Abstract
Loss of heterozygosis (LOH) on chromosome (Chr) 18q21-23 was reported to be one of the most common genetic alterations identified in bladder cancer. The current study aimed to determine the prognostic role of LOH on Chr 18q21-23 in patients diagnosed with muscle-invasive urothelial bladder carcinoma (MIBC). A total of 34 consecutive patients were enrolled in the present prospective study. LOH on Chr 18 was assessed by performing multiplex polymerase chain reaction on paired blood and tumour tissue samples from each patient. The following primers were used in the present study: D18S51, MBP LW and MBP H. These data were then compared with follow-up information. The main outcome measure was patient status at the end of the follow-up. Cox regression was used to evaluate the impact of each parameter on cancer-specific survival and the Kaplan Meier test for disease-free survival was plotted in order to estimate survival. Out of 34 patients, 18 (52.9%) exhibited ≥1 alteration in one of the loci analysed on chromosome 18, while 16 (47.1%) revealed no alterations. No correlation was identified with stage (P=0.18) or grade (P=0.06); however, LOH on Chr 18q21-23 was significantly associated with a lower recurrence-free probability (P<0.0001). Kaplan-Meier curves demonstrated a significant association between patient status at follow-up and LOH on Chr 18 (P<0.001). In addition, multivariate analysis identified LOH on Chr 18 (P<0.001) and stage (P=0.01) as independent survival predictors. Furthermore, artificial neural network analysis was consistent with the results of the multivariate analysis. In conclusion, the present study highlighted the role of LOH on Chr 18q21-23 in predicting the clinical outcome of patients with MIBC.
Keywords: urothelial cancer, invasive bladder cancer, microsatellite analysis, chromosome 18, loss of heterozygosis
Introduction
Urothelial carcinoma (UC) of the urinary bladder is a relevant social problem with almost 67,160 novel cases diagnosed each year and accounts for ~13,750 cancer-associated mortalities each year in the United States (1). Mhawech-Fauceglia et al (2) suggested that the pathology of bladder carcinoma was a difficult to fully elucidate due to the complex oncogenic pathways involved and the inconsistent clinical behaviour of the disease.
Numerous previous studies have identified potential molecular markers for bladder carcinoma in an effort to fully elucidate the cellular mechanisms involved in its pathogenesis and development. Consequently, the prediction of tumour biological potential may help to select patients for treatment, thus improving the survival rates and quality of life of these patients (3–5). Tumour genome analysis has been used to obtain information regarding the natural history of UC (6). Of note, the loss of heterozygosis (LOH) on chromosome (Chr) 18 was reported to be the initial genetic event in bladder cancer (7).
As tumour-suppressor genes, including the DCC (18q21.3) and DPC4 (18q21.1) genes were identified on Chr 18q (8), it was suggested that somatic alterations on this chromosome may be a critical step for bladder carcinogenesis. In addition, it was reported that loss or inactivation of the SMAD4/DPC4 gene may be involved in the onset of various types of cancer, while LOH of 18q21.1 was demonstrated to be associated with a poor prognosis in bladder carcinoma patients (8). The distal section of Chr 18 (18q21-q23) was considered to be a potential locus of numerous crucial genes for the pathogenesis and progression of bladder cancer. A previous study highlighted the role of LOH analysis of Chr 18 for enhancing the prediction of recurrence in patients with low-grade non-muscle-invasive bladder cancer (4); however, further studies are required. Notably, the D18S51, MBP LW and MBP H loci are located on the long arm of Chr 18, where a number of tumor suppressor genes, including DCC and DPC4, are located (6).
The present study aimed to evaluate LOH on Chr 18 in patients with muscle-invasive urothelial bladder cell carcinomas in order to determine whether there is an association between LOH on Chr 18 and tumour stage. In addition, the present study aimed to investigate whether LOH on Chr 18 has a role in predicting the clinical outcome of patients with muscle-invasive urothelial bladder cancer.
