Abstract
Purpose
The purpose of this study was to describe the types and combinations of clinicians who are delivering babies in rural hospitals, their employment status, the relationship between hospital birth volume and staffing models, and the staffing challenges faced by rural hospitals.
Methods
We conducted a telephone survey of 306 rural hospitals in 9 states: Colorado, Iowa, Kentucky, New York, North Carolina, Oregon, Vermont, Washington, and Wisconsin, from November 2013-March 2014 to assess their obstetric workforce. Bivariate associations between hospitals’ annual birth volume and obstetric workforce characteristics were examined, as well as qualitative analysis of workforce changes and staffing challenges.
Findings
Hospitals with lower birth volume (< 240 births per year) are more likely to have family physicians and general surgeons attending deliveries, while those with a higher birth volume more frequently have obstetricians and midwives attending deliveries. Reported staffing challenges include scheduling, training, census fluctuation, recruitment and retention, and intra-hospital relationships.
Conclusions
Individual hospitals working in isolation may struggle to address staffing challenges. Federal and state policy makers, regional collaboratives, and health care delivery systems can facilitate solutions through programs such as telehealth, simulation training, and interprofessional education.
Keywords: access to care, family medicine, health services research, hospitals, physician supply
Timely access to obstetric services provided by skilled clinicians is critically important for the health of pregnant women and infants. However, hospitals offering obstetric services are unevenly distributed in the United States, and women living in rural areas experience substantial driving times to access obstetric care.1 Women who travel further for maternity services have worse birth outcomes, including higher rates of infant mortality and admission to the neonatal intensive care unit.2 Closure of obstetric units in rural hospitals has accelerated in recent years, raising concerns about access for rural women; low patient volume and staffing difficulties are among the most frequently cited reasons for closures of rural obstetric units.3,4
Birth volume varies among rural hospitals, and lower-volume rural hospitals (< 100 births per year) have higher rates of primary cesarean delivery and non-indicated cesarean delivery compared with their higher-volume counterparts.5 These patterns may be related to workforce and staffing limitations, and they have implications for maternal and infant health.
Health care workforce shortages have been a long-term problem in rural areas, especially in geographically isolated areas.6,7 Obstetrician-gynecologists provide the vast majority of obstetric care in the US, but their geographic distribution is uneven, contributing to disparities in access in rural areas.8 Family physicians, who have historically provided both prenatal and obstetric care in many rural settings, are attending fewer births and providing prenatal care less frequently over time.9,10 The supply of general surgeons has not kept pace with population increases,11 which is a concern for smaller rural hospitals that rely on general surgeons to do cesarean deliveries. The availability of clinicians to provide obstetric anesthesia services12 and trained nursing staff to safely care for patients in labor and delivery, postpartum, and neonatal units4,13 are additional concerns in rural areas. Further, access and quality challenges in maternity care may be greater among racial/ethnic minorities in rural areas.14,15
In recent years, hospitals have increased their employment of physicians (vs contracting with private practices) as a recruitment and retention strategy. More than half of practicing US physicians are now employed by hospitals or integrated delivery systems, a trend accelerated by implementation of health care reform, the rising costs of private practice, and the desires of younger physicians for better work-life balance.16,17
However, whether and how these trends affect the obstetric care workforce in rural hospitals is not known. The purpose of this study is to describe the types and combinations of clinicians who are delivering babies in rural hospitals, their employment status, the relationship between hospital birth volume and staffing models, and the staffing challenges faced by rural hospitals. The goal of this research is to inform the implementation of policy initiatives that can help rural areas maintain access to a skilled obstetric care workforce.
Methods
We conducted a telephone survey of rural hospitals that provide obstetric services in 9 states: Colorado, Iowa, Kentucky, New York, North Carolina, Oregon, Vermont, Washington, and Wisconsin. The survey sample consisted of all 306 rural hospitals in these 9 states with at least 10 births in the 2010 Health Care Cost and Utilization Project (HCUP) Statewide Inpatient Databases (SID). These all-payer databases contain information on 100% of hospital discharges; obstetric deliveries were identified using a validated methodology.18 The 9 states were chosen because of the size of their rural population, number of rural hospitals providing obstetric care, US regional distribution, and the availability of SID data that allow linkage with American Hospital Association (AHA) Annual Survey data. Critical Access Hospitals (CAHs) were identified using the Flex Monitoring Team CAH database. Rural areas were defined based on the Office of Management and Budget non-metropolitan county definition.
