Abstract
Background
Concerns have been raised that the 2013 atherosclerotic cardiovascular disease (ASCVD) risk estimator overpredicts risk in contemporary cohorts. Whether suboptimal calibration will lead to overtreatment with statins is unknown. We investigated the numbers of people eligible for statin treatment in the Framingham Heart Study Offspring Cohort, based on the 2013 cholesterol guidelines, and estimated the proportion that may be overtreated as a result of potential miscalibration of the ASCVD estimator.
Methods and Results
During a median follow‐up of 10 years, we observed 285 ASCVD events (8.4%; comprising ischemic stroke, myocardial infarction, and coronary artery disease death) among 3396 men and 112 events (2.9%) among 3838 women. Hosmer–Lemeshow chi‐square statistics were 16.3 in men (340 predicted versus 285 observed events) and 29.1 in women (166 predicted versus 112 observed events). Overprediction predominantly occurred among women in the highest risk decile and among men in the ≥7th risk deciles, for which observed ASCVD event rates were ≥7.5%. In total, 2615 participants (36%; 867 women) were eligible for statins based on the new guidelines. Of these, 171 women (20%) and 154 men (9%) were reclassified downward (as not eligible for statin therapy) using a recalibrated ASCVD estimator. In the latter group, 18 women (10.5%; 95% CI 5.9% to 15.2%) and 11 men (7.1%; 95% CI 3.0% to 11.3%) experienced ASCVD.
Conclusions
The risk estimator overpredicted ASCVD risk but did so mainly among high‐risk participants who would be considered eligible for statin use anyway. Our findings may mitigate concerns regarding the potential impact of miscalibration of the ASCVD estimator in contemporary cohorts.
Keywords: primary prevention, risk prediction, statin
Introduction
Although the 2013 American College of Cardiology/American Heart Association (ACC/AHA) cholesterol guidelines for primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been well received by the medical community, there is an ongoing debate about who should be classified as eligible for statin treatment in the general population.1–3 Concerns have been raised about the validity of the Pooled Cohort Equations cardiovascular risk estimator, which forms the basis of further patient–physician discussions about statin treatment, because some recent observations have noted much higher predicted ASCVD risk (relative to observed ASCVD risk) when used in contemporary cohorts.4–6
The new ASCVD risk estimator, which is used as an initial screening tool to identify people who may benefit from statin therapy in a primary prevention setting (ie, those with an estimated 10‐year risk of ASCVD ≥7.5% and circulating low‐density lipoprotein cholesterol [LDL‐C] ≥70 mg/dL), was developed using data from several prospective US cohorts collected mainly in the “prestatin” era.7 The working group behind the risk calculator acknowledged that the risk score was not optimally calibrated for sex and for most ethnic groups (with the exception of black women) in more recent external validation cohorts.8 Ridker and Cook later underscored the potential hazard of overpredicting ASCVD risk by showing discrepancies in predicted versus observed risks in the Women's Health Study, the Physicians' Health Study, and the Women's Health Initiative observational study.5 A much higher predicted than observed ASCVD risk was also demonstrated in a European cohort, the Rotterdam Study.9 Data on these contemporary cohorts were collected in the “statin era,” whereas the data on cohorts used for deriving the ASCVD risk score came largely from the prestatin era, in part by choice, because incident statin use throughout follow‐up might confound the observed ASCVD risks in more recent cohorts.2 These observations, however, also raise the possibility that observed ASCVD rates may be lower in contemporary cohorts than in cohorts collected in the prestatin era and thus that the ASCVD estimator might be miscalibrated for use in statin era populations.2,4
Pencina et al recently estimated that the number of people eligible for statins under the new cholesterol guidelines compared with the old guidelines (ATP III)10 increased by 56 million in the United States.11 This number, however, assumed that the risk estimator was well calibrated for the population to which it was applied, namely, that the predicted risk reflected the true (observed) risk in patients. If the new ASCVD risk estimator systematically overestimates risk, some people may be misclassified as eligible for discussing initiation of statin treatment with their health care provider. This will occur for people with a true 10‐year cardiovascular disease risk of <7.5% but a predicted risk of ≥7.5% (ie, the cutoff point used to determine eligibility for discussions regarding statin initiation with doctors according to the new guidelines). An analysis of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study confirmed that the new risk calculator was suboptimally calibrated in the overall study population, yet when the analyses were restricted to a subgroup with cardiovascular disease risk ≥7.5%, the ASCVD score was reasonably well calibrated.12
Taken together, the proportion of people (if any) that may be inappropriately classified as eligible for statin therapy by the new ASCVD risk calculator remains to be firmly established. In the present investigation, we assessed the potential contribution of miscalibration of the new ASCVD risk estimator to the number of people eligible for statins (or for discussion regarding statin initiation) in a primary prevention setting using a sample from the Framingham Heart Study Offspring Cohort. In addition, we sought to address the impact of incident use of lipid‐lowering medications during follow‐up on the observed risks in a sample using data collected during the statin era because it has been hypothesized that statin use contributes to the lower observed than predicted risks in modern cohorts.4
Methods
Sample, Follow‐up, and Definition of End Points
We used a pooled sample of participants from the Framingham Heart Study Offspring Cohort attending examination cycles 1 (1971–1975), 3 (1983–1987), and/or 6 (1995–1998).13 During the initial 2 time periods, statins were not available for prescription, and during the third time period, statins became more routinely available. We restricted the sample to participants who were aged 40 to 75 years at examination (n=8358). We excluded people with prevalent myocardial infarction or stroke (recognized or silent; n=324) and those with missing values of blood pressure, treatment for hypertension, cholesterol values, diabetes, and smoking (n=436); these participants had more adverse risk profiles compared with the final study sample (Table 1) but a nonsignificant difference in incidence of ASCVD (7% versus 5%, P=0.21). We also excluded people treated with lipid‐lowering medications at baseline (n=364, corresponding to 5% of the source sample). All participants provided written informed consent, and the study protocol was approved by the institutional ethics review board at the Boston University Medical Center.
