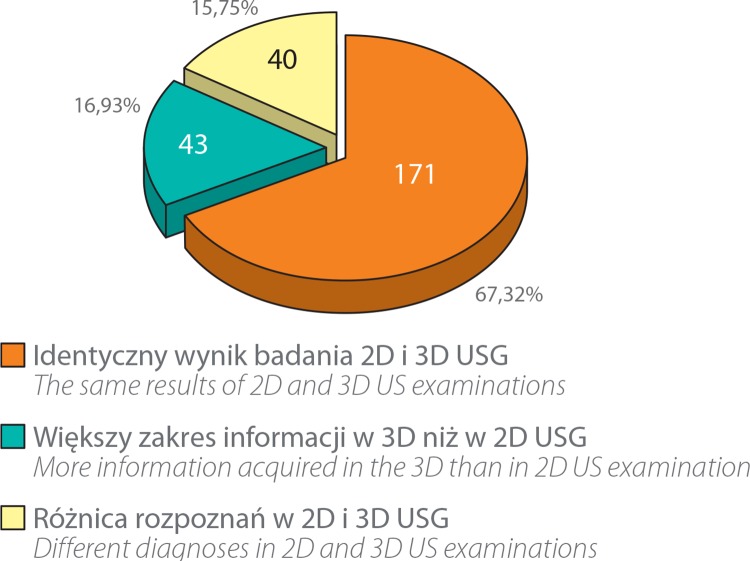
Despite the agreement between the 2D and 3D examinations, in 43 (16.93%) patients, 3D sonography revealed a considerable larger range of information concerning the observed pathology. These data are presented in fig. 2.
Fig. 2.
Assessment of the agreement of diagnoses established on the basis of 2D and 3D US examinations
The number of hemorrhages to the ventricular system and cerebral tissue diagnosed in sonography was higher in a statistically significant way (p = 0.0006) in a 3D examination – 72 from among 254 (28.34%) patients, than in a 2D examination – 50 out of 283 (17.66%) patients.
The statistically significant difference in sensitivity (p = 0.0003) was associated with grade I hemorrhage (IVH I°) which was visualized in 2 out of 283 (0.7%) patients in a 2D examination and in 17 out of 254 (6.69%) patients in a 3D examination.
In 5 out of 19 (26.32%) patients in whom grade II–IV hemorrhage was diagnosed based on the 2D method, the diagnosis concerning the grade or localization of bleeding was changed following a 3D examination (tab. 1).
Tab. 1.
Differences in the localization and classification of hemorrhages (grade II–IV) to the CNS according to 2D and 3D ultrasound examinations in 5 patients
| Diagnoses in 2D US | Diagnoses in 3D US | ||
|---|---|---|---|
| Grade of hemorrhage | Localization of hemorrhage | Grade of hemorrhage | Localization of hemorrhage |
| IVH II° | Intraventricular | IVH I° | Region of the thalamocaudate groove |
| IVH III° | Mural in the right ventricle | IVH IV° | Mural in the right ventricle and intracerebral |
| IVH III° | Mural in the right ventricle | IVH IV° | Mural in the right ventricle and intracerebral |
| IVH III° | Bilateral in the ventricle: mural and in the region of plexuses | IVH III° | In the right ventricle – in the region of the foramen of Monro, and in the third ventricle; in the left ventricle – as in 2D US |
| IVH III° | Mural in the left ventricle | IVH III° | Region of the left foramen of Monro |
In a 2D examination, the assessment of the ventriculoperitoneal valve was satisfactory in 2 out of 7 (28.57%) patients with a shunt but in 5 (71.42%) cases, the shunt was not sufficiently visible.
In a 3D US examination, the localization of the shunt was assessed in 6 patients with hydrocephalus. The localization of the shunt was visible in a satisfactory way in all patients (100%).
In 2 out of 14 patients with signs of pericerebral space extension detected by means of 2D sonography and in 2 out of 12 patients examined with the use of the 3D method, hyperechoic reflections with a broad base directed towards the internal aspect of the cranium were visualized. This suggested the presence of bleeding to the pericerebral spaces. In one case, the lesions were localized in the parieto-occipital region and in the other – in the temporo-occipital region. The diagnoses established based on 2D and 3D examinations were in agreement, but the 3D examination delivered additional information concerning the localization, distribution and size of the hemorrhagic focus.
