Abstract
We sought to develop and pilot an intervention to improve blood pressure (BP) and other intermediate outcomes (A1c, LDL) of diabetes in a low-income ethnically diverse population. English- or Spanish-speaking primary care patients with BP ≥ 140/90 on two visits in the last 12 months and any level of A1c were randomized to usual care (n=24) or intervention (n=31). Home health nurses assessed self-management, medication adherence, and performed health behavior counseling. Participants transmitted daily BP and glucose results using simple home telemetry units to the nurse coordinator; these results were then aggregated and transmitted weekly to primary care providers [PCP] to facilitate intensified treatment. After controlling for baseline levels, a significantly larger proportion of the intervention group was at goal for BP (adjusted OR = 9.3, p = .006), and A1c (AOR = 4.3, p = .049), but not for LDL (AOR = 1.1, p =.86). Clinicians made more BP medication changes in the intervention compared to control group (8.3 vs 3.8, approaching significance at p= .06). Self-reported medication adherence and self-care behaviors were not significantly improved. We successfully developed a telephone- and email-based collaboration between home health nurses and primary care clinicians to address poorly controlled hypertension in an ethnically diverse population. The intervention, combining enhanced feedback to patients and their PCPs and individualized behavior change support by home health nurses is effective for improving BP and glucose in this setting.
Keywords: Diabetes Mellitus, Hypertension, Primary Care, Telemonitoring, Underserved Populations
Introduction
Evidence strongly supports control of blood pressure (BP), hyperglycemia and lipid levels to decrease vascular complications in diabetes (1–3). Yet evidence-based targets for BP, glucose, and lipids are often not met in primary care (4, 5). Clinical inertia, or physician failure to intensify therapy during office visits, has been implicated as contributing to poor chronic disease management (6–9). Not all failure to achieve targets is due to poor quality care (10). Multifaceted approaches are needed that target the provider, patient, and system simultaneously. The heightened risk of cardiovascular complications among ethnic minorities with diabetes (11) underscores the need for more effective strategies to control multiple risk factors especially among underserved patients.
In a Collaborative Approach to Control Hypertension in Diabetes (COACH-D), we developed a multi-component intervention in a multi-ethnic, low-income primary care population. We hypothesized that the intervention as a whole would be effective in improving blood pressure and other intermediate outcomes of diabetes management (glycosylated hemoglobin [A1c] and LDL cholesterol). The cornerstone of our patient-centered intervention was a collaboration between home health care nurses and primary care clinicians, employing home telemetry units that transmitted home blood pressure and blood glucose results to facilitate intensification of treatment by the primary care provider. Here we report outcomes of the pilot and feasibility study.
Methods
Participants/Sampling. Participants were English- or Spanish-speaking adult patients, age ≥ 30 years, receiving care for type 2 diabetes, with blood pressure (BP) above 140/90 recorded at two or more clinic visits in the past 12 months. Because of the nature of the intervention, a touchtone home phone was also required. Patients were excluded if they could not participate in the intervention or provide informed consent due to psychiatric or cognitive impairment, and if they had renal failure (Cr ≥4).
Setting
The study was conducted at a federally qualified health center in the Bronx, NY.
Procedures
After informed consent, participants completed a baseline interview, laboratory assessments of A1c and LDL cholesterol, and were then immediately randomly assigned to usual primary care or the collaborative intervention.
The Intervention
In brief physician training sessions, clinicians were educated to to meet guidelines of BP <130/80 (12), A1c <7% and LDL below 100 (13) as appropriate for individual patients. Home health nurses participated in workshops to enhance skills in promoting self-management, covering selected health behavior counseling techniques to control primarily blood pressure and also glucose and lipids (14,15). During home visits, nurses instructed participants in a protocol of daily telemonitoring using simple, inexpensive, leased Cardiocomtm equipment, and they provided self-management support focused on goal setting for behavior change and targeted health/risk communications related to improving the “ABCs” (A1c, BP and cholesterol). Daily BP and glucose readings were transmitted to the program manager and formatted as weekly reports; they were sent to the primary care providers via secure clinical e-mail. The primary care providers had been instructed to review these reports and to modify treatment plans appropriately. The Telehealth program manager, a nurse certified diabetes educator, provided ongoing support to both the nurses delivering the intervention and to the patients as needed. She monitored daily transmissions, reminded patients who did not transmit, and evaluated when values were outside the established parameters. Nurses communicated urgent symptoms to physicians immediately for additional orders.
