Abstract
Background
Patients with myocardial infarction (MI) and concomitant chronic obstructive pulmonary disease (COPD) constitute a high‐risk group with increased mortality. β‐Blocker therapy has been shown to reduce mortality, prevent arrhythmias, and delay heart failure development after an MI in broad populations. However, the effect of β‐blockers in COPD patients is less well established and they may also be less treated due to fear of adverse reactions. We investigated β‐blocker prescription at discharge in patients with COPD after MI.
Methods and Results
Patients hospitalized for MI between 2005 and 2010 were identified from the nationwide Swedish SWEDEHEART registry. Patients with COPD who were alive and discharged after an MI were selected as the study population. In this cohort, patients who were discharged with β‐blockers were compared to patients not discharged with β‐blockers. The primary end point was all‐cause mortality. A total of 4858 patients were included, of which 4086 (84.1%) were discharged with a β‐blocker while 772 (15.9%) were not. After adjusting for potential confounders including baseline characteristics, comorbidities, and in‐hospital characteristics, patients discharged with a β‐blocker had lower all‐cause mortality (hazard ratio 0.87, 95% CI 0.78 to 0.98) during the total follow‐up time (maximum 7.2 years). In the subgroup of patients with a history of heart failure, the corresponding hazard ratio was 0.77 (95% CI 0.63 to 0.95).
Conclusions
Patients with COPD discharged with β‐blockers after an MI had a lower all‐cause mortality compared to patients not prescribed β‐blockers. The results indicate that MI patients with COPD may benefit from β‐blockers.
Keywords: epidemiology, mortality, myocardial infarction, prevention
Introduction
β‐Blockers have long been a cornerstone in secondary prevention after a myocardial infarction (MI). The European Society of Cardiology recommends treatment with oral β‐blockers in all acute coronary syndromes with concomitant left ventricular dysfunction and consideration of β‐blockers in all other acute coronary syndrome patients.1–2 β‐Blockers have been proven to reduce mortality, reduce the risk of malignant arrhythmias, and delay heart failure development, although most of the clinical trials proving these benefits stem from before the modern reperfusion era.3–6
Patients with MI and chronic obstructive pulmonary disease (COPD) constitute a high‐risk group.7–9 They often present with atypical symptoms, such as dyspnea, and more often have aggravating comorbidities.9–10 Furthermore, they less often receive reperfusion therapy during hospitalization and are less often treated with standard post‐MI secondary prevention.9,11 These complicating factors might contribute to the high mortality seen after MI for COPD patients.9
Historically, β‐blockers have sometimes been withheld from COPD patients.12 There has been a fear that β‐blockers would induce respiratory adverse reactions such as bronchospasm, but cardioselective β‐blockers have been proven safe in meta‐analyses.13–14 Furthermore, several studies including a meta‐analysis of observational studies involving COPD and β‐blocker treatment found a protective effect on all‐cause mortality,15–16 and a previous study showed a lower rate of COPD exacerbations, suggesting dual cardiopulmonary protective properties.17 However, the established benefit of β‐blockers as secondary prevention post‐MI has not been studied extensively in patients with COPD, although a recent observational study from the United Kingdom seems to suggest benefit in these patients.18
In this study, we aimed to study the association between prescription of β‐blockers at discharge after MI and all‐cause mortality for COPD patients in the present era of interventional cardiology and dual antiplatelet therapy in Sweden.
Materials and Methods
Registries
Consecutive MI patients admitted to Swedish coronary care units and entered in the nationwide Swedish Web‐system for Enhancement and Development of Evidence‐based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART)19 registry were available for analyses. The SWEDEHEART registry enrolls consecutive patients admitted to a Swedish coronary care unit because of symptoms suggestive of an acute coronary syndrome. On admission, patients receive written information about SWEDEHEART and other quality‐of‐care registries; patients are permitted to deny participation in the registry, although few of them exercise this right. According to Swedish law, written consent is not required because quality control is an inherent element of hospital health care. An institutional ethics committee approved this study. Information was collected prospectively regarding baseline characteristics such as age and smoking status as well as electrocardiographic findings, examinations, interventions, in‐hospital complications, diagnoses, and discharge medications such as β‐blockers.19 Information on time of death was obtained from the Swedish National Cause of Death Registry. Information regarding previous medical history, including previous COPD diagnoses and other comorbidities, were obtained from the Swedish National Patient Registry20 that includes diagnoses based on International Classification of Diseases (ICD) codes for all patients hospitalized in Sweden from 1987 and onward. Since 2001 the specialized outpatient care has also been included. All of the information from the different registries was merged into a single database for analysis.
