Abstract
In order to create a three-dimensional (3D) documentation of findings which can be reassessed if necessary by other experts, the research project ‘Virtopsy®’ was launched in the late 1990s. This project combined autopsy results with forensic imaging in the form of computed tomography, magnetic resonance tomography and 3D surface scanning. The success of this project eventually succeeded in convincing the courts in Switzerland to accept these novel methods as evidence. As opposition towards autopsies has grown over the last decades, Virtopsy also strives to find and elaborate additional methods which can answer the main forensic questions without autopsy. These methods comprise post-mortem angiography for illustration of the vascular bed and image-guided tissue and fluid sampling for histological, toxicological and microbiological examinations. Based on the promising results, post-mortem imaging, especially with 3D surface scanning, has meanwhile also been applied to living victims of assault, who have suffered patterned injuries due to bites, blows with objects, etc. In our opinion, forensic imaging is an objective method which offers the possibility for a reassessment of the findings by other experts, even after burial or cremation of the corpse, or healing of the injuries in living victims, thus leading to a greater security in court.
Keywords: Virtopsy, forensic imaging, magnetic resonance imaging, computed tomography, photogrammetry
1. Introduction
Although forensic science has experienced ground-breaking innovations in crime-scene investigation methods, genetics and toxicology, forensic pathology seems to have been subjected to a Sleeping Beauty sleep, still relying on time-old, evidence-based methods introduced centuries ago: namely the dissection of corpses and an oral description plus written documentation of the findings [1], augmented in the past decades by photography and X-ray examinations.
Even though clinical medicine adopted computed tomography (CT) and magnetic resonance imaging (MRI) and relies on the findings presented by these cross-sectional modalities for planning even the most complicated and intricate interventions, and a first forensic CT was performed in 1977 [2], forensic pathology somehow did not realize the potential of these novel examination techniques.
This is indeed surprising, as prosecutors and defence lawyers are, in our experience, often eager to test new methods to make their case.
Despite this obvious general disinterest (and on occasion downright enmity) towards cross-sectional imaging in forensic pathology, many different institutions have implemented CT in post-mortem investigations on a broad scale, such as groups from the Office of the Armed Forces Medical Examiners in the USA (Armed Forces Institute of Pathology, Washington, DC and Dover, DE), from Denmark (Copenhagen), Sweden (Linköping), Australia (Victorian Institute of Pathology, Melbourne) and the UK (University of Leicester).
In Switzerland, this revolution in forensic medicine started off in the late 1990s, when the Institute of Forensic Medicine of the University of Bern started a collaboration with the Scientific Service of the City Police of Zurich, aiming at documenting the surfaces of objects and bodies in a three-dimensional (3D) manner [3]. After the turn of the century, the Institute of Forensic Medicine in Bern started a collaboration with the institutes of Diagnostic Radiology and Neuroradiology of the University of Bern. The ambitious aim of this newly founded research project called Virtopsy® was to detect forensic findings in corpses using CT and MRI and to compare these with those obtained by autopsy [4–8].
The Virtopsy® project started off with surface documentation by 3D photogrammetry-based optical surface scanning, CT and MRI.
It evolved over the years, implementing other methods such as post-mortem biopsy and angiography. The initial hostility towards the project slowly succumbed and courses teaching the use of the Virtopsy methods were started in 2006.
This was indeed the beginning of a success story; forensic pathologists and radiologists from all over the world participating in these Virtopsy® courses returned to their home countries and often enough succeeded in implementing at least some of the learnt methods. In order to disseminate the experiences even further, the founders of the Virtopsy® project, Professors Michael Thali, Richard Dirnhofer and Peter Vock, edited a textbook dedicated to forensic imaging [9].
Now, over two decades after the first, nascent steps towards a new future in forensic medicine and pathology, it is definitely time to reflect on the achievements, the strengths, the weaknesses, the threats and the opportunities of forensic imaging.
2. Methods
To date, forensic imaging comprises two cross-sectional modalities, namely CT and MRI, which are augmented by minimally invasive techniques such as post-mortem angiography and biopsy, and 3D photogrammetry-based optical surface scanning. These methods are presented briefly below.
(a). Computed tomography
Computed tomography is the most frequent imaging tool in forensic pathology besides X-ray. With modern scanners, 2D and 3D reconstructions based on slice thicknesses of 0.5 mm are not only possible, but are becoming routine standard.
Although soft tissues can also be seen and assessed with CT, the main strength lies in the detection and depiction of foreign bodies (figure 1), fractures (figure 2), gas (figure 3) and fluid accumulations, such as blood [10–13].
Figure 1.
