Abstract
The primary aim of this paper was to assess the relevance of high-frequency ultrasound examination in qualifying patients for either surgical or conservative treatment of posttraumatic peripheral neuropathies. The study was conducted in a group of 47 patients aged 16–65 (mean age 33) who in 2009–2011 were referred to ultrasound examinations due to a clinical suspicion of posttraumatic peripheral neuropathies. The group included 30 females and 17 males. The patients examined presented with neuropathies of the following peripheral nerves: median, ulnar, common peroneal, digital, cutaneous in the deltoid area, mental, PIN and RSNR. In 21 patients, nerve injuries were partial, and in 24 – complete. In 2 cases, the nerve was entrapped between bony fragments. 17 of 21 patients with partial nerve injuries (80.95%) underwent an EMG examination. No functional tests were conducted in the cases of complete injuries when ultrasound imaging had confirmed the result of the clinical examination. All patients underwent the interview, physical examination and ultrasound examination. Ultrasound examinations were performed with Esaote MyLab 50 and MyLab 60 systems using high-frequency broadband linear transducers: 6–18 MHz. The nerves were evaluated in the gray-scale and in the power Doppler mode in longitudinal and transverse sections for localization, morphology and the grade of injury as well as for possible anatomic variants of the nerve trunk and pathologies of the adjacent tissues. Moreover, a dynamic examination was performed, and it was attempted to induce pain or paresthesia by palpation at the site of the visualized pathology. Additionally, the motor and sensory–motor nerves were assessed indirectly based on the images of the skeletal muscles innervated by these nerves. The analyses of the collected material were performed by means of descriptive statistics. The results of clinical and surgical verification were consistent with ultrasound findings in 100% of cases. The results obtained indicate that high-frequency ultrasonography is a valuable method in qualifying patients for various types of treatment of peripheral neuropathies resulting from trauma.
Keywords: ultrasonography, posttraumatic peripheral neuropathies, diagnosis, partial nerve injury, complete nerve injury
Abstract
Podstawowym celem pracy była ocena przydatności badania ultrasonograficznego z zastosowaniem głowic wysokiej częstotliwości w kwalifikowaniu do leczenia operacyjnego albo zachowawczego neuropatii obwodowych o charakterze pourazowym. Materiał pracy stanowiła grupa 47 osób w wieku 16–65 lat (średnia wieku 33 lata) kierowanych w latach 2009–2011 na badanie USG z klinicznym podejrzeniem neuropatii pourazowych. W grupie tej było 30 mężczyzn i 17 kobiet. Zbadano pacjentów ze zmianami pourazowymi nerwów obwodowych: pośrodkowego, łokciowego, promieniowego, strzałkowego wspólnego, nerwów palcowych, skórnych okolicy naramiennej, nerwu bródkowego, PIN, RSNR. U 21 osób uszkodzenia miały charakter częściowy, u 24 całkowity, w 2 przypadkach doszło do usidlenia nerwu pomiędzy odłamami kostnymi. U 17 spośród 21 chorych z rozpoznaniem częściowego uszkodzenia nerwu (80,95%) wykonano badanie EMG. Nie przeprowadzano badań czynnościowych w przypadku uszkodzeń całkowitych, gdy obraz ultrasonograficzny potwierdził wynik badania klinicznego. U wszystkich pacjentów wykonano badanie podmiotowe, przedmiotowe oraz ultrasonograficzne. Do badań ultrasonograficznych wykorzystano aparaty Esaote MyLab 50 i MyLab 60 z zastosowaniem szerokopasmowych głowic liniowych o wysokich częstotliwościach: 6–18 MHz. Nerwy oceniano w skali szarości oraz w opcji dopplera mocy, w przekroju podłużnym i poprzecznym pod kątem lokalizacji, morfologii i stopnia uszkodzenia, ewentualnych wariantów anatomicznych pnia nerwu i patologii przylegających tkanek. Ponadto wykonywano badanie dynamiczne oraz próbę wywołania objawów bólu lub parestezji poprzez palpację miejsca uwidocznionej patologii, a także dokonywano pośredniej oceny nerwów ruchowych i czuciowo-ruchowych na podstawie obrazu unerwianych przez nie mięśni szkieletowych. Analizę zebranego materiału przeprowadzono za pomocą statystyki opisowej. W odniesieniu do weryfikacji klinicznej i operacyjnej zgodność z rozpoznaniem ultrasonograficznym uzyskano w 100% przypadków. Wyniki wskazują, że badanie ultrasonograficzne z zastosowaniem głowic wysokiej częstotliwości jest cenną metodą w kwalifikowaniu do rodzaju leczenia neuropatii obwodowych o charakterze pourazowym.
Introduction
The diagnosis of nerve trauma, particularly at an early posttraumatic stage, is of fundamental importance in planning the treatment and for its late results. Apart from clinical and functional assessment, ultrasonography is the main imaging examination. The aim of a US examination is to determine the level and extent of damage (complete or partial injury), but also, in the case of complete injuries, to assess the localization and condition of the nerve stumps and their distance from each other.
