Abstract
Pain in the lateral compartment of the elbow joint and decreased strength of the extensor muscle constitute a fairly common clinical problem. These symptoms, occurring in such movements as inverting and converting the forearm, pushing, lifting and pulling, mostly affect people who carry out daily activities with an intense use of wrist, e.g. work on computer. Strains in this area often result from persistent overload and degeneration processes of the common extensor tendon and the radial collateral ligament. Similar symptoms resulting from the compression of deep branch of the radial nerve in radial nerve tunnel should be remembered as well. It happens that both conditions occur simultaneously. A proper diagnosis is essential in undertaking an effective treatment. Ultrasonography is a non-invasive method and the application of high-end apparatus with heads of frequencies exceeding 12 MHz allows for a precise evaluation of joint structures, tendons and nerves. In case of the so-called tennis elbow, the examination allows for evaluation of the degree and extent of injury to the radial collateral ligament and common extensor tendon, in addition to the presence of blood vessels in inflicted area. Administration of autologous blood platelets concentrate containing growth factors, used in treatment of tennis elbow, is performed under ultrasound image control conditions. This allows for a precise incision of scar whilst keeping a healthy (unaffected) tissue margin to form fine channels enabling the penetration of growth factors. Post-surgery medical check-up allows for the evaluation of treatment effectiveness. In radial nerve tunnel syndrome, the ultrasound examination can reveal abnormalities in the deep branch of the radial nerve and within the anatomical structures adjacent to the nerve in the radial nerve tunnel. Furthermore, the ultrasound examination allows for detection of other articular and extraarticular pathologies, which affect the compression of the deep branch of radial nerve, such as skeletal deformations, post-traumatic changes, arthritis, and the presence of tumors. The ultrasonography is also helpful in differentiation of symptoms arising from cervical radiculopathy or brachial plexus injury.
Keywords: tennis elbow, common extensor tendon, lateral collateral ligament complex, radial tunnel syndrome, deep branch of the radial nerve
Abstract
Ból bocznego przedziału stawu łokciowego oraz osłabienie siły mięśniowej prostowników są dość powszechnym problemem klinicznym. Objawy te, występujące podczas ruchów odwracania i nawracania przedramienia, pchania, podnoszenia i pociągania dotyczą najczęściej osób, które na co dzień wykonują czynności z aktywnym angażowaniem nadgarstka, na przykład pracując przy komputerze. Dolegliwości w tej okolicy najczęściej powstają w wyniku przewlekłych przeciążeń i procesów degeneracyjnych ścięgna wspólnego prostowników oraz więzadła pobocznego promieniowego. Należy pamiętać o podobnych objawach wynikających z ucisku gałęzi głębokiej nerwu promieniowego w kanale nerwu promieniowego. Zdarza się, że obydwa schorzenia występują jednocześnie. Właściwa diagnoza stanowi podstawę skutecznego leczenia. Badanie ultrasonograficzne jest nieinwazyjną metodą obrazowania, a zastosowanie wysokiej klasy aparatu z głowicami o częstotliwościach powyżej 12 MHz pozwala na precyzyjną ocenę struktur stawowych, ścięgien i nerwów. W przypadku tzw. łokcia tenisisty badanie umożliwia ocenę stopnia i rozległości uszkodzenia więzadła pobocznego promieniowego i ścięgna wspólnego prostowników, a także obecności naczyń w obszarach uszkodzenia. Stosowane w leczeniu łokcia tenisisty podawanie koncentratu płytek autologicznej krwi zawierającej czynniki wzrostu wykonuje się pod kontrolą obrazu ultrasonograficznego. Dzięki temu możliwe jest precyzyjne nakłucie blizny z marginesem zdrowych tkanek, aby wytworzyć drobne kanaliki, które umożliwią penetrację czynników wzrostowych. Kontrolne badania po zabiegu pozwalają na ocenę skuteczności leczenia. W przypadku zespołu kanału nerwu promieniowego badanie ultrasonograficzne umożliwia wykrycie nieprawidłowości w gałęzi głębokiej nerwu promieniowego oraz w obrębie struktur anatomicznych graniczących z nerwem w kanale nerwu promieniowego. Badanie umożliwia wykrycie innych patologii stawowych i pozastawowych, które mają wpływ na ucisk gałęzi głębokiej nerwu promieniowego, takich jak deformacje kostne, zmiany pourazowe, zapalenie stawu oraz obecność guzów. Badanie pomaga także w różnicowaniu dolegliwości wynikających z radikulopatii szyjnej i uszkodzenia splotu barkowego.
Introduction
Burdensome dysfunction of the upper limb due to pain around a lateral epicondyle of the humerus, which appears during supination and pronation of the forearm while the elbow is stretched out, belongs to the most common complaints regarding the upper extremity.
