Abstract
Modern echocardiographic techniques, i.e. tissue Doppler imaging and speckle tracking echocardiography, allow for an assessment of global and regional right ventricular function. The right ventricular myocardial performance index and tricuspid annulus motion are used in the assessment of global right ventricular function, whereas duration of the cardiac cycle phases and myocardial velocities are used in the assessment of regional function. Strain and strain rate allow for an evaluation of both regional and global myocardial function. Literature reports provide data on the usefulness of these methods in patients with pressure and volume overload as well as with direct myocardial damage involving the right ventricle. In pulmonary hypertension, S’ wave assessment may be used for therapeutic efficacy evaluation. Longitudinal strain reduction indicates an increased risk of vascular events, while an increased value of myocardial performance index is a predictor for a survival in pulmonary hypertension. A decreased S’ wave velocity is associated with limited pulmonary vascular flow in patients with pulmonary embolism. In patients after atrial baffle repair for transposition of the great arteries, decreased longitudinal strain was an independent predictor for heart failure. A statistically significant decrease in both the S’ wave as well as acceleration during isovolumic contraction were observed in arrhythmogenic right ventricular cardiomyopathy. S’ wave and global right ventricular longitudinal strain values were lower in patients in the acute phase of myocardial infarction involving the right ventricle compared to the corresponding parameters in healthy individuals. In the case of tetralogy of Fallot correction, the evaluation of S’ wave velocity may prove useful in identifying patients with reduced cardiac systolic reserve; a good correlation was also found between the global right ventricular longitudinal strain and right ventricular ejection fraction in MRI.
Keywords: tissue Doppler imaging, speckle tracking echocardiography, right ventricle
Abstract
Nowoczesne techniki obrazowania echokardiograficznego – tkankowa echokardiografia dopplerowska i metoda śledzenia markerów akustycznych – umożliwiają ocenę globalnej i regionalnej funkcji mięśnia prawej komory serca. Do oceny globalnej funkcji prawej komory serca wykorzystuje się: wskaźnik funkcji prawej komory oraz ruch pierścienia zastawki trójdzielnej, a do oceny funkcji regionalnej: pomiary czasów trwania faz cyklu pracy serca i prędkości miokardialnych. Określenie odkształcenia i szybkości odkształcenia umożliwia ocenę zarówno czynności regionalnej, jak i globalnej miokardium. W piśmiennictwie istnieją doniesienia o przydatności tych metod u pacjentów z przeciążeniem ciśnieniowym i objętościowym, jak i bezpośrednim uszkodzeniem miokardium prawej komory serca. W nadciśnieniu płucnym ocena fali S’ może służyć monitorowaniu skuteczności terapii. Obniżenie odkształcenia podłużnego wskazuje na zwiększone ryzyko zdarzeń naczyniowych, natomiast wzrost wartości wskaźnika funkcji prawej komory jest czynnikiem predykcyjnym przeżywalności w nadciśnieniu płucnym. U pacjentów z zatorowością płucną spadek prędkości fali S’ ma związek z ograniczeniem przepływu przez łożysko płucne. W przypadku osób po chirurgicznej korekcji czynnościowej przełożenia wielkich pni tętniczych obniżenie odkształcenia podłużnego było niezależnym czynnikiem rokowniczym wystąpienia niewydolności serca. W arytmogennej kardiomiopatii prawej komory stwierdzano statystycznie istotne zmniejszenie wartości fali S’ i przyspieszenia w fazie izowolumetrycznego skurczu. W okresie ostrym zawału obejmującego prawą komorę wartości fali S’ i globalnej wielkości odkształcenia podłużnego prawej komory były niższe w porównaniu do analogicznych parametrów u osób zdrowych. Po operacji tetralogii Fallota ocena prędkości fali S’ może być przydatna w identyfikacji pacjentów z obniżoną rezerwą skurczową; stwierdzono też dobrą korelację pomiędzy globalną wielkością odkształcenia podłużnego prawej komory serca a jej frakcją wyrzutową ocenianą rezonansem magnetycznym.
In the last 40 years there has been an intensive development of echocardiography, which has become the primary cardiac imaging technique. Recently, novel methods for quantitative assessment of myocardial function have been developed: tissue Doppler imaging (TDI) and speckle tracking echocardiography (STE)(1–4). This has resulted in their application for the assessment of right ventricular function, although the complex anatomy and shape as well as the retrosternal position of the right ventricle significantly reduce the acoustic window and hinder the analysis(1).