Outcomes assessment
The primary outcome was achieving BP target of <130/80, measured at home by a trained research assistant. Following established protocol, we used the average of two readings taken with an aneroid sphygmomanometer. Laboratory specimens for secondary outcomes (A1c and fasting lipids) were drawn on the day of randomization and 6 months later. Surveys for demographics, literacy (16), self-care behaviors (17), and medication adherence (18) were administered at baseline and 4 months. Initiations, discontinuations, or dose changes of anti-hypertensive, lipid lowering, and glucose lowering medications were tracked using the clinical system’s electronic prescription database. Participants received modest incentives for completing the research interviews, but not for home visits or telemonitoring.
Analysis
Logistic regression models estimated group odds ratios of goal attainment for each outcome (BP, A1c, LDL) at 6-month follow-up, adjusting for baseline level of the measured outcome to control for pre-treatment differences between groups. SPSS version 17.0 (SPSS Co., Chicago, IL) and Stata version 11 (Stata Corp., College Station, TX) software were used.
Results
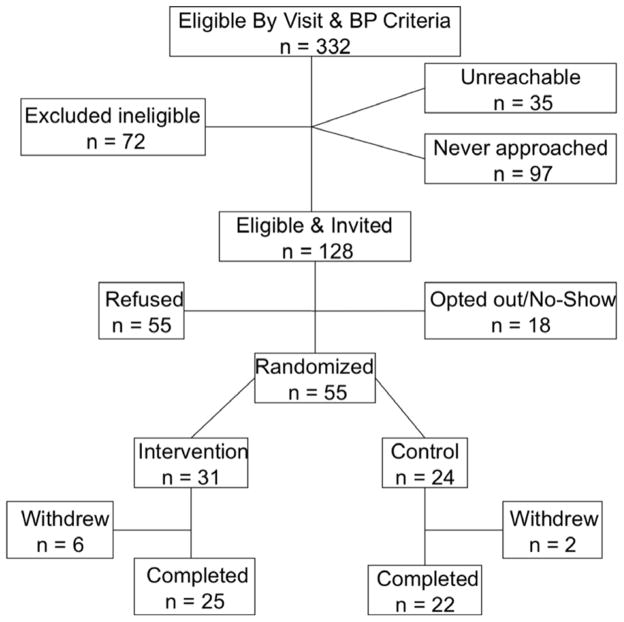
Figure 1 describes results of eligibility screening and recruitment. Of 1,268 patients with type 2 diabetes meeting visit criteria (attending a visit at the participating health center within the last 6 months and at least two visits within one year), 332 met eligibility criteria of having BP persistently well above recommended targets (above 140/90 at their last visit and at least one other visit in the preceding year). During the initial screening process, 72/332 (21.7%) were excluded, and 35/332 (10.5%) could not be reached by the study team. The most common reasons for exclusion were inability to speak English or Spanish, no primary care provider, or no longer receiving care at the health center, not available due to moving or travel, and inappropriate for study as determined by their PCP (most commonly due to severe psychiatric or cognitive impairment, or homelessness). Of the 128 eligible patients who were invited, 55 (43%) refused participation. Most common reasons for refusal were lack of interest (64.8%) or time (20.4%) to participate.
Figure 1.
Study Eligibility and Recruitment
Randomized participants (n=55, 24 usual care and 31 intervention) were mostly female (65%), low health literacy (62%), Medicaid insured (62%), and Hispanic (73%) with a mean age of 60.0 years. Half (51%) chose to complete the interview in Spanish. Table 1 reflects demographics by treatment group, as well as baseline and 6 month values for clinical characteristics. Intervention and usual care arms had appreciable differences in baseline characteristics, though only the proportion with Medicaid reached statistical significance.
Table 1.