Pain symptoms within the lateral compartment of the elbow are fairly common, particularly in the fourth and fifth decade of life, regardless of gender(1). Pain appears also during the extension of wrist in movements such as grasping, lifting, pushing, pulling and turning. Occasionally, weakening of the extensor muscles may occur as well. The above set of symptoms is commonly referred to as “tennis elbow”, however similar symptoms could occur in radial tunnel syndrome in the course of chronic compression of deep branch of a radial nerve in the radial tunnel(2–4). In both diseases the pathogenesis of pain is different and clinical examination is crucial in differentiating between these two pathologies. Ultrasonography (US) constitutes an extremely important technique for imaging the area in question, by helping in formulation of proper diagnosis and determination of further proceedings.
Tennis elbow
Anatomy
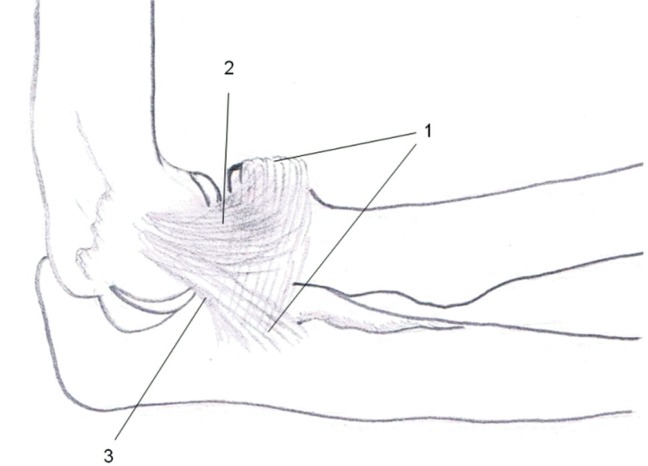
The lateral epicondyle of the humerus serves as a zone of attachment for the lateral collateral ligament as well as the common extensor, anconeus and supinator muscle proximal tendons. The deepest layer of the common extensor complex is formed by the lateral collateral ligament, which lies below the common extensor tendon, and inserts on the distal lateral surface of the lateral epicondyle, below the humeral attachment of the common extensor tendon. The lateral collateral ligament complex consists of: radial collateral, lateral ulnar collateral ligament and annular ligament. The radial collateral ligament blends fibers with the annular ligament and supinator's fascia. Fibers of the lateral ulnar collateral ligament run posteriorly to the radial collateral ligament and attach to the ulna below the attachment of the annular ligament(5) (fig. 1). The lateral ulnar collateral ligament is rather insignificant in the diagnosis of tennis elbow.
Fig. 1.
Diagram of lateral collateral ligament complex: anular ligament (1), radial collateral ligament (2), and lateral ulnar collateral ligament (3)
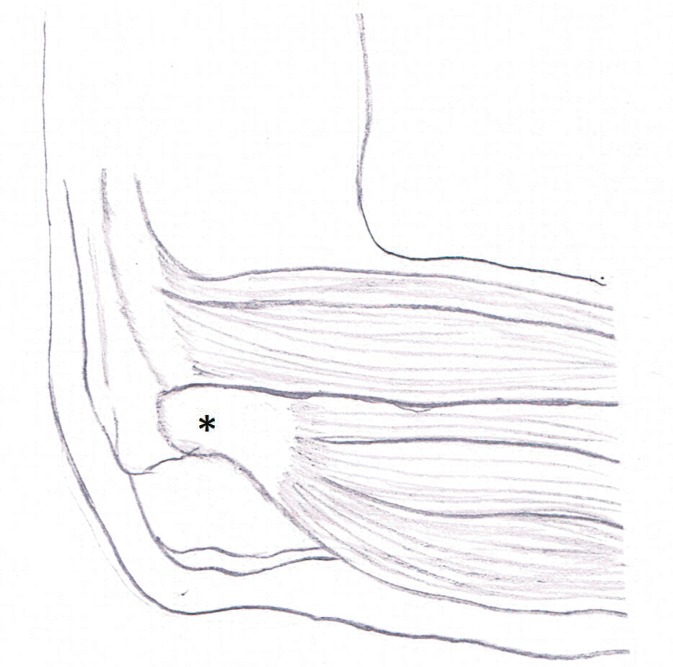
The common extensor tendon is composed of the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi and extensor carpi ulnaris tendons. The origin of the common extensor tendon covers the lateral surface of lateral epicondyle of the humerus (fig. 2). The largest area of the common extensor tendon is covered by fibers of the extensor carpi radialis brevis with length of 13±2 mm and width of 7±2 mm(6). Thus the extensor carpi radialis brevis forms a dominant anterolateral part of the common tendon. The tendon of the extensor digitorum forms the most superficial layer of the common tendon(7). The extensor digiti minimi and the extensor carpi ulnaris minimally contribute to the common tendon, being located in its posterior aspect(5).
Fig. 2.
Diagram of common extensor tendon's attachment to lateral epicondyle of the humerus (*)
The common extensor tendon adheres to the attachment of the extensor carpi radialis longus and brachioradialis tendons near the superolateral border of the lateral epicondyle. The anterolateral surface of the common extensor tendon (the area of the extensor carpi radialis brevis) borders with posterior aspect of the extensor carpi radialis longus and, to a lesser extent, from the posterolateral aspect, it lies alongside the tendon of brachioradialis muscle. The extensor carpi radialis brevis borders directly with a more deeply located radial collateral ligament and lateral ulnar collateral ligament; the deep layers of the ECRB tendon covers the anterior surface of the humeroradial joint(8).