Both, tissue Doppler imaging and speckle tracking echocardiography allow for an assessment of global systolic and diastolic function as well as regional myocardial function. These methods are increasingly used in the diagnostics of many heart diseases(5–7).
Tissue Doppler echocardiography uses the technique of:
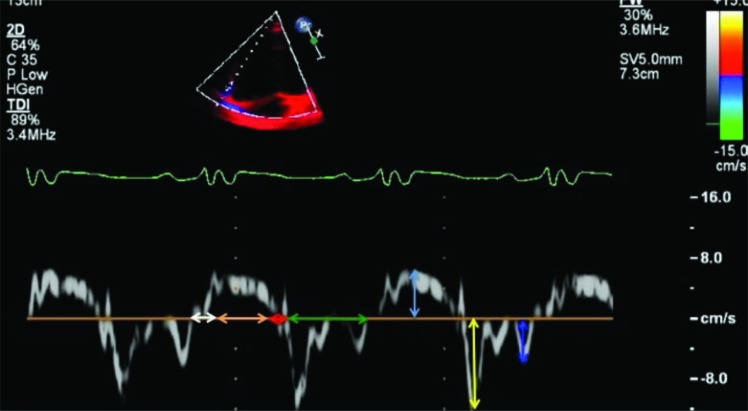
spectral Doppler (fig. 1), which allows for an analysis of real-time myocardial velocity change curves – recordings are performed by inserting a sample of pulsed Doppler measurement volume in the region of interest (ROI)(5);
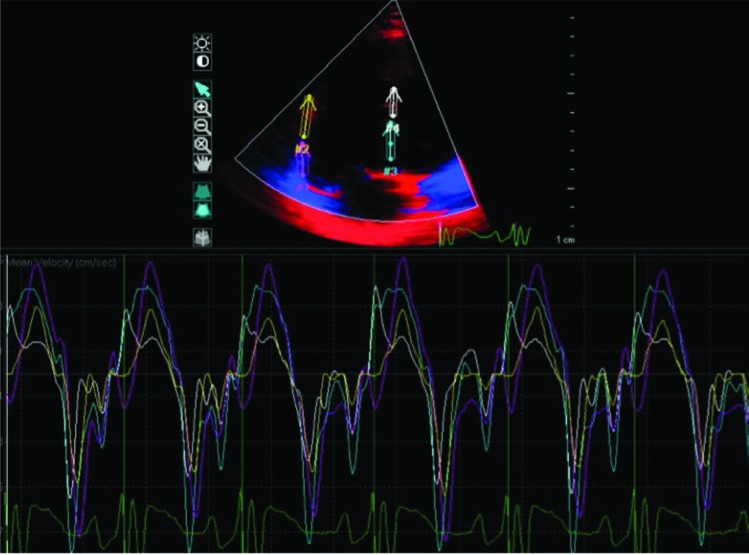
color Doppler (fig. 2), which allows for a measurement of myocardial velocities and strain by analyzing previously recorded images of one- or two-dimensional color-coded myocardial segments – this allows for a simultaneous assessment of several segments using the same view(5).
Fig. 1.
Spectral tissue Doppler. Myocardial velocity curve of the tricuspid annulus and cardiac cycle phases
Legend: blue arrow – myocardial systolic velocity (S’); yellow arrow – early diastolic myocardial velocity (E’); dark blue arrow – late diastolic myocardial velocity (A’); orange arrow – contraction time (CT); green arrow – myocardial diastolic wave time; white arrow – isovolumetric contraction time (ICT); red arrow – isovolumetric relaxation time (IRT)
Fig. 2.