Table 1.
Comparison of Characteristics Between Final Study Sample and Those Excluded for Missing Covariates
| Sample (n=7234) | Excluded for Missing Covariates (n=436) | Numbers With Available Covariates Among Those Excluded | P Value | |
|---|---|---|---|---|
| Age, y | 53 (9) | 53 (9) | 436 | 0.83 |
| Male, sex, n (%) | 3396 (47) | 205 (47) | 436 | 0.98 |
| Systolic blood pressure, mm Hg | 127 (18) | 131 (19) | 433 | <0.0001 |
| Diastolic blood pressure, mm Hg | 79 (10) | 81 (11) | 432 | 0.0001 |
| Treatment for hypertension, n (%) | 1212 (17) | 86 (21) | 413 | 0.03 |
| Total cholesterol, mg/dL | 212 (39) | 246 (71) | 277 | <0.0001 |
| HDL‐C, mg/dL | 52 (16) | 41 (16) | 251 | <0.0001 |
| LDL‐C, mg/dL | 136 (36) | 147 (46) | 109 | 0.02 |
| Triglycerides, mg/dL | 118 (66) | 419 (488) | 276 | <0.0001 |
| Diabetes, n (%) | 358 (5) | 53 (25) | 209 | <0.0001 |
| Current smokers, n (%) | 1928 (27) | 147 (35) | 422 | 0.0002 |
| Incident ASCVD events, n (%) | 396 (5) | 30 (7) | 436 | 0.21 |
Values are presented as mean (standard deviation) except as noted. ASCVD indicates atherosclerotic cardiovascular disease; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol.
We followed participants up to 10 years for new‐onset ASCVD, defined as incident myocardial infarction, nonfatal or fatal ischemic stroke (excluding transient ischemic attack), or death due to coronary artery disease, corresponding to the events used to develop the ASCVD calculator. The process for adjudicating ASCVD outcomes at the Framingham Heart Study has been described in detail.14 In brief, all participants are under continuous surveillance for the development of possible ASCVD events, which are documented by a review of hospitalization records and physician office visits, by communication with personal physicians, and by medical history and physical examinations conducted during periodic visits to the Framingham Heart Study clinic. An adjudication panel comprising 3 experienced physician investigators evaluates all possible ASCVD events by reviewing medical records and electrocardiograms. The adjudication of cerebrovascular events is accomplished by a special review committee that includes at least 1 neurologist. Use of medications, including lipid‐lowering agents, was updated at each Framingham Heart Study examination visit (taking place approximately every fourth year), based on medications participants brought with them and/or for which participants self‐reported use.
Statistical Methods
In accordance with the current ACC/AHA guidelines,3 we classified participants as eligible for statin therapy if they met the following criteria: They had blood LDL‐C concentration ≥70 mg/dL plus either 10‐year ASCVD risk of ≥7.5% or diabetes or they had LDL‐C levels ≥190 mg/dL regardless of other risk factors.7 To compare the numbers of people eligible for statins under old versus new cholesterol guidelines, we also used the ATP III risk estimator to calculate the 10‐year risk of myocardial infarction or coronary heart disease death (ie, coronary heart disease risk; http://cvdrisk.nhlbi.nih.gov/calculator.asp). The ATP III guidelines recommend that statin treatment should be considered if coronary heart disease risk is >20% plus blood LDL‐C concentration ≥100 mg/dL, if coronary heart disease risk is ≤20% plus ≥2 risk factors plus LDL‐C ≥100 mg/dL, or if a person has 0 to 1 risk factors plus LDL‐C ≥160 mg/dL. We estimated the proportion of persons eligible for statin therapy according to the new but not the old (ATP III) guidelines (ie, classified upward) and the proportion of persons eligible for statins under the old but not the new guidelines (ie, classified downward).