Ultrasonography is a valuable modality in extensive injuries of the extremities (e.g. after traffic accidents or accidents involving agricultural machinery) with resulting massive soft tissue damage, often with its defects that complicate the clinical examination. Fractures resulting from such traumas are usually treated by metal implant fixation, which renders further EMG or MRI examinations impossible. Ultrasonography becomes therefore a method of choice both in initial assessment and when the course of treatment is monitored.
There are several classifications of traumas, but the division made by Seddon in 1943 and by Sunderland in 1951 are the most universal(1, 2). The Seddon classification distinguishes three classes of nerve injuries(1):
Neuropraxia – consists in the interruption of impulse conduction without the loss of axonal continuity; the regeneration process lasts several weeks;
Axonotmesis – consists in the injury of the axon and the myelin sheath with the preservation of the continuity of the endoneurium, perineurium and epineurium. Regeneration is possible and occurs spontaneously and slowly at a pace of 1 mm per day;
Neurotmesis – is the most serious nerve damage consisting in total transection of the axons and their myelin sheaths, endoneurium perineurium and epineurium.
The Sunderland classification(2) distinguishes five classes of nerve injury. When compared with the Seddon classification, the first class of the Sunderland classification corresponds to neurotmesis and the second to axonotmesis. The third class is a disruption of the axons and endoneurium with the preservation of the perineurium and epineurium. In the fourth class, only the epineurium is preserved, and in the fifth class, the entire nerve trunk is severed with two stumps visible in a certain distance from each other. In neurotmesis injuries, surgical reconstruction of the nerve continuity is necessary. Preferably, this should be done in the first week following the trauma. Ultrasound assessment is therefore important. An EMG examination in such an early stage is not reliable.
When taking into account the mechanisms of trauma, three types of nerve injury may be distinguished:
stretching;
crushing or bruising [in the Polish literature called “choking” (Polish zdławienie)];
severance.
Stretch injuries may accompany joint dislocations (e.g. peroneal nerve injury may follow knee luxation)(3, 4). This mechanism is also observed in brachial plexus damage after motorcycle accidents.
The traumas resulting from crushing (compression) usually concern the nerves located directly on the bone(5).
Nerve severance may be partial or complete. In the first days following the trauma, particularly following partial injury, assessment may be complicated by edema and the presence of an isoechoic hematoma. In such a situation, the examination should be repeated after several days so as to establish the final diagnosis within the first week following the trauma. This will increase the chance to restore proper function of the nerve by means of an early surgical intervention.
During a preoperative examination, one may simultaneously asses the nerve which could be used for a potential transplant and check it for possible asymptomatic pathologies such as benign proliferative lesions or anatomical variants. Such knowledge facilitates the planning of surgical procedures.
Early diagnosis of posttraumatic peripheral neuropathies involves a complete interview, physical examination with a proper neurological assessment of the sensory, motor and vegetative components of the nerve and functional tests. Ultrasonography is more and more often included as well. In some cases, MRI is conducted.
Ultrasonography allows the localization and character of the peripheral neuropathy to be accurately determined. It is used both pre- and postoperatively. It enables the assessment of slight nerve branches as well as long nerve trunks. Moreover, both static and dynamic examinations can be performed. Nerves are assessed in the conventional gray-scale in the B-mode and Doppler mode.
Material and methods
The primary aim of this paper was to assess the relevance of high-frequency US examination in qualifying patients for either surgical or conservative treatment of posttraumatic peripheral neuropathies.
The specific objectives were:
to specify ultrasound features of peripheral nerve injuries in terms of their qualification for surgical or conservative treatment;
to determine the diagnostic value of ultrasonography in the assessment of nerve injuries with respect to clinical and surgical verification as well as results of functional examinations.
Material
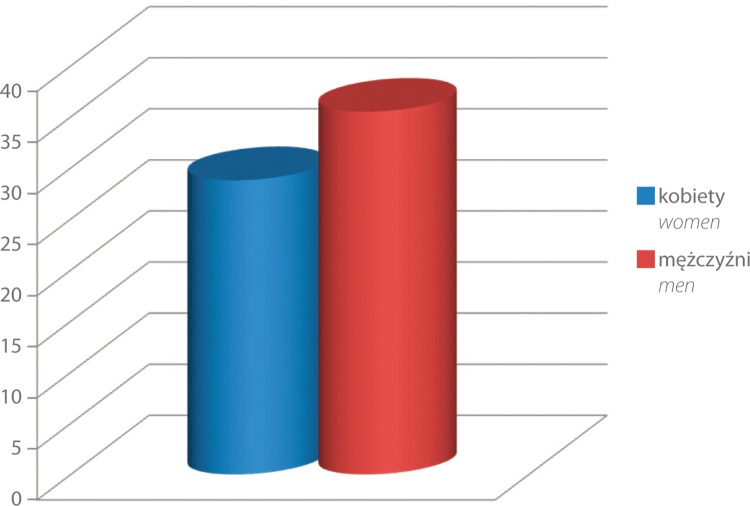
The study was conducted in a group of 47 patients aged 16–65 (mean age 33) who in 2009–2011 were referred to ultrasound examinations due to a clinical suspicion of peripheral neuropathies. The group included 30 males aged 16–62 (mean age 35.5) and 17 females aged 20–65 (mean age 28.8) (Fig. 1).