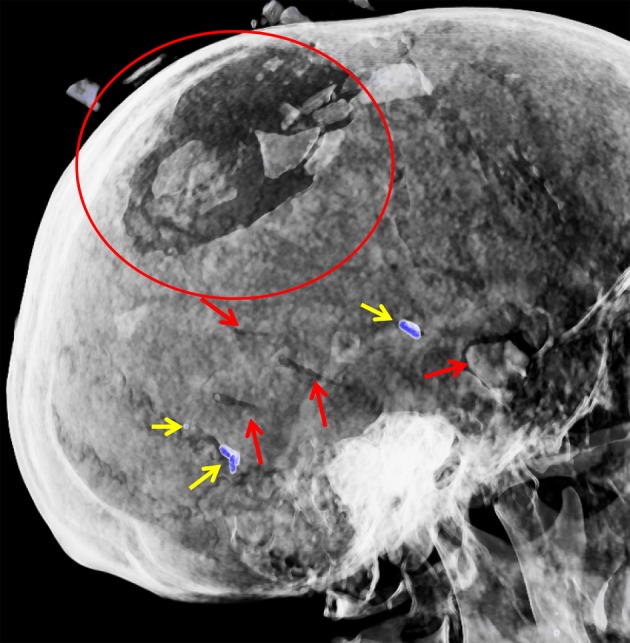
CT, 3D reconstruction of the skull of a homicide victim who was stabbed with a large kitchen knife. Besides a stab-induced fracturing of the skull (encircled) and multiple stab defects to the skull (red arrows), radiopaque fragments (coloured blue by the computer) are seen (yellow arrows). These fragments turned out to be knife tip fragments.
Figure 2.
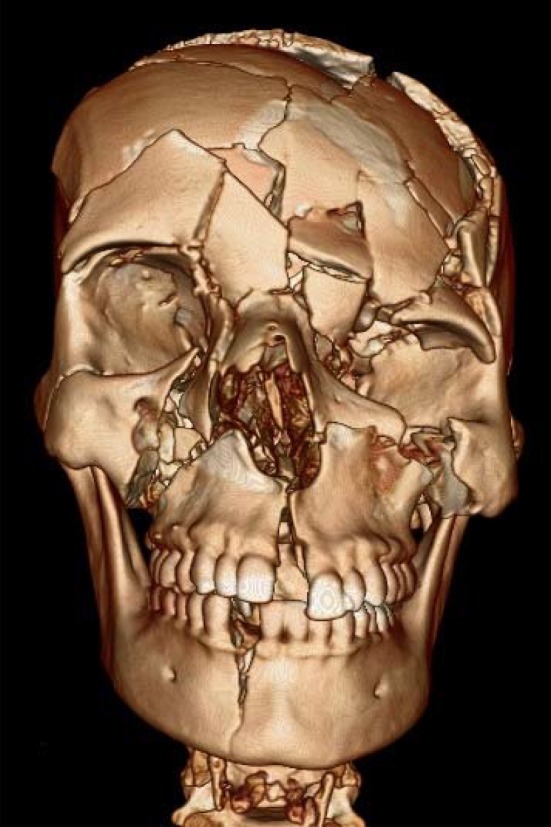
CT, 3D reconstruction of the skull of a young woman who fell from a window on the 4th floor. Note the extensive fractures.
Figure 3.
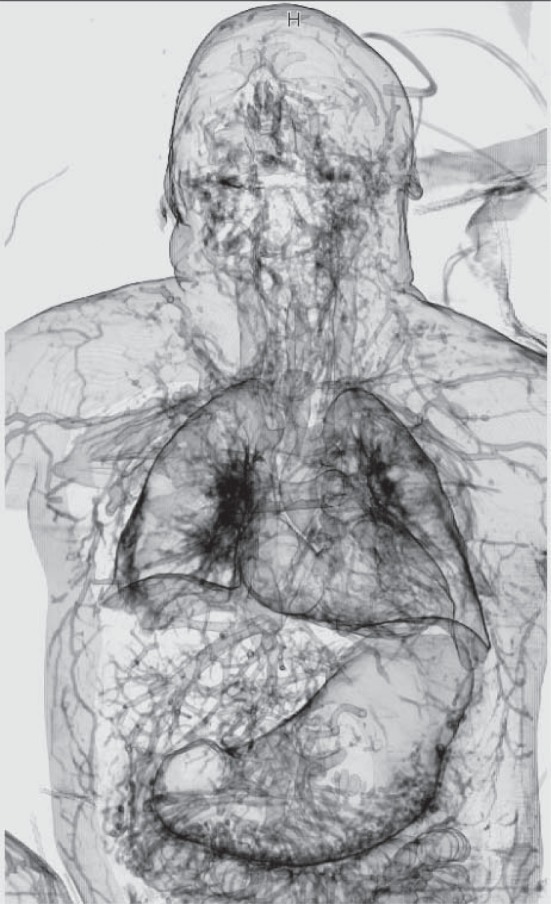
CT, 3D reconstruction of a fatal scuba diving accident. This reconstruction shows gas in the vascular bed throughout the body due to decompression disease.