We evaluated the calibration of the ASCVD risk score using the Hosmer–Lemeshow chi‐square statistic in men and women separately. We estimated cumulative incidence at 10 years using a Kaplan–Meier‐like estimator adjusted for the competing risk of death to assess the cumulative incidence rates for sex‐specific risk deciles. Frequencies of observed events in each stratum were calculated by multiplying the cumulative 10‐year incidence for that stratum by the number of participants included at baseline: observed=sum over I of Ni×(1−St(10)i). In this calculation, S(t) is the Kaplan–Meier‐like estimator. Because we observed a higher predicted than observed risk overall and because the fit and adequacy of the calculator has been questioned, we recalibrated the calculator by correcting the baseline hazard rates for men and women according to the total numbers of observed events based on Kaplan–Meier‐like estimates with censoring for statin treatment (ie, by correcting the overall mean in men and women separately). All analyses were done in SAS version 9.2 (SAS Institute Inc). Two‐sided P values <0.05 were considered statistically significant. The authors had full access to the data and take responsibility for its integrity. All authors read and agreed with the manuscript as written.
Results
A total of 7234 participants (53% women) were included in our analyses. Baseline characteristics for women and men stratified by ASCVD risk deciles are given in Tables 2 and 3. The mean age and the concomitant burden of risk factors increased with higher risk deciles for both sexes. Only 126 participants (2%) had LDL‐C <70 mg/dL.
Table 2.
Baseline Characteristics and Events During Follow‐up of Women in the Study Sample According to Deciles of ASCVD Risk Based on the ACC/AHA Calculator
| Predicted ASCVD Risk Decile | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| n | 383 | 384 | 384 | 384 | 384 | 384 | 384 | 384 | 384 | 383 |
| Age, y | 44 (2) | 46 (4) | 48 (4) | 50 (5) | 51 (5) | 53 (6) | 55 (7) | 57 (7) | 61 (7) | 66 (7) |
| Systolic blood pressure, mm Hg | 110 (11) | 115 (12) | 119 (14) | 120 (15) | 122 (15) | 125 (17) | 126 (16) | 131 (16) | 135 (17) | 146 (20) |
| Diastolic blood pressure, mm Hg | 72 (8) | 75 (8) | 77 (9) | 76 (10) | 76 (9) | 78 (10) | 78 (10) | 78 (10) | 79 (10) | 79 (12) |
| Treatment for hypertension, n (%) | 4 (1) | 11 (3) | 23 (6) | 29 (8) | 35 (9) | 54 (14) | 74 (19) | 72 (19) | 117 (30) | 198 (52) |
| Total cholesterol, mg/dL | 181 (28) | 193 (29) | 203 (33) | 209 (36) | 214 (36) | 217 (39) | 224 (35) | 230 (40) | 236 (42) | 234 (41) |
| HDL‐C, mg/dL | 69 (15) | 63 (15) | 64 (16) | 61 (15) | 59 (15) | 57 (14) | 56 (16) | 54 (15) | 53 (15) | 53 (17) |
| LDL‐C, mg/dL | 100 (24) | 114 (25) | 122 (31) | 129 (33) | 135 (32) | 138 (37) | 143 (33) | 149 (38) | 154 (41) | 151 (38) |
| LDL‐C <70 mg/dL, n (%) | 37 (10) | 15 (4) | 11 (3) | 6 (2) | 2 (0.5) | 8 (2) | 2 (0.5) | 4 (1) | 1 (0.3) | 1 (0.3) |
| Triglycerides, mg/dL | 62 (26) | 79 (36) | 86 (41) | 94 (45) | 99 (48) | 118 (57) | 123 (64) | 131 (62) | 143 (70) | 156 (68) |
| Diabetes, n (%) | 1 (0.3) | 0 | 1 (0.3) | 0 | 0 | 6 (1.6) | 6 (1.6) | 17 (4) | 24 (6) | 83 (22) |
| Current smokers, n (%) | 0 | 11 (3) | 47 (12) | 83 (22) | 120 (31) | 141 (37) | 156 (41) | 164 (43) | 166 (43) | 136 (36) |
| Pooled risk, % mean (minimum to maximum) | 0.3 (0.1 to 0.5) | 0.6 (0.5 to 0.8) | 1.0 (0.8 to 1.2) | 1.4 (1.2 to 1.7) | 2.0 (1.7 to 2.4) | 2.8 (2.4 to 3.3) | 3.8 (3.3 to 4.5) | 5.4 (4.5 to 6.6) | 8.4 (6.6 to 10.7) | 17.3 (10.8 to 47.5) |
| Eligible for statin therapy, n (%) | 1 (0.3) | 0 (0) | 8 (2) | 16 (4) | 25 (7) | 34 (9) | 38 (10) | 68 (18) | 295 (77) | 382 (99.7) |
| Follow‐up | ||||||||||
| Observed risk, % (95% CI) | 0.8 (−0.1 to 1.7) | 1.0 (0.02 to 2.1) | 0.5 (−0.2 to 1.2) | 0.8 (−0.1 to 1.7) | 1.3 (0.2 to 2.4) | 1.6 (0.3 to 2.8) | 1.0 (0.02 to 2.1) | 3.9 (2.0 to 5.9) | 8.1 (5.3 to 10.8) | 10.2 (7.1 to 13.2) |
| New‐onset lipid therapy on follow‐up, n (%) | 5 (1) | 11 (3) | 29 (8) | 25 (7) | 45 (12) | 38 (10) | 61 (14) | 65 (17) | 79 (21) | 94 (25) |
| Censored due to death from non‐ASCVD causes, n (%) | 4 (1) | 2 (0.5) | 5 (1) | 7 (2) | 9 (2) | 17 (4) | 14 (4) | 23 (6) | 17 (4) | 47 (12) |
Data are presented as mean (SD) or numbers (percentages) unless otherwise specified. New‐onset lipid therapy refers to numbers of participants within each group initiating statin therapy. Sample eligible for statin therapy was based on the new risk calculator and 2013 guidelines. ACC/AHA indicates American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol.