Materials and methods
Study design
LOH on Chr 18 was investigated in muscle-invasive UC of the urinary bladder and the findings were then correlated with patient follow-up data. A total of 34 consecutive patients were recruited for the present prospective study who underwent a transurethral resection of bladder tumour (TURBT) at the Department of Urology, University of Florence (Florence, Italy), between January and December 2002. All patients enrolled in the present study were diagnosed with muscle-invasive urothelial bladder cancer [MIBC; ≥primary tumour stage (pT)2, according to the European Association of Urology guidelines] and were able to comply with the follow-up schedules. Patients were excluded if they had a history of UC of the upper urinary tract, prostate cancer or other urologic cancer; in addition, patients with associated carcinoma in situ were omitted from the present study. All patients with other urologic diseases were also excluded, as were all patients lost to follow-up. All selected patients provided written informed consent and the study was approved by the research ethics committee of the University of Florence. The present study was conducted in accordance with the latest version of the Declaration of Helsinki (2008) and in line with Good Clinical Practice guidelines (9).
Specimen collection, histological and molecular analysis
Blood samples were collected from all patients during clinical evaluation and stored at −80°C until molecular analysis. Fresh tumour tissue samples were obtained during TURBT for pathological evaluation and were snap-frozen in liquid nitrogen in the operating room and stored at −80°C until molecular analysis. Tumour and normal DNA were extracted using the methods previously described (5). Briefly, the DNA of each sample underwent digestion with sodium dodecyl sulfate proteinase K (recombinant; Worthington Biochemical Corporation, Lakewood, NJ, USA; 55°C overnight), ribonuclease (Multiplex PCR Kit; Qiagen Spa, Milan, Italy) treatment (2 h at 37°C) and phenol chloroform (Life Technologies Italia, Monza, Italy) extraction. DNA was resuspended in 700 ml Tris EDTA (Life Technologies Italia). The quantity of DNA was evaluated by spectrophotometry optical density (NanoDrop® 1000UV spectrophotometer; Thermo Fisher Scientific, Inc., Wilmington, DE, USA), and the samples were diluted to a concentration of 4 ng/µl for amplification by polymerase chain reaction (PCR). PCR was performed in a final volume of 15 ml with 10 ng DNA in order to amplify genomic DNA at three specific Chr 18 loci: D18S51, MBP LW and MBP H. The primer sequences were as follows: Forward, 5′-TTC TTG AGC CCA GAA GGT TA-3′ and reverse, 5′-ATT CTA CCA GCA ACA ACA CAA ATA AAC-3′ for D18S51; forward, 5′-TGG CTA CTT GGG CTA TTG TAA ACG-3′ and reverse, 5′-GGT GGT TCT GTT CCC TCT ATC TCC-3′ for MBP LW; and forward, 5′-TCC GAG CAG CAG CCA GCA C-3′ and reverse, 5′-AAG CTC GTC GGA CTC TGA G-3′ for MBP H. Each primer was fluorescently marked with the dyes 6-FAM, NED and HEX (Applied Biosystems Life Technologies, Foster City, CA, USA). Normal and pathological DNA underwent amplification in an Applied Biosystems® 2720 Thermal Cycler (Life Technologies Italia); three PCRs were performed per patient. The amplification conditions of the reactions were a denaturation cycle at 95°C for 10 min, 32 cycles at 95°C for 30 sec, 56°C for D18S51 and 52°C for MBP LW and MBP H, for 30 sec, and 72°C for 1 min, and final extension at 72°C for 45 min. DNA quality was assessed by agarose gel and ethidium bromide staining (Life Technologies Italia). Amplification products (1 µl) were mixed with 12 µl formamide (molecular biology grade; Life Technologies Italia) and 0.5µl GeneScan ROX400 (Perkin Elmer Biosystems, Foster City, CA, USA), denatured at 95°C for 10 min and then rapidly iced. Up to 48 samples were then electrophoresed in an ABI Prism® 310 Genetic Analyzer (Life Technologies Italia). Amplification products (50 µl) were injected electrokinetically in a 47 cm capillary (Applied Biosystems Life Technologies) filled by performance optimized polymer 4 (Life Technologies Italia). Electrophoresis was conducted at 15 kV for 24 min at 60°C and electrodes were immersed in ABI Prism® 310 Genetic Analyzer Buffer (Life Technologies Italia). Numerical data collected during electrophoresis were analyzed by GeneScan software (version 3.1; Thermo Fisher Scientific, Inc.) to produce graphic and numerical results of dimension of amplified DNA fragments. The microsatellite markers employed in the present study and their locations were taken from the Genome Database (http:www.ncbi.nlm.nih.gov/genome). The primers for the MBP gene repeats also amplified two short tandem repeat loci (locus A and locus B) (10). Microsatellite sequences observed to be most frequently altered in previous studies (6,11,12) were selected for the present study. LOH was characterised as the complete or almost complete absence of one allele in tumour DNA. All molecular tests were performed in duplicate using isolated PCR reactions. All available haematoxylin and eosin-stained slides of bladder carcinomas were reviewed by one pathologist. Specimens were pathologically staged according to the 2010 Tumour-Node-Metastasis classification of the American Joint Committee on Cancer (13) and tumour grade was assigned in line with the 2004 World Health Organization/International Society of Urologic Pathology classification (14).