Pathogenesis
The term tennis elbow constitutes a clinical diagnosis, referring to pain in the area of the common extensor tendon. Structural changes of the common extensor include injuries and scarring at its attachment and/or injuries and scar formation of the radial collateral ligament. Both conditions result from microtrauma during repeated supination and pronation movements of a forearm with extended elbow, whether in the context of occupational or sports activity(7, 9–11). Microtrauma initiates the healing process, which usually takes place under nonoptimal conditions, such as continued use of hand in daily and sport related activities. This leads to abnormal remodeling of scars with the formation of degenerated areas, with hypocellular regions, hyalinization, fatty degeneration or even necrosis. Repeating microtrauma sequences and disturbed healing processes (interrupted by new microtrauma incidents) lead to partial tendon tears, often occurring without a distinct and single traumatic incident. The region of the extensor carpi radialis brevis tendon is most prone to such injuries, with the anterior part of the extensor digitorum to a lesser extent(5, 7, 12).
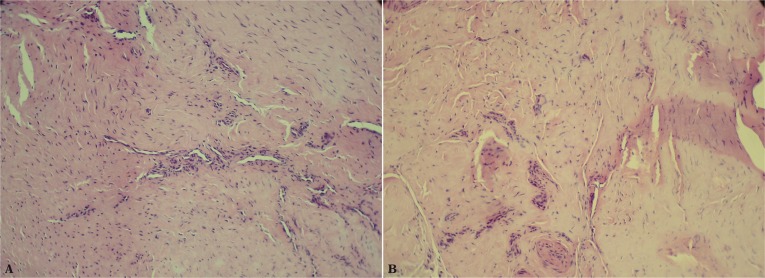
The tendon of the extensor carpi radialis brevis muscle lies directly on anterior surface of the humeroradial joint and participates in every flexor/extensor movement of an elbow. These properties probably account for microtrauma taking place within this tendon(8). Histopathological examinations of damaged structures, literature and own sources demonstrate collagen remodeling dependent on fibroblast infiltration as well as an immature healing reaction, in the absence of inflammatory cells(13) (fig. 3). Due to the absence of inflammatory cells the process was called as angiofibroblastic hyperplasia(13), later termed as angiofibroblastic tendinosis. It should be noted that referring to tennis elbow as tendinitis, which infers an inflammatory process, is incorrect.
Fig. 3.
Histopathological images of material obtained from scars on common extensor tendon: connective tissue which structure resembles that of a tendon, but with disturbed architecture, with areas of tears and evidence of a healing process and scar formation. There is no evidence of an inflammatory reaction
Clinical signs and symptoms
The main symptom is pain around the lateral compartment of elbow joint, which increases by grasping or lifting motions (chair test or coffee cup test)(1). The physical examination reveals a localized pain while application of pressure upon the lateral epicondyle of the humerus(1). Five percent of patients with tennis elbow were found to have suffered from radial tunnel syndrome with decreased muscle strength during grasping, extension and rotation movements of the wrist(14).
Diagnosis
Ultrasonography is a non-invasive technique that can help in establishing the diagnosis and determining further proceedings(1). The examination should be performed using the state-of-the-art US machine with a linear probe of a frequency higher than 12 MHz. Descriptions in the scientific literature of the use of lower frequency probes should be considered historical(1).
In addition to pathologies of extensor tendon attachment and symptoms of radial nerve neuropathy, the US examination may reveal other causes of lateral elbow compartment pain, such as occult fractures, osteochondritis dissecans of the distal humeral epiphysis, degeneration of the lateral compartment of humeroradial joint, instability of the lateral radial ligament or radial tunnel syndrome(1).
Tendinopathy and enthesopathy of the common attachment of the forearm extensor tendons
The extensor carpi radialis brevis is located most anteriorly, and its humeral enthesis covers the majority of the common extensor tendon's footprint(15). The radial collateral ligament and the lateral ulnar collateral ligament are located deeply underneath the common extensor tendon.
Imaging of these structures requires transverse and longitudinal sections made with the elbow in flexion. The initial diagnosis of tendinopathy or enthesopathy is confirmed when injuries are found in areas corresponding to clinical symptoms (pain on palpation)(16). Injury to the common extensor tendon usually affects its anterolateral and medial regions formed by the extensor carpi radialis brevis and, to a lesser extent, the extensor digitorum. The posterior region of the tendon (the area corresponding to the extensor digiti minimi and the extensor carpi ulnaris) usually remains unaffected by disease processes(5).