Table 3.
Baseline Characteristics and Events During Follow‐up of Men in the Study Sample According to Deciles of ASCVD Risk Based on the ACC/AHA Calculator
| Predicted ASCVD Risk Decile | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| n | 339 | 340 | 340 | 339 | 340 | 340 | 339 | 340 | 340 | 339 |
| Age, y | 44 (3) | 46 (3) | 48 (4) | 50 (5) | 52 (5) | 53 (6) | 55 (6) | 58 (7) | 61 (7) | 66 (7) |
| Systolic blood pressure, mm Hg | 117 (11) | 122 (13) | 123 (13) | 124 (13) | 127 (15) | 128 (15) | 129 (15) | 134 (16) | 138 (17) | 148 (18) |
| Diastolic blood pressure, mm Hg | 77 (8) | 80 (10) | 80 (10) | 82 (9) | 82 (10) | 82 (9) | 82 (10) | 83 (10) | 82 (11) | 83 (11) |
| Treatment for hypertension, n (%) | 8 (2) | 22 (6) | 26 (8) | 36 (11) | 44 (13) | 43 (13) | 57 (17) | 80 (24) | 101 (30) | 178 (53) |
| Total cholesterol, mg/dL | 187 (29) | 203 (34) | 204 (35) | 210 (33) | 217 (35) | 213 (36) | 216 (37) | 219 (38) | 218 (39) | 214 (43) |
| HDL‐C, mg/dL | 53 (12) | 48 (12) | 47 (12) | 46 (12) | 46 (12) | 44 (13) | 42 (12) | 43 (12) | 42 (12) | 41 (11) |
| LDL‐C, mg/dL | 118 (27) | 134 (30) | 134 (32) | 139 (31) | 146 (32) | 144 (35) | 146 (34) | 146 (36) | 147 (38) | 141 (38) |
| LDL‐C <70 mg/dL, n (%) | 6 (2) | 5 (1) | 5 (1) | 3 (1) | 0 (0) | 6 (2) | 4 (1) | 6 (2) | 0 (0) | 4 (1) |
| Triglycerides, mg/dL | 83 (41) | 108 (62) | 115 (63) | 127 (67) | 126 (61) | 124 (63) | 140 (67) | 154 (75) | 152 (74) | 160 (77) |
| Diabetes, n (%) | 1 (0.3) | 2 (0.6) | 5 (1.5) | 5 (1.5) | 2 (0.6) | 14 (4) | 14 (4) | 21 (6) | 42 (12) | 111 (33) |
| Current smokers, n (%) | 7 (2) | 27 (8) | 55 (16) | 87 (26) | 103 (30) | 136 (40) | 132 (39) | 140 (41) | 118 (35) | 99 (29) |
| Pooled risk, % (minimum to maximum) | 1.3 (0.3 to 1.9) | 2.5 (1.9 to 3.0) | 3.6 (3.0 to 4.3) | 5.1 (4.3 to 5.9) | 6.6 (5.9 to 7.4) | 8.3 (7.4 to 9.3) | 10.5 (9.3 to 12.1) | 13.7 (12.1 to 15.6) | 18.0 (15.6 to 21.2) | 30.4 (21.2 to 67.7) |
| Eligible for statin therapy, n (%) | 4 (1) | 12 (4) | 20 (6) | 30 (9) | 31 (9) | 307 (90) | 335 (99) | 334 (98) | 340 (100) | 335 (99) |
| Follow‐up | ||||||||||
| Observed risk, % (95% CI) | 0.6 (−0.2 to 1.4) | 2.6 (0.9 to 4.4) | 3.5 (1.6 to 5.5) | 5.0 (2.7 to 7.3) | 8.5 (5.5 to 11.5) | 6.5 (3.8 to 9.1) | 7.7 (4.8 to 10.5) | 11.5 (8.1 to 14.9) | 14.7 (10.9 to 18.5) | 23.0 (18.5 to 27.5) |
| New‐onset lipid therapy on follow‐up, n (%) | 9 (3) | 17 (5) | 25 (7) | 40 (12) | 42 (12) | 44 (13) | 63 (19) | 50 (15) | 74 (22) | 91 (27) |
| Censored due to death from non‐ASCVD causes, n (%) | 5 (1) | 7 (2) | 6 (2) | 9 (3) | 7 (2) | 16 (5) | 25 (7) | 24 (7) | 38 (11) | 60 (18) |
Data are presented as mean (SD) or numbers (percentages) unless otherwise specified. New‐onset lipid therapy refers to numbers of participants within each group initiating statin therapy. Sample eligible for statin therapy is based on the new risk calculator and 2013 guidelines. ACC/AHA indicates American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol.