Comparison of ultrasound findings with the CT of the CNS
The extended diagnosis in the form of a CNS assessment in computed tomography was necessary in 23 out of 283 (8.12%) patients. In 20 out of 23 (86.95%) cases, the outcome was in line with the US findings. In the 3 remaining patients (13.03%) there were discrepancies in the diagnoses. In 2 patients, the hemorrhagic foci, previously visualized in the US examination, were not visible. In one patient, the presence of the hemorrhagic focus in the region of the lateral ventricle was not confirmed. A focus of malacia was detected instead. In one case, CT revealed normal image of the cerebral structures.
Discussion
Sonography is of key importance in assessing the cerebral structures in neonates and infants.
Novel US techniques, including the 3D US, have undoubtedly increased the diagnostic possibilities of sonography and retained all its advantages (such as accessibility, possibility of bedside examination and harmless character of ultrasonic waves). They allow to overcome limitation of the 2D sonography, such as considerable examiner-dependency and associated difficulty in treatment monitoring as well as low reproducibility of results and low accuracy of volumetric measurements(3, 8, 10, 11).
In 32.68% of patients, the results indicated that additional 3D ultrasound imaging is useful. In 15.75% of cases, the diagnosis was changed following a 3D US examination and in the remaining 16.93%, 3D sonography provided additional diagnostic information. Moreover, in a 3D examination, the existing anomalies were detected more frequently when compared to 2D sonography (p = 0.007).
The higher level of sensitivity of the 3D method results from the possibility to return to and re-analyse the volumetric data stored in the memory. Not only does it allow for the re-analysis of the stored data slice by slice, but also enables visual quality improvement and parametric assessment of the examined structure, including volume measurements based on genuine volumetric data. As a result, one may detect pathological lesions which were not detected earlier(4, 6).
An undoubted advantage is fast acquisition of data in 3D imaging in comparison to the time needed to conduct a 2D US examination. On the other hand, more time is needed for processing and analyzing the 3D image.
In the authors’ own studies, the greatest sensitivity and statistically significant superiority of the 3D method over the 2D one referred to intraventricular or intracerebral hemorrhages. In the authors’ own studies, 2D sonography visualized bleeding to the CNS in 17.66% of infants; in the 3D examination, the sensitivity was significantly higher – 28.34% of hemorrhages were detected (p = 0.0006).
In the authors’ own material, it was observed that a 3D US examination was more effective in visualizing subtle changes, such as subependymal hemorrhage (IVH I°) (6.69% compared to 0.7% of cases detected in a 2D examination – p = 0.0003) or subependymal cysts (14.57% compared to 10.24% of cases detected in a 2D examination – p = 0.026).
The outcomes of this study are in line with the results of other studies whose authors report the superiority of 3D imaging in differentiating hemorrhages to the germinal matrix (IVH I°) with choroid plexuses. Since they are both hyperechoic in the ultrasound image and have similar localizations, their differentiation may be facilitated by an additional axial projection or oblique views(4, 6).
A low number of data concerning the application of 3D sonography in brain imaging reveal that it shows not only bleeding, but also allows for an accurate assessment of localization, grade of hemorrhage, amount of extravasated blood and further development of hemorrhagic lesions(4).