Computed tomography can also show calcifications such as coronary sclerosis and larger vessels easily. However, the extent of vessel occlusion or a vascular rupture is, depending on the size of the vessel, difficult or impossible to appraise. This is where post-mortem angiography can be of great value (figure 4).
Figure 4.
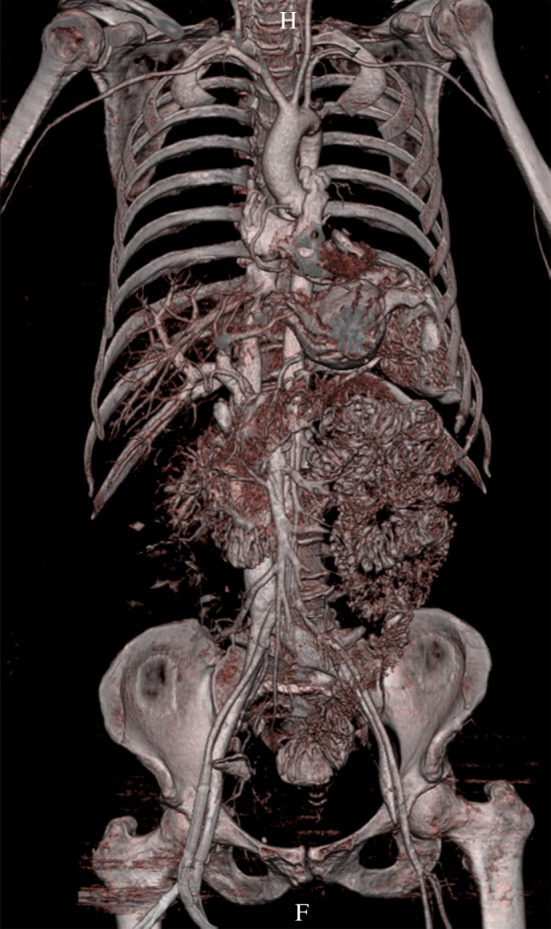
CT, 3D reconstruction of the arterial system after post-mortem angiography.
Although there are other groups using special pumps and contrast agents [14,15], our group uses a simple roller-pump, in order to administer an ionized water-soluble contrast medium mixed with polyethylene glycol [16–18] for whole-body post-mortem angiography.
(b). Magnetic resonance imaging
Although CT is the method of choice in showing foreign bodies, fractures and gas, it has limitations regarding the assessment of soft tissues and internal organs. MRI, by contrast, can depict soft-tissue injuries and pathologies clearly [19–22]. By virtue of this method being non-ionizing, it is also the imaging method of choice when examining living victims of assault, such as manual strangulation (figure 5) [23–25].
Figure 5.
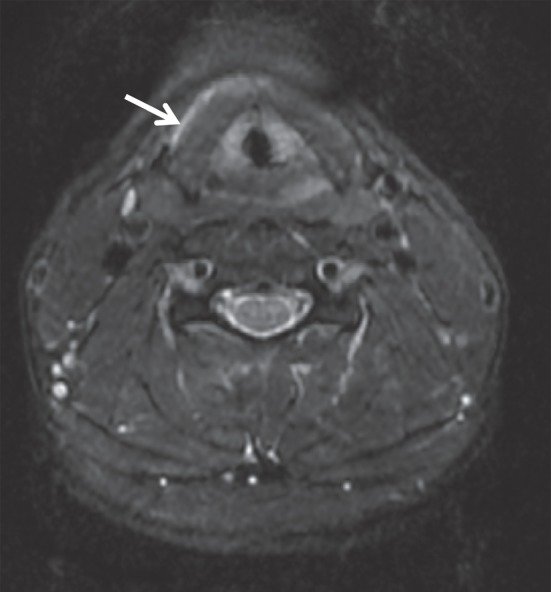
MRI (T2-weighted) of the neck of a victim of alleged manual strangulation at the level of the larynx. At external inspection, the skin of the neck only displayed very discreet superficial excoriations. MRI, however, showed a fluid (blood) accumulation (arrow) on the left side of the larynx.
(c). Post-mortem biopsy
Although the term ‘post-mortem biopsy’ is unfortunate, as the part ‘bios’ is ancient Greek for ‘life’ and is therefore, strictly speaking, not applicable for a post-mortem method, this terminology has established itself in forensic pathology in analogy to biopsies performed in clinical medicine. With a biopsy gun, samples of organs of interest, e.g. the heart, or specific pathologies seen at CT or MRI, e.g. tumours of unknown dignity, can be taken and examined histologically [26]. Also, tissue and fluid samples can be collected for toxicological and microbiological examinations.