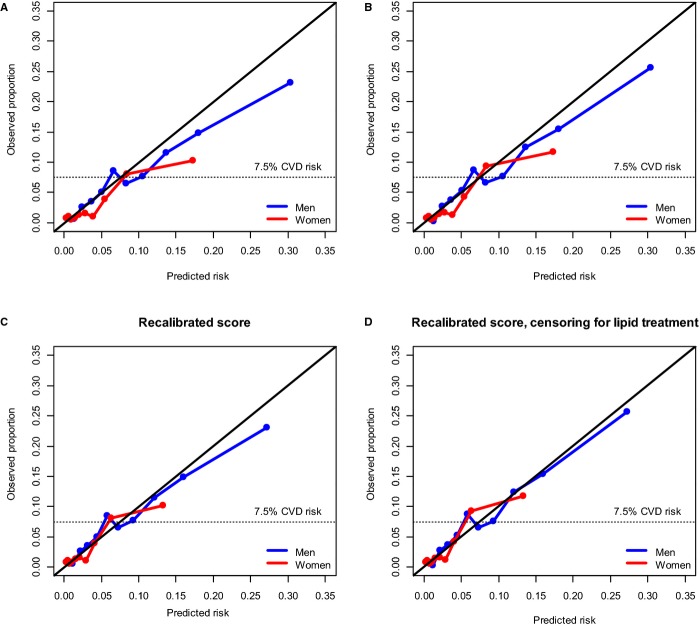
On follow‐up (median duration 10 years), we observed a total of 284 incident ASCVD events (8.4%) in men and 112 events (3%) in women (translating to 285 estimated events among men and 112 events among women after censoring for follow‐up <10 years). The observed number of events was lower than that predicted by the ASCVD risk estimator: Hosmer–Lemeshow chi‐square values were 16.3 for men (340 predicted versus 285 observed events) and 29.1 for women (166 predicted versus 112 observed events). Plots of observed versus predicted risks for women and men (by risk deciles) are displayed in Figure 1A. The greatest discrepancy between predicted versus observed events was seen for women in the top risk decile and for men in the ≥7th risk deciles. The observed 10‐year ASCVD event rates were all ≥7.5% in these groups.
Figure 1.
Plots of observed vs predicted ASCVD risks for the original ACC/AHA calculator and the recalibrated version with and without censoring for lipid treatment during follow‐up. Calibration plots of predicted vs observed events in the original (ie, uncalibrated) risk score and recalibrated risk score without and with censoring for the initiation of lipid‐lowering treatment during follow‐up, by risk deciles. Predicted events refer to probability of having an ASCVD event, and observed events refer to the proportion of people suffering an ASCVD event during follow‐up. ACC/AHA indicates American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease.
Numbers Eligible for Statins Based on New and Old Guidelines
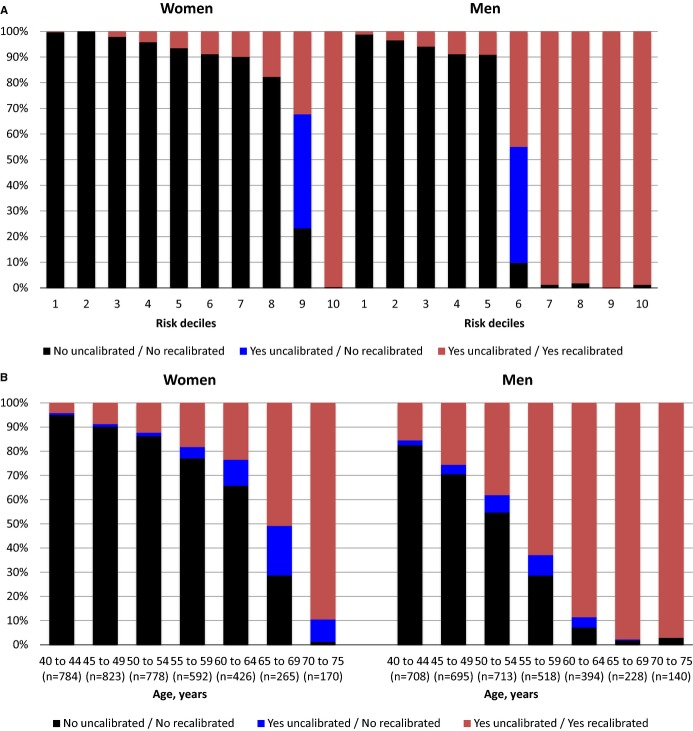
Assessed by the original ASCVD estimator, 2615 participants (36%; 867 women) had estimated ASCVD risks ≥7.5% (or diabetes) and LDL‐C concentrations ≥70 mg/dL and thus were eligible for statins according to the new guidelines. In contrast, only 1737 participants (24%; 544 women) were eligible for statin therapy according to the old ATP III guidelines, translating into a net increase of 878 participants (overall 51% increase; 59% increase in women and 47% increase in men). The discrepancy between number of participants eligible for statins in the new versus old guidelines increased in the higher age groups, exceeding 10% in men aged >50 years and in women aged >60 years (Figure 2). The discordance in statin eligibility between the 2 guidelines was particularly striking in women aged >65 years (Figure 2).