Participant Demographics and Clinical Characteristics by Treatment Group
| Demographics | Control (n=24) | Intervention (n=31) | |||
|---|---|---|---|---|---|
|
| |||||
| M | sd | M | sd | p | |
| Age | 58.6 | 7.9 | 61.2 | 11.2 | 0.31 |
| n | (%) | n | (%) | ||
|
|
|||||
| Female | 16 | 66.7 | 20 | 66.7 | 1.0 |
| Latino/Hispanic | 18 | 75.0 | 22 | 70.9 | 0.71 |
| Non-Hispanic Black | 6 | 25.0 | 7 | 22.6 | 0.55 |
| US Born | 10 | 41.7 | 12 | 40.0 | 0.9 |
| Married | 8 | 33.3 | 10 | 33.3 | 0.42 |
| Unable to work due to disability | 6 | 25.0 | 12 | 40.0 | 0.22 |
| Foodstamps | 7 | 29.2 | 10 | 33.3 | 0.48 |
| SSI, SS retirement, disability, survivor benefit | 8 | 33.3 | 16 | 51.6 | 0.14 |
| Education | 0.32 | ||||
| Less than HS | 13 | 54.1 | 13 | 43.3 | |
| HS Grad | 5 | 20.8 | 12 | 40.0 | |
| Some college+ | 6 | 25.0 | 4 | 13.3 | |
| Medicaid | 19 | 79.2 | 15 | 48.4 | 0.02 |
| No insurance/Self-pay | 2 | 8.3 | 2 | 6.7 | 0.39 |
| Annual income < $20,000 | 18 | 75.0 | 22 | 70.9 | 0.49 |
| Completed survey in Spanish | 11 | 45.8 | 17 | 56.7 | 0.35 |
|
| |||||
| Clinical Characteristics | M | sd | M | sd | |
|
| |||||
| BMI | |||||
| Baseline | 34.6 | 9.8 | 32.5 | 6.6 | 0.38 |
| A1C | |||||
| Baseline | 8.5 | 2.3 | 8 | 1.9 | 0.41 |
| 6-month | 8.3 | 2.3 | 7.7 | 2.1 | 0.28 |
| LDL | |||||
| Baseline | 114.9 | 45.2 | 95.7 | 29.1 | 0.07 |
| 6-month | 109.3 | 41.3 | 102.9 | 46.4 | 0.61 |
| Systolic | |||||
| Baseline | 143.1 | 14.6 | 138.6 | 14.1 | 0.27 |
| 6-month* | 137.5 | 15.5 | 129.1 | 15.2 | 0.07 |
| Diastolic | |||||
| Baseline | 76.6 | 13.9 | 71.9 | 10.1 | 0.17 |
| 6-month* | 77.8 | 13.3 | 71.5 | 7.1 | 0.05 |
6-month blood pressure data reported only for participants who completed the protocol (Control n=22, Intervention n=23)
Nearly all participants completed the protocol (22 usual care, 25 intervention). Two participants were withdrawn due to telephone incompatibility with the Cardiocom unit. Intervention participants transmitted BP and glucose readings almost every day (86% and 85% of possible days, respectively), and received on average 10.4 home nursing visits over an average of 75.2 days (35.6 sd) or 10.7 weeks of intervention.
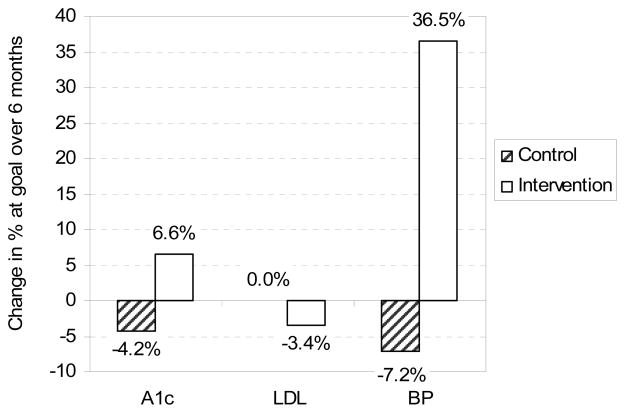
The proportion of the usual care group at goal decreased or stayed the same for each measure between baseline and 6-months. The intervention group showed improvement for A1c and blood pressure, but a decrease in the proportion at goal for LDL (Figure 2). Using logistic regression controlling for baseline levels, a significantly larger proportion of the intervention group was at goal for BP (adjusted OR = 9.3, p = .006) and A1c (AOR = 4.3, p = .049), but not for LDL (AOR = 1.1, p =.86).
Figure 2.
Change in Proportion at Goal for A1c, LDL and BP
With regard to potential mediators of the intervention effect, medication adherence scores and diet-related behaviors improved, though not significantly. More changes in prescribed hypertension medications or doses (but not glucose or cholesterol medications) were recorded for the intervention participants compared to usual care (8.3 vs 3.8 changes per year, approaching significance at p=.06).
Discussion
We developed, implemented and evaluated a novel intervention to improve blood pressure and other intermediate outcomes of diabetes management in a multi-ethnic, low-income primary care population. We used simple in-home telemetry to enhance feedback of clinical information to patients and their PCPs. High rates of daily blood pressure and glucose monitoring and transmission suggest overall high acceptability of the device. Through collaboration with home health nurses, home telemonitoring was coupled with health behavior counseling to support self-management. This approach has advantages in that it utilizes a simple inexpensive device, and support from home health nurses potentially available in most communities.