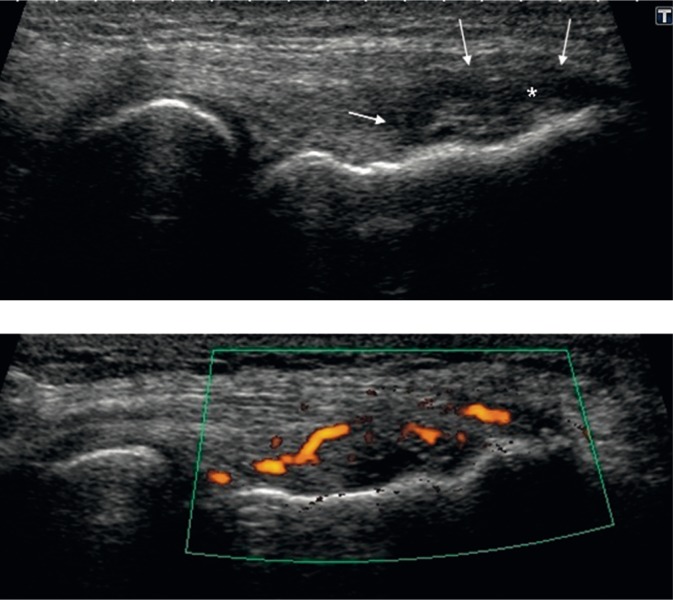
Injury to the common extensor tendon is displayed in US as a hypoechogenic area with a disrupted fibrilar structure in a thickened tendon complex. Occasionally, some fluid can be observed, indicating a fresh tear of the fiber bundles. In case of recent trauma, edema of the tendon is reported. Blood vessels may be found as a part of active healing process, rather than an inflammatory process, as commonly considered. Lack of vessels with or around the injury area indicates presence of fluid and too early stage for vessels to be detected, rebuilt “metabolically silent” scar or areas of severe degeneration. Remodeled scars of the tendon may have a fibrillar or hetereogeneous structure, often containing foci of mineralization or bone formation (fig. 4).
Fig. 4.
US image of common extensor tendon's attachment in a longitudinal section, with a tear in the area of extensor carpi radialis brevis: A. edema of common extensor tendon (arrowheads), with the region of tear appearing hypoechogenic (*); B. US Doppler showing increased vascularity in the area of injury
Injury to the humeral enthesis of the common extensor tendon and the lateral collateral ligament is displayed as irregular bone outline, erosions. Bony erosions always mean an advanced microtrauma to the enthesis, and may also suggest a rheumatological background of the trauma. However, up to now, no specific elements of the US picture have been identified that could differentiate traumatic disease resulting from an inflammatory one. Instead, it has been suggested that the mechanical element (microtrauma) may be a trigger point for spondyloarthropathy.
Injury of the radial collateral ligament
The radial collateral ligament is located directly under the extensor carpi radialis brevis tendon. Injury to the radial collateral ligament may be isolated or may coexist with lesions of the common extensor tendon (fig. 5).
Fig. 5.
Radial collateral ligament with calcified scar at the humeral attachment
Injury most commonly affects the ligament's proximal part and the humeral attachment. On the other hand, a complete tear of the radial collateral ligament could occur, which is of key importance in planning the surgical correction of an injury to the common extensor tendon. Under these circumstances, a typical procedure of separating the tendon from the enthesis could result in deterioration of a patient's clinical state due to iatrogenic posterolateral instability of the joint.
Treatment
As the first step, a conservative treatment is applied, i.e. limited physical activity and cryotherapy, which constricts the blood vessels and provides analgesia(1). Various physiotherapeutic techniques are recommended, including shock waves therapy. A more recent approach is the injection of autologous platelet concentrates containing platelet growth factors, in order to stimulate the healing process(1, 12, 17) (fig. 6).
Fig. 6.
Procedure of administering growth factors into common extensor tendon tear area
It should be emphasized that administering even 1 or 3 ml blood-derived concentrate could be harmful. The high-pressure injection of a growth factor concentrate could cause delamination of degenerated layers from unaffected tissues. And this should be avoided. The GF injection procedure must be preceded by multiple needle stabs of the scar, with a healthy tissue margin, so that tiny canaliculi are formed, local bleeding is generated and the area will be infiltrated by the growth factors, and later by cells of all stages of healing process.
After such a procedure, US with color Doppler demonstrates an increase of vessels within the area of the needling procedure and growth factor's administration, indicating an active healing process.
If such treatment turns ineffective, the patient is referred for surgical treatment.
Surgical treatment is considered very effective due to fast healing of wounds and quick mobilization of the extremity(1, 18, 19). The tendon of the extensor carpi radialis brevis is reached through an anterolateral incision, after the separation of the extensor carpi radialis brevis and longus tendons. Degenerated tissue is removed, and the extensor carpi radialis brevis/ common extensor tendon is cut off from its humeral enthesis. The tendon does not require suturing as it is kept in place by the adherent fascia, which prevents retraction of the proximal segment(7, 8). Due to the extra-articular approach, the time and costs of the procedure are lower when comparing to arthroscopy(1). Within 3–4 months, the majority of patients who underwent this treatment, fully return to their pre-injury, daily and sports activities(1, 7, 11).
Radial tunnel syndrome
In literature, the pathologies of deep branch of the radial nerve at the level of the radial nerve tunnel are referred to as the radial tunnel syndrome or the posterior interosseous nerve (PIN) syndrome.