Figure 2.
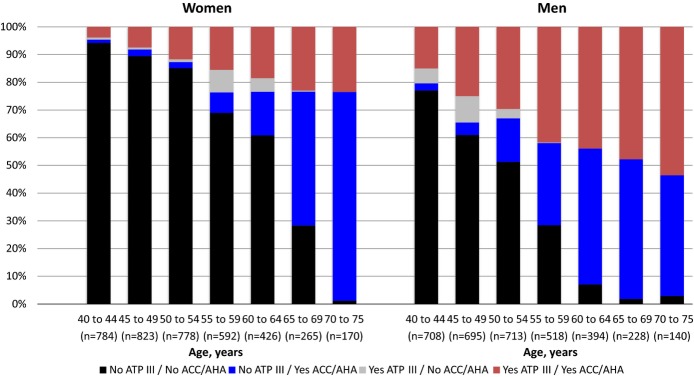
Percentage of people eligible for statins under the new vs old guidelines. Proportion of women and men eligible for statins according to new (ACC/AHA) vs old (ATP III) guidelines by age group. ACC/AHA indicates American College of Cardiology/American Heart Association.
A total of 1518 participants were eligible for discussion of statin therapy according to both guidelines. Of these, 341 (22%) initiated lipid‐lowering medications, and 206 (13.6%; 95% CI 11.8% to 15.3%) had ASCVD events during follow‐up. Among the subgroup eligible for discussion regarding statin initiation according to the new ACC/AHA guidelines but not the old ATP III guidelines (n=1097), 197 (18%) commenced treatment with lipid‐lowering medications, and 88 (8.0%; 95% CI 6.4% to 9.6%) had ASCVD events. There were 219 participants (3%) who were eligible for statins according to the old ATP III guidelines but not according to the new ACC/AHA guidelines. Of these, 37 (18%) initiated treatment with statins during follow‐up, and 13 (5.9%; 95% CI 2.8% to 9.1%) had an ASCVD event.
Importance of Risk Estimator Miscalibration With Regard to Predicted ASCVD Risk and Eligibility for Statins
After recalibrating the risk calculator, Hosmer–Lemeshow chi‐square values were 9.8 (301 events predicted, 285 observed) for men and 17.3 (126 events predicted, 112 observed) for women (Figure 1C). After assessing ASCVD risk with the recalibrated risk estimator instead of the original risk estimator, a total of 171 women (20%) and 154 men (9%) were moved downward, that is, were designated as not eligible for statin therapy from a status of eligible for statin therapy. These people belonged to the 9th risk decile for women and the 6th risk decile for men (Figure 3A) and were distributed among the higher age groups for women and the intermediate age groups for men (Figure 3B). Among the group that moved downward, 33 women (19%) and 22 men (14%) initiated treatment with lipid‐lowering medications during follow‐up, and of these 325 people, 18 women (10.5%; 95% CI 5.9% to 15.2%) and 11 men (7.1%; 95% CI 3.0% to 11.3%) experienced an ASCVD event.
Figure 3.
Eligibility for statins with original and recalibrated risk scores. A, By risk decile. B, By age group. Percentage of participants potentially misclassified as eligible for statin therapy based on atherosclerotic cardiovascular disease risk assessment with original vs recalibrated risk score. Blue solid lines indicate the percentage of people classified as eligible for statins with the uncalibrated risk score only.
Influence of Incident Statin Treatment on Observed Risks
A total of 907 participants (12.5%) initiated treatment with lipid‐lowering medications throughout the observational period (more in the upper risk score categories than in the lower) (Tables 2 and 3). On censoring for initiation of lipid‐lowering treatment, the estimated risks were slightly higher and the calibration of the original risk calculator was slightly improved, with chi‐square values of 13.1 (340 predicted versus 301 observed) among men and 22.8 (166 predicted versus 126 observed) among women (Figure 1B). Using the recalibrated risk estimator and censoring for lipid‐lowering treatment, the predicted and observed numbers of events corresponded well: Chi‐square values were 10.1 (301 predicted versus 301 observed events) for men and 17.7 (126 predicted versus 126 observed events) for women (Figure 1D). The observed risks, however, were higher than the predicted risks for women in the 9th risk decile (36 observed versus 24 predicted; chi‐square value 5.2) and for men in the 5th risk decile (30 observed versus 20 predicted; chi‐square value 4.9) using the recalibrated risk score after censoring for statin treatment.