Besides the manual sampling, image-guided sampling with a dedicated robot has been introduced recently [27–29].
(d). 3D photogrammetry-based optical surface scanning
With a surface-scanning unit, which projects a fringe pattern onto a surface and is in turn recorded by two cameras, a 3D image can be calculated using special software. Digital photography of the surface from different angles can then be added to the data, thus enabling a true colour 3D surface reconstruction. This very accurate documentation, which—depending on the applied resolution—can document structures less than 1 mm in size, is applicable not only for the documentation of vehicles (its original purpose in the automobile industry), but also for injuries in corpses and living victims [30,31] (figure 6).
Figure 6.
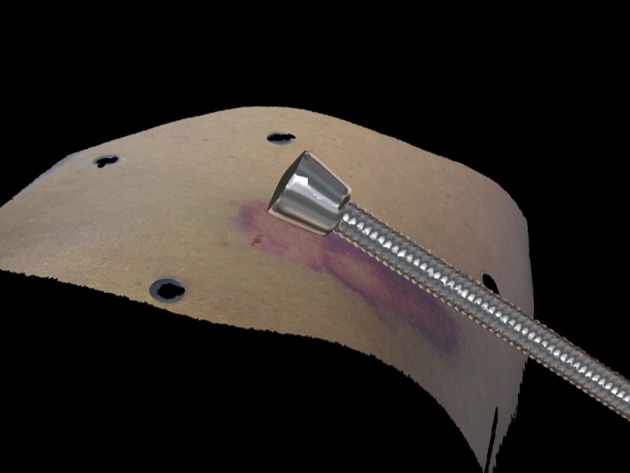
3D photogrammetry reconstruction of the skin of a living victim of physical assault with the weapon (truncheon) used.
3. Strengths
(a). Identification
One of the foremost questions in forensic pathology is the identity of the deceased. Not only does this enable the filling out of a death certificate and is obviously extremely important for the next-of-kin of a missing person, but it also serves to collect a deceased's biography, a feature which very often will affect further examinations.
The secure identification methods to date consist of a comparison of dental records, fingerprints and DNA of the corpse with ante-mortem data or DNA of blood-related family members.
With post-mortem CT, other singular traits enabling an identification of a corpse (or parts of it) beyond reasonable doubt can also be readily found. Such traits may be anatomical, such as the structure of the frontal sinus [32,33], degenerative changes of the skeleton such as the spine, healed fractures and unique calcifications. Surgical implants, i.e. the form of sternotomy wires, plates, screws, pacemakers, joint prostheses, etc., may also allow for identification of unknown corpses. As CT is a very rapid examination technique necessitating only a few minutes to perform, a great number of corpses can be scanned, a valuable feature in mass catastrophes [34–36].
(b). Foreign bodies
The detection of foreign bodies is indeed a cardinal aspect in forensic radiology. CT can, in addition to plain X-rays, depict a potential foreign body in a 3D manner in one single examination, as opposed to X-ray, in which images are taken from different angles, thus necessitating a sometimes tedious repositioning the corpse. This 3D depiction of the location of the foreign body facilitates its extraction tremendously. In X-rays, the size of the foreign object within a corpse can be difficult to assess; if the object is located near the X-ray source it will seem larger, if it is further away it will appear smaller. In CT, the object can be measured very accurately, very often in the dimension of less than one millimetre, regardless of where it is. The knowledge of the presence of a foreign body and its size, e.g. the calibre of a bullet, even before autopsy has begun, is to our experience very much appreciated by crime-scene investigators. Another aspect is that CT can measure the radiopacity of foreign bodies precisely in Hounsfield units (HU). As different materials possess different HU, a more or less precise determination of the material of which a foreign body consists can be rapidly made. This feature is especially valuable in explosion victims. These victims may be riddled by a multitude of foreign bodies, e.g. glass shards, brickwork, timber, etc., besides bomb fragments. Although foreign bodies such as brickwork or glass fragments may have killed the victim, they are of minimal importance for bomb investigators, who need to gather information on the type of bomb used in order to try to find the perpetrators. With the HU values determined by CT, possibly bomb-associated fragments, e.g. fragments consisting of steel, aluminium, copper, etc., can be located and extracted rapidly for further analysis [37].
(c). Adjuvant to autopsy
Several advantages arise due to the fact that forensic imaging does not necessitate a physical contact or severing of tissue in order to see findings. For example, in decomposing brains, the anatomical structures, i.e. the skull and the cerebral coverings, are left intact, so the cerebral tissues tend to keep their anatomical relation to each other. This facilitates assessment enormously compared with classical autopsy, where the decomposing, liquefying brain oozes out as a papescent mass after opening of the skull [38,39].