Patients
Following the diagnosis of MIBC, all patients underwent radical cystectomy with standard bilateral pelvic lymphadenectomy and urinary diversion. Radical cystectomy was performed by an expert uro-oncology consultant according to the procedure described by the International Consultation on Bladder Cancer (15). The lymph node dissection performed involved the excision of all lymphatic tissues surrounding the common iliac, external iliac, internal iliac and obturator arteries as well as the presacral region. Following cystectomy and urinary diversion, all patients underwent follow-up examinations, which were performed according to the European Association of Urology guidelines (16). In brief, chest x-rays and abdominal ultrasound were required every 3 months, computerised tomography of the abdomen every 6 months and bone scan and excretory urography every 12 months. Additional examinations were required for symptomatic disease (16). Concomitant urethrectomy was performed only in patients who had preoperative histologically proven UC of the prostate and/or urethra in association with MIBC (16).
Statistical analysis
As the null hypothesis, LOH on Chr 18 was assumed to have no impact on survival rate in patients with MIBC. The significance of all parameters was assessed using the Fisher's exact test and chi-square test, where P<0.05 was considered to indicate a significant difference between values. The 95% confidence intervals (CIs) were calculated for the probability of survival for the Kaplan-Meier estimates. Mann-Whitney tests were also used in order to compare the means of the different parameters. Univariate and multivariate relative risk was calculated using Cox proportional hazards regression analysis. SPSS 11.5 for Apple-Macintosh (SPSS, Inc., Chicago, IL, USA) was used to perform all statistical analyses.
Artificial Neural Network (ANN) analysis was employed in order to enhance the standard statistical analysis, as previously described (17,18). In brief, a neural network was used in order to predict the outcome of patients with MIBC, according to the findings of the univariate and multivariate analyses. The following factors were the input parameters (input neuron) for ANN analysis: Age, gender, number of lesions, diameter of lesions, LOH on Chr 18, stage and grade. ANN setup was performed using the commercially available NeuralWorks Predict software (2005; NeuralWare Inc., Carnegie, PA, USA).
Results
Patient and tumour characteristics
A total of 34 patients were enrolled in the present study, 32 of which were male and 2 were female (mean age, 69.9±8.7). The patient and tumour characteristics are detailed in Table I.
Table I.
Summary of clinical and histopathological patient data.
| A, Patient characteristics | |
|---|---|
| Characteristic | n (%) |
| No. of patients | 34 |
| Mean age ± standard deviation | 69.9±8.7 |
| Gender | |
| Male | 32 (94.1) |
| Female | 2 (5.9) |
| B, Patient anamnestic, pathological and clinical data | |
| Characteristic | n (%) |
| No. of recurrences/year | |
| 1 | 16 (47.1) |
| 2 | 9 (26.5) |
| ≥3 | 9 (26.5) |
| No. of lesions | |
| 1 | 21 (61.8) |
| 2 | 7 (20.6) |
| ≥3 | 6 (17.6) |
| Diameter of lesion (if multiple, diameter of the largest) | |
| <3 cm | 24 (70.6) |
| ≥3 cm | 10 (29.4) |
| Stage | |
| pT2 | 19 (55.9) |
| pT3a | 7 (20.6) |
| pT3b | 5 (14.7) |
| pT4 | 3 (8.8) |
| Grade | |
| G3 | 34 (100) |
| Lymph node involvement | |
| N0 | 28 (82.3) |
| N1 | 6 (17.7) |
| N2 | 0 (0.0) |
| N3 | 0 (0.0) |
| Previous intravesical therapy | 34 (100) |
| Cigarette smokers | 18 (52.9) |
| Charlson comorbidities index | |
| <2 | 26 (76.5) |
| 2 | 6 (17.6) |
| ≥3 | 2 (5.9) |
| Urinary diversion | |
| Cutaneous ureterostomy | 11 (32.4) |
| Ileal conduit | 6 (17.6) |
| Neobladder | 17 (50.0) |
| Mean no. of lymph nodes removed (range) | 15.1 (11–23) |
| Adjuvant chemotherapy | 3 (8.8) |
pT, primary tumour stage; G, grade; N, node involvement.
