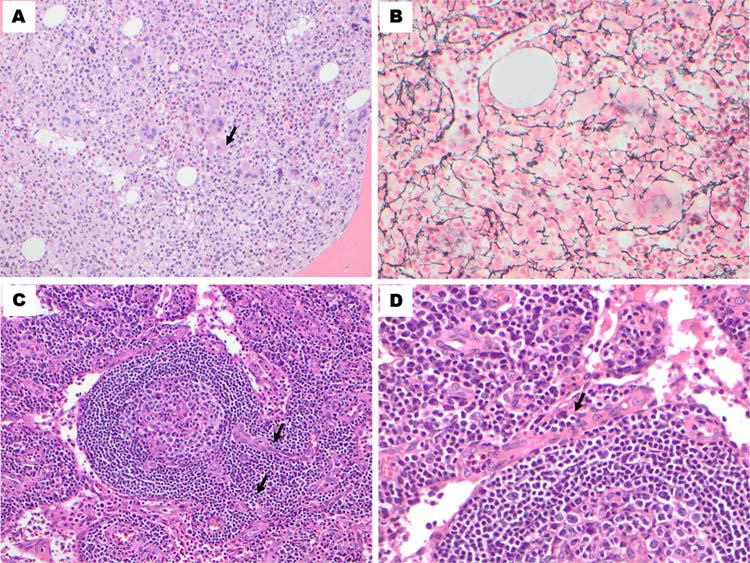
A 28-year-old man was referred to our institution in 2012 with a 3 month history of progressive weakness and fatigue, fever, night sweats, abdominal discomfort, shortness of breath, generalized swelling and an overall poor performance status. His initial investigations showed hemoglobin 89 g/L, white blood cell 2.3 × 109/L, platelets 75 × 109/L, blood urea nitrogen 50 mg/dL, and creatinine 2.5 mg/dL. Physical examination showed diffuse lymphadenopathy and splenomegaly. Computerized tomography scan showed diffuse lymphadenopathy (including mediastinal and retroperitoneal), pleural effusions and massive splenomegaly. Bone marrow (BM) evaluation revealed a hypercellular marrow (90%) showing atypical megakaryocytic hyperplasia with aberrant clustering and frequent nuclear hyperlobulation (Fig. 1A; Hematoxylin and Eosin H&E: 200× magnification). Blasts were not increased. A reticulin stain demonstrated coarse fibers with many interconnections (Fig. 1B; 400×) with an overall MF-2 grade fibrosis. The trabeculated bone was mildly thickened. Cytogenetic analysis of the BM aspirate demonstrated a diploid male karyotype. Molecular studies were negative for a BCR/ABL-1 fusion as well as JAK-2, MPL, and CALR mutations. An inguinal lymph node biopsy demonstrated germinal center regression with vessels extending into the germinal centers, exhibiting the so-called “lollipop” morphology (Fig. 1C,H,E; 200×). The interfollicular regions were expanded by numerous mature-appearing plasma cells and high endothelial venules (Fig. 1D,H,E; 400×). Anti-CD138 immunohistochemistry highlighted numerous plasma cells, which showed polytypic kappa and lambda light chain expression. There was no immunophenotypic aberrancy by flow cytometry analysis. The overall morphologic and immunophenotypic findings supported Castleman's disease (CD) with mixed features of hyaline-vascular and plasma cell variants. At the outside hospital, the patient was treated with packed red blood cell transfusions and oral steroids with improvement in symptoms and cell counts. Our investigations showed elevated LDH and β2 micro-globulin, polymerase chain reaction positive for HHV-6 in the BM and negative for HHV-8, EBV, hepatitis viruses and HIV 1 and 2. Other infectious and autoimmune work up was negative. Serum IL-6 levels were normal (likely due to the steroids he has received at the outside hospital). The patient was treated with 4 weekly doses of single agent rituximab at 375 mg/m2. The patient had remarkable clinical improvement with the first dose of rituximab and after 4 doses achieved remission. After 16 months of follow up, the patient maintains a normal clinical examination, normalized blood counts, and is transfusion-independent. A recent BM biopsy showed minimal reticulin fibrosis and mild dysplasia in megakaryocytes.
Figure 1.
A–D: Histopathological features of the BM and the lymph node biopsy. A: The BM core biopsy showed a hypercellular marrow with megakaryocytic hyperplasia and frequent clustering. The megakaryocytes are variable in size with a subset showing hyperlobation of the nuclei. (H&E, 200×). B: There is diffuse and dense increase in reticulin fibers with numerous intersections. (Gomori's silver impregnation, 400×). C: Inguinal lymph node with a lymphocyte-depleted germinal center. The mantle zone lymphocytes are arranged in onion-skin-like concentric whorls. A vessel is extending into the germinal center (“lollipop” morphology) (H&E, 200×). D: The interfollicular regions are expanded by a proliferation of plasma cells and high endothelial venules (H&E, 400×).
CD and myelofibrosis are cytokine driven diseases [1]. Myelofibrosis with CD is uncommon. Our patient had evidence of thrombocytopenia, anasarca, fever, reticulin fibrosis, and organomegaly (TAFRO). The constellation of these features with polyserositis, and non HHV-8 CD with mixed histology was recently described as TAFRO syndrome or Castleman-Kojima disease [2–5]. Patients have an indolent disease course and respond well to immunosuppressive therapy. Presence of HHV-6 in the BM of this patient is interesting and indicates that a combination of factors (viruses, cytokines, and microenvironment) is responsible for promoting different lymphoproliferative disorders. Further studies are required to understand the pathogenesis of this novel clinical entity.
Footnotes
Conflicts of interest: All Authors have reviewed and approved the manuscript and do not have any disclosures/conflicts of interest.
References
- 1.Tefferi A, Vaidya R, Caramazza D, et al. Circulating interleukin (IL)-8, IL-2R, IL-12, and IL-15 levels are independently prognostic in primary myelofibrosis: A comprehensive cytokine profiling study. J Clin Oncol. 2011;29:1356–1363. doi: 10.1200/JCO.2010.32.9490. [DOI] [PubMed] [Google Scholar]
- 2.Takai K, Nikkuni K, Shibuya H, Hashidate H. [thrombocytopenia with mild bone marrow fibrosis accompanied by fever, pleural effusion, ascites and hepatosplenomegaly]. Rinsho Ketsueki. 2010;51:320–325. [PubMed] [Google Scholar]
- 3.Kawabata H, Takai K, Kojima M, et al. Castle-man-kojima disease (TAFRO syndrome): A novel systemic inflammatory disease characterized by a constellation of symptoms, namely, thrombocytopenia, ascites (anasarca), microcytic anemia, myelofibrosis, renal dysfunction, and organomegaly: a status report and summary of fukushima (6 june, 2012) and nagoya meetings (22 september, 2012). J Clin Exp Hematop. 2013;53:57–61. doi: 10.3960/jslrt.53.57. [DOI] [PubMed] [Google Scholar]
- 4.Kawabata H, Kotani S, Matsumura Y, et al. Successful treatment of a patient with multicentric castleman's disease who presented with throm bocytopenia, ascites, renal failure and myelofibrosis using tocilizumab, an anti-interleukin-6 receptor antibody. Intern Med. 2013;52:1503–1507. doi: 10.2169/internalmedicine.52.9482. [DOI] [PubMed] [Google Scholar]
- 5.Tedesco S, Postacchini L, Manfredi L, et al. Successful treatment of a caucasian case of multifocal castleman's disease with TAFRO syndrome with a pathophysiology targeted therapy - a case report. Exp Hematol Oncol. 2015;4:3. doi: 10.1186/2162-3619-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]