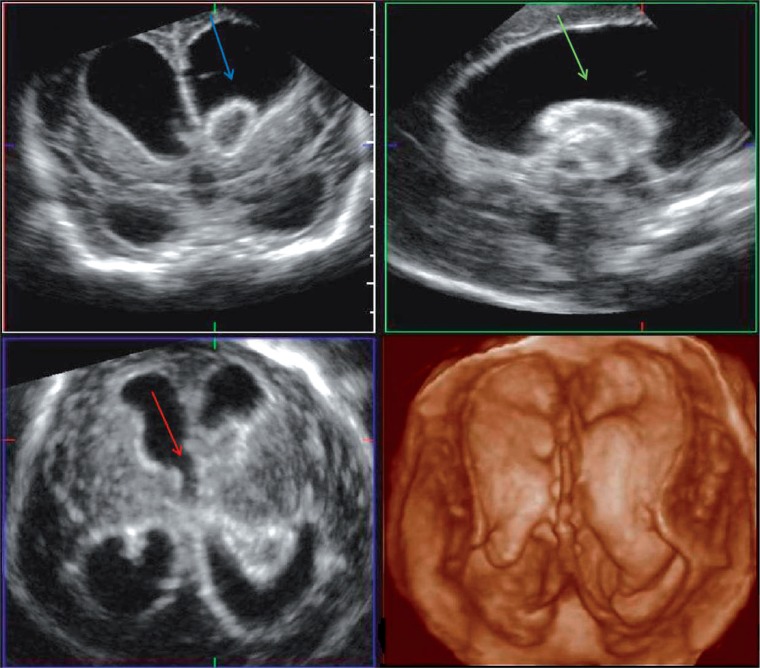
In 3D US examination, it is possible to thoroughly evaluate the distribution of thrombi within the ventricular system and their relation to the ways of cerebrospinal fluid's circulation – the foramina of Monro, or, which is slightly more difficult, the cerebral aqueduct. In the authors’ own material, the usefulness of 3D diagnosis was judged as significantly superior (p = 0.013) to the 2D sonography in determining the localization of hemorrhagic lesions. As a result, in 5 out of 19 (26.32%) patients in whom grade II–IV hemorrhage was diagnosed based on a 2D examination, the diagnosis concerning the grade or localization of bleeding was changed following a 3D examination. In further 2 out of 5 patents, 2D examinations revealed hydrocephalus and IVH III° and insignificant localization of thrombi in the ventricular system. Following evaluation of the blood clots distribution in the ventricular system, their unfavorable localization with respect to the ways of cerebrospinal fluid's circulation was demonstrated. In one of the patients a blood clot involved the left foramen of Monro and in the other, it blocked the right foramen and entered into the third ventricle. In both cases, the diagnosis was facilitated by the axial plane, in which the connection of the lateral ventricles with the third ventricle by the paired foramina of Monro is best visualized (fig. 3).
Fig. 3.
3D US: post-hemorrhagic hydrocephalus. A thrombus blocks the right foramen of Monro (blue arrow) and enters into the third ventricle (green arrow). The left foramen of Monro (red arrow)
In both patients with IVH III° in the US examination, a cerebral CT scan was performed. It visualized the features of active periventricular transudation resulted from increased pressure in the ventricular system. However, a CT examination did not confirm the presence of intraventricular hemorrhage in either case even though in one patient, CT was performed after 4 days and in the second case – after 12 days of the ultrasound-based diagnosis. Therefore, it is difficult to concur with the opinion of the authors who claim that cerebral CT is the best tool for visualizing intraventricular or intracerebral bleeding (at least not in every situation). It cannot be denied, however, that CT is superior to any US examination in revealing the signs of increased intracranial pressure, periventricular transudation or herniation risk(2, 12).
When assessing the sensitivity of the imaging method, including US and CT, in detecting pathological lesions, one should take into consideration the quality of the equipment, size of the lesion, experience of the examiner and, in the case of CT, also the protocol according to which the examination is performed.
In both cases, thrombi with the size of 7 and 15 mm were not visible in CT. This might have been caused by too low density of these post-hemorrhagic lesions or by the examination protocol – the failure to visualize smaller lesions may be associated with table movement by 5 mm. In the case of hemorrhage to the third ventricle, the fact that the lesion may disappear within 12 days must also be considered.
Apart from the CT examination conducted in 23 patients, in whom extended diagnosis was indicated, there was no other way to review the diagnoses established by means of 2D and 3D ultrasound examinations. In the presented patients, the results were verified in the 3D ultrasound examination – it allows for collecting data from the studied cerebral region and enables their subsequent analysis.