The fact that forensic imaging does not tamper with pre-existing structures can also be of assistance when assessing multiple comminute fractures of, for example, the skull after repeated blows or gunshots. At autopsy, one is forced to pull off the scalp, which may lead to the skull fragments dislodging, which in turn will make a painstaking and time-consuming reconstruction of the shattered skull necessary. With CT one can evaluate the fracture pattern reliably and easily and then, due to the fact that later fracture lines do not cross pre-existing ones, determine which blows or gunshots occurred first.
Another example is gas embolism; gas embolism diagnostic is difficult at autopsy, as, by opening the body, air will obviously enter the vascular system. For this reason, the heart is submerged in water filled into the pericardial sac and the cardiac chambers then punctured. If gas bubbles rise, then there was gas, e.g. air, within the heart. This classical method is inaccurate, as it only proves the presence of gas in the heart, and not if this gas was pumped into the vascular bed in the sense of an ‘embolism’ or how much gas there was. CT can show not only the presence but also the amount and distribution very accurately [40].
Certain areas of the human body are difficult to examine, for example the topmost region of the spinal cord, which is generally severed when extracting the brain at autopsy. CT can deliver information as to osseous lesions here, and with MRI it is even possible to assess the spinal cord. The face is another region in which post-mortem imaging is a valuable tool; in order for the next-of-kin to be able to see the corpse even after autopsy, the face is generally spared from dissection. With forensic imaging, the soft tissues and skeleton of the face can be examined in a non-destructive fashion.
(d). Adjuvant to external inspection
The surface of a victim, living or dead, is of utmost importance in medico-legal examinations. Beside traces such as DNA and fibres, etc., patterned injuries very often lead to identification of the injury-causing object or structure, and may eventually solve the case.
Obviously, a thorough visual examination is of paramount importance. Indeed, in our experience, the external examination of a corpse may often exceed the actual autopsy or examination of the internal findings with regard to time and documentation.
However, photographs reduce a 3D finding to a 2D image, a feature which may affect future reappraisals negatively. Sketches and written reports are subject to an examiner's interpretation and are therefore not an objective documentation method. With 3D photogrammetry-based optical scanning, external findings can be documented in an objective, 3D, and readily reproducible fashion. With these data, the injury inflicting object or structure of a vehicle can be identified [30,31].
Although autopsy is the traditional method of documenting internal findings in corpses, this obviously does not apply to living victims. In the medico-legal assessment of, for example, a person who claims to have been subjected to manual strangulation, one may or may not detect evidence supporting this claim. This forces the examiner to rely on statements given by the examined person, which may be inaccurate or downright false. With MRI, by contrast, lesions to the deeper soft tissues of the neck, otherwise unseen at external, forensic-clinical inspection, may be documented and prove blunt trauma, thus supporting the victim's claim in an objective, reproducible fashion [23–25].
(e). Demonstration at court
Although many judges, district and defence attorneys and jurors accumulate a certain medical knowledge over the years and are often advised by physicians, they are essentially medical laymen. A clear and understandable presentation of the findings is absolutely essential if these medical laymen are to understand the presented findings properly and thus (hopefully) judge correctly. Typical ‘blood-and-guts’ photographs of autopsies, often presented at court, do not necessarily help in giving a neutral, fact-based verdict, as especially jurors may be emotionally influenced by such images or reluctant to study them with the necessary attention due to an intense aversion to the documentation. Forensic imaging can be of help in these situations; indeed, it is our experience, that ‘clean’, bloodless images are easier to appreciate than a photograph of an opened body in which only a physician acquainted with such images may see and appreciate the findings and draw the proper conclusions.
To date, as post-mortem imaging is an emerging discipline, our group only presents radiological findings together with autopsy findings at court. Radiological findings such as fractures, retained bullets, knife tips, which are readily distinguishable even by medical laypersons, have, according to our experience, never been challenged at court. However, more discreet findings such as pneumonic infiltrates, etc. have given rise to discussion and should only be presented in combination with fully established methods.
Furthermore, the stored data can be retrieved long after burial or cremation of a corpse or healing of the wounds of a living victim, thus allowing for a new assessment by a different expert should the need arise.
4. Weaknesses and threats
Apart from surface scanning, post-mortem imaging lacks an important feature that classic methods possess, namely colour. Colour, as well as the texture and smell of an organ are important diagnostics which cannot be shown at forensic imaging. Another aspect complicating forensic imaging is a potential lack of knowledge regarding the visual evidence. Forensic radiology is not clinical radiology performed on a corpse; indeed, forensic radiologists encounter a vast amount of findings that a clinical radiologist will never have seen, such as livores, which in the lungs are easily misinterpreted as pneumonia, or putrefaction gases in the soft tissues mimicking emphysema, or maggots, which confound clinical radiologists completely, just to name a few such findings.
Additionally, advanced putrefaction or extensive lacerations may also render certain methods such as post-mortem angiography inapplicable, as the disintegrating or destroyed vascular bed will not be able to keep the contrast medium sufficiently for assessment to be possible.