Echocardiography, apical 4-chamber view. Color tissue Doppler. Myocardial velocity curves analyzed simultaneously in four segments
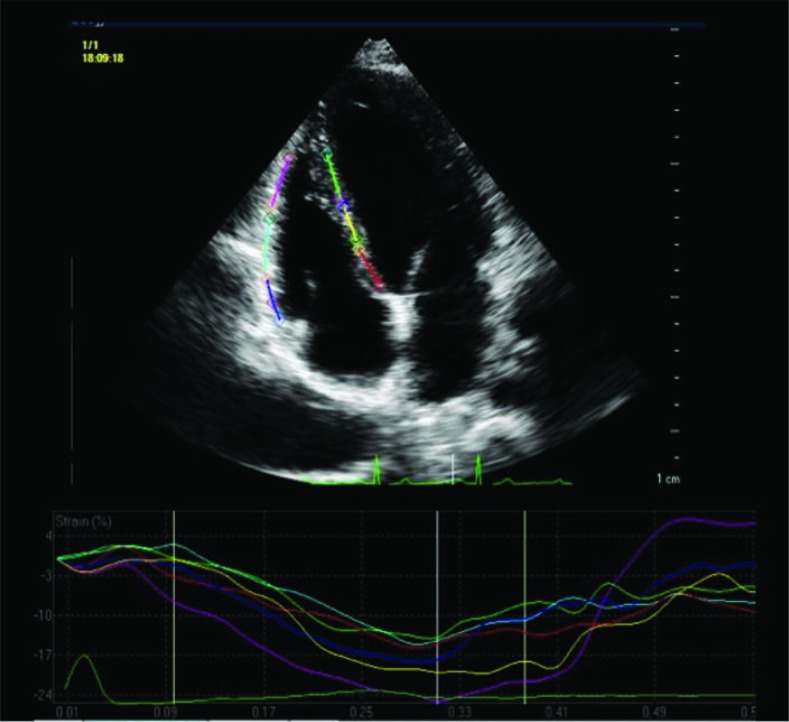
The STE is the innovative method for the assessment of myocardial strain. It uses the presence of numerous spots (speckles) in the myocardium, which reflect ultrasonic waves in a constant manner throughout the cardiac cycle. Tracking the movement of individual acoustic markers within the myocardium as well as changes in their relative position allow for an assessment of strain during the cardiac cycle. STE-based assessment is also performed on the basis of previously recorded images. Accurate determination of the ROI border, i.e. myocardial segments for an analysis in the subsequent stages (fig. 3) is the most laborious part of assessment. Appropriately selected refresh rate, i.e. between 50 and 110 Hz, is of key importance for reliable results. This allows for a precise demarcation of the boundary between the myocardium and the endocardium. Too low or too high frequency results in imprecise tracking of the selected acoustic markers. It ought to be noted that manual correction is necessary following automatic analysis as even slightly crossed myocardial border may alter the obtained results. In the case of suboptimal quality imaging, maximum magnification of individual myocardial wall fragments followed by “segment by segment” parameter analysis is useful. However, this method is laborious and time-consuming, therefore its usefulness in clinical practice is limited. The obtained results are automatically averaged based on three recorded consecutive cardiac cycles and may be expressed globally or separately for individual myocardial segments. Speckle tracking method avoids the primary limitation of tissue Doppler echocardiography, i.e. measurement dependence on the angle of Doppler beam movement relative to myocardial motion(7, 8).
Fig. 3.
Echocardiography, apical 4-chamber view. Speckle tracking. Regions of interest. Below myocardial longitudinal strain curves determined by speckle tracking imaging
Legend: myocardial segments (regions of interest): dark blue line – basal segment of the lateral wall; red line – basal segment of the septum; blue line – middle segment of the lateral wall; yellow line – middle segment of the septum; purple line – apical segment of the lateral wall; green line – apical segment of the septum
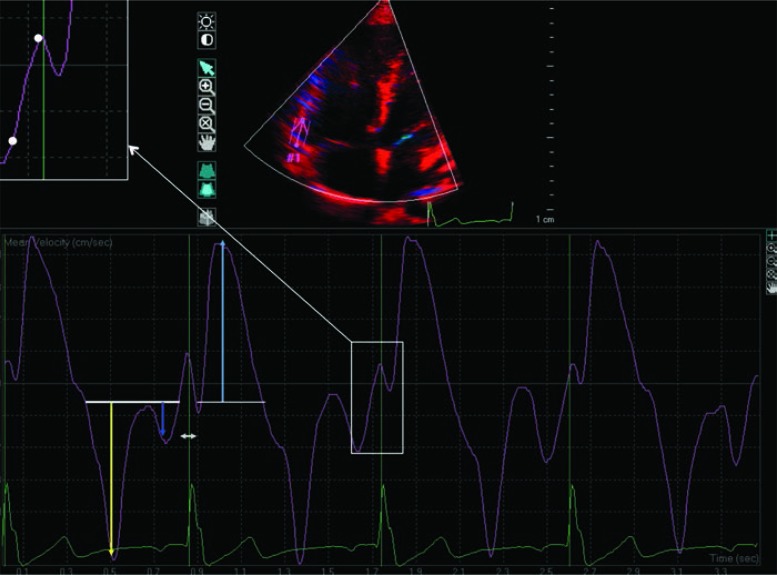
Cardiac cycle phases and myocardial velocities (fig. 4) are made in order to assess the myocardial function using TDI(6).