MI and COPD Definitions
An MI diagnosis in the SWEDEHEART registry is a clinical diagnosis made by the patient's treating physician based on patient history, laboratory values, electrocardiographic findings, angiography, and other examinations based on current definitions of MI.21 For a COPD diagnosis, we used J41 to J44 from ICD‐10 and 491 to 492, 496 from ICD‐9, not including Asthma. This definition has previously been validated22 with a misclassification of <10% in the Swedish National Patient Registry.
Study Sample
MI patients, both ST‐segment elevation myocardial infarction (STEMI) and non‐STEMI, enrolled in the SWEDEHEART registry between 2005 and 2010 with a concurrent COPD diagnosis were included in the study. COPD was defined as having an electronic healthcare record of ICD codes either at baseline or during follow‐up. The rationale for also including patients diagnosed during follow‐up was that since COPD is an underdiagnosed disease and often diagnosed in a late stage that takes many years to reach, patients diagnosed during follow‐up would have undiagnosed COPD at the time of the MI. A similar approach has been adopted previously.18 Since the study aimed to investigate the effect of β‐blockers for secondary prevention, all patients who died in the hospital were excluded (341/6476, 5.3%). Missing information on whether the patient was being discharged with β‐blocker or not led to exclusion from the study (n=16). Patients with relative or absolute contraindications (discharged with digoxin [n=355], bradycardia [n=566], AV block II or III [n=65], hypotension [n=232], and cardiogenic shock [n=43]) to β‐blockers were excluded.
End point
The primary analysis tested the relationship between the exposure of being discharged with a β‐blocker and the predefined primary end point of all‐cause mortality at 30 days, at 1 year, and during the total available follow‐up time after the initial coronary care unit hospitalization.
Statistical Analyses
Differences between normally distributed continuous variables were evaluated using the Student t test. Differences between non‐normally distributed continuous variables were evaluated using the Mann–Whitney U test. Differences between categorical variables were tested with the Pearson χ2 test. Rates of the end point in patients with and without a β‐blocker were calculated with the Kaplan–Meier estimator. Univariate and multivariate hazard ratios were estimated using Cox proportional hazard models. Covariates were tested for proportionality of hazards by visual inspection. Potential confounders were identified using an a priori direct acyclic graph23 via a web‐based tool (http://www.dagitty.net). The multivariate model included the following covariates: age, sex, smoking status, comorbidities (previous MI, previous stroke, heart failure, renal failure, hypertension, diabetes, and cancer), in‐hospital characteristics (STEMI, angiography, coronary stenting), β‐blocker therapy at presentation, COPD medication at presentation, and discharge medications (angiotensin‐converting enzyme inhibitors, angiotensin‐II receptor blockers, aspirin, clopidogrel, statins, calcium channel blockers, and diuretics). To crosscheck the results data from different angles, several sensitivity analyses were conducted. A second adjustment method using a propensity score as a continuous covariate in a Cox proportional hazard model was tested to ascertain whether a different adjustment model would impact the result differently. The propensity score was calculated using a logistic regression model, and using the direct acyclic graph, the following covariates were identified as dependent determinants for the exposure of being discharged with β‐blockers: age, sex, smoking status, previous stroke, previous MI, heart failure, diabetes, hypertension, renal failure, cancer, β‐blockers therapy at presentation, STEMI, coronary angiography, coronary stenting, and COPD medications at presentation. All tests were 2‐sided with a P‐value for significance of <0.05. All analyses were performed in SPSS (SPSS version 20, IBM SPSS statistics).
Results
Patient Characteristics
Out of 62 855 MI hospital survivors with complete data on β‐blocker treatment at discharge and exclusion criteria applied, 4858 (7.7%) COPD patients were identified. Out of these 4858 patients, 4086 (84.1%) were discharged with a β‐blocker while 772 (15.9%) were not. Baseline characteristics are outlined in Table 1, both in patients with and without COPD for comparison. Patients with COPD were more often discharged without β‐blockers (15.9 versus 9.6%, P<0.001) compared to patients without COPD.
Table 1.