The survey questions were based on a review of the literature and recommendations from an advisory committee of obstetric nurse managers from 8 rural hospitals. They included closed and open-ended questions about the hospital's obstetric services, including delivery volume, types and numbers of clinicians attending deliveries, staffing challenges, staffing changes over the past 3 years, and changes expected in the future.
The survey interviews were conducted by the Office of Measurement Services at the University of Minnesota from November 2013 to March 2014. The vast majority of survey respondents (95%) had a managerial role in the obstetrics or women's health department (eg, Director or Nurse Manager); less than 5% of respondents had a broader managerial role in the hospital (eg, Chief Nursing Officer, Vice President for Patient Care) or were designated by the Obstetrics Director/Nurse Manager to complete the survey.
A total of 263 hospitals (86%) responded to the survey. They did not differ significantly from non-respondents in terms of organizational characteristics including size (adjusted daily census, inpatient days, number of beds, and number of births), accreditation, or system affiliation. Among the responding hospitals, 244 were currently providing obstetric services and 19 had stopped providing obstetric services since 2010. The survey data were merged with SID data and FY 2011 AHA Annual Survey data for the analysis.
Based on annual birth volume quartiles, we categorized hospitals as low (10-110), medium (111-240), medium-high (241-460), or high (> 460). We compared hospital categories across volume groups using 2-tailed Mantel–Haenszel chi-square statistics. Bivariate associations between numeric characteristics of hospitals (number and proportion of physicians) and birth volume were examined by Fisher's analysis of variance. Responses to open-ended questions about clinician changes and staffing challenges were thematically coded and analyzed. All quantitative analyses were performed using SAS 9.3 software (SAS Institute Inc., Cary, North Carolina).
This research was approved by the University of Minnesota Institutional Review Board (ID 1209S20781).
Findings
Characteristics of Surveyed Rural Hospitals
The surveyed rural hospitals are similar to all 1,195 US rural hospitals providing obstetric care in terms of accreditation rates, hospital system membership, birth volumes, and the number of beds and obstetric beds (Table 1). A higher percentage of the surveyed hospitals (51.2%) are CAHs, compared with 40.9% of all rural hospitals, reflecting a higher concentration of CAHs in some of the surveyed states.
Table 1. Characteristics of Surveyed Rural Hospitals and All Rural Hospitals Providing Obstetric Services.
| Hospital Characteristics | Surveyed Rural Hospitals (N=244) | All Rural Hospitals with Obstetric Servicesb (N=1144) |
|---|---|---|
| N (%) | N (%) | |
| Critical Access Hospital | 125 (51.2%) | 451 (39.4%) |
| Accreditationa | 152 (62.3%) | 654 (57.2%) |
| System Affiliation | 122 (50.0%) | 544 (47.6%) |
| Annual Birth Volume (2010) | ||
| Low (10-110) | 43 (17.6%) | 234 (20.4%) |
| Medium (111-240) | 75 (30.7%) | 250 (21.9%) |
| Medium-high (241-460) | 65 (26.6%) | 347 (30.3%) |
| High (> 460) | 61 (25.0%) | 313 (27.4%) |
| Mean (SD) | Mean (SD) | |
| Number of Beds | 64.6 (66.5) | 68.8 (64.7) |
| Number of Obstetric Beds | 7.1 (5.2) | 7.7 (6.4) |
| Number of Operating Rooms | 4.4 (2.8) | 4.3 (3.2) |
| Adjusted Average Daily Census | 139.0 (141.9) | 116.8 (119.0) |
Notes:
Joint Commission or American Osteopathic Association.
Defined as 10 or more births in 2010.
Based on annual birth volume in 2010, 17.6% of the surveyed rural hospitals had 10-110 births (low volume), 30.7% had 111-240 births (medium), 26.6% had 241-460 births (medium-high), and 25% had more than 460 births (high).
Clinicians Attending Deliveries
More than three-quarters (77%) of the surveyed rural hospitals have obstetricians attending deliveries (Table 2). Over half (55.3%) of hospitals have family physicians doing deliveries; in 32% of hospitals, family physicians perform cesarean deliveries. Certified Nurse Midwives (CNMs) attend deliveries in almost one-third (31.6%) of hospitals, and general surgeons perform cesarean deliveries in 23.4% of the hospitals.