Anatomy
The radial nerve is the end branch of the posterior cord of the brachial plexus. In the proximal part of the arm it follows the brachial artery, while more distally the nerve courses more laterally. Along with a deep artery of the arm which branches off the brachial artery, the radial nerve runs on the posterior aspect of the middle one third of the humerus, within the radial groove. Subsequently it runs obliquely between the superolateral border of medial and lateral heads of the triceps muscle. Approximately 10–12 cm above the elbow joint, the radial nerve pierces the lateral intermuscular septum to appear on the lateral aspect of the brachioradialis muscle and the medial aspect of the brachialis muscle. When following the deep aspect of the brachioradialis muscle and the extensor carpi radialis longus, it divides into deep and superficial branches(20). Further along, the deep branch of the radial nerve runs within the radial nerve tunnel – the space between the humeroradial joint and the distal end of the supinator muscle(20), anterior to the humeroradial joint beneath the extensor carpi radialis brevis muscle – to pass between the supinator's muscle fibers, separating it into superficial and deep parts (fig. 7).
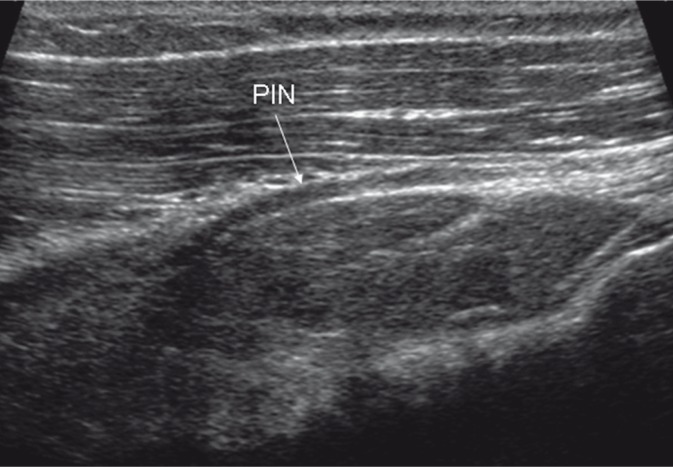
Fig. 7.
Deep branch of radial nerve around the supinator muscle, between its superficial and deep parts
After piercing the supinator muscle and leaving the radial nerve tunnel, the deep branch of the radial nerve, at this point referred to as the posterior interosseous nerve, moves laterally to the posterior extensor compartment, where it gives off further branches(21).
The deep branch of the radial nerve and the posterior interosseous nerve innervate the muscles of the lateral compartment of the forearm (the supinator, extensor carpi radialis brevis muscles), the superficial layer of the posterior compartment of the forearm (the extensor digitorum, extensor digiti minimi, and the extensor carpi ulnaris muscles) and the deep layer of the posterior compartment of the forearm (the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and the extensor indicis muscles).
Pathoanatomy
There are five potential areas within the radial tunnel where the deep branch of the radial nerve may be compressed(22):
the fibrous band of tissue anterior to the humeroradial joint capsule, between the brachioradialis and brachialis muscles;
the radial recurrent vessels, called leash of Henry, which surround the deep nervous branch at the level of radius neck;
the fibrous medial border of the extensor carpi radialis brevis muscle;
the fibrous proximal border of the superficial head of the supinator muscle, called the arcade of Frohse;
The arcade of Frohse constitutes the most common site of impingement of the deep branch of the radial nerve. This structure is formed by a fibrous border of the most proximal part of the superficial head of the supinator, and occurs in 30% of adults(23). Since this structure has not been seen in mature fetuses, it is thought to develop from repeated rotation movements of a forearm(23, 24). Such repetitive movements may cause fibrous remodelling of the border of the extensor carpi radialis brevis, which covers the nerve from the anterior aspect, as well as the ligamentous arch on the distal border of the supinator muscle, resulting in compression of the deep branch of the radial nerve(6, 21, 22).
Other causes for the pathology of the deep branch of the radial nerve and the posterior interosseous nerve should be kept in mind. These include systemic diseases, such as diabetes, rheumatoid arthritis, vasculitis, muscle atrophy, neurovascular diseases(2, 20), benign tumors, such as gangliomas and adipomas as well as displaced bones and scarring after fractures of the head and neck of the radius(20, 23).
Temporary palsy of the posterior interosseous nerve may occur due to the nerve being compressed by the head of persons in deep sleep, a so-called “Saturday night palsy”.
Clinical symptoms
The main clinical manifestation of a neuropathy of the deep branch of the radial nerve, called the radial tunnel syndrome, includes the pain over the point of compression. The paralysis of the muscles innervated by the nerve occurs rather exceptionally. Extension of the fingers in the metacarpophalangeal joints is impaired, as well as the extension and abduction of the thumb. Also during extension of the wrist, the hand deviates laterally.
This syndrome does not cause hand drop since the function of the extensor carpi radialis longus is intact, as this muscle is innervated by branches of the radial nerve proximal to its division into end branches.