Fig. 4.
Echocardiography, apical 4-chamber view. Tissue color Doppler. Myocardial velocity and cardiac cycle phase curve – the basal part of the lateral wall
Legend: blue arrow – maximum systolic velocity (S’); yellow arrow – maximum early diastolic velocity (E’); dark blue arrow – maximum late diastolic velocity (A’); grey arrow – isovolumetric contraction time; white dots designate the ascending arm of isovolumetric contraction curve – acceleration during isovolumetric contraction (IVA) is automatically calculated based on its inclination
Systolic:
isovolumic contraction time (ICT);
contraction time (CT);
systolic myocardial velocity (S’).
Diastolic:
isovolumetric relaxation time (IRT);
relaxation time;
early diastolic myocardial velocity (E’);
late diastolic myocardial velocity (A’).
Furthermore, myocardial acceleration during isovolumic contraction (IVA) may be calculated. The IVA is considered to be associated with direct myocardial damage and is independent of alterations in RV shape(9).
Right ventricular myocardial performance index (Tei index, RVMPI) is used for the assessment of global right ventricular function. RVMPI is defined by the formula:
RVMPI – right ventricular myocardial performance index
CT – contraction time
ICT – isovolumic contraction time
IRT – isovolumic relaxation time
Literature data indicate its good correlation with systolic function markers(10, 11).
E’/A’ and E/E’ ratios are measured for an assessment of right ventricular diastolic function. An early diastolic tricuspid inflow assessed using standard echocardiography technique is designated as E. Studies in adults have shown that increased E/E’ ratio is closely associated with right ventricular filling pressure(12), however, this relationship has not been confirmed in pediatric patients after teratology of Fallot repair(13).
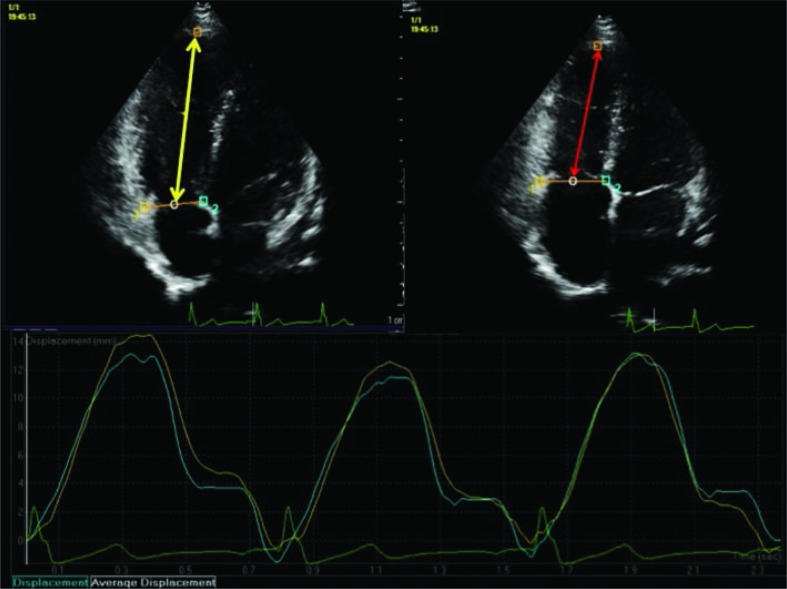
Tricuspid valve annulus (TV) motion analysis using STE is used for the assessment of global systolic right ventricular function. This allows for a quantitative evaluation of ventricular systolic shortening (fig. 2). Although this parameter bears similarity to tricuspid annular plane systolic excursion (TAPSE) registered in the M-mode, it is by contrast independent of the imaging angle. The amplitude of tricuspid valve annulus motion is calculated automatically and presented as integers as well as in the form of right ventricular longitudinal shortening fraction (RVSF), expressed in percentage, according to the following formula:
RVEDL – right ventricular end-diastolic length
RVESL – right ventricular end-systolic length
Previous studies demonstrated a very good correlation between RVSF and RV ejection fraction assessed by magnetic resonance imaging. The value of this parameter was higher than TAPSE, which showed poorer correlation with ejection fraction compared to RVSF. RVSF is likely to be associated with preload, and is less dependent on the direct myocardial damage(14, 15).