Our results provide preliminary evidence of effectiveness of the intervention for improving the primary target, BP, as well as glucose. A possible mechanism for the effect is decreasing PCP clinical inertia (20), as suggested by more blood pressure medication changes in the intervention group with a significantly greater proportion at BP goal by end of the study. The health behavior change counseling was not effective in producing improvements in the individual self-care behaviors measured, suggesting the need for more behavior change training for home health nurses, a different measure for self care, or an alternate delivery strategy. Additionally, more focused attention on medication adherence may facilitate additional improvement in all 3 outcomes of interest.
Limitations of this pilot and feasibility study include conducting it in a single primary care site, and its small sample size, which resulted in a somewhat underpowered study particularly for examining mediators of the intervention. Baseline differences between intervention and control groups were present for both demographic and clinical characteristics, though it was not possible to adjust for all of these due to small sample size. We adjusted for clinical characteristics because these were most closely related to study outcomes. Despite these limitations, we conclude that this collaborative approach is feasible and has potential to improve intermediate outcomes of diabetes management, and that further study of the intervention with appropriate statistical power is warranted.
Table 2.
Results from logistic models predicting goal attainment at 6-month follow-up
| A1c (≤7) | AOR | CI 95% for AOR | p |
|---|---|---|---|
| Intervention | 4.3 | (1.006, 18.2) | 0.049 |
| Baseline A1c (mg/dL) | .411 | (0.247, 0.685) | 0.001 |
|
| |||
| LDL (≤ 100) | |||
|
| |||
| Intervention | 1.13 | (0.3, 4.4) | 0.86 |
| Baseline LDL (mg/dL) | .957 | (0.933, 0.982) | 0.001 |
|
| |||
| BP (<130/80) | |||
|
| |||
| Intervention | 9.3 | (1.9, 44.9) | 0.006 |
| Baseline systolic (mm/dl) | 0.95 | (0.893, 1.0007) | .053 |
| Baseline diastolic (mm/dl) | 1.02 | (0.957, 1.094) | .496 |
Adjusted odds-ratios reflect odds of being at goal at 6-months adjusted for baseline values. Control group is reference group
References
- 1.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pyorala K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) Diabetes Care. 1997;20(4):614–20. doi: 10.2337/diacare.20.4.614. [DOI] [PubMed] [Google Scholar]
- 3.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. New England Journal of Medicine. 2003;348(5):383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 4.McBride P, Schrott HG, Plane MB, Underbakke G, Brown RL. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Archives of Internal Medicine. 1998;158(11):1238–44. doi: 10.1001/archinte.158.11.1238. [DOI] [PubMed] [Google Scholar]
- 5.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291(3):335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor PJ. Overcome clinical inertia to control systolic blood pressure. Arch Intern Med. 2003;163(22):2677–8. doi: 10.1001/archinte.163.22.2677. [DOI] [PubMed] [Google Scholar]
- 7.Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. New England Journal of Medicine. 1998;339(27):1957–63. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 8.Headrick LA, Speroff T, Pelecanos HI, Cebul RD. Efforts to improve compliance with the National Cholesterol Education Program guidelines. Results of a randomized controlled trial. Archives of Internal Medicine. 1992;152(12):2490–6. [PubMed] [Google Scholar]
- 9.Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Archives of Internal Medicine. 2000;160(15):2281–6. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 10.Kerr EA, Smith DM, Hogan MM, Hofer TP, Krein SL, Bermann M, et al. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Medical Care. 2003;41(10):1173–82. doi: 10.1097/01.MLR.0000088453.57269.29. [DOI] [PubMed] [Google Scholar]
- 11.Weng C, Coppini DV, Sonksen PH. Geographic and social factors are related to increased morbidity and mortality rates in diabetic patients. Diabetic Medicine. 2000;17(8):612–7. doi: 10.1046/j.1464-5491.2000.00352.x. [DOI] [PubMed] [Google Scholar]
- 12.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Standards of Medical Care in Diabetes-2010. Diabetes Care. 2010;33:S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller W, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guilford Press; 1991. [Google Scholar]
- 15.Dunn C, Rollnick S. Lifestyle Change. Philadelphia: Mosby; 2003. [Google Scholar]
- 16.Bakers DW, William MW, Parker RM, Nurss J. Development of a Brief Test to Measure Health Literacy. Patient education and counseling. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 17.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 18.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Raudenbush S, Bryk A. Hierarchical Linear Models Applications and Data Analysis Methods. 2. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 20.Berlowitz DR, Ash AS, Glickman M, Friedman RH, Pogach LM, Nelson AL, et al. Developing a quality measure for clinical inertia in diabetes care. Health Services Research. 2005;40(6 Pt 1):1836–53. doi: 10.1111/j.1475-6773.2005.00436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]