Diagnosis
The ultrasonography can be a valuable and non-invasive tool to examine patients with clinical signs and symptoms of compression of the deep branch of the radial nerve(6). Due to similar clinical manifestations of radial tunnel syndrome, radiculopathy or brachial plexus neuropathy(2–4, 6, 20), patients often undergo MR imaging of the cervical spine and brachial plexus as well as physiotherapy(20). The persistence of symptoms after physiotherapy should prompt a search for pathologies in the upper limb(20).
The deep branch of the radial nerve and its end branch – the posterior interosseous nerve, contain purely motor fibers. In case of compression, some abnormalities occur in nerve conductivity with slowing of and decrease in amplitude of the muscle potentials(25).
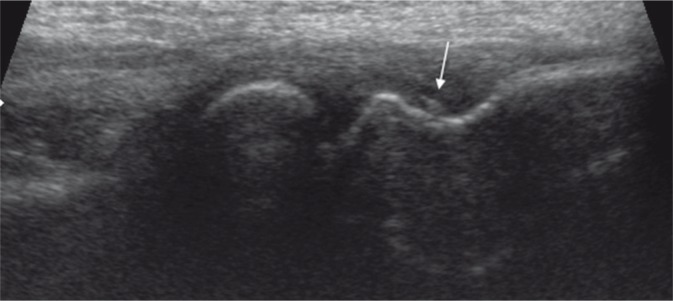
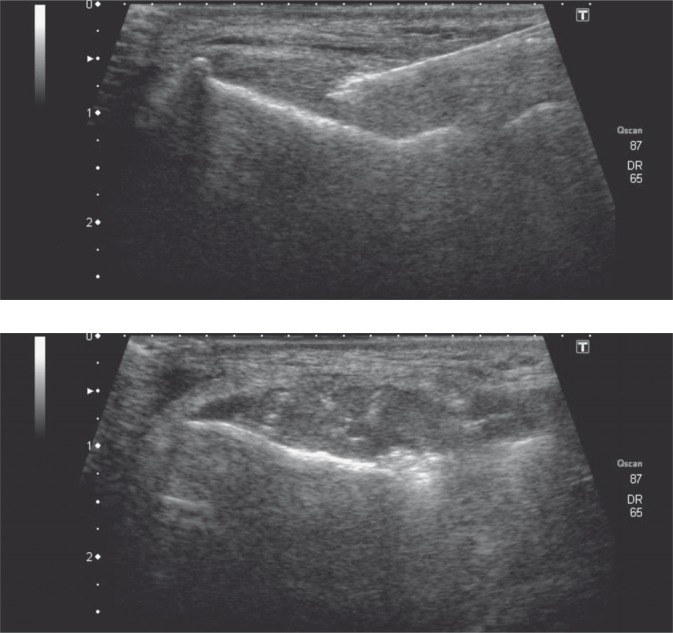
If no conductivity abnormalities are found, the ultrasonographic examination should be used in the diagnostic process, as this technique can show abnormalities within the radial nerve tunnel. A proper US examination of the deep branch of the radial nerve requires the state-of-the-art equipment with a linear probe of a frequency above 12 MHz. The examiner must have a background knowledge of the region's crossectional anatomy. By applying the probe to longitudinal and transverse sections, it is possible to evaluate precisely the nerve cross-section, its outline and internal structure. The examination should start at the level of the radial nerve's division, then the deep branch of the radial nerve should be followed, so as to visualize the nerve within the radial nerve tunnel. An irregular outline, decreased echogenicity, a spindle-shaped focal thickening of the nerve indicate its edema or a neuroma (fig. 8).
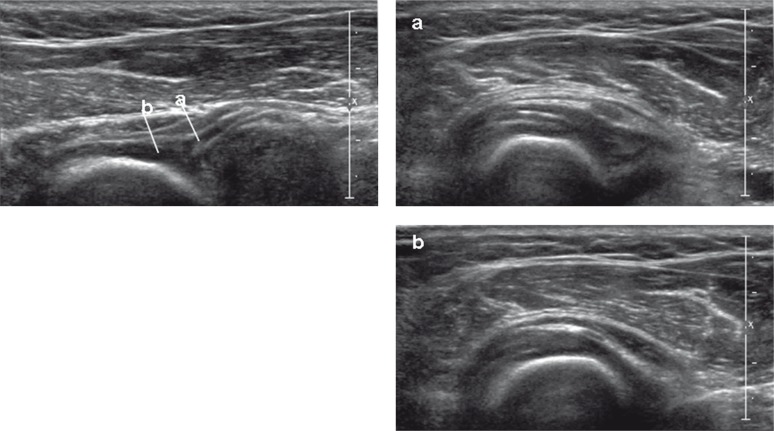
Fig. 8.
Deep branch of radial nerve in the region of the supinator muscle, with evidence of thickening in its middle segment (a), whereas the nerve's distal segment has no abnormalities (b)
All the structures surrounding the deep branch of the radial nerve should be evaluated for the presence of masses and potential functional conflicts or impingement. A quite useful option is the use of ultrasonographic imaging during movement. In visualizing the arcade of Frohse, the structure and shape of the deep branch of the radial nerve is evaluated with the forearm slightly bent during supination against resistance. In case of compression at the level of the arcade, the nerve may be thickened (edematous, scarred) proximal to the arcade of Frohse, and may become wrinkled proximal to the point of compression in the course of supination against resistance(26).