TDI and STE are also used for the assessment of the relative systolic myocardial strain (ɛ) and strain rate. Myocardial strain is defined as a deformation of the myocardium relative to its baseline state, i.e. a change in the size of a selected myocardial fragment in a specific direction during one cardiac cycle. It is expressed in percentage relative to the initial size(2, 3, 7).
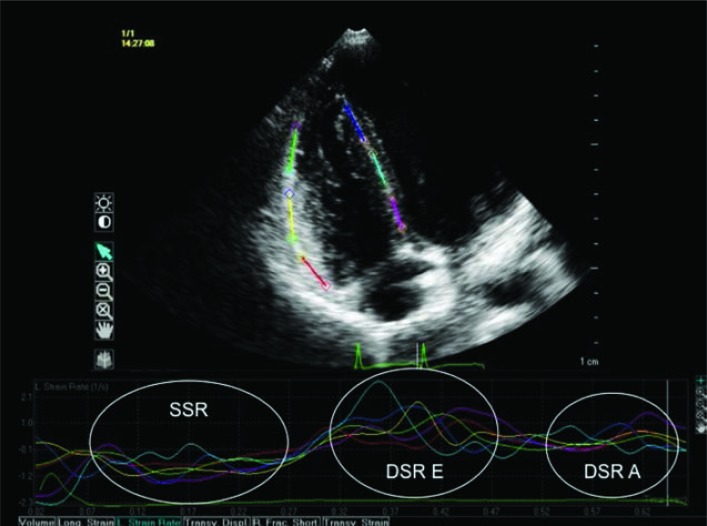
Strain rate assessment involves the following phases:
systolic (SSR);
early diastolic (DSRE);
late diastolic (DSRA) (fig. 5).
Fig. 5.
Echocardiography, apical 4-chamber view. Speckle tracking. Longitudinal strain rate assessment
Legend – SSR – longitudinal strain rate in the systolic phase of the cardiac cycle; DSRE – longitudinal strain rate in early diastolic phase of the cardiac cycle; DSRA – longitudinal strain rate in late diastolic phase of the cardiac cycle
TDI strain measurements use the phenomenon of velocity gradient, which consists in the fact that cardiac muscle contracts at different velocities from the apex to the atrioventricular annuli. The difference in the velocity between two endpoints of a selected region of interest allows to calculate strain rate, and then the strain itself (ɛ)(6).
Grayscale analysis in two-dimensional images is used in the STE with ɛ calculated in the first place, followed by strain rate as its derivative. Negative strain value indicates myocardial shortening or thinning, whereas lengthening or thickening is indicated by a positive value. Strain is assessed in the longitudinal, transverse and circular directions(7, 8).
RV transverse strain assessment is of minor use due to the specific structure of the right ventricular wall, i.e. a very thin circular layer, and also because the contraction of the free wall is phasic primarily in the longitudinal direction. Therefore, only longitudinal strain and strain rate are determined for the RV. The measurement of ɛ allows for an analysis of RV phasic character. Its synchrony may be assessed by measuring time to peak strain in subsequent segments. Post-systolic shortening occurs when maximum values are recorded following vascular valve closure(16).
Myocardial strain analysis is particularly useful in a situation when the global hemodynamic function has not been impaired by the developing heart disease at its initial stage(5).
Recommendations of the American Society of Echocardiography for the assessment of RV structure and function in adults, endorced by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, were published in 2010. According to these recommendations, TDI-based RV assessment may be useful in a variety of clinical situations. The STE method is still used mainly in research(5).
There are literature reports concerning the utility of the described methods for the assessment of RV function in conditions involving:
RV pressure overload – pulmonary hypertension (PH), pulmonary embolism, sleep apnea syndrome(17–21);
RV volume overload – atrial septal defect (ASD), pulmonary valve regurgitation(22, 23);
RV pressure and volume overload – transposition of the great arteries following an atrial baffle repair(24);
direct RV myocardial damage – arrhythmogenic right ventricular cardiomyopathy (ARVC), infarction of the right ventricle(25, 26);
pressure and volume overload as well as direct RV myocardial damage – after tetralogy of Fallot repair (F4)(27–28);
left ventricular load – heart failure(29).