Furthermore, due to the fact that forensic radiology is a new discipline, there is still a general lack of experience in the interpretation.
A caveat deserves mentioning: many natural causes of death are difficult to determine with post-mortem imaging and the most common cause of sudden and unexpected death, namely arrhythmogenic coronary artery disease, cannot be diagnosed. However, this also applies for autopsy in such cases, as these cases often only display coronary stenosis or occlusions, possibly in combination with cardiac hypertrophy and unspecific findings such as pulmonary congestion. Here, if at all, the diagnosis is based on exclusion of other causes of death and the possible, albeit rare, presence of histological changes in the cardiac musculature.
And last, but unfortunately not least, there are pecuniary issues. In many countries, even in the so-called ‘first world’, not every larger hospital possesses its own CT, let alone an MR unit. It goes without saying that, should finances be made available, these will primarily be allocated to help the living, and not for examining corpses. Therefore, even though many forensic pathologists today would very much embrace post-mortem imaging, the lack of money will prevent such undertakings.
Apart from this, there is the issue of who should pay for such examinations. In Switzerland, even middle-sized hospitals and every university-based Institute of Forensic Medicine possess at least a CT. Although clinical CT and MR scanners are perfectly suitable for forensic purposes, there may be difficulties arising out of the sharing of such units for forensic and clinical purposes. For example, not many clinics (or patients) will be fond of the notion of scanning patients after a decomposed, maggot-ridden corpse has been in the machine before. Furthermore, most clinical radiology departments have more than enough workload themselves without having to deal with forensic cases. For this reason, specially dedicated forensic imaging units, such as ours, are definitely advisable.
Furthermore, the district attorneys, under pressure from the cantonal governments, are forced to save money and will therefore occasionally object to a rather cost-intensive examination in addition to the already expensive forensic autopsy.
5. Opportunities
Despite the above-mentioned weaknesses and threats, there are, according to our experience, many opportunities for forensic imaging in the future.
The drawback of not being able to assess the colour and texture of organs can be relativized; firstly, the main question posed to the forensic pathologist is whether there are signs of a third-party involvement. Gross injuries, especially regarding the more critical regions of the body such as the head, neck and trunk are adequately examinable using CT and, if need be, MRI.
If these cross-sectional modalities do not suffice to determine the cause, and, more importantly, the manner of death, then toxicology and/or microbiological analysis are warranted, just as in conventional autopsies. In order to take samples for such examinations, one can either take blood, tissue and urine samples with manual autopsy, or in an image-guided fashion using a robot. This approach is very promising, as it may reduce the risk of infection of autopsy technicians and pathologists. Especially in the light of the possibly upcoming Ebola epidemic, the minimally invasive examination of corpses without autopsy is certainly not unattractive.
However, not only infections may give rise to hesitation towards performing an autopsy. Different religious beliefs, e.g. Judaism, explicitly prohibit autopsy. The Koran does not literally prohibit it, but says that breaking a dead person's bones is comparable to breaking a living persons bones, which implies that autopsies are not welcomed in Islam either. Besides religious beliefs, many people object to autopsies for a number of reasons, the most prevalent in our experience being that the peace of the dead may be disturbed. These cultural, religious and personal aversions towards autopsy stand in contrast to a modern judicial system, in which the possibility of foul play must be examined and perpetrators must be brought to justice. With post-mortem imaging, the district attorney has a triage tool based on which he may either deem a case as being clear or deserving further attention, if need be with autopsy against the will of the relatives.
Against a background of a reducing rate of autopsies, many forensic pathologists object to post-mortem imaging as they fear further reduction of autopsies. This is, in our opinion, not justified. A very likely future scenario may be that more deceased receive a preliminary external inspection and CT, and, based on the results, receive an autopsy. This would lead to a far larger percentage of post-mortem examinations, lead to a higher homicide detection rate and, as more examinations overall take place, not even lead to a relevant reduction of autopsy numbers. Obviously, medical examiners and radiologists should be trained in forensic imaging in order to detect possible signs of foul play. Therefore, additional training is of paramount importance. Such additional training—besides on the job teaching—is offered by annual meetings such as those of the International Society of Forensic Radiology and Imaging (ISFRI) as well as the meanwhile well-established ‘Virtopsy Basic’ and ‘Virtopsy Advanced’ courses.
Another great opportunity of forensic imaging is the possibility of reassessing a case. The obtained and stored data can, for example, be assessed by an appropriate expert of a specific subspecialty anywhere at any time. By being able to involve other specialists, the case will be dealt with in an optimal manner. This is not only true for possible criminal cases; in mass catastrophes, a multitude of corpses can be scanned with mobile CT units at the incident location. This would require only a minimum of trained personnel at the location. The obtained data could be sent to a distinct location, preferably where most missing persons came from, examined by forensic radiologists there and compared with ante-mortem data, thus enabling a rapid processing of corpse identifications.