The radial recurrent artery comes off the radial artery at the level of the supinator muscle, around the area of the deep branch of the radial nerve, between the brachioradialis and brachilis muscles. It anastomoses with the deep radial artery that accompanies the radial nerve. When the so-called leash of Henry is present, the power Doppler examination can show arterial vessels crossing the deep branch of the radial nerve. A nerve that is persistently irritated by such a blood vessel loop may demonstrate similar structural changes as in the case of other conflict syndromes.
Treatment
In case of no clinical improvement within 3 months, spontaneous resolution of symptoms is unlikely, and surgical intervention should be considered, as it has better results than conservative treatment(20, 25). Surgical decompression of the nerve prevents fibrous muscle atrophy, which is very likely when clinical symptoms persist for more than 18 months(27).
If the imaging studies fail to locate lesions responsible for compression, such as ganglions, adipomas, scars, synovitis with distention of the joint cavity, and symptoms persist after 3 months, an incision should be made on supinator muscle along with the arcade of Frohse(20, 25) (fig. 9).
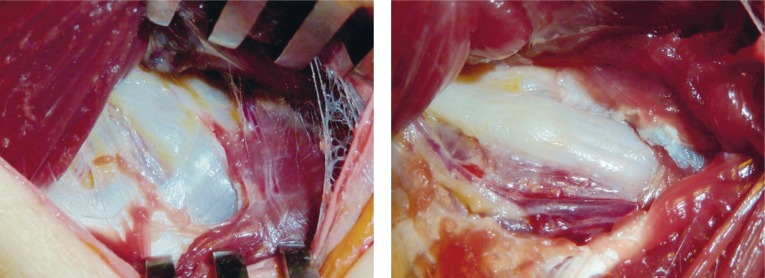
Fig. 9.
Intraoperative picture of a thickened posterior interosseous nerve
In the majority of patients after such decompression, a complete remission of symptoms is observed. In case of elderly or post-op patients whose proper muscle function does not return after 18 months, a tendon transfer procedure is recommended(20). In case of prolonged compression with permanent palsy of the deep branch of the radial nerve, the same surgical procedures are carried out as in proximal injury to the radial nerve, aside from reconstructing wrist extension. It is suggested to restore the extension and abduction of the thumb by transplanting the palmaris longus tendon, to strengthen wrist extension by transferring the pronator teres muscle to the extensor carpi radialis brevis and longus, as well as to transfer the tendon of the flexor carpi ulnaris onto the common extensor digitorum muscle(27). In the recent years, particularly with the introduction of robotic microsurgery technology such as Da Vinci surgical apparatus, methods for transferring peripheral nerves have been developed. To this end, additional motor branches of the main trunks are used, to be sutured end-to-end or end-to-side with the injured peripheral motor nerves. It is possible to regain control of motor function in the injured regions thanks to brain plasticity. This is a more subtle and physiological method when compared to traditional tendon transfers. If there is injury to the posterior interosseous nerve, it is recommended to transfer one motor branch of the flexor digitorum superficialis, flexor carpi radialis or the palmaris longus(28).
References
- 1.Walz DM, Newman JS, Konin GP, Ross G. Epicondylitis: pathogenesis, imaging, and treatment. RadioGraphics. 2010;30:167–184. doi: 10.1148/rg.301095078. [DOI] [PubMed] [Google Scholar]
- 2.Umehara F, Yoshino S, Arimura Y, Fukuoka T, Arimura K, Osame M. Posterior interosseous nerve syndrome with hourglass-like fascicular constriction of the nerve. J Neurol Sci. 2003;15:111–113. doi: 10.1016/s0022-510x(03)00164-3. [DOI] [PubMed] [Google Scholar]
- 3.Ebraheim NA, Jin F, Pulisetti D, Yeasting RA. Quantitative anatomical study of the posterior interosseous nerve. Am J Orthop. 2000;29:702–704. [PubMed] [Google Scholar]
- 4.Fuss FK, Wurzl GH. Radial nerve entrapment at the elbow: surgical anatomy. J Hand Surg [Am] 1991;16:742–747. doi: 10.1016/0363-5023(91)90205-p. [DOI] [PubMed] [Google Scholar]
- 5.Bianchi S, Martinoli C. Ultrasound of the Musculoskeletal System. Berlin, Heidelberg: Springer-Verlag; 2007. pp. 349–405. [Google Scholar]
- 6.Connell D, Burke F, Coombes P, McNealy S, Freeman D, Pryde D, et al. Sonographic examination of lateral epicondilitis. Am J Roentgenol. 2001;176:777–782. doi: 10.2214/ajr.176.3.1760777. [DOI] [PubMed] [Google Scholar]