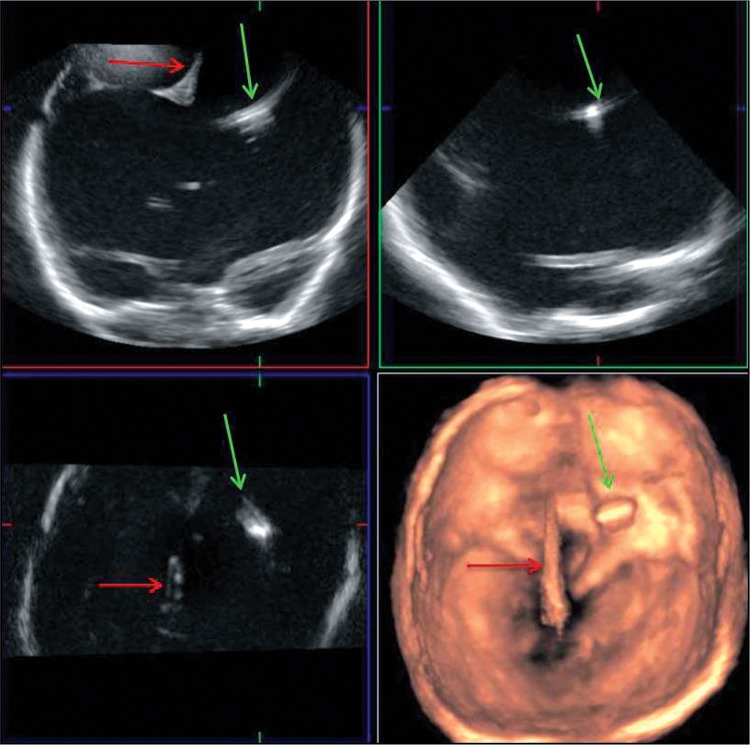
In the 3D US examination, the monitor displays coronal, sagittal and axial planes simultaneously. Moreover, it enables volumetric reconstruction of the examined structure (rendered view), which facilitates the spatial localization of a lesion or a given anatomic structure. In the assessment of the ventriculoperitoneal shunt, it is necessary to determine the localization of its end to ensure that its position has not shifted beyond the ventricular system. In sagittal planes in 2D sonography, the end of the shunt may be parallel to the ultrasound beam, which makes it poorly visible. In the coronal plane, also available in 2D sonography, its cephalocaudal location is difficult to determine since it is frequently visible in a short fragment as a hyperechoic dot or line(13).
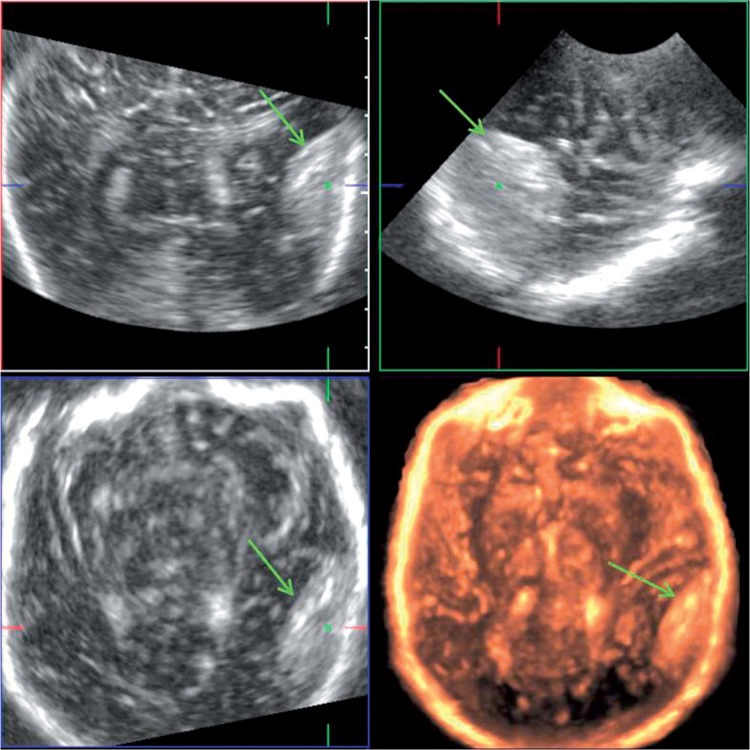
The possibilities to assess shunt placement in 3D sonography is illustrated in fig. 4.
Fig. 4.
3D US: shunt localization (green arrow) in giant hydrocephalus. A fragment of the cerebral falx (red arrow). The lack of the folded structure of the brain caused by the compression of a huge ventricular system; best visible in the rendered view (bottom right image)
In the author's own material, the pericerebral collection was visualized – a hematoma in the right parieto-occipital region, which in the axial plane, available to obtain in the 3D sonography, was in a complete agreement with the CT image. The CT scan confirmed the presence of an epidural fluid collection with blood attenuation (fig. 5).