Table 2. Clinicians Delivering Babies in Surveyed Rural Hospitals by Birth Volume.
| 2010 Hospital Annual Birth Volume | ||||||
|---|---|---|---|---|---|---|
| Surveyed Hospitals (N = 244) | Low (N=43) | Medium (N=75) | Medium High (N=65) | High (N=61) | P value | |
| Percent of Hospitals With: | ||||||
| Types of Clinicians Delivering Babies | ||||||
| Obstetricians | 77.0 | 37.2 | 66.7 | 93.8 | 100.0 | < .001 |
| Family Physicians | 55.3 | 93.0 | 70.7 | 41.5 | 24.6 | < .001 |
| Family Physicians Performing Cesareans | 32.0 | 58.1 | 44.0 | 23.1 | 8.2 | < .001 |
| Certified Nurse Midwives | 31.6 | 23.3 | 24.0 | 33.8 | 44.3 | .005 |
| General Surgeons | 23.4 | 58.1 | 32.0 | 12.3 | 0.0 | < .001 |
| Combinations of Clinicians | ||||||
| Obstetricians but No Family Physicians | 44.7 | 4.5 | 28.4 | 58.9 | 75.0 | < .001 |
| Family Physicians but No Obstetricians | 23.0 | 61.4 | 35.8 | 6.8 | 0.0 | < .001 |
| Both Obstetricians and Family Physicians | 32.4 | 34.1 | 35.8 | 34.2 | 25.0 | .220 |
| Anesthesia Services for Deliveries | ||||||
| Anesthesiologists Only | 11.9 | 0.0 | 8.0 | 12.3 | 24.6 | < .001 |
| CRNA Only | 50.0 | 97.7 | 66.7 | 33.8 | 13.1 | < .001 |
| Both Anesthesiologists and CRNAs | 38.1 | 2.3 | 25.3 | 53.8 | 62.3 | < .001 |
| Nurse Staffing for Deliveries | ||||||
| Nurses Work Exclusively in Maternity and Newborn Care (vs Other Areas of Hospital) | 43.4 | 7.0 | 29.3 | 58.5 | 70.5 | < .001 |
Notes: CRNA is Certified Registered Nurse Anesthetist. P values presented are from Mantel-Haenszel chi-square tests of significant difference across birth volume.
The type of clinicians attending deliveries varies significantly by hospital birth volume (P < .001 for all relationships described, unless noted otherwise). Hospitals with a lower volume of births are more likely to have family physicians and general surgeons attending deliveries, while high-volume hospitals are more likely to have obstetricians and CNMs (P = .005). Most (93%) hospitals with a low birth volume have one or more family physicians attending deliveries, while 100% of high-volume hospitals have at least one obstetrician attending deliveries. Just over a third of the low, medium, and medium-high volume hospitals have both family physicians and obstetricians attending deliveries. General surgeons perform cesarean deliveries in 58.1% of the low-volume hospitals, but in none of the high-volume hospitals surveyed.
Clinicians providing obstetric anesthesia and nurse staffing also vary by birth volume. Almost all (97.7%) low-birth-volume hospitals only have Certified Registered Nurse Anesthetists (CRNAs) providing anesthesia services. As birth volume increases, the percentage of hospitals where only anesthesiologists provide these services increases—from 8.0% of medium-volume hospitals to 24.6% of high-volume hospitals. Higher volume hospitals are significantly more likely to have obstetric nurses who work exclusively in labor and delivery vs other units in the hospital.