- 7.Cohen MS, Romeo AA, Hennigan SP, Gordon M. Lateral epicondilitis: anatomic relationship of the extensor tendon origins and implications for arthroscopic treatment. J Should Elbow Surg. 2008;17:954–960. doi: 10.1016/j.jse.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Bunata RE, Brown DS, Sapelo R. Anatomic factors related to the cause of tennis elbow. J Bone Joint Surg Am. 2007;89:1955–1963. doi: 10.2106/JBJS.F.00727. [DOI] [PubMed] [Google Scholar]
- 9.Nirschl RP, Pettrone FA. Lateral and medial epicondilitis. In: Morrey BF, editor. Master Techniques in Orthopedic Surgery: The Elbow. New York: Raven; 1994. pp. 537–552. [Google Scholar]
- 10.Bernard FM, Regan WD. Elbow and forearm. In: DeLee JC, editor. DeLee and Drez's Orthopaedic Sports Medicine. Wyd. 2. Philadelphia, PA: Saunders; 2003. [Google Scholar]
- 11.Faro F, Wolf JM. Lateral epicondilitis: review and current concepts. J Hand Surg Am. 2007;32:1271–1279. doi: 10.1016/j.jhsa.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 12.Connell DA, Ali KE, Ahmad M, Lambert S, Corbett S, Curtis M. Ultrasoud-guided autologous blood injection for tennis elbow. Skeletal Radiol. 2006;35:371–377. doi: 10.1007/s00256-006-0081-9. [DOI] [PubMed] [Google Scholar]
- 13.Nirsch RP, Pettrone FA. Tennis elbow: the surgical treatment of lateral epicondilitis. J Bone Joint Surg Am. 1979;61:832–839. [PubMed] [Google Scholar]
- 14.Ferdinand BD, Rosenberg ZS, Schwaitzer ME, Stuchin SA, Jazrawi LM, Lenzo SR, et al. MR imaging features of radial tunnel syndrome: initial experience. Radiology. 2006;240:161–168. doi: 10.1148/radiol.2401050028. [DOI] [PubMed] [Google Scholar]
- 15.Blease S, Stoller DW, Safran MR, Li AE, Fritz RC. The elbow. In: Stroller DW, editor. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine. Wyd. 3. Philadelphia, Pa: Lippincott, Williams & Wilkins; 2007. pp. 1463–1626. [Google Scholar]
- 16.Noh KH, Moon YL, Jacir AM, Kim KH, Gorthi V. Sonographic probe induced tenderness for lateral epicondylitis: an accurate technique to confirm the location of the lesion. Knee Surg Sports Traumatol Artrosc. 2010;18:836–839. doi: 10.1007/s00167-009-1037-0. [DOI] [PubMed] [Google Scholar]
- 17.Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34:1774–1778. doi: 10.1177/0363546506288850. [DOI] [PubMed] [Google Scholar]
- 18.Byung-Ki C, Yong-Min K, Dong-Soo K, Eui-Sung C, Hyun-Chul S, Kyoung-Jin P, et al. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg. 2009;1:123–127. doi: 10.4055/cios.2009.1.3.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36:261–266. doi: 10.1177/0363546507308932. [DOI] [PubMed] [Google Scholar]
- 20.Thomas SJ, Yakin DE, Parry BR, Lubahn JD. The anatomical relationship between the posterior interosseus nerve and the supinator muscle. J Hand Surg [Am] 2000;25:936–941. doi: 10.1053/jhsu.2000.16360. [DOI] [PubMed] [Google Scholar]
- 21.Dang AC, Rodner CM. Unusual compression neuropathies of the forearm, Part I: Radial nerve. JHS. 2009;34A:1906–1914. doi: 10.1016/j.jhsa.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg. 1968;50B:809–812. [PubMed] [Google Scholar]
- 23.Omura T, Nagano A, Murata H, Takahashi M, Ogihara K. Simultaneous anterior and posterior interosseous nerve paralysis with several hourglass-like fascicular constrictions in both nerves. J Hand Surg [Am] 2001;26:1088–1092. doi: 10.1053/jhsu.2001.27766. [DOI] [PubMed] [Google Scholar]
- 24.Chien AJ, Jamadar DA, Jacobson JA, Hayes CW, Louis DS. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. AJR Am J Roentgenol. 2003;181:219–221. doi: 10.2214/ajr.181.1.1810219. [DOI] [PubMed] [Google Scholar]
- 25.Bodner G, Harpf C, Meirer R, Gardetto A, Kovacs P, Gruber H. Ultrasonographic appearance of supinator syndrome. J Ultrasound Med. 2002;21:1289–1293. doi: 10.7863/jum.2002.21.11.1289. [DOI] [PubMed] [Google Scholar]
- 26.Spinner M. Injuries to the Major Branches of Peripheral Nerves of the Forearm. Wyd. 2. Philadelhia: WB Saunders; 1978. p. 234. [Google Scholar]
- 27.Kevin CC. Hand and wrist surgery. 2008;1:400–410. [Google Scholar]
- 28.Weber RV, Mackinnon SE. Upper extremity nerve transfers. In: Slutsky DJ, Hentz VR, editors. Peripheral Nerve Surgery – Practical Application in the Upper Extremity. Philadelphia: Elsevier; 2006. pp. 89–109. [Google Scholar]