Baseline Characteristics of Consecutive MI Hospital Survivors With COPD (4858) and Without COPD (57 997) in Sweden Between 2005 and 2010
| Characteristic | Patients With COPD | Patients Without COPD | ||||
|---|---|---|---|---|---|---|
| No β‐Blocker | β‐Blocker | P Value | No β‐Blocker | β‐Blocker | P Value | |
| n=772 | n=4086 | n=5548 | n=52 449 | |||
| Age | 77 (69 to 83) | 74 (67 to 80) | <0.001 | 75 (64 to 83) | 70 (60 to 79) | <0.001 |
| Body mass index | 24.3 (21.1 to 27.7) | 25.1 (22.3 to 28.7) | <0.001 | 25.7 (23.4 to 28.4) | 26.3 (24.1 to 29.2) | <0.001 |
| Female sex | 390 (50.5) | 1785 (43.7) | 0.004 | 2269 (40.9) | 18 059 (34.4) | <0.001 |
| Smoker | 234 (33.5) | 1521 (39.6) | <0.001 | 939 (19.2) | 11 674 (24.0) | <0.001 |
| Comorbidities | ||||||
| Previous stroke | 157 (20.3) | 612 (15.0) | 0.001 | 747 (13.5) | 5223 (10.0) | <0.001 |
| Previous MI | 156 (20.2) | 810 (19.8) | 0.908 | 739 (13.3) | 6039 (11.5) | <0.001 |
| Heart failure | 204 (26.4) | 814 (19.9) | <0.001 | 646 (11.6) | 4223 (8.1) | <0.001 |
| Renal failure | 32 (4.1) | 159 (3.9) | 0.739 | 118 (2.1) | 904 (1.7) | 0.030 |
| Diabetes | 164 (21.2) | 913 (22.3) | 0.499 | 1084 (19.5) | 10 688 (20.4) | 0.139 |
| Peripheral artery disease | 80 (10.4) | 385 (9.4) | 0.415 | 261 (4.7) | 1846 (3.5) | <0.001 |
| Cancer | 37 (4.8) | 170 (4.2) | 0.425 | 150 (2.7) | 1030 (2.0) | <0.001 |
| Hypertension | 376 (48.7) | 2227 (54.5) | 0.003 | 2417 (43.6) | 24 903 (47.5) | <0.001 |
| Previous CABG | 43 (5.6) | 206 (5.0) | 0.542 | 269 (4.8) | 2134 (4.1) | 0.006 |
| Previous PCI | 35 (4.5) | 174 (4.3) | 0.730 | 155 (2.8) | 1712 (3.3) | 0.059 |
| Previous cardiovascular medications | ||||||
| ACE inhibitor | 140 (18.3) | 792 (19.5) | 0.434 | 867 (15.7) | 8089 (15.5) | 0.664 |
| Angiotensin II receptor blocker | 97 (12.7) | 502 (12.4) | 0.814 | 598 (10.9) | 5504 (10.6) | 0.500 |
| Warfarin | 36 (4.7) | 167 (4.1) | 0.457 | 227 (4.1) | 1455 (2.8) | <0.001 |
| Aspirin | 310 (40.5) | 1581 (38.8) | 0.398 | 1801 (32.6) | 15 044 (28.8) | <0.001 |
| Clopidogrel | 40 (5.3) | 173 (4.3) | 0.238 | 177 (3.2) | 1483 (2.9) | 0.114 |
| β‐Blocker | 107 (14.0) | 1640 (40.3) | <0.001 | 844 (15.3) | 18 486 (35.4) | <0.001 |
| Calcium channel blocker | 160 (20.9) | 714 (17.6) | 0.028 | 927 (16.8) | 7761 (14.9) | <0.001 |
| Digoxin | 21 (2.7) | 83 (2.0) | 0.222 | 115 (2.1) | 476 (0.9) | <0.001 |
| Diuretic | 339 (44.2) | 1406 (34.6) | <0.001 | 1437 (26.1) | 10 512 (20.1) | <0.001 |
| Statin | 153 (19.9) | 894 (22.0) | 0.210 | 982 (17.8) | 9883 (18.9) | 0.042 |
| Nitrate | 116 (15.1) | 481 (11.8) | 0.010 | 515 (9.3) | 4070 (7.8) | <0.001 |
| Previous COPD medications | ||||||
| Any inhalation therapy | 464 (60.1) | 2118 (51.8) | <0.001 | 464 (7.3) | 2118 (3.7) | <0.001 |
| Long‐acting anticholinergic | 201 (26.0) | 897 (22.0) | 0.013 | 25 (0.5) | 163 (0.3) | 0.081 |
| Short‐acting anticholinergic | 118 (15.3) | 431 (10.5) | <0.001 | 15 (0.3) | 139 (0.3) | 0.941 |
| Glucocorticoid | 133 (17.2) | 579 (14.2) | 0.028 | 190 (3.4) | 1020 (1.9) | <0.001 |
| β‐2‐Agonist | 258 (33.4) | 1097 (26.8) | <0.001 | 260 (4.7) | 1484 (2.8) | <0.001 |
| β‐2‐agonist combo (ATC: R03AK) | 263 (34.1) | 1112 (27.2) | <0.001 | 152 (2.7) | 884 (1.7) | <0.001 |
For normally distributed continuous variables, mean and SD are presented. For non‐normally distributed continuous variables (age and body mass index), median and 25th to 75th percentiles are presented. Count and percentage are presented for categorical variables. ACE indicates angiotensin‐converting enzyme; CABG, coronary artery bypass graft surgery; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
COPD patients not receiving β‐blocker treatment at discharge were older, had a lower body mass index, were less frequently current smokers, and had a higher prevalence of previous stroke and heart failure but a lower prevalence of hypertension. COPD patients not receiving β‐blocker treatment at discharge had less β‐blocker treatment, more digoxin, and more diuretics at baseline.