Fig. 1.
Mean age versus sex in the group of patients with posttraumatic neuropathies
The patients examined presented with neuropathies of the following peripheral nerves: median, ulnar, common peroneal, digital, cutaneous in the deltoid area, mental, PIN and RSNR. In 21 patients, nerve injuries were partial, and in 24 – complete. In 2 cases, the nerve was entrapped between bony fragments. In the case of partial injuries, the percentage extent of damage in relation to the remaining normal structure was assessed in the transverse section. 17 of 21 patients with partial nerve injuries (80.95%) underwent an EMG examination. No functional tests were conducted in the cases of complete injuries when ultrasound imaging had confirmed the result of the clinical examination.
The patients were referred to a US examination by orthopedists, neurologists and physiotherapists. All patients gave written consent to the participation in the study. The examinations were conducted in two health care facilities in Krakow: Intermed and TLK Med.
The US examinations were performed with Esaote MyLab 50 and MyLab 60 systems using high-frequency broadband linear transducers: 6–18 MHz (mainly of 12–18 MHz). Additionally, in obese patients and when examining deeplocated nerves, convex transducers were applied which enabled deeper penetration of the ultrasound beam.
The nerves were evaluated in the gray-scale and in the power Doppler mode in longitudinal and transverse sections in terms of:
localization, morphology and the grade of injury;
possible anatomic variants of the nerve trunk and pathologies of the adjacent tissues.
Furthermore:
a dynamic examination was performed to observe the sliding of the nerve trunk in relation to the adjacent tissues in the maximal movement range of the nearest joints;
it was attempted to induce pain or paresthesia by palpation at the site of the visualized pathology;
the motor and sensory-motor nerves were assessed indirectly based on the images of the skeletal muscles innervated by these nerves.
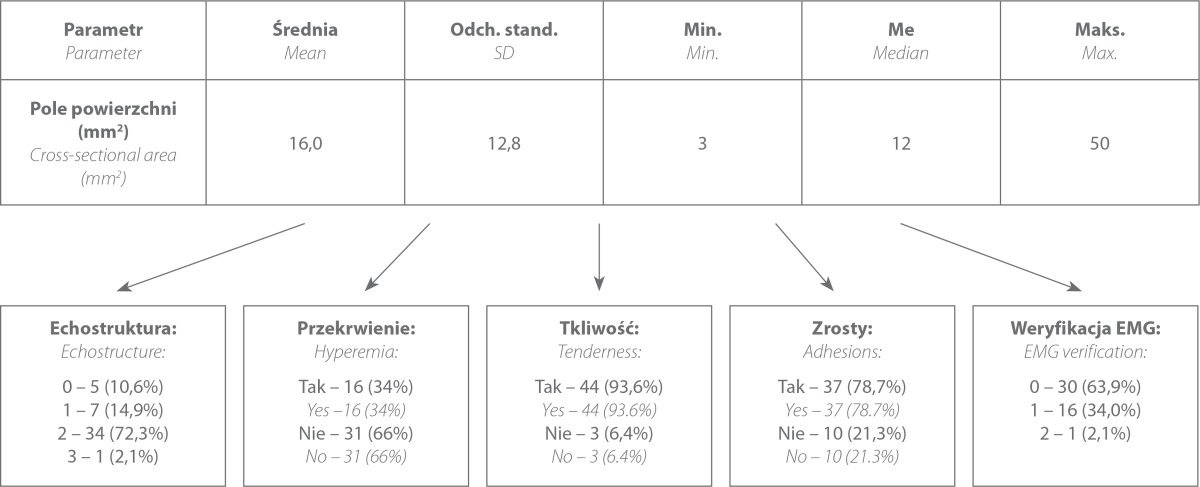
The analyses of the collected material were performed by means of descriptive statistics. Mean cross-sectional areas and diameters of the posttraumatic lesions of the peripheral nerve trunks were calculated. The individual ultrasound features of the peripheral nerves analyzed in this study, such as echostructure and hyperemia, were divided into subgroups to determine the most common US features in individual neuropathies. Moreover, the authors determined the frequency of adhesions between the nerve trunks and adjacent tissues as well as the frequency of pain on compression with the transducer. The agreement of the US examinations with EMG tests, clinical examination and surgical verification was also checked. The values obtained were presented in the figures.
The article is the second part of a series of publications prepared on the basis of the author's doctoral thesis entitled: Usefulness of ultrasonography with high-frequency transducers in the diagnosis of peripheral neuropathies (supervised by: Prof. Iwona Sudoł-Szopińska, MD, PhD, defended on November 4, 2014 in Warsaw).