Number of Clinicians and Practice Arrangement
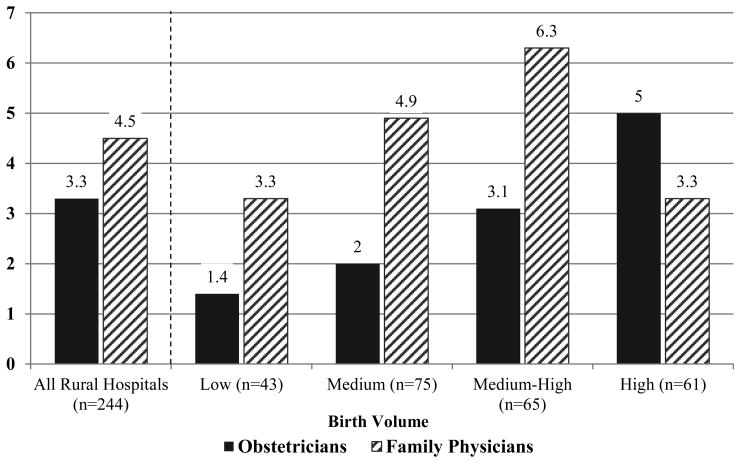
The relationship between birth volume and number of obstetricians is strong and positive. The mean number of obstetricians per hospital increases with birth volume, ranging from 1.4 in low-volume hospitals to 5 in high-volume hospitals (Figure 1). However, the relationship between birth volume and number of family physicians is slightly more complicated. The mean number of family physicians per hospital peaks at 6.3 in medium-high-volume hospitals, but it drops in high-volume hospitals to 3.3 family physicians, the same as hospitals with a low birth volume.
Figure 1. Average Number of Obstetricians and Family Physicians in Rural Hospitals by Birth Volume.
Notes: P values for significant differences across birth volume groups were from one-way ANOVA tests. Differences in number of obstetricians across birth volumes were statistically significant at P < .001. Differences in number of family physicians were not statistically significant.
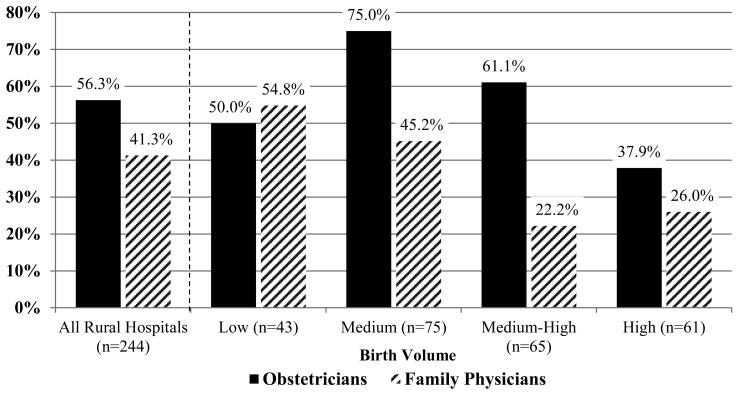
The proportions of obstetricians and family physicians who are employed by the hospital (vs in private practice) also differ significantly by hospital birth volume (Figure 2). On average, medium-birth-volume hospitals have the highest proportion (75%) of employed obstetricians, while low-birth-volume hospitals have the highest proportion (54.8%) of employed family physicians.
Figure 2. Proportion of Obstetricians and Family Physicians Employed by Rural Hospital (vs Private Practice), Stratified by Birth Volume.
Notes: P values for significant differences across birth volume groups were from one-way ANOVA tests. Differences in proportion of employed obstetricians across birth volumes were statistically significant at P < .001. Differences in proportion of employed family physicians were significant at P = .03.
Workforce Changes
Over half (55.7%) of the hospitals reported obstetric workforce changes over the past 3 years. These changes include both increases and decreases in the total number of clinicians providing obstetric care as well as one-for-one replacements of individual clinicians. More hospitals reported decreases in family physicians and obstetricians attending deliveries (24 and 28 hospitals, respectively) than those reporting increases (16 and 21 hospitals, respectively). This was not the case, however for CNMs, where 17 hospitals increased the number of CNMs and only 11 hospitals decreased their CNM workforce over the past 3 years (data not shown). The most commonly cited reasons for workforce decreases were that family physicians were no longer doing deliveries (11 hospitals) and clinicians had retired (7 hospitals).
Half of the hospitals expect changes in their obstetric workforce in the next 3 years. Among those anticipating staff changes, the majority are hoping to increase their workforce (77.3%). Respondents stressed the difficulty of recruiting needed obstetric providers in rural settings. In the words of one respondent: “We lost several midwives. We recruited a female OB to our team, but it is very hard to recruit in deeply rural country.” Another stated, “I expect a doctor to retire and then we don’t know what we will do. One provider can’t be on call 365 days a year. We have been recruiting for years, but it is hard to get an obstetric doctor to come to a small community.”
Challenges in Staffing Rural Obstetric Units
Nearly all (98%) of the surveyed hospitals reported challenges in staffing their obstetric units. Our analysis of their responses revealed 5 themes: scheduling, training, recruitment and retention, census fluctuation, and intra-hospital relationships (Table 3).