In‐Hospital Characteristics
In‐hospital characteristics in patients with and without COPD are outlined in Table 2. Blood pressure at presentation was lower for patients with COPD not receiving β‐blocker treatment at discharge. Use of in‐hospital anticoagulants and in‐hospital β‐blockers differed between the groups. STEMI was less common in COPD patients not receiving β‐blocker treatment at discharge, as well as angiography and percutaneous coronary intervention. This group also received more continuous positive airway pressure treatment. In patients investigated with echocardiography, patients not receiving β‐blocker treatment at discharge had a lower frequency of reduced left ventricular ejection fraction. However, this group had a higher rate of patients discharged without receiving an echocardiographic investigation at all.
Table 2.
In‐Hospital Characteristics of Consecutive MI Hospital Survivors With COPD (4858) and Without COPD (57 997) in Sweden Between 2005 and 2010
| Characteristic | Patients With COPD | Patients Without COPD | ||||
|---|---|---|---|---|---|---|
| No β‐Blocker | β‐Blocker | P Value | No β‐Blocker | β‐Blocker | P Value | |
| n=772 | n=4086 | n=5548 | n=52 449 | |||
| Heart rate | 89±23 | 88±23 | 0.534 | 78±22 | 81±21 | <0.001 |
| Systolic blood pressure | 143±29 | 146±28 | 0.004 | 146±28 | 150±28 | <0.001 |
| Diastolic blood pressure | 79±18 | 83±17 | <0.001 | 81±16 | 86±17 | <0.001 |
| Creatinine | 85 (67 to 109) | 85 (69 to 108) | 0.977 | 84 (70 to 103) | 82 (70 to 98) | <0.001 |
| In‐hospital anticoagulant | <0.004 | <0.001 | ||||
| Heparin | 25 (3.2) | 205 (5.0) | 255 (4.6) | 3934 (7.5) | ||
| Enoxaparin | 393 (51.0) | 2038 (50.0) | 2415 (43.6) | 23 017 (44.0) | ||
| Fondaparinux | 149 (19.3) | 932 (22.9) | 1261 (22.8) | 1 2017 (23.0) | ||
| In‐hospital β‐blocker | <0.001 | <0.001 | ||||
| Intravenous | 78 (10.1) | 869 (21.3) | 797 (14.4) | 12 616 (24.1) | ||
| Oral | 128 (16.6) | 2088 (51.3) | 1337 (24.2) | 27 582 (52.7) | ||
| STEMI | 131 (17.1) | 1034 (25.4) | <0.001 | 1421 (25.7) | 17 304 (33.1) | <0.001 |
| Angiography | 324 (42.0) | 2544 (62.3) | <0.001 | 3459 (62.3) | 40 400 (77.0) | <0.001 |
| PCI | 195 (25.3) | 1761 (43.1) | <0.001 | 2349 (42.3) | 31 262 (59.6) | <0.001 |
| Stented | 194 (25.1) | 1698 (41.6) | <0.001 | 2251 (40.6) | 30 089 (57.4) | <0.001 |
| CABG | 18 (2.3) | 102 (2.5) | 0.787 | 149 (2.7) | 1614 (3.1) | 0.106 |
| CPAP | 73 (9.5) | 287 (7.0) | 0.018 | 219 (4.0) | 1790 (3.4) | 0.039 |
| AF at discharge | 51 (6.9) | 270 (6.8) | 0.909 | 413 (7.8) | 2332 (4.6) | <0.001 |
| Bleeding req. surgery/transfusion | 10 (1.3) | 79 (1.9) | 0.229 | 101 (1.8) | 707 (1.4) | 0.004 |
| LVEF at discharge | <0.001 | <0.001 | ||||
| Normal (≥50%) | 213 (27.6) | 1317 (32.2) | 2155 (38.8) | 21 595 (41.2) | ||
| Mildly reduced (40% to 49%) | 95 (12.3) | 711 (17.4) | 681 (12.3) | 8921 (17.0) | ||
| Moderately reduced (30% to 39%) | 56 (7.3) | 516 (12.6) | 351 (6.3) | 5361 (10.2) | ||
| Severely reduced (<30%) | 32 (4.1) | 279 (6.8) | 166 (3.0) | 1980 (3.8) | ||
| Unknown (missing data) | 376 (48.7) | 1263 (30.9) | 2195 (39.6) | 14 592 (27.8) | ||
| Discharge medications | ||||||
| ACE inhibitor | 313 (40.6) | 2310 (56.6) | <0.001 | 2414 (43.6) | 31 156 (59.5) | <0.001 |