Results
The following ultrasound features were assessed:
1. Nerve trunk continuity
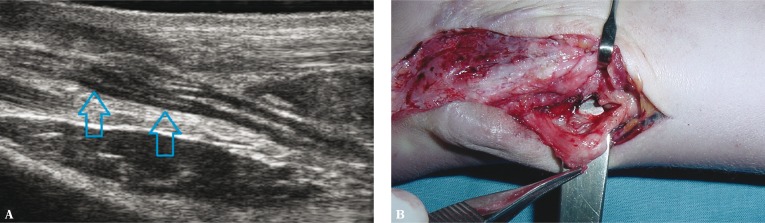
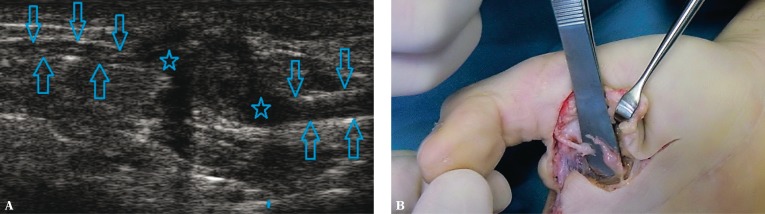
In the case of partial injuries, the extent of damage was estimated in the transverse section by providing the percentage of damaged nerve bundles in relation to the entire nerve section. Moreover, it was specified which bundles were damaged: medial, lateral, ventral or dorsal (Fig. 2A, B). In the case of complete injuries, the localization of stumps was specified, the size of possible neuromas was determined and the distance between the unaltered tissue of both stumps was measured (Fig. 3A, B).
Fig. 2.
Neuroma-in-continuity of the median nerve (arrows) resulting from partial injury: A. ultrasound image – longitudinal view; B. intraoperative image
Fig. 3.
A. Ultrasound image of complete injury to the common digital nerve – neuromas (asterisks), nerve stumps (arrows); B. intraoperative picture
In each case, the site of nerve damage was specified, and its distance from characteristic anatomic structures was provided in centimeters or millimeters.
echostructure of the peripheral nerves;
vascularization of the peripheral nerves;
measurement results.
The diameter and length or neuromas were measured. In the case of complete nerve damage, the distance between the unaltered tissue of both stumps was determined (i.e. peripherally to the neuroma-like deformations of the nerve ends).
2. Adhesions
The patients underwent a dynamic US examination to determine the presence of adhesions between nerve trunks and adjacent tissues. By mobilizing the nearest joints or activating the adjacent muscle parts, it was observed whether normal sliding of the epineurium occurs or whether it is “wrinkled.” The transducer was applied parallelly to the course of the nerve trunk.
3. Tenderness on palpation
The aforementioned terms were explained in the article entitled: Assessment of the utility of ultrasonography with high-frequency transducers in the diagnosis of entrapment neuropathies which was published in the 59th issue of „Journal of Ultrasonography”(6).
Based on the clinical and US examinations, the patients were qualified for either surgical or conservative treatment. Thirty-nine patients were operated, and 8 received conservative treatment.
The ultrasound presentation of posttraumatic neuropathies encompasses a wide range of morphological changes. In the author's own study, the continuity of the epineurium, the continuity and homogeneity of the bundle structure of the nerve and its vascularization were assessed. Edema at the preserved epineurium presents itself as a fusiform thickening of the trunk outlines. The measurement of the cross-sectional area at the apex of this thickening was the most reliable and repeatable parameter used in follow-up examinations.
The assessment of the inner structure of the nerve did not pose any problems when high-frequency transducers were applied. The percentage of damaged bundles in relation to the preserved structure was specified.
In the case of partial injuries, “a neuroma-in-continuity” develops in the regeneration process. Such a neuroma is a lesion of a fusiform which models the part of intact bundles. Its length and diameter were measured.
In the case of complete nerve severance, the distance between the stumps and between the normal nervous tissue was measured.
In the stretch injuries, the lesions involved a long fragment of the nerve trunk with the disruption of the continuity of individual bundles at many levels.