Molecular results
At the baseline, 18 (52.9%) patients exhibited ≥1 alteration in one of the loci analysed on Chr 18, while 16 (47.1%) showed no alterations on Chr 18. Out of the 18 patients with altered loci, the MBP LW locus was altered in 6 (33.3%), MBP H in 7 (38.9%) and D18S51 in 5 (27.8%) patients. In 2 patients the D18S51 locus was singularly altered, in 1 patient alterations occurred on both MBP H and D18S51 loci and 2 patients exhibited altered MBP LW and D18S51 loci.
Follow-up results
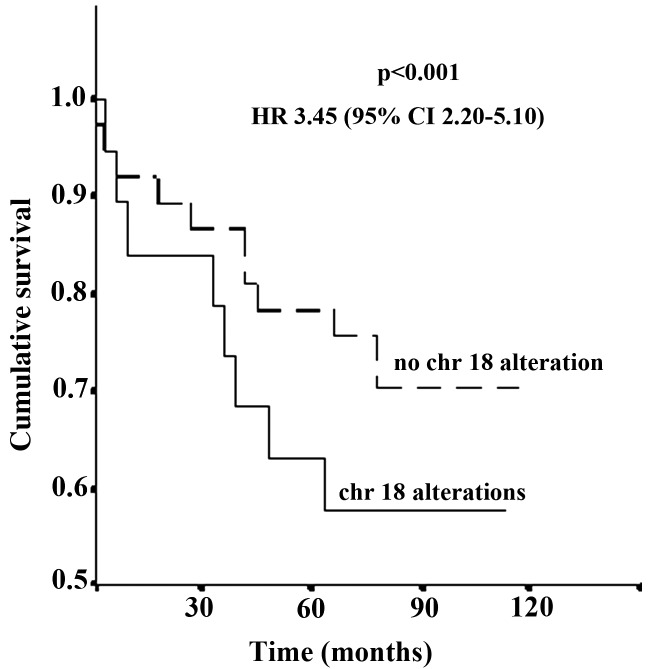
At a mean follow-up duration of 128.6 months post-surgery, 11 patients (32.3%) were alive with no evidence of disease (mean disease-free survival time, 126.6 months; 95% CI, 119.2–129.1 months). In addition, 8 patients were alive with evidence of tumour recurrence (mean disease-free survival time, 10.8 months; 95% CI, 103.5–115.1 months) and a further 11 patients succumbed to their disease (mean disease-free survival time, 23.2 months; 95% CI, 19.7–29.1 months) as well as four mortalities from non-associated causes. Cumulative cancer-specific survival rates of the whole study group at 1, 3 and 5 years were 88.2, 64.7 and 52.9%, respectively. No correlation was identified between clinical or pathological factors and the detection of LOH on Chr 18. Kaplan-Meier analysis revealed a significant correlation between patient status at follow-up and LOH on Chr 18 [hazard ratio (HR), 3.45; 95% CI, 2.20–5.10; P<0.001] (Fig. 1). The comparison of microsatellite analysis with follow-up data identified significant correlations between altered D18S51 (P<0.001) or MBP H (HR, 2.61; 95% CI, 1.80–3.12; P<0.001) loci and patient status at follow-up. However, no significant correlation was demonstrated between MBP LW and status at follow-up (P=0.6).
Figure 1.
Kaplan-Meier curves illustrating the association between LOH on chr 18 (HR, 3.45; 95% CI, 2.20–5.10; P<0.001) and cancer-specific survival patient probability. Mortality was used as endpoint in Kaplan-Meier analysis. Time (months), time from initial diagnosis to first recurrence (months); LOH, loss of heterozygosis; chr, chromosome; HR, hazard ratio; CI, confidence interval.
Univariate analysis, multivariate analysis and artificial ANN results
As determined using univariate analysis, stage, lymph node status, LOH on Chr 18 and age proved to be significantly associated with patient survival. According to the multivariate analysis, the detection of LOH on Chr 18 (HR, 4.08; 95% CI, 2.09–6.61; P=0.001) and stage (≥pT2; HR, 2.23; 95% CI, 1.17–3.46; P=0.01) were identified as independent prognostic factors in predicting status at follow-up. ANN analysis identified LOH on Chr 18 and stage as the most powerful variables affecting the output decision and predicting the natural history of MIBC; these results were consistent with those obtained by multivariate analysis.