Discussion
In agreement with previous reports,11 we observed a substantial increase in numbers of persons eligible for statin treatment under the new ACC/AHA guidelines compared with the older ATP III guidelines. In total, 36% of our study population was eligible for statins according to the new cholesterol guidelines, corresponding to a net increase of 51% compared with the old ATP III guidelines. In accordance with previous reports, the new ASCVD risk calculator overpredicted the true risks in our sample.5,9 The greatest discrepancy between the predicted and observed ASCVD event rates, however, was noted for those at the upper end of the estimated ASCVD risk spectrum, for whom the observed event rate exceeded 7.5% anyway, suggesting that such miscalibration would likely not affect treatment decisions regarding statin use.
Using the new risk estimator, Karmali et al recently reported that if age‐adjusted national mean levels of risk factors were used, all non‐Hispanic white men aged >60 years and all women older than 65 or 70 years (for those treated or not treated with antihypertensive medications) would have estimated ASCVD risks ≥7.5%.15 This means that the option of statin therapy should be discussed by physicians with virtually all men aged >60 and women >69 years based on the 2013 cholesterol guidelines (given that LDL‐C is ≥70 mg/dL, which was the case for >98% of our study sample). Whether statin therapy is appropriate for all of these people warrants further investigation (and, ideally, a randomized clinical trial), but estimated from our calibration plots, predicted and observed ASCVD risks were ≥7.5% for most of these people.
When we applied a recalibrated version of the risk calculator (ie, baseline hazard was lowered to fit the observed events), we observed that 20% of women (all in the 9th risk decile) and 9% of men (all in the 6th risk decile) went from being classified as eligible to being not eligible for a discussion regarding statin therapy. The observed ASCVD event rates, however, exceeded the predicted event rates for many of the intermediate‐ and high‐risk groups after recalibration, and this was especially evident on censoring for statin treatment. With the recalibrated risk estimator, women in the 9th risk decile and men in the 5th risk decile had higher observed than predicted risks (observed risks were 8.1% [95% CI 5.3% to 10.8%] for women and 8.5% [95% CI 5.5% to 11.5%] for men) (Tables 2 and 3). These 2 risk deciles were predominantly composed of middle‐aged people (mean age was 61 years in women and 52 years in men) with rather large risk‐factor burdens (eg, high prevalence of smoking, high blood pressure values, and high prevalence of antihypertensive treatment). Unfortunately, our study sample was too small to explore this group in greater detail. Further collaborative efforts pooling other studies may be needed to see if the risk calculator is well calibrated for this segment of the general population or if it could benefit from additional fine tuning (the risk calculator has been criticized for weighting age inappropriately).7 It may be reasonable to consider statin therapy for this intermediate‐risk segment despite the downward classification after recalibration, given that the observed event rates tended to exceed the predicted event rates (and exceeded the 7.5% cutoff point defined by the guidelines) when assessed using the recalibrated risk calculator. Furthermore, other risk measures such as presence of coronary artery calcium may be of additional value when considering optimal treatment strategies for this intermediate‐risk group, although more research is needed to establish the incremental prognostic yield accruing from the use of subclinical disease measures.3,16–17
Although it has been speculated that frequent use of statins in the contemporary time period might have attenuated the observed ASCVD event rates,4 this premise has been investigated previously only in the Women's Health Study.18 In that cohort, statin therapy did not explain the lower observed than expected ASCVD risks with the use of the new calculator.18 It is also possible that the observed low event rates in the Women's Health Study may be explained, to some extent, by the relatively healthier population and higher socioeconomic status among those who volunteered to participate in a randomized clinical trial. We observed in the present study that >20% of those within the upper risk groups initiated treatment with lipid‐lowering medications during follow‐up. On censoring for lipid‐lowering medication use, the ASCVD risk score was better calibrated; this observation suggests that initiation of lipid‐lowering therapy may explain, in part, the lower observed versus predicted ASCVD event rates in some recent cohorts. Based on data from randomized clinical trials, the use of statins reduces ASCVD by ≈20% to 30%,19 which (in agreement with our observations) would not correspond to the whole gap between the observed and predicted event rates unless statin treatment were initiated in everyone in the upper risk spectra during follow‐up. It is also possible that aspirin treatment and coronary revascularizations might have contributed to the lower observed versus predicted ASCVD event rates seen in our and other contemporary cohorts. We decided not to account for these therapies in our estimates because these treatments are an integral part of modern strategies to prevent and treat ASCVD.