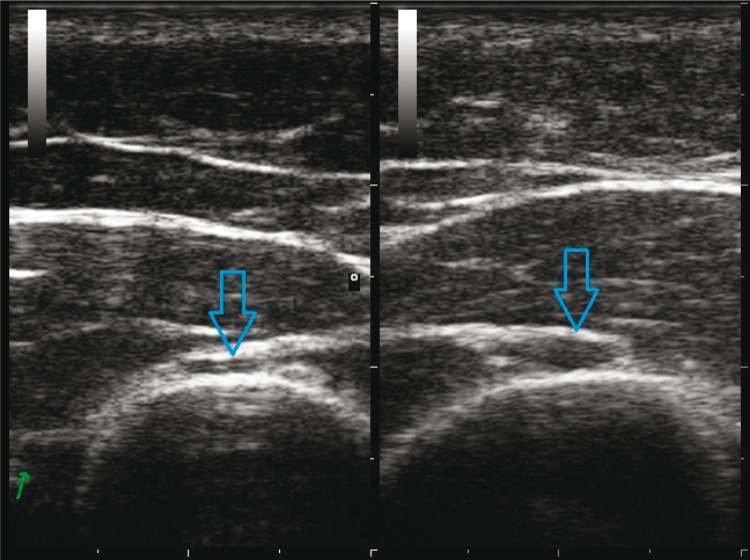
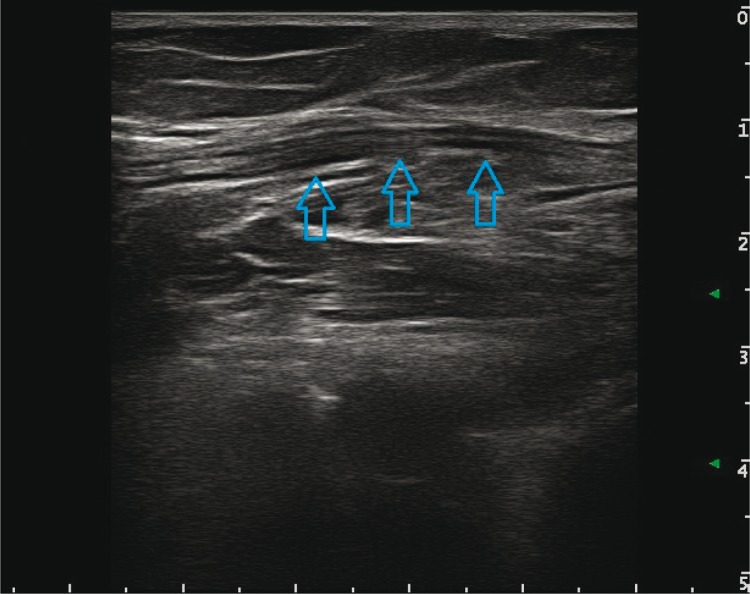
The traumas resulting from crushing/compression usually concerned nerves located directly on the bone surface. The image of the damaged nerve varied depending on the force and repeatability of the trauma. Slight, but repeatable traumas led to a fusiform, reactive thickening of the nerve trunk, including thickening and fibrosis of the epineurium and its hyperemia. For instance, such a situation is observed in cyclists who develop neuropathic changes of the superficial branch of the ulnar nerve at the level of the hook of the hamate bone (as a result of micro-traumas against the handlebar). A similar damage mechanism was observed in a female patient who incompetently used automassage in the area of the spiral groove of the humerus (which resulted in transient radial nerve palsy) (Fig. 4) and in a hockey player who was hit with a hockey puck in the region of the neck of the fibula (with transient common peroneal nerve palsy) (Fig. 5). A single high-energy trauma rarely led to a disruption of the nerve continuity. In a US examination, focal or complete blurring of the bundle structure as well as nerve edema and hyperemia were observed. The epineurium itself was also thickened (edema).
Fig. 4.
Ultrasound image of the normal radial nerve (left side) and the radial nerve with features of edema (right side) resulting from chronic mechanical compression
Fig. 5.
Ultrasound image of the common peroneal nerve (arrows) following a hit with a hockey puck – longitudinal view
Nerve severance may be partial or complete. In the case of a partial injury to the nerve, a fragmentary, non-transmural severance of the epineurium and a part of nerve bundles was observed. In an early posttraumatic stage, the following were observed: edema of the remaining bundles, developing hematoma at the site of injury and nerve hyperemia. Over time, a regenerate of the nervous and connective tissue formed. When the outcome of the healing process of a partial injury was unfavorable, “a neuroma-in-continuity” developed.
In single cases of a complete (transmural) injury of the nerve trunk, the ends of the stumps adhered to each other thus mimicking preserved nerve continuity. In such situations, pressure was applied with the transducer which caused their separation and induced a paradoxical reciprocal movement. Over time, neuromas developed at the stump ends. Stumps and their neuromas were sometimes pulled into scars of adjacent muscle or fascia structures. In such a situation, the role of a US examination was to determine their accurate location, which considerably facilitated the planning of the surgical approach. Frequently, the location of stumps was highlighted with a marker on the patients’ skin and photographed, or the patients with such markings were referred directly to the surgeon (Fig. 6).
Fig. 6.
Schematic figure showing the localization of the stumps of the damaged radial nerve
Comparison of EMG and US findings
EMG examinations were conducted in 17 patients (36.1%). They did not confirm US findings and were inconsistent with the surgical verification in one case. In the remaining cases, they were consistent.
Discussion
Peripheral neuropathies are a group of numerous pathologies bordering neurology, orthopedics and traumatology. Patients with such conditions also report to rehabilitation clinics. For many years, the basis for the diagnosis was the clinical assessment. In the 1940s, the diagnosis of peripheral nerve pathologies was expanded to include functional electromyographic tests(7–9). Since the 1990s, ultrasonography has been gaining popularity, also in the diagnosis of posttraumatic peripheral neuropathies. In the past decade, this examination has become the leading method for diagnosis of these pathologies and monitoring of their treatment.
Post-traumatic changes of the peripheral nerves (47 patients)
The first reports concerning the usage of ultrasonography in the assessment of posttraumatic nerve trunk changes appeared in 1995(10). Despite the access to low-frequency transducers, these reports concerned the anatomically complex brachial plexus that is difficult to visualize. Japanese researchers analyzed the shape, echostructure, outlines and diameter of the roots and trunks of the plexus in 12 patients with traumas following motorcycle accidents.