Fig. 5.
3D US: lentiform shape of the epidural hematoma in the right temporoparietal region (green arrow)
An important advantage of three-dimensional sonography is also the possibility to send the three-dimensional data stored in the memory to other specialists for consultation. Moreover, it is possible to use them for education of future physicians and students.
Conclusions
By comparison with 2D US, 3D sonography shows higher sensitivity in detecting anomalies within the CNS structures in neonates and infants.
3D sonography provided additional diagnostic information (by comparison with 2D sonography) in 43 (16.93%) patients. In further 40 (15.75%) cases, it led to changing the diagnosis.
Although 3D US examination significantly more frequently visualized all hemorrhages to the ventricular system and cerebral tissue, the greatest diagnostic sensitivity of the 3D method refers to detecting subtle changes, such as IVH I° or subependymal cysts.
By comparison with 2D sonography, the 3D method allowed for a significantly more accurate assessment of the extensiveness of hemorrhagic lesions within the cerebral structures.
3D sonography enabled unambiguous assessment of the shunt position in the ventricle in all patients with ventriculoperitoneal shunt.
Conflict of interest
The authors do not report any financial or personal links with other persons or organizations that might negatively affect the content of this publication and claim authorship rights to this publication.
References
- 1.O'Hara SM. Extended field of view imaging: the big picture of pediatric patients. J Ultrasound Med. 2002;21:S38. [Google Scholar]
- 2.Barnes PD. Neuroimaging and the timing of fetal and neonatal brain injury. J Perinatol. 2001;21:44–60. doi: 10.1038/sj.jp.7200483. [DOI] [PubMed] [Google Scholar]
- 3.Riccabona M, Fritz G, Ring E. Potential applications of three-dimensional ultrasound in the pediatric urinary tract: pictorial demonstration based on preliminary results. Eur Radiol. 2003;13:2680–2687. doi: 10.1007/s00330-003-2075-5. [DOI] [PubMed] [Google Scholar]
- 4.Salerno CC, Pretorius DH, Hilton SW, O'Boyle MK, Hull AD, James GM, et al. Three-dimensional ultrasonographic imaging of the neonatal brain in high-risk neonates: preliminary study. J Ultrasound Med. 2000;19:549–555. doi: 10.7863/jum.2000.19.8.549. [DOI] [PubMed] [Google Scholar]
- 5.Fenster A, Downey DB. Three-dimensional ultrasound imaging. Annu Rev Biomed Eng. 2000;2:457–475. doi: 10.1146/annurev.bioeng.2.1.457. [DOI] [PubMed] [Google Scholar]
- 6.Riccabona M. Pediatric three-dimensional ultrasound: basics and potential clinical value. Clin Imaging. 2005;29:1–5. doi: 10.1016/j.clinimag.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Riccabona M, Nelson TR, Weitzer C, Resch B, Pretorius DP. Potential of three-dimensional ultrasound in neonatal and paediatric neurosonography. Eur Radiol. 2003;13:2082–2093. doi: 10.1007/s00330-003-1845-4. [DOI] [PubMed] [Google Scholar]
- 8.Gordon I, Riccabona M. Investigating the newborn kidney: update on imaging techniques. Semin Neonatol. 2003;8:269–278. doi: 10.1016/S1084-2756(03)00031-9. [DOI] [PubMed] [Google Scholar]
- 9.Szopiński K. Ultrasonografia 3D i 4D. Ultrasonografia. 2004;4(15):33–34. [Google Scholar]
- 10.Riccabona M. Advanced techniques in paediatric cranial ultrasound. J Ultrasound Med. 2002;21:S90. [Google Scholar]
- 11.Szopiński K, Rakoczy A, Słapa RZ. Podstawowe techniki prezentacji trójwymiarowej stosowane w diagnostyce obrazowej. Pol Merkur Lekarski. 2002;12:5–10. [PubMed] [Google Scholar]
- 12.Neil JJ, Inder TE. Imaging perinatal brain injury in premature infants. Semin Perinatol. 2004;28:433–443. doi: 10.1053/j.semperi.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Ichihashi K. Three-dimensional ultrasonography of hydrocephalus. J Med Ultrasonics. 2005;32:181–185. doi: 10.1007/s10396-005-0056-9. [DOI] [PubMed] [Google Scholar]