It was found that STE-based decreased ɛ values for the free RV wall in patients with pulmonary hypertension indicate an increased risk of vascular events during a 4-year follow up period(19). Patients receiving treatment due to PH were shown to have increased RV myocardial contractile activity expressed in higher systolic myocardial velocity values compared to pre-treatment measurements. According to the authors, S’ wave assessment may be used for therapeutic efficacy monitoring in PH patients(20). In this group of patients, RVMPI analysis is also of high clinical value. An increase in this ratio is considered to be a predictor of survival in pulmonary hypertension(10, 21).
It was found, based on a study by Kjaergaard et al.(17), that S’ wave assessment may find use in patients with pulmonary embolism. The authors claim that a decrease in S’ wave velocity is associated with limited pulmonary vascular flow, assessed by perfusion scintigraphy.
Abnormal myocardial velocity ratio, i.e. low E’ wave and high A’ wave, was found in patients with sleep apnea syndrome(18).
Fig. 6.
Echocardiography, apical 4-chamber view. Speckle tracking. Right ventricular shortening fraction analysis. Once three points have been manually marked on an image stopped in RV end-diastolic phase (two within the TV at the site of attachment of anterior and septal leaflet, and a third one within the apex of the apical portion of the RV), automatic tracking of TV motion and a change in the RV length during cardiac cycle proceeds
Legend: yellow arrow – right ventricular end-diastolic length; red arrow – right ventricular end-systolic length
S’ wave and ɛ values are higher in ASD patients compared to healthy individuals, which may result from an increased preload. It was further shown that the method of ASD treatment has an effect on these values. They were lower in patients receiving surgical treatment compared to those treated with interventional cardiology(22).
On the other hand, a decrease in free wall and septum ɛ value as well as SR, both in systolic and diastolic phase of the cardiac cycle was found in patients after atrial baffle repair for transposition of the great arteries, with RV as a systemic ventricle. Based on the above mentioned studies, RV systolic dysfunction was an independent predictor for heart failure during a two-year follow-up period(24).
Reduced systolic myocardial velocity and longitudinal strain values were shown in arrhythmogenic right ventricular cardiomyopathy. ARVC patients had statistically significantly smaller S’ wave and IVA velocity differences compared to healthy individuals(25).
Systolic dysfunction: decreased S’ and ɛ values within the lateral RV wall as well as diastolic dysfunction: decreased E’ wave value and an increased A’ wave velocity were observed in patients in the acute phase of RV myocardial infarction(26).
In the case of F4 patients, exercise stress testing showed a reduced increase in S’ wave velocity within the lateral wall at the level of TV during exercise. The authors have found that S’ wave assessment may be useful in identifying patients with reduced systolic reserve(27). Bernard et al.(28) observed a good correlation between global ɛ of the RV free wall and its ejection fraction assessed by magnetic resonance imaging in patients after F4 correction.
When using TDI and STE techniques, it should be noted that these methods require images of excellent quality. In order to perform a reliable assessment of TDI-measured strain the Doppler beam must be parallel or nearly parallel to the direction of myocardial motion (the maximum beam angle relative to strain direction should not exceed 15°). The STE technique does not find application in situations where visualization of the whole ventricle is impossible, which occurs in ventricular dilation or in the case of narrow diagnostic imaging window. The above limitation does not apply to RVSF assessment. Lack of standardization of software used by different manufacturers is an important issue in relation to the discussed techniques(5, 6, 8).
The discussed methods of RV function analysis are a dynamically developing branch of echocardiography, which allow for an accurate location of affected areas. They provide new, valuable data that optimizes and individualizes further diagnostic and therapeutic management. The dynamic development of three-dimensional imaging techniques and their application in STE analysis further expands the possibilities of echocardiogram in the aspect of both, RV's complex structure and its function.
Conflict of interest
The authors do not report any financial or personal links with other persons or organizations, which might affect negatively the content of this publication or claim authorship rights to this publication.