The image was compared with the contralateral side, and verified intraoperatively. The US findings were surgically confirmed in 8 of 12 subjects.
A year later, Martinoli et al. published a paper on ultrasonography in diagnosing posttraumatic neuropathies(11). Even then, the authors emphasized that with the development of ultrasound technique and knowledge as well as experience, ultrasonography had a chance to become a reliable tool in initial diagnosis, prognosis, monitoring of conservative treatment and postoperative follow-up of peripheral nerve trunk injuries.
In a paper published in 2004, Turkish authors presented their conclusions from the study conducted in a group of 14 patients with posttraumatic nerve injuries(12). In 4 cases, they observed bundle edema, in 3 – neuromas on the stumps, in 9 – transmural injuries and in 5 – scar tissue in the vicinity of the nerve. All US examinations were verified in surgery. As in the author's own study, the aforementioned authors agreed that the most relevant information for the surgeon concerns: the type of damage (partial, complete), level of damage, presence of neuromas and their localization as well as presence of scars fixing the damaged nerve trunk.
In 2006, a report on 4 patients with posttraumatic brachial plexus injury appeared(13). The US image was verified surgically in 3 patients. In one case, ultrasonography failed to visualize the pathology detected during the surgery, i.e. a neuroma on the fibers of C5–7 roots localized at the level of the pectoralis minor muscle. The authors emphasized the need for experience in assessing neuropathies, particularly at such a region. Other authors also emphasize the long learning curve in US assessment of peripheral nerves and indicate other limitations and advantages of a US examination(14). They draw attention to the examiner-dependent interpretation. Moreover, they emphasize the superiority of US to MRI in the scope of possibilities to assess long nerve trunk fragments during a single examination, the speed of assessment and high image resolution.
Tab. 1.
Frequency in which individual ultrasound elements occurred in patients with symptoms of posttraumatic neuropathies
The sensitivity and specificity of a US examination in posttraumatic radial, ulnar and median neuropathies was 89% and 95% respectively in a study of Cartwright et al. from 2007(15). The study involved ultrasound assessment of 12 upper extremities of cadavers in which the nerves were damaged in a controlled fashion. In the group of 60 transected nerves, 2 false positive and 2 false negative results were obtained. The remaining examinations were verified upon dissection.
In the same year, Çokluk et al. presented the results of the analysis concerning the usefulness of an ultrasound examination in 22 patients with sciatic nerve injury (17) and femoral nerve injury (5)(16). Complete nerve trunk injury was observed in one patient; in the remaining cases, the injury was partial. The injuries were accurately localized in 95.5% of cases. The authors emphasized the advantages of ultrasonography by comparing it to neurophysiological tests: determining localization and morphology of nerve injuries, identification of the adjacent hematomas, foreign bodies, necrotic tissue and injuries to the neighboring vessels, tendons and muscles. All neuromas and foreign bodies were visualized. The conclusions drawn from the two papers described above are similar to those obtained in this paper.
To date, the largest study (202 patients, including 117 cases verified surgically) on the usefulness of ultrasonography in the assessment of posttraumatic neuropathies was published in 2011(17). The US findings were verified surgically in 93.7% of cases. The bundle structure, perineurium and epineurium as well as adjacent tissues were assessed. Various nerves were examined including the median nerve (58), ulnar nerve (51), radial nerve (57), common peroneal nerve (28) and tibial nerve (8). The authors divided nerve injuries into seven groups based on the bundle structure, structure of the perineurium and epineurium as well as the morphology of the adjacent tissues. According to the author of this paper, the description should, from the practical point of view, facilitate making correct decisions about the manner of treatment, planning and conducting the surgery.
Particular attention should be paid to posttraumatic injuries of the radial nerve. Due to its direct position on a bony surface, it is susceptible to all types of damage. They are usually associated with humerus fractures (2–18% of patients)(18, 19). Moreover, this nerve may sometimes be damaged during treatment of such fractures (conservative or surgical).
One of the first papers on diagnostic ultrasound in radial nerve palsy was a prospective analysis of 11 patients following humerus fractures(20). Surgical treatment was conducted in 5 patients; the remaining 6 patients received conservative treatment which, as it occurred later, was effective. All patients underwent an X-ray examination of the humerus as well as US and neurophysiological examinations of the nerve. As in the author's own study, patients with neuropraxia did not show the loss of continuity of any of the sheaths (either perineurium or epineurium). However, compared to the contralateral healthy extremity, significant thickening of the nerve outlines was observed expressed with an increase in the cross-sectional diameter of the nerve trunk (mean mediolateral dimension in the aforementioned paper was 5.4 mm and in the author's own study – 6.7 mm). These findings were compared with the diameter of normal radial nerves measured in 10 healthy volunteers, the mean value of which was 2.4 mm. Moreover, disordered bundle echostructure was also observed; some bundles were dilated over a long fragment. This is consistent with the author's own findings and concerned all patients from this group.