Table 3. Obstetric Staffing Challenges in Surveyed Rural Hospitals (N=238).
| Main Challenges | Description | Frequency |
|---|---|---|
| Scheduling | Scheduling obstetric nurses, dealing with vacation, sick, medical, maternity leaves; covering night shifts and weekends; getting nurses to be on call and on-call nurses to come in when needed | 88 (36.2%) |
| Training | Difficulty in getting access to training; maintaining nurse competencies in low- birth-volume settings; need to cross-train nurses for obstetrics and other areas of hospital | 56 (23.0%) |
| Recruitment and Retention | Recruiting and retaining qualified physicians or nurses, including dealing with turnover and having enough staff overall | 50 (20.6%) |
| Census Fluctuation | Not having enough nurses when census is high; having to have nurses on unit during times of low census | 48 (19.8%) |
| Intra-Hospital Relationships | Others do not understand high risk nature of obstetrics or why it is difficult to follow guidelines and meet productivity standards; difficulty in justifying obstetric nurse staffing to administration when census is low; financial issues related to obstetric unit staffing | 29 (11.9%) |
Notes: Hospitals could report more than one type of staffing challenge. Six hospitals reported no staffing challenges.
Scheduling obstetric nurse staff, including dealing with vacation, sick, medical, and maternity leaves; covering night shifts and weekends; and managing on-call systems, was the most common challenge, reported by 36.2% of hospitals.
Many rural hospitals find it difficult to access training opportunities and maintain staff competencies in low-birth-volume settings. One respondent explained, “We have to travel a long way for training—2 to 3 hours.” Another stated, “We have so few deliveries that it is difficult to keep staff fully trained.” Hospitals with lower birth volumes also have more fluctuation in their obstetric patient load, “the flux of increased number of deliveries and then down time. At times I may need 5 nurses and other times I need 2. I don't have a consistent flow of patients.”
Challenges with recruiting and retaining obstetric providers were reported by 21% of the hospitals. The vast majority of responses related to nursing staff, including dealing with turnover and having enough nursing staff overall for the unit. One respondent said, “In rural hospitals, the challenge is finding competent nurses who are willing to live in a rural area…it's hard to attract skilled nursing to a rural setting.” Others explained the challenges as “finding obstetric registered nurses that are qualified and willing to work in a low-volume hospital and willing to work in non-obstetric units.”
Twelve percent of the hospitals reported staffing challenges in relationships between the obstetric unit and the rest of the hospital. Specific concerns include difficulty in getting other hospital staff and administrators to understand the high-risk nature of obstetrics, following guidelines and meeting hospital productivity standards, justifying obstetric staffing when census is low, and financial issues related to obstetric unit staffing.
Limitations
The results from these 9 states may not be generalizable to other states, and while all 4 US Census regions were included, some sub-regions of the country are not represented in this analysis. Rural hospitals vary widely across regions, level of rurality, and different rural settings. However, the characteristics of the surveyed hospitals are similar to all rural hospitals with obstetric units, as reported in the AHA Annual Survey (Table 1). Hospital birth volume and degree of rurality are highly correlated. Thus, it is difficult to disentangle the effects of being in a highly rural or frontier location from the effects of very low birth volume in rural obstetric units. We achieved an 86% response rate among all rural hospitals with obstetric units in the surveyed states, and no statistical differences were detected between responding hospitals and those that did not respond after multiple attempts. However, it is possible that hospital non-response may introduce some bias. Survey responses were collected from only one person per hospital; others in the hospital may have had different perspectives.
Discussion
Many of the obstetric workforce challenges reported by surveyed hospitals, including recruitment and retention of obstetric clinicians, accessing training opportunities, and maintaining staff competencies, are related to their rural location and low birth volume.