| Angiotensin II receptor blocker | 112 (14.5) | 518 (12.7) | 0.166 | 635 (11.4) | 5935 (11.3) | 0.782 |
| Warfarin | 44 (5.7) | 231 (5.7) | 0.963 | 306 (5.5) | 2465 (4.7) | 0.007 |
| Aspirin | 638 (82.6) | 3748 (91.8) | <0.001 | 4789 (86.3) | 49 521 (94.4) | <0.001 |
| Clopidogrel | 405 (53.2) | 2826 (69.7) | <0.001 | 3437 (62.8) | 40 221 (77.5) | <0.001 |
| Calcium channel blocker | 193 (25.0) | 563 (13.8) | <0.001 | 992 (17.9) | 6435 (12.3) | <0.001 |
| Diuretic | 407 (52.7) | 1947 (47.7) | 0.010 | 1747 (31.5) | 14 635 (27.9) | <0.001 |
| Statin | 441 (57.1) | 3195 (78.2) | <0.001 | 3718 (67.1) | 44 938 (85.7) | <0.001 |
| Nitrate | 162 (21.0) | 753 (18.5) | 0.100 | 834 (15.1) | 6539 (12.5) | <0.001 |
For normally distributed continuous variables, mean and SD are presented. For non‐normally distributed continuous variables (creatinine), median and 25th to 75th percentiles are presented. Count and percentage are presented for categorical variables. ACE indicates angiotensin‐converting enzyme; AF, atrial fibrillation; CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; CPAP, continuous positive airway pressure; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction.
Patients with COPD not receiving β‐blocker treatment at discharge were also discharged to a lower degree with the standard guideline‐recommended post‐MI secondary prevention medications. In contrast, they were more often discharged with calcium channel blockers and diuretics.
Outcomes
The median follow‐up time for MI patients with concomitant COPD was 1033 days (interquartile range 1141 days). The unadjusted hazard ratio (HR) for all‐cause mortality in COPD patients with β‐blocker treatment at discharge was 0.64 (95% CI 0.58 to 0.71). After adjusting for potential confounders using the multivariate model, COPD patients with β‐blocker treatment at discharge still showed lower all‐cause mortality compared to COPD patients without β‐blocker treatment at discharge, but the HR was increased (HR 0.87, 95% CI 0.78 to 0.98, P=0.017). In the other predefined time intervals of 30 days and of 1 year, similar trends were seen although not statistically significant. These analyses are illustrated in Figure 1.
Figure 1.
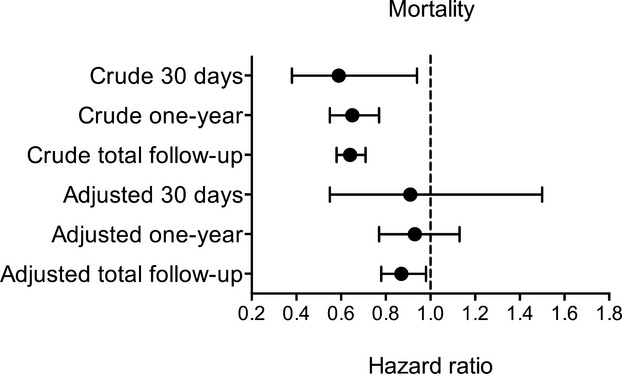
Hazard ratio and confidence intervals for MI patients with COPD discharged with β‐blocker compared to MI patients with COPD not discharged with β‐blocker. Crude all‐cause mortality was calculated with the univariate Cox proportional hazard model. Adjusted all‐cause mortality was calculated with the multivariate Cox proportional hazard model. Total follow‐up time was up to 7.2 years. COPD indicates chronic obstructive pulmonary disease; MI, myocardial infarction.
Sensitivity and Subgroup Analyses
A sensitivity analysis testing the effect of β‐blocker treatment at discharge for the whole MI hospital survivor population of 62 855 patients between 2005 and 2010, regardless of COPD status, yielded similar results using the multivariate model (HR 0.87, 95% CI 0.83 to 0.91, P<0.001).
Testing the multivariate model in patients only diagnosed with COPD before the MI admission did not change the results (HR 0.87, 95% CI 0.76 to 0.99, P=0.039).