Discussion
Optimal control and management of patients with bladder cancer is primarily dependent on appropriate risk-group stratification, which is established according to the correct assessment of biological and clinical characteristics (19). Numerous previous studies have identified several sequential genetic events, which were found to be associated with tumour natural history (8). A novel bladder cancer susceptibility locus, the urea transporter gene SLC14A1 was identified on Chr 18q (20,21). In addition, LOH on Chr 18q and 9q was reported to be able to predict the clinical outcome of patients with bladder cancer (8).
The present study demonstrated that LOH on Chr 18 was an independent prognostic indicator of survival in MIBC patients. Three loci were evaluated on the q arm of Chr 18 (18q21-23), where two tumour-suppressor genes, DCC (18q21.3) and DPC4 (18q21.1), are located (8). Uchida et al (8) suggested that Chr 18q was crucial in the development of the malignant phenotype, particularly in bladder cancer (7,8). Of note, in the present study, a strong correlation was observed between altered D18S51 or MBP H loci and patient outcome. A previous study, which investigated non-muscle-invasive UC, reported no notable correlation between D18S51 locus and status at follow-up (4), emphasising that LOH on Chr 18q22 (D18S51 locus) may be a late event in bladder tumorigenesis (22). Brewster et al (22) demonstrated that loss of genetic material on 18q21.3, which includes DCC, was associated with MIBC disease and was frequently present in tumour recurrences. The results of the present study confirmed that alterations in MBP LW and MBP H loci occurred in the early phase of bladder tumorigenesis, while the D18S51 locus was implicated in a later phase. Therefore, alteration in the D18S51 locus identified on tissue samples following TURBT may be considered as a negative prognostic factor affecting survival in patients with MIBC. A limitation of the present study is the small number of the patients analysed, this was due to the time-consuming and labour-intensive, thus expensive, molecular biology techniques employed. To the best of our knowledge, the current study was the first to demonstrate the use of LOH on Chr 18q21-23 in predicting the clinical outcome of patients with MIBC; however, further studies are required in order to confirm the present findings.
In conclusion, the present study highlighted the role of LOH on Chr 18q21-23 in predicting the clinical outcome of patients with MIBC. In addition, the present study elucidated the feasibility and utility of Chr 18 LOH as a potential clinical marker, in conjunction with well-established clinico-pathological factors, for the development of an effective adjuvant treatment schedule in MIBC patients.
Acknowledgements
The authors would like to thank Professor John Denton, Department of Modern Philology, University of Florence (Florence, Italy) for manuscript language revision.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.MhawechFauceglia P, Cheney RT, Schwaller J. Genetic alterations in urothelial bladder carcinoma: An updated review. Cancer. 2006;106:1205–1216. doi: 10.1002/cncr.21743. [DOI] [PubMed] [Google Scholar]
- 3.Tomasini JM, Konety BR. Urinary markers/cytology: What and when should a urologist use. Urol Clin North Am. 2013;40:165–173. doi: 10.1016/j.ucl.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Cai T, Nesi G, Dal Canto M, Mondaini N, Piazzini M, Bartoletti R. Prognostic role of loss of heterozygosity on chromosome 18 in patients with low-risk nonmuscle-invasive bladder cancer: Results from a prospective study. J Surg Res. 2010;161:89–94. doi: 10.1016/j.jss.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 5.Bartoletti R, Cai T, Nesi G, Roberta Girardi L, Baroni G, Dal Canto M. Loss of P16 expression and chromosome 9p21 LOH in predicting outcome of patients affected by superficial bladder cancer. J Surg Res. 2007;143:422–427. doi: 10.1016/j.jss.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 6.Bartoletti R, Cai T, Dal Canto M, Boddi V, Nesi G, Piazzini M. Multiplex polymerase chain reaction for microsatellite analysis of urine sediment cells: A rapid and inexpensive method for diagnosing and monitoring superficial transitional bladder cell carcinoma. J Urol. 2006;175:2032–2037. doi: 10.1016/S0022-5347(06)00283-7. [DOI] [PubMed] [Google Scholar]