Three-quarters of the surveyed rural hospitals anticipating future obstetric staffing changes are hoping to recruit more clinicians. Historically, rural hospitals have used a variety of educational, financial, regulatory, and support strategies to recruit and retain needed clinicians, with varying degrees of success.19 However, recruiting and retaining obstetric clinicians is especially challenging in light of decreases in the percentage of family physicians attending deliveries,9,10 predicted shortages in the overall supply of obstetricians,20 and the workload and on-call requirements inherent in obstetric practice.21 Our results suggest that hospital employment may be one strategy that rural hospitals are successfully using to recruit and retain obstetric clinicians. In fact, the surveyed rural hospitals are employing family physicians and obstetricians at a much higher rate than hospitals nationally.22
Three-quarters of surveyed hospitals have at least one obstetrician doing deliveries. Rural hospitals with lower birth volumes are more likely than those with higher volumes to have attending clinicians, such as family physicians and general surgeons, for whom obstetric care is only part of their clinical practice. Lower-volume hospitals are also more likely to have labor and delivery nurses who work in other areas of the hospital, rather than exclusively in maternity and newborn care. In addition, more than half of the surveyed rural hospitals have clinicians from more than one specialty (eg, obstetricians, family physicians, CNMs, and general surgeons) attending deliveries.
These staffing patterns reflect the realities of surveyed rural hospitals, where overall low patient volume and limited specialist supply means that physicians and nurses have a broader scope of practice than in larger urban facilities.6 However, having obstetric care as only part of a clinical practice and having clinicians from multiple specialties attend deliveries present additional challenges, with implications for training both during clinical education and in practice. These challenges are unlikely to be overcome by individual rural hospitals working in isolation, and policy solutions will likely require collaboration across hospital networks, health systems, regions, and states.
Policy Implications and Conclusions
Preparing Clinicians for Rural Obstetric Practice
The overall decline in provision of maternity care by family physicians and how to best structure residency training to prepare family physicians to provide these services have been debated by clinicians, professional associations, and residency programs for some time.23,24 A tiered training system has been proposed that would provide more advanced maternity care training to family medicine residents who are interested in providing prenatal and intrapartum care, and basic training for those who do not plan to provide maternity care.25 Although the Residency Review Committee for Family Medicine has not adopted the change, a national survey of obstetrics curriculum directors at family medicine residency programs indicated that 61% plan to offer advanced training, either in addition to basic training (41.7%) or alone (19.6%).26 More extensive and advanced maternity training could help interested family physicians be better prepared to practice obstetrics in rural areas.
With so many rural hospitals having clinicians from more than one specialty attending deliveries, the need for interprofessional education and training is clear, and medical and nursing education policies, standards and curricula can be adapted to reflect the reality of rural obstetric practice. Interprofessional education could help improve health care processes and patient outcomes27 and the practice culture of professionals working in rural areas.
Maintaining Skills in Low-Birth-Volume Settings
Beyond their initial clinical training, obstetric clinicians and nurses in rural settings could benefit from ongoing training to maintain competencies and improve skills, as well as structured opportunities to consult with specialists regarding obstetric complications. Training focused on addressing obstetric emergencies and rare events is especially important in low-birth-volume settings.
Interdisciplinary training programs such as the Advanced Life Support in Obstetrics (ALSO) program, an evidence-based program developed by the American Academy of Family Physicians to prepare clinicians to better manage obstetric emergencies, have been shown to improve clinical competency of providers delivering obstetric care,28 and they could be replicated in other rural settings.
Several studies have shown that team training using a simulation lab or mobile simulation equipment can effectively improve obstetric clinician skills and outcomes. Teamwork training in a simulation setting improved knowledge, practical skills, communication, and team performance in acute obstetric situations in 7 studies29 and improved perinatal outcomes in 3 studies.29-31
Obstetric simulation training initiatives have been successfully implemented in rural hospitals in Wisconsin32 and Oregon33 with funding from the Health Resources and Services Administration and the Agency for Healthcare Research and Quality, respectively. Many hospitals in our survey reported participating in obstetric quality improvement and patient safety initiatives in partnership with hospital networks, hospital systems, state hospital associations, state health departments, or other private and public partners. Building on these networks could offer opportunities for collaborative training efforts.
Other innovative models to help rural hospitals overcome training-related challenges include use of obstetric telemedicine to share resources and expertise in a region or state. Obstetric telemedicine programs in Arkansas and Tennessee are providing rural hospitals with maternal-fetal medicine specialty consultation regarding high-risk obstetric patients and continuing education for physicians and nurses.34,35
In summary, efforts to address health care workforce and access issues have accelerated with implementation of the Affordable Care Act. Federal and state policy makers, regional collaboratives, and health care delivery systems can facilitate solutions through support for programs such as interprofessional education, simulation training, and telemedicine.