Strengths and Limitations
Our sample was not a completely independent external validation sample of the risk estimator because data from some of the participants were included in the derivation of the equation (ie, Offspring Cohort examination cycles 1 and 3). Consequently, the performance of the risk equation in our cohort might be expected to be better than in completely independent external validation cohorts. Moreover, baseline examination for some people was done as early as 1971, which may not be considered modern or contemporary. In contrast, even with this cohort from an older time period, the initiation of statin therapy during follow‐up was high and can challenge accurate risk estimation. Moreover, although we had a sample of 7234 participants, the number of observed ASCVD events was modest; therefore, the confidence intervals of our estimates were rather wide, which precluded the exploratory analysis of selected subgroups. In addition, although we observed that as much as 20% of the women and 9% of the men in our sample were classified as eligible for statins using the uncalibrated ACC/AHA risk score but not so with the recalibrated version, we cannot determine whether these participants truly had an observed ASCVD event rate <7.5% and consequently were inappropriately classified as eligible for statins. Furthermore, our sample included only white people; therefore, it remains to be established whether potential miscalibration of the new pooled risk estimator would have consequences for statin eligibility among other races. Finally, we excluded participants with missing data on covariates (≈6% of the sample). Although incidence of ASCVD was not statistically significantly different between excluded participants and the final study sample (7% versus 5%, P=0.21), it is conceivable that such exclusions may have influenced our estimates of observed ASCVD event rates.
Conclusions
In total, 36% of our study sample was eligible for statins according to the new cholesterol‐lowering guidelines, corresponding to a net increase of 51% in statin eligibility compared with the older ATP III guidelines. The risk calculator overpredicted risks but did so predominantly among people with observed ASCVD risks of ≥7.5%. Intermediate‐risk participants (with predicted ASCVD risks of ≈5% to 8%) may or may not be inaccurately classified as eligible (or not eligible) for statin therapy based on the pooled risk calculator, but this premise warrants further investigation.
Sources of Funding
This study was funded by the National Institute of Health's Heart, Lung and Blood Institute (Contract #N01‐HC‐25195, PI Vasan). Charlotte Andersson was financed by an independent research grant from the Danish Agency for Science, Technology and Innovation (grant number FSS‐11‐120873).
Disclosures
None.
References
- Krumholz HM. The new cholesterol and blood pressure guidelines: perspective on the path forward. JAMA. 2014; 311:1403-1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Agostino RB, Sr, Ansell BJ, Mora S, Krumholz HM. Clinical decisions. The guidelines battle on starting statins. N Engl J Med. 2014; 370:1652-1658. [DOI] [PubMed] [Google Scholar]
- Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Tomaselli GF. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 129:S1-S45. [DOI] [PubMed] [Google Scholar]
- Muntner P, Safford MM, Cushman M, Howard G. Comment on the reports of over‐estimation of ASCVD risk using the 2013 AHA/ACC risk equation. Circulation. 2014; 129:266-267. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013; 382:1762-1765. [DOI] [PubMed] [Google Scholar]
- Raymond C, Cho L, Rocco M, Hazen SL. New cholesterol guidelines: worth the wait? Cleve Clin J Med. 2014; 81:11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff DC, Jr, Lloyd‐Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Tomaselli GF. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:S49-S73. [DOI] [PubMed] [Google Scholar]
- 2013 Report on the assessment of cardiovascular risk: full work group report supplement. Available at: http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assesment.pdf. Accessed March 25, 2015.
- Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, Ikram MA, Stricker BH, Hofman A, Franco OH. Comparison of application of the ACC/AHA guidelines, adult treatment panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014; 311:1416-1423. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004; 110:227-239. [DOI] [PubMed] [Google Scholar]
- Pencina MJ, Navar‐Boggan AM, D'Agostino RB, Sr, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014; 370:1422-1431. [DOI] [PubMed] [Google Scholar]
- Muntner P, Colantonio LD, Cushman M, Goff DC, Jr, Howard G, Howard VJ, Kissela B, Levitan EB, Lloyd‐Jones DM, Safford MM. Validation of the atherosclerotic cardiovascular disease pooled cohort risk equations. JAMA. 2014; 311:1406-1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham Offspring Study. Am J Epidemiol. 1979; 110:281-290. [DOI] [PubMed] [Google Scholar]
- D'Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008; 117:743-753. [DOI] [PubMed] [Google Scholar]
- Karmali KN, Goff DC, Jr, Ning H, Lloyd‐Jones DM. A systematic examination of the 2013 ACC/AHA pooled cohort risk assessment tool for atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2014; 64:959-968. [DOI] [PubMed] [Google Scholar]
- Andersson C, Vasan RS. Is there a role for coronary artery calcium scoring for management of asymptomatic patients at risk for coronary artery disease? Clinical risk scores are sufficient to define primary prevention treatment strategies among asymptomatic patients. Circ Cardiovasc Imaging. 2014; 7:390-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaha MJ, Silverman MG, Budoff MJ. Is there a role for coronary artery calcium scoring for management of asymptomatic patients at risk for coronary artery disease?: clinical risk scores are not sufficient to define primary prevention treatment strategies among asymptomatic patients. Circ Cardiovasc Imaging. 2014; 7:398-408. [DOI] [PubMed] [Google Scholar]
- Cook NR, Ridker PM. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women's Health Study. JAMA Intern Med. 2014; 174:1964-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta‐analysis of individual data from 27 randomised trials. Lancet. 2012; 380:581-590. [DOI] [PMC free article] [PubMed] [Google Scholar]