6. Afterword
No commander-in-chief will wage war relying on one type of force alone; depending on the situation, he will employ the infantry, artillery, mechanized troops, the air force, etc. The same should also apply for forensic medicine; depending on the situation, a medical examiner should be able to resort to the most appropriate, or a combination of the most appropriate methods, be it autopsy, forensic imaging, surface scanning, etc.
In our opinion, it is irrelevant who gives expert advice to the court, be it the forensic pathologist, the forensic anthropologist, the forensic toxicologist or even the forensic radiologist. The main issue is that the court receives an optimum in facts and findings, therefore improving justice.
Summarizing the above, the main question which should be asked is how much a country and its judicial system are willing to invest in an improved court system and greater protection of its people from crime and terror.
Acknowledgements
We are deeply obliged to the members of the Virtopsy group; without their invaluable support, this article would not have been possible. We would also like to thank Renate and Werner Bolliger, PhD, for language editing of the manuscript.
Competing interests
We declare we have no competing interests.
Funding
We received no funding for this study.
References
- 1.Lundberg GD. 1998. Low-tech autopsies in the era of high-tech medicine: continued value for quality assurance and patient safety. J. Am. Med. Assoc. 280, 1273–1274. ( 10.1001/jama.280.14.1273) [DOI] [PubMed] [Google Scholar]
- 2.Wüllenweber R, Schneider V, Grumme T. 1977. [A computer-tomographical examination of cranial bullet wounds]. Z. Rechtsmed. 80, 227–246. ( 10.1007/BF02114619). [In German.] [DOI] [PubMed] [Google Scholar]
- 3.Thali MJ, Braun M, Brüschweiler W, Dirnhofer R. 2000. Matching tire tracks on the head using forensic photogrammetry. Forensic Sci. Int. 113, 281–287. ( 10.1016/S0379-0738(00)00234-6) [DOI] [PubMed] [Google Scholar]
- 4.Thali MJ, Schweitzer W, Yen K, Vock P, Ozdoba C, Spielvogel E, Dirnhofer R. 2003. New horizons in forensic radiology: the 60-second digital autopsy–full-body examination of a gunshot victim by multislice computed tomography. Am. J. Forensic Med. Pathol. 24, 22–27. ( 10.1097/01.PAF.0000050694.17624.B1) [DOI] [PubMed] [Google Scholar]
- 5.Thali MJ, et al. 2003. Virtopsy, a new imaging horizon in forensic pathology: virtual autopsy by postmortem multislice computed tomography (MSCT) and magnetic resonance imaging (MRI)—a feasibility study. J. Forensic Sci. 48, 386–403. [PubMed] [Google Scholar]
- 6.Thali MJ, Braun M, Wirth J, Vock P, Dirnhofer R. 2003. 3D surface and body documentation in forensic medicine: 3-D/CAD photogrammetry merged with 3D radiological scanning. J. Forensic Sci. 48, 1356–1365. [PubMed] [Google Scholar]
- 7.Thali MJ, Yen K, Vock P, Ozdoba C, Kneubuehl BP, Sonnenschein M, Dirnhofer R. 2003. Image-guided virtual autopsy findings of gunshot victims performed with multi-slice computed tomography and magnetic resonance imaging and subsequent correlation between radiology and autopsy findings. Forensic Sci. Int. 138, 8–16. ( 10.1016/S0379-0738(03)00225-1) [DOI] [PubMed] [Google Scholar]
- 8.Yen K, et al. 2004. Virtopsy: forensic traumatology of the subcutaneous fatty tissue; multislice computed tomography (MSCT) and magnetic resonance imaging (MRI) as diagnostic tools. J. Forensic Sci. 49, 799–806. ( 10.1520/JFS2003299) [DOI] [PubMed] [Google Scholar]
- 9.Thali M, Dirnhofer R, Vock P. (eds). 2010. The Virtopsy approach: 3D optical and radiological scanning and reconstruction in forensic medicine. Boca Raton, FL: CRC Press, Taylor & Francis. [DOI] [PubMed] [Google Scholar]
- 10.Le Blanc-Louvry I, Thureau S, Duval C, Papin-Lefebvre F, Thiebot J, Dacher JN, Gricourt C, Touré E, Proust B. 2013. Post-mortem computed tomography compared to forensic autopsy findings: a French experience. Eur. Radiol. 23, 1829–1835. ( 10.1007/s00330-013-2779-0) [DOI] [PubMed] [Google Scholar]