Acknowledgments
Funding: Support for this research was provided by the Federal Office of Rural Health Policy, Health Resources and Services Administration (PHS Grant No. U1CRH03717). This work was also supported by the Building Interdisciplinary Research Careers in Women's Health Grant (K12HD055887) from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors wish to acknowledge the State Inpatient Databases, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality; our Rural Hospital Obstetric Advisory Group; the rural hospital survey respondents; the Office of Measurement Services at the University of Minnesota, for fielding the survey; and Alex Evenson, MA, for editing assistance.
References
- 1.Rayburn WF, Richards ME, Elwell EC. Drive times to hospitals with perinatal care in the United States. Obstet Gynecol. 2012;119(3):611–616. doi: 10.1097/AOG.0b013e318242b4cb. [DOI] [PubMed] [Google Scholar]
- 2.Grzybowski S, Stoll K, Kornelsen J. Distance matters: a population based study examining access to maternity services for rural women. BMC Health Serv Res. 2011;11(1):147–155. doi: 10.1186/1472-6963-11-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao L. Working paper #2007–04. Chapel Hill, NC: The Walsh Center for Rural Health Analysis; Apr, 2007. Why are fewer hospitals in the delivery business? cited 2014 August 8. [Google Scholar]
- 4.Simpson KR. An overview of distribution of births in United States hospitals in 2008 with implications for small volume perinatal units in rural hospitals. J Obstet Gynecol Neonatal Nurs. 2011;40(4):432–439. doi: 10.1111/j.1552-6909.2011.01262.x. [DOI] [PubMed] [Google Scholar]
- 5.Kozhimannil KB, Hung P, Prasad S, Casey M, McClellan M, Moscovice IS. Birth volume and the quality of obstetric care in rural hospitals. J Rural Health. 2014;30(4):335–43. doi: 10.1111/jrh.12061. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine Quality through collaboration: the future of rural health. Washington, DC: National Academy of Science Press; 2005. [Google Scholar]
- 7.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Health disparities in rural women. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2014;123:384–388. doi: 10.1097/01.AOG.0000443278.06393.d6. Committee Opinion No. 586. [DOI] [PubMed] [Google Scholar]
- 9.Cohen D, Coco A. Declining trends in the provision of prenatal care visits by family physicians. Ann Fam Med. 2009;7(2):128–133. doi: 10.1370/afm.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tong ST, Makaroff LA, Xierali IM, Puffer JC, Newton WP, Bazemore AW. Family physicians in the maternity care workforce: Factors influencing declining trends. Matern Child Health J. 2013;17(9):1576–1581. doi: 10.1007/s10995-012-1159-8. [DOI] [PubMed] [Google Scholar]
- 11.Thompson MJ, Lynge DC, Larson EH, Tachawachira P, Hart LG. Characterizing the general surgery workforce in rural America. Arch Surg. 2005;140(1):74–79. doi: 10.1001/archsurg.140.1.74. [DOI] [PubMed] [Google Scholar]
- 12.Bucklin BA, Hawkins JL, Anderson JR, Ullrich FA. Obstetric anesthesia workforce survey: twenty-year update. Anesthesiology. 2005;103(3):645–653. doi: 10.1097/00000542-200509000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Jukkala AM, Kirby RS. Challenges faced in providing safe care in rural perinatal settings. MCN The Am J Matern child Nurs. 2009;34(6):365–371. doi: 10.1097/01.NMC.0000363685.20315.0e. [DOI] [PubMed] [Google Scholar]
- 14.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94(10):1695–1703. doi: 10.2105/ajph.94.10.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldwin LM, Grossman DC, Murowchick E, et al. Trends in perinatal and infant health disparities between rural American Indians and Alaska natives and rural Whites. Am J Public Health. 2009;99(4):638–646. doi: 10.2105/AJPH.2007.119735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kocher R, Sahni NR. Hospitals’ race to employ physicians—the logic behind a money-losing proposition. N Engl J Med. 2011;364(19):1790–1793. doi: 10.1056/NEJMp1101959. [DOI] [PubMed] [Google Scholar]
- 17.Iglehart JK. Doctor-workers of the world, unite! Health Aff (Millwood) 2011;30(4):556–558. doi: 10.1377/hlthaff.2011.0286. [DOI] [PubMed] [Google Scholar]
- 18.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469–477. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 19.Lee DM, Nichols T. Physician recruitment and retention in rural and underserved areas. Int J Health Care Qual Assur. 2014;27(7):642–652. doi: 10.1108/ijhcqa-04-2014-0042. [DOI] [PubMed] [Google Scholar]
- 20.Satiani B, Williams T, Landon M, Ellison C, Gabbe S. A Critical Deficit of OBGYN Surgeons in the US by 2030. Surg Sci. 2011;2(02):95. [Google Scholar]
- 21.Dresden GM, Laura-Mae B, Andrilla CHA, Skillman SM, Benedetti TJ. Influence of Obstetric Practice on Workload and Practice Patterns of Family. Ann Fam Med. 2008:5–11. doi: 10.1370/afm.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kane CK, Emmons DW. New Data On Physician Practice Arrangements: Private Practice Remains Strong Despite Shifts Toward Hospital Employment. Chicago, IL: American Medical Association; 2013. [Google Scholar]
- 23.Nesbitt TS. Obstetrics in family medicine: can it survive? J Am Board Fam Pract. 2002;15(1):77–79. [PubMed] [Google Scholar]
- 24.American Academy of Family Physicians. [Accessed August 8, 2014];Maternal/Child Care (Obstetrics/Perinatal Care) Available from: http://www.aafp.org/about/policies/all/maternal-child.html.