References
- 1.Horton KD, Meece RW, Hill JC. Assessment of the right ventricle by echocardiography: a primer for cardiac sonographers. J Am Soc Echocardiogr. 2009;22:776–792. doi: 10.1016/j.echo.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 2.Isaaz K, Thompson A, Ethevenot G, Cloez JL, Brembilla B, Pernot C. Doppler echocardiographic measurement of low velocity motion of the left ventricular posterior wall. Am J Cardiol. 1989;64:66–75. doi: 10.1016/0002-9149(89)90655-3. [DOI] [PubMed] [Google Scholar]
- 3.Reisner SA, Lysyansky P, Agmon Y, Mutlak D, Lessick J, Friedman Z. Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr. 2004;17:630–633. doi: 10.1016/j.echo.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M, et al. Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr. 2004;17:1021–1029. doi: 10.1016/j.echo.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Ng AC, Thomas L, Leung DY. Tissue Doppler echocardiography. Minerva Cardioangiol. 2010;58:357–378. [PubMed] [Google Scholar]
- 7.Siwińska A, Werner B, Rudziński A, Kawalec W, Moll J, Szydłowski L, et al. Echokardiografia dziecięca w praktyce klinicznej. Rekomendacje 2012 Sekcji Echokardiografii Polskiego Towarzystwa Kardiologicznego. Kardiol Pol. 2012;70:632–640. [PubMed] [Google Scholar]
- 8.Biswas M, Sudhakar S, Nanda NC, Buckberg G, Pradhan M, Roomi AU, et al. Two- and three-dimensional speckle tracking echocardiography: clinical applications and future directions. Echocardiography. 2013;30:88–105. doi: 10.1111/echo.12079. [DOI] [PubMed] [Google Scholar]
- 9.Frigiola A, Redington AN, Cullen S, Vogel M. Pulmonary regurgitation is an important determinant of right ventricular contractile dysfunction in patients with surgically repaired tetralogy of Fallot. Circulation. 2004;110(Suppl 1):153–157. doi: 10.1161/01.CIR.0000138397.60956.c2. [DOI] [PubMed] [Google Scholar]
- 10.Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ, et al. Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr. 1996;9:838–847. doi: 10.1016/s0894-7317(96)90476-9. [DOI] [PubMed] [Google Scholar]
- 11.Abd El Rahman MY, Abdul-Khaliq H, Vogel M, Alexi-Meskischvili V, Gutberlet M, Hetzer R, et al. Value of the new Doppler-derived myocardial performance index for the evaluation of right and left ventricular function following repair of tetralogy of fallot. Pediatr Cardiol. 2002;23:502–507. doi: 10.1007/s00246-002-1469-5. [DOI] [PubMed] [Google Scholar]
- 12.Nageh MF, Kopelen HA, Zoghbi WA, Quiñones MA, Nagueh SF. Estimation of mean right atrial pressure using tissue Doppler imaging. Am J Cardiol. 1999;84:1448–1451. doi: 10.1016/s0002-9149(99)00595-0. [DOI] [PubMed] [Google Scholar]
- 13.Hayabuchi Y, Sakata M, Ohnishi T, Inoue M, Kagami S. Ratio of early diastolic tricuspid inflow to tricuspid lateral annulus velocity reflects pulmonary regurgitation severity but not right ventricular diastolic function in children with repaired Tetralogy of Fallot. Pediatr Cardiol. 2013;34:1112–1117. doi: 10.1007/s00246-012-0612-1. [DOI] [PubMed] [Google Scholar]
- 14.Ahmad H, Mor–Avi V, Lang RM, Nesser HJ, Weinert L, Tsang W, et al. Assessment of right ventricular function using echocardiographic speckle tracking of the tricuspid annular motion: comparison with cardiac magnetic resonance. Echocardiography. 2012;29:19–24. doi: 10.1111/j.1540-8175.2011.01519.x. [DOI] [PubMed] [Google Scholar]
- 15.Buss SJ, Mereles D, Emami M, Korosoglou G, Riffel JH, Bertel D, et al. Rapid assessment of longitudinal systolic left ventricular function using speckle tracking of the mitral annulus. Clin Res Cardiol. 2012;101:273–280. doi: 10.1007/s00392-011-0389-x. [DOI] [PubMed] [Google Scholar]
- 16.Kjærgaard J. Assessment of right ventricular systolic function by tissue Doppler echocardiography. Dan Med J. 2012;59:B4409. [PubMed] [Google Scholar]