Landmark analysis from 30 days after the MI up to the maximum follow‐up time showed the same HR of 0.87 (95% CI 0.78 to 0.98, P=0.017) as the main analysis.
A sensitivity analysis using a propensity score as a continuous covariate in a Cox proportional hazard model was also performed. Patients with COPD not discharged with β‐blockers had a median propensity score of 0.76 (25th to 75th percentile: 0.67 to 0.85). Patients with COPD discharged with β‐blockers had a median propensity score of 0.88 (25th to 75th percentile: 0.80 to 0.94). The HR in this analysis was 0.84 (95% CI 0.75 to 0.94, P=0.002).
Subgroup analyses in patients with or without a history of congestive heart failure are shown in Figure 2. Patients with COPD and a history of congestive heart failure had a hazard ratio of 0.77 (95% CI 0.63 to 0.95, P=0.012) for all‐cause mortality. Patients with COPD without a history of congestive heart failure had a hazard ratio of 0.90 (95% CI 0.78 to 1.03).
Figure 2.
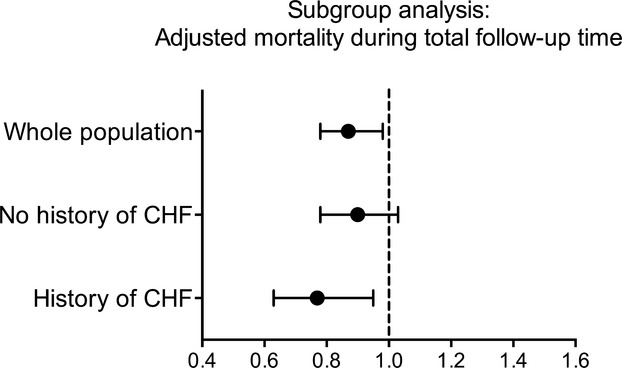
Hazard ratio and confidence intervals for MI patients with COPD discharged with β‐blocker compared to MI patients with COPD not discharged with β‐blocker. Adjusted all‐cause mortality was calculated with the multivariate Cox proportional hazard model. CHF indicates congestive heart failure; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction.
Discussion
The main finding in this study was an association between prescription of β‐blockers at discharge and lower all‐cause mortality in MI hospital survivors with concomitant COPD. After adjustment for potential confounders identified a priori, the association remained statistically significant but with lower relative risks. Patients with COPD and heart failure showed a numerically larger mortality difference; however, a trend toward lower mortality was also seen in patients with COPD without heart failure.
A total of 15.9% of the MI hospital survivors with COPD were not discharged with β‐blockers. This group was older, had a higher frequency of previous stroke, less hypertension and more heart failure, yet less β‐blockers at baseline. Instead, this group was more often prescribed calcium channel blockers and diuretics. Also, this group had more COPD medications at baseline, suggesting a more severe COPD. As a result, this group may have experienced more side effects and discontinued β‐blockers earlier, or the treating physicians might have been more reluctant to prescribe β‐blockers to these patients. Patients who were not discharged with β‐blockers also underwent less invasive investigation during hospitalization and were also undertreated with other proven secondary prevention agents upon discharge, suggesting that a more conservative treatment approach was adopted.
Comparison With Previous Studies
Several other studies have reported that COPD patients are less likely to be discharged with β‐blockers.8,24–25 As shown in Table 1, our findings are consistent with these studies, but the frequency of β‐blocker prescriptions was higher than in a recent study by Quint and co‐workers.18 This could reflect more underuse of β‐blockers in COPD patients in the United Kingdom compared to Sweden as supported by a recent study investigating acute MI care in Sweden compared to the United Kingdom.26 Differences in baseline‐ and in‐hospital characteristics between the groups defined by β‐blocker prescription were similar to findings from other studies.18,25 Taken together, the evidence indicates that patients not treated with β‐blockers have more cardiovascular comorbidities and especially more heart failure, which is problematic considering that one of the main indications for β‐blocker treatment is heart failure. Whether these patients have unmeasured contraindications or if this reflects true undertreatment remains speculative.
After adjustments for confounders, the HR for all‐cause mortality between the groups was 0.87. This effect estimate is lower compared to previous studies.15,17–18,27 Reasons for this could range from different study population characteristics to slightly different study designs. Our study population was particularly old, which could be due to underdiagnosis of mild COPD leading to a later diagnosis when symptoms are more pronounced in an older patient population. Our study design excluded patients who died in‐hospital, in part because of patients often being incorrectly classified as receiving no β‐blockers when they died before being discharged, which creates a strong reverse causal link between not receiving β‐blocker treatment and death, confounding the results in favor of β‐blocker treatment. Our study goal was to study the effect of β‐blockers as secondary prevention after patients leave the hospital.