The US examinations of the radial nerve in asymptomatic patients, the aim of which was to specify the cross-sectional area of the radial nerve at the level of the spiral groove, were also conducted by Foxall et al. in 2007, Martinoli et al. in 2004 and Rossey-Marec et al. in 2004(21–23). The normal values fell within the range of 4.0–4.2 mm2, and the anteroposterior dimension was 2.3–3.5 mm.
In five cases of radial nerve neuropraxia in the author's own study, the cross-sectional area ranged from 8 to 38 mm2, which is consistent with the results quoted above. This group includes patients with transient compression or irritation of the radial nerve trunk at the level of the spiral groove. In one case, transient nerve palsy developed due to incompetent automassage of the arm. In three cases, palsy developed due to assuming a specific position at night, and in a case of a motorcyclist – as a result of compression applied by a protective shoulder pad. In all patients, ultrasonography ruled out the necessity for surgical treatment due to preserved bundle structure of the nerve. In three patients, EMG tests were conducted and confirmed minimal conduction disorders. The nerve returned to its full function after 6 weeks in all the patients.
Moreover, in the author's own material, a pathological image of the nerve with signs of neuropraxia was found in a patient with damage to the mental nerve resulting from crushing. Following repeated ultrasound-guided injections with low doses of Diprophos (in 6-week intervals), a full return of sensation and normalization of a US image were obtained (the US image of the nerve was comparable to the contralateral side).
The peroneal nerve with features of posttraumatic changes associated with neuropraxia was observed in one patient – a hockey player with transient nerve palsy after being hit with a hockey puck in the region of the head of the fibula. Following the injury, the cross-sectional area of the nerve amounted to 45 mm2, the bundle structure was disordered and slight hyperemia was observed. A follow-up US examination conducted after a month showed complete normalization of the image.
In a study conducted in an Austrian center in 2005, the analysis concerned 9 patients with peroneal nerve palsy after knee luxation(24). The continuity of the nerve and cross-sectional area were assessed and compared with the contralateral side and the images of 11 healthy volunteers. The mean value in the healthy individuals was 18 mm2. In the case of nerve palsy, its cross-sectional area amounted to 70 mm2. In 5 cases, a surgical procedure was conducted which confirmed the US findings. The remaining patients received effective conservative treatment. In the author's own study, the cross-sectional area of the nerve was lower than in the paper discussed above, which apparently resulted from a mild injury sustained by the hockey player. This is confirmed by a short recovery period.
Another case with symptoms of transient nerve palsy was a 45-year-old male chronically treated with antithrombotic medications due to artificial aortic valve implantation. Following a fall on the elbow, the blood was extravasated to the subcutaneous tissue of the cubital fossa and to the median nerve itself. Three days after the injury, edema increased and pain in the region of the elbow exacerbated. Simultaneously, the patient lost sensation in his second and third fingers and on the ventral aspect of his hand, including the region of the thenar eminence. The US examination at the pronator teres muscle showed an extensive hematoma in the subcutaneous tissue in the direct vicinity of the nerve and in the region of the nerve trunk itself. The patient was followed-up repeatedly with ultrasonography. It was observed how the hematoma and edema reduced gradually and how the bundle picture of the nerve trunk returned. Following 17 months, neurological symptoms subsided completely. The ultrasound image remained, however, altered permanently (thickened nerve trunk outline, disordered echostructure).
Conclusions
High-frequency ultrasonography is a valuable modality in qualifying patients to surgical procedures or conservative treatment of posttraumatic peripheral neuropathies.
- The ultrasound features of peripheral nerve injuries which in the author's own studies occurred to be the most relevant in terms of qualifying patients for surgical or conservative neuropathy treatment were:
- diameter or cross-sectional area of the nerve at the site of the visualized pathology;
- nerve echostructure, hyperemia;
- presence of adhesions in a dynamic US examination;
- abnormalities of the adjacent tissues (including muscles, bone surfaces and tendon sheaths);
- pain reaction to nerve compression with the transducer.
The results of clinical and surgical verification were consistent with the ultrasound findings in all patients.
Conflict of interest
The author does not report any financial or personal links with other persons or organizations, which might negatively affect the content of this publication and claim authorship rights to this publication.