- 25.Coonrod RA, Kelly BF, Ellert W, Loeliger SF, Rodney WM, Deutchman M. Tiered maternity care training in family medicine. Fam Med. 2011;42(9):631–637. [PubMed] [Google Scholar]
- 26.Meunier MR, Apgar BS, Ratcliffe SD, Mullan PB. Plans to accommodate proposed maternity care training requirements: a national survey of family medicine directors of obstetrics curricula. J Am Board Fam Med. 2012;25(6):827–831. doi: 10.3122/jabfm.2012.06.120132. [DOI] [PubMed] [Google Scholar]
- 27.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update) Cochrane Database Syst Rev. 2013;(3):CD002213. doi: 10.1002/14651858.CD002213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beasley JW, Dresang LT, Winslow DB, Damos JR. The Advanced Life Support in Obstetrics (ALSO®) Program: Fourteen Years of Progress. Prehosp Disaster Med. 2005;20(04):271–275. doi: 10.1017/s1049023x00002661. [DOI] [PubMed] [Google Scholar]
- 29.Merién AER, Van de Ven J, Mol BW, Houterman S, Oei SG. Multidisciplinary team training in a simulation setting for acute obstetric emergencies: a systematic review. Obstet Gynecol. 2010;115(5):1021–1031. doi: 10.1097/AOG.0b013e3181d9f4cd. [DOI] [PubMed] [Google Scholar]
- 30.Riley W, Davis S, Miller K, Hansen H, Sainfort F, Sweet R. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf. 2011;37(8):357–364. doi: 10.1016/s1553-7250(11)37046-8. [DOI] [PubMed] [Google Scholar]
- 31.Marshall NE, Vanderhoeven J, Eden KB, Segel SY, Guise JM. Impact of Simulation and Team Training on Postpartum Hemorrhage Management in Non-Academic Centers. J Matern Neonatal Med. 2014 May 29;:1–5. doi: 10.3109/14767058.2014.923393. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 32.RWHC Receives $254,431 Federal Grant for Simulation Equipment Project for Advancing Nurse Competency. Rural Wisconsin Health Cooperative News Release; Sep 1, 2010. [Accessed Feburary 9. 2015]. Available at: http://www.rwhc.com/Portals/0/papers/RWHC_HRSA_Nursing_Grant.pdf. [Google Scholar]
- 33.Curricula for obstetric emergency response drills and safety. Oregon State Obstetric and Pediatric Research Collaboration; [Accessed August 13, 2014]. Available from: http://www.obsafety.org/content/blogcategory/53/101. [Google Scholar]
- 34.Odibo IN, Wendel PJ, Magann EF. Telemedicine in obstetrics. Clin Obstet Gynecol. 2013;56(3):422–433. doi: 10.1097/GRF.0b013e318290fef0. [DOI] [PubMed] [Google Scholar]
- 35.Wood D. STORC helps deliver healthy babies: the telemedicine program that serves rural women with high-risk pregnancies. Telemed J E Health. 2011;17(1):2–4. doi: 10.1089/tmj.2011.9996. [DOI] [PubMed] [Google Scholar]