Study Strengths and Limitations
Our study has several strengths. First, it was conducted in a modern setting, reflecting conditions in the present era of interventional cardiology with widespread use of percutaneous coronary intervention and modern secondary prevention, including dual antiplatelet treatment and statins. Second, it was a multicenter, nationwide study in a heterogeneous patient population with many complicating risk factors and comorbidities, reflecting real‐life clinical circumstances. Third, the study sample size was large, considering the clinical question of β‐blockers effect on all‐cause mortality after MI in COPD patients.
The main limitation of our study is its observational nature, and thus a certain degree of residual confounding cannot be excluded. Also, we do not know whether patients not receiving a β‐blocker at discharge were introduced to β‐blockers at a later time, or if patients actually discharged with a β‐blocker discontinued them during the follow‐up time. We did not have data on COPD severity as we did not have measurements on pulmonary function. Furthermore, a wide range of physicians diagnosed the COPD cases and therefore diagnostic criteria might have varied between patients. However, the validity of a COPD diagnosis in our registry has recently been reported to be good.22 Lastly, we want to point out that this study investigated all‐cause mortality, instead of cardiovascular mortality, to account for the high probability of competing risk of death since the patients with COPD were at high risk of both respiratory and infectious causes of death. As such, the manuscript does not provide insights into the specific cardioprotective effects of β‐blockers in MI patients with concomitant COPD.
Conclusions
Being discharged with a β‐blocker after an MI in COPD patients was associated with lower all‐cause mortality compared to being discharged without a β‐blocker. The association was stronger in patients with a history of congestive heart failure. The results indicate that MI patients with COPD may benefit from treatment with β‐blockers.
Acknowledgments
The authors would like to thank the staff members in all coronary care units in Sweden for their help and cooperation in contributing data to the Swedish Web‐system for Enhancement and Development of Evidence‐based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) system.
Sources of Funding
This study has been funded by research grants from the Swedish Foundation of Strategic Research (http://www.stratresearch.com/en/). The SWEDEHEART registry is publicly funded by the Swedish state and regional authorities.
Disclosures
None.
References
- Task Force on the management of ST‐segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, Atar D, Badano LP, Blomstrom‐Lundqvist C, Borger MA, Di MC, Dickstein K, Ducrocq G, Fernandez‐Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van‘t Hof A, Widimsky P, Zahger D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation. Eur Heart J. 2012; 33:2569-2619. [DOI] [PubMed] [Google Scholar]
- Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger DGuidelines ESCCfP. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST‐segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2999-3054. [DOI] [PubMed] [Google Scholar]
- Group TNMS. Timolol‐induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med. 1981; 304:801-807. [DOI] [PubMed] [Google Scholar]
- Hjalmarson A, Herlitz J, Holmberg S, Ryden L, Swedberg K, Vedin A, Waagstein F, Waldenstrom A, Waldenstrom J, Wedel H, Wilhelmsen L, Wilhelmsson C. The Goteborg metoprolol trial. Effects on mortality and morbidity in acute myocardial infarction. Circulation. 1983; 67:I26-I32. [PubMed] [Google Scholar]
- Gottlieb SS, McCarter RJ, Vogel RA. Effect of beta‐blockade on mortality among high‐risk and low‐risk patients after myocardial infarction. N Engl J Med. 1998; 339:489-497. [DOI] [PubMed] [Google Scholar]
- Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, O'Neill WW, Grines CL. Does beta‐blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 2004; 43:1773-1779. [DOI] [PubMed] [Google Scholar]
- Campo G, Guastaroba P, Marzocchi A, Santarelli A, Varani E, Vignali L, Sangiorgio P, Tondi S, Serenelli C, De Palma R, Saia F. Impact of COPD on long‐term outcome after ST‐segment elevation myocardial infarction receiving primary percutaneous coronary intervention. Chest. 2013; 144:750-757. [DOI] [PubMed] [Google Scholar]
- Bursi F, Vassallo R, Weston SA, Killian JM, Roger VL. Chronic obstructive pulmonary disease after myocardial infarction in the community. Am Heart J. 2010; 160:95-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andell P, Koul S, Martinsson A, Sundstrom J, Jernberg T, Smith JG, James S, Lindahl B, Erlinge D. Impact of chronic obstructive pulmonary disease on morbidity and mortality after myocardial infarction. Open Heart. 2014; 1:e000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadi HA, Zubaid M, Al MW, El‐Menyar AA, Ridha M, Alsheikh‐Ali AA, Singh R, Assad N, Al HK, Al SJ. Prevalence and prognosis of chronic obstructive pulmonary disease among 8167 Middle Eastern patients with acute coronary syndrome. Clin Cardiol. 2010; 33:228-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury AC, Reid KJ, Spertus JA. Impact of chronic obstructive pulmonary disease on post‐myocardial infarction outcomes. Am J Cardiol. 2007; 99:636-641. [DOI] [PubMed] [Google Scholar]