References
- 1.Seddon H. Edinburgh: Churchill Livingstone; 1975. Surgical Disorders of the Peripheral Nerves. [Google Scholar]
- 2.Sunderland S. Edinburgh: Churchill Livingstone; 1978. Nerves and Nerve Injuries. [Google Scholar]
- 3.Martinoli C. Imaging of the peripheral nerves. Semin Musculoskelet Radiol. 2010;14:461–462. doi: 10.1055/s-0030-1268395. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi S, Martinoli C. Warszawa: Medipage; 2009. Ultrasonografia układu mięśniowo-szkieletowego. Tom II. [Google Scholar]
- 5.Marhofer P. Warszawa: MedMedia; 2010. Zastosowanie ultrasonografii w blokadach nerwów obwodowych. Zasady i praktyka. [Google Scholar]
- 6.Kowalska B. Assessment of the utility of ultrasonography with high- frequency transducers in the diagnosis of entrapment neuropathies. J Ultrason. 2014;14:371–392. doi: 10.15557/JoU.2014.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banach M, Bogucki A, editors. Kraków: Medycyna Praktyczna; 2003. Zespoły z ucisku – diagnostyka i leczenie. [Google Scholar]
- 8.Żyluk A, Walaszek I, Szlosser Z. No correlation between sonographic and electrophysiological parameters in carpal tunnel syndrome. J Hand Surg Eur Vol. 2014;39:161–166. doi: 10.1177/1753193413489046. [DOI] [PubMed] [Google Scholar]
- 9.Lee D, van Holsbeeck MT, Janevski PK, Ganos DL, Ditmars DM, Darian VB. Diagnosis of carpal tunnel syndrome. Ultrasound versus electromyography. Radiol Clin North Am. 1999;37:859–872. doi: 10.1016/s0033-8389(05)70132-9. [DOI] [PubMed] [Google Scholar]
- 10.Hayamizu K, Naito K, Ito K. Ultrasonography for traction injuries of the brachial plexus. Nihon Igaku Hoshasen Gakkai Zasshi. 1995;55:873–877. [PubMed] [Google Scholar]
- 11.Martinoli C, Serafini G, Bianchi S, Bertolotto M, Gandolfo N, Derchi LE. Ultrasonography of peripheral nerves. J Peripher Nerv Syst. 1996;1:169–178. [PubMed] [Google Scholar]
- 12.Cokluk C, Aydin K, Senel A. Presurgical ultrasound-assisted neuro- examination in the surgical repair of peripheral nerve injury. Minim Invasive Neurosurg. 2004;47:169–172. doi: 10.1055/s-2004-818486. [DOI] [PubMed] [Google Scholar]
- 13.Haber HP, Sinis N, Haerle M, Schaller HE. Sonography of brachial plexus traction injuries. AJR Am J Roentgenol. 2006;186:1787–1791. doi: 10.2214/AJR.04.1861. [DOI] [PubMed] [Google Scholar]
- 14.Bodner G, Buchberger W, Schocke M, Bale R, Huber B, Harpf C, et al. Radial nerve palsy associated with humeral shaft fracture: evaluation with US – initial experience. Radiology. 2001;219:811–816. doi: 10.1148/radiology.219.3.r01jn09811. [DOI] [PubMed] [Google Scholar]
- 15.Cartwright MS, Chloros GD, Walker FO, Wiesler ER, Campbell WW. Diagnostic ultrasound for nerve transection. Muscle Nerve. 2007;35:796–799. doi: 10.1002/mus.20761. [DOI] [PubMed] [Google Scholar]
- 16.Çokluk C, Aydin K. Ultrasound examination in the surgical treatment of lower extremity peripheral nerve injuries: part II. Turk Neurosurg. 2007;17:197–201. [PubMed] [Google Scholar]
- 17.Zhu J, Liu F, Li D, Shao J, Hu B. Preliminary study of the types of traumatic peripheral nerve injuries by ultrasound. Eur Radiol. 2011;21:1097–1101. doi: 10.1007/s00330-010-1992-3. [DOI] [PubMed] [Google Scholar]
- 18.Samardzić M, Grujicić D, Milinković ZB. Radial nerve lesions associated with fractures of the humeral shaft. Injury. 1990;21:220–222. doi: 10.1016/0020-1383(90)90006-g. [DOI] [PubMed] [Google Scholar]
- 19.Böstman O, Bakalim G, Vainionpää S, Wilppula E, Pätiälä H, Rokkanen P. Immediate radial nerve palsy complicating fracture of the shaft of the humerus: when is early exploration justified? Injury. 1985;16:499–502. doi: 10.1016/0020-1383(85)90181-0. [DOI] [PubMed] [Google Scholar]
- 20.Bodner G, Huber B, Schwabegger A, Lutz M, Waldenberger P. Sonographic detection of radial nerve entrapment within a humerus fracture. J Ultrasound Med. 1999;18:703–706. doi: 10.7863/jum.1999.18.10.703. [DOI] [PubMed] [Google Scholar]
- 21.Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, et al. Sonography of entrapment neuropathies in the upper limb (wrist excluded) J Clin Ultrasound. 2004;32:438–450. doi: 10.1002/jcu.20067. [DOI] [PubMed] [Google Scholar]
- 22.Foxall GL, Skinner D, Hardman JG, Bedforth NM. Ultrasound anatomy of the radial nerve in the distal upper arm. Reg Anesth Pain Med. 2007;32:217–220. doi: 10.1016/j.rapm.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Rossey-Marec D, Simonet J, Beccari R, Michot C, Bencteux P, Dacher JN, et al. Ultrasonographic appearance of idiopathic radial nerve constriction proximal to the elbow. J Ultrasound Med. 2004;23:1003–1007. doi: 10.7863/jum.2004.23.7.1003. [DOI] [PubMed] [Google Scholar]
- 24.Gruber H, Peer S, Meirer R, Bodner G. Peroneal nerve palsy associated with knee luxation: evaluation by sonography – initial experiences. AJR Am J Roentgenol. 2005;185:1119–1125. doi: 10.2214/AJR.04.1050. [DOI] [PubMed] [Google Scholar]