- 17.Kjaergard J, Schaadt BK, Lund JO, Hassager C. Quantification of right ventricular function in acute pulmonary embolism: relation to extent of pulmonary perfusion defects. Eur J Echocardiogr. 2008;9:641–645. doi: 10.1093/ejechocard/jen033. [DOI] [PubMed] [Google Scholar]
- 18.Tugcu A, Guzel D, Yildirimturk O, Aytekin S. Evaluation of right ventricular systolic and diastolic function in patients with newly diagnosed obstructive sleep apnea syndrome without hypertension. Cardiology. 2009;113:184–192. doi: 10.1159/000193146. [DOI] [PubMed] [Google Scholar]
- 19.Motoji Y, Tanaka H, Fukuda Y, Ryo K, Emoto N, Kawai H, et al. Efficacy of right ventricular free-wall longitudinal speckle tracking strain for predicting long-term outcome in patients with pulmonary hypertension. Circ J. 2013;25:756–763. doi: 10.1253/circj.cj-12-1083. [DOI] [PubMed] [Google Scholar]
- 20.Ruan Q, Nagueh RF. Clinical application of tissue Doppler imaging in patients with idiopathic pulmonary hypertension. Chest. 2007;131:395–401. doi: 10.1378/chest.06-1556. [DOI] [PubMed] [Google Scholar]
- 21.Sebbag I, Rudski LG, Therrien J, Hirsch A, Langleben D. Effect of chronic infusion of epoprostenol on echocardiographic right ventricular myocardial performance index and its relation to clinical outcome in patients with primary pulmonary hypertension. Am J Cardiol. 2001;88:1060–1063. doi: 10.1016/s0002-9149(01)01995-6. [DOI] [PubMed] [Google Scholar]
- 22.Di Salvo G, Drago M, Pacileo G, Carrozza M, Santoro G, Bigazzi MC, et al. Comparison of strain rate imaging for quantitative evaluation of regional left and right ventricular function after surgical versus percutaneous closure of atrial septal defect. Am J Cardiol. 2005;96:299–302. doi: 10.1016/j.amjcard.2005.02.060. [DOI] [PubMed] [Google Scholar]
- 23.Kjærgaard J, Iversen KK, Vejlstrup NG, Smith J, Bonhoeffer P, Søndergaard L, et al. Effects of chronic severe pulmonary regurgitation and percutaneous valve repair on right ventricular geometry and contractility assessed by tissue Doppler echocardiography. Echocardiography. 2010;27:854–863. doi: 10.1111/j.1540-8175.2010.01153.x. [DOI] [PubMed] [Google Scholar]
- 24.Kalogeropoulos AP, Deka A, Border W, Pernetz MA, Georgiopoulou VV, Kiani J, et al. Right ventricular function with standard and speckle-tracking echocardiography and clinical events in adults with D-transposition of the great arteries post atrial switch. J Am Soc Echocardiogr. 2012;25:304–312. doi: 10.1016/j.echo.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Kjærgaard J, Hastrup Svendsen J, Sogaard P, Chen X, Bay Nielsen H, Køber L, et al. Advanced quantitative echocardiography in arrhythmogenic right ventricular cardiomyopathy. J Am Soc Echocardiogr. 2007;20:27–35. doi: 10.1016/j.echo.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Yilmaz M, Erol MK, Acikel M, Sevimli S, Alp N. Pulsed Doppler tissue imaging can help to identify patients with right ventricular infarction. Heart Vessels. 2003;18:112–116. doi: 10.1007/s00380-003-0703-2. [DOI] [PubMed] [Google Scholar]
- 27.Harada K, Toyono M, Yamamoto F. Assessment of right ventricular function during exercise with quantitative Doppler tissue imaging in children late after repair of tetralogy of Fallot. J Am Soc Echocardiogr. 2004;17:863–869. doi: 10.1016/j.echo.2004.04.037. [DOI] [PubMed] [Google Scholar]
- 28.Bernard Y, Morel M, Descotes-Genon V, Jehl J, Meneveau N, Schiele F. Value of speckle tracking for the assessment of right ventricular function in patients operated on for tetralogy of Fallot. Comparison with magnetic resonance imaging. Echocardiography. 2014;31:474–482. doi: 10.1111/echo.12386. [DOI] [PubMed] [Google Scholar]
- 29.Dokainish H, Sengupta R, Patel R, Lakkis N. Usefulness of right ventricular tissue Doppler imaging to predict outcome in left ventricular heart failure independent of left ventricular diastolic function. Am J Cardiol. 2007;99:961–965. doi: 10.1016/j.amjcard.2006.11.042. [DOI] [PubMed] [Google Scholar]