- Egred M, Shaw S, Mohammad B, Waitt P, Rodrigues E. Under‐use of beta‐blockers in patients with ischaemic heart disease and concomitant chronic obstructive pulmonary disease. QJM. 2005; 98:493-497. [DOI] [PubMed] [Google Scholar]
- Salpeter S, Ormiston T, Salpeter E. Cardioselective beta‐blockers for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005; 4:CD003566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Y, Shi G, Wan H. Use of cardioselective beta‐blockers in patients with chronic obstructive pulmonary disease: a meta‐analysis of randomized, placebo‐controlled, blinded trials. J Int Med Res. 2012; 40:2051-2065. [DOI] [PubMed] [Google Scholar]
- Etminan M, Jafari S, Carleton B, FitzGerald JM. Beta‐blocker use and COPD mortality: a systematic review and meta‐analysis. BMC Pulm Med. 2012; 12:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short PM, Lipworth SI, Elder DH, Schembri S, Lipworth BJ. Effect of beta blockers in treatment of chronic obstructive pulmonary disease: a retrospective cohort study. BMJ. 2011; 342:d2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten FH, Zuithoff NP, Hak E, Grobbee DE, Hoes AW. Beta‐blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med. 2010; 170:880-887. [DOI] [PubMed] [Google Scholar]
- Quint JK, Herrett E, Bhaskaran K, Timmis A, Hemingway H, Wedzicha JA, Smeeth L. Effect of beta blockers on mortality after myocardial infarction in adults with COPD: population based cohort study of UK electronic healthcare records. BMJ. 2013; 347:f6650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernberg T, Attebring MF, Hambraeus K, Ivert T, James S, Jeppsson A, Lagerqvist B, Lindahl B, Stenestrand U, Wallentin L. The Swedish Web‐system for enhancement and development of evidence‐based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart. 2010; 96:1617-1621. [DOI] [PubMed] [Google Scholar]
- Swedish National Board of Health and Welfare. Swedish National Patient Register Available at: http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish. Accessed February 17, 2012.
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HDJoint ESC/ACCF/AHA/WHF Task Force for Universal Definition of Myocardial Infarction; Authors/Task Force Members Chairpersons, Thygesen K, Alpert JS, White HDBiomarker Subcommittee, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DAECG Subcommittee, Chaitman BR, Clemmensen PM, Johanson P, Hod HImaging Subcommittee, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJClassification Subcommittee, Fox KA, Atar D, Newby LK, Galvani M, Hamm CWIntervention Subcommittee, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde JTrials & Registries Subcommittee, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons MLTrials & Registries Subcommittee, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos GTrials & Registries Subcommittee, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood DTrials & Registries Subcommittee, Smith SC, Hu D, Lopez‐Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis SESC Committee for Practice Guidelines (CPG), Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck‐Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker SDocument Reviewers. Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012; 60:1581-1598.22958960 [Google Scholar]
- Inghammar M, Engstrom G, Lofdahl CG, Egesten A. Validation of a COPD diagnosis from the Swedish Inpatient Registry. Scand J Public Health. 2012; 40:773-776. [DOI] [PubMed] [Google Scholar]
- Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011; 22:745. [DOI] [PubMed] [Google Scholar]
- Stefan MS, Bannuru RR, Lessard D, Gore JM, Lindenauer PK, Goldberg RJ. The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction: a 10‐year retrospective observational study. Chest. 2012; 141:1441-1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olenchock BA, Fonarow GG, Pan W, Hernandez A, Cannon CPGet With The Guidelines Steering C. Current use of beta blockers in patients with reactive airway disease who are hospitalized with acute coronary syndromes. Am J Cardiol. 2009; 103:295-300. [DOI] [PubMed] [Google Scholar]
- Chung SC, Gedeborg R, Nicholas O, James S, Jeppsson A, Wolfe C, Heuschmann P, Wallentin L, Deanfield J, Timmis A, Jernberg T, Hemingway H. Acute myocardial infarction: a comparison of short‐term survival in national outcome registries in Sweden and the UK. Lancet. 2014; 383:1305-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Radford MJ, Wang Y, Marciniak TA, Krumholz HM. Effectiveness of beta‐blocker therapy after acute myocardial infarction in elderly patients with chronic obstructive pulmonary disease or asthma. J Am Coll Cardiol. 2001; 37:1950-1956. [DOI] [PubMed] [Google Scholar]