- 7.Knowles MA. What we could do now: Molecular pathology of bladder cancer. Mol Pathol. 2001;54:215–221. doi: 10.1136/mp.54.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uchida A, Tachibana M, Miyakawa A, Nakamura K, Murai M. Microsatellite analysis in multiple chromosomal regions as a prognostic indicator of primary bladder cancer. Urol Res. 2000;28:297–303. doi: 10.1007/s002400000137. [DOI] [PubMed] [Google Scholar]
- 9.Switula D. Principles of good clinical practice (GCP) in clinical research. Sci Eng Ethics. 2000;6:71–77. doi: 10.1007/s11948-000-0025-z. [DOI] [PubMed] [Google Scholar]
- 10.Polymeropoulos MH, Xiao H, Merril CR. Tetranucleotide repeat polymorphism at the human myelin basic protein gene (MBP) Hum Mol Genet. 1992;1:658. doi: 10.1093/hmg/1.8.658. [DOI] [PubMed] [Google Scholar]
- 11.Bartoletti R, Dal Canto M, Cai T, Piazzini M, Travaglini F, Gavazzi A, Rizzo M. Early diagnosis and monitoring of superficial transitional cell carcinoma by microsatellite analysis on urine sediment. Oncol Rep. 2005;13:531–537. [PubMed] [Google Scholar]
- 12.DalCanto M, Bartoletti R, Travaglini F, Piazzini M, Lodovichi G, Rizzo M, Selli C. Molecular urinary sediment analysis in patients with transitional cell bladder carcinoma. Anticancer Res. 2003;23:5095–5100. [PubMed] [Google Scholar]
- 13.Edge SB, Byrd DR, Compton CC, et al. American Joint Committee on Cancer Staging Manual. 7th. Springer; New York, NY: 2010. pp. 117–126. [Google Scholar]
- 14.Eble JN, Sauter G, Epstein JI, Sesterhenn IA, editors. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. IARC Press; Lyon, France: 2004. pp. 89–154. [Google Scholar]
- 15.Gakis G, Efstathiou J, Lerner SP, et al. International Consultation on Urologic Disease-European Association of Urology Consultation on Bladder Cancer 2012: ICUD-EAU International Consultation on Bladder Cancer 2012: Radical cystectomy and bladder preservation for muscle-invasive urothelial carcinoma of the bladder. Eur Urol. 2013;63:45–57. doi: 10.1016/j.eururo.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Stenzl A, Cowan NC, De Santis M, Kuczyk MA, Merseburger AS, Ribal MJ, Sherif A, Witjes JA. European Association of Urology (EAU): Treatment of muscle-invasive and metastatic bladder cancer: Update of the EAU guidelines. Eur Urol. 2011;59:1009–1018. doi: 10.1016/j.eururo.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 17.Cai T, Conti G, Lorenzini M, Bartoletti R. Artificial intelligences in urological practice: The key to success? Ann Oncol. 2007;18:604. doi: 10.1093/annonc/mdl411. [DOI] [PubMed] [Google Scholar]
- 18.Cai T, Conti G, Nesi G, et al. Artificial intelligence for predicting recurrence-free probability of noninvasive high-grade urothelial bladder cell carcinoma. Oncol Rep. 2007;18:959–964. [PubMed] [Google Scholar]
- 19.Lee SE, Park MS. Prognostic factors for survival in patients with transitional cell carcinoma of the bladder: Evaluation by histopathologic grade, pathologic stage and flow-cytometric analysis. Eur Urol. 1996;29:193–198. [PubMed] [Google Scholar]
- 20.GarciaClosas M, Ye Y, Rothman N, Figueroa JD, Malats N, Dinney CP, Chatterjee N, Prokunina Olsson L, Wang Z, Lin J, et al. A genome-wide association study of bladder cancer identifies a new susceptibility locus within SLC14A1, a urea transporter gene on chromosome 18q12.3. Hum Mol Genet. 2011;20:4282–4289. doi: 10.1093/hmg/ddr342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koutros S, Baris D, Fischer A, et al. Differential urinary specific gravity as a molecular phenotype of the bladder cancer genetic association in the urea transporter gene, SLC14A1. Int J Cancer. 2013;133:3008–3013. doi: 10.1002/ijc.28325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brewster SF, Gingell JC, Browne S, Brown KW. Loss of heterozygosity on chromosome 18q is associated with muscle-invasive transitional cell carcinoma of the bladder. Br J Cancer. 1994;70:697–700. doi: 10.1038/bjc.1994.376. [DOI] [PMC free article] [PubMed] [Google Scholar]