- 11.Leth PM. 2009. Computerized tomography used as a routine procedure at postmortem investigations. Am. J. Forensic Med. Pathol. 30, 219–222. ( 10.1097/PAF.0b013e318187e0af) [DOI] [PubMed] [Google Scholar]
- 12.Levy AD, Abbott RM, Mallak CT, Getz JM, Harcke HT, Champion HR, Pearse LA. 2006. Virtual autopsy: preliminary experience in high-velocity gunshot wound victims. Radiology 240, 522–528. ( 10.1148/radiol.2402050972) [DOI] [PubMed] [Google Scholar]
- 13.Zech WD, Jackowski C, Buetikofer Y, Kara L. 2014. Characterization and differentiation of body fluids, putrefaction fluid, and blood using Hounsfield unit in postmortem CT. Int. J. Legal Med. 128, 795–802. ( 10.1007/s00414-014-1030-0) [DOI] [PubMed] [Google Scholar]
- 14.Grabherr S, et al. 2011. Multi-phase post-mortem CT angiography: development of a standardized protocol. Int. J. Legal Med. 125, 791–802. ( 10.1007/s00414-010-0526-5) [DOI] [PubMed] [Google Scholar]
- 15.Grabherr S, et al. 2008. Two-step postmortem angiography with a modified heart-lung machine: preliminary results. Am. J. Roentgenol. 190, 345–351. ( 10.2214/AJR.07.2261) [DOI] [PubMed] [Google Scholar]
- 16.Ross S, Spendlove D, Bolliger S, Christe A, Oesterhelweg L, Grabherr S, Thali MJ, Gygax E. 2008. Postmortem whole-body CT angiography: evaluation of two contrast media solutions. Am. J. Roentgenol. 190, 1380–1389. ( 10.2214/AJR.07.3082) [DOI] [PubMed] [Google Scholar]
- 17.Ruder TD, Hatch GM, Ebert LC, Flach PM, Ross S, Ampanozi G, Thali MJ. 2012. Whole body postmortem magnetic resonance angiography. J. Forensic Sci. 57, 778–782. ( 10.1111/j.1556-4029.2011.02037.x) [DOI] [PubMed] [Google Scholar]
- 18.Ross SG, Bolliger SA, Ampanozi G, Oesterhelweg L, Thali MJ, Flach PM. 2014. Postmortem CT angiography: capabilities and limitations in traumatic and natural causes of death. Radiographics 34, 830–846. ( 10.1148/rg.343115169) [DOI] [PubMed] [Google Scholar]
- 19.Bisset RA, Thomas NB, Turnbull IW, Lee S. 2002. Postmortem examinations using magnetic resonance imaging: four year review of a working service. Br. Med. J. 324, 1423–1424. ( 10.1136/bmj.324.7351.1423) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patriquin L, Kassarjian A, Barish M, Casserley L, O'Brien M, Andry C, Eustace S. 2001. Postmortem whole-body magnetic resonance imaging as an adjunct to autopsy: preliminary clinical experience. J. Magn. Reson. Imaging 13, 277–287. () [DOI] [PubMed] [Google Scholar]
- 21.Ros PR, Li KC, Vo P, Baer H, Staab EV. 1990. Preautopsy magnetic resonance imaging: initial experience. Magn. Reson. Imaging 8, 303–308. ( 10.1016/0730-725X(90)90103-9) [DOI] [PubMed] [Google Scholar]
- 22.Ross S, Ebner L, Flach P, Brodhage R, Bolliger SA, Christe A, Thali MJ. 2012. Postmortem whole-body MRI in traumatic causes of death. Am. J. Roentgenol. 199, 1186–1192. ( 10.2214/AJR.12.8767) [DOI] [PubMed] [Google Scholar]
- 23.Christe A, Oesterhelweg L, Ross S, Spendlove D, Bolliger S, Vock P, Thali MJ. 2010. Can MRI of the neck compete with clinical findings in assessing danger to life for survivors of manual strangulation? A statistical analysis. Leg. Med. (Tokyo) 12, 228–232. ( 10.1016/j.legalmed.2010.05.004) [DOI] [PubMed] [Google Scholar]
- 24.Christe A, et al. 2009. Life-threatening versus non-life-threatening manual strangulation: are there appropriate criteria for MR imaging of the neck? Eur. Radiol. 19, 1882–1889. ( 10.1007/s00330-009-1353-2) [DOI] [PubMed] [Google Scholar]
- 25.Yen K, Thali MJ, Aghayev E, Jackowski C, Schweitzer W, Boesch C, Vock P, Dirnhofer R, Sonnenschein M. 2005. Strangulation signs: initial correlation of MRI, MSCT, and forensic neck findings. J. Magn. Reson. Imaging 22, 501–510. ( 10.1002/jmri.20396) [DOI] [PubMed] [Google Scholar]
- 26.Bolliger SA, Filograna L, Spendlove D, Thali MJ, Dirnhofer S, Ross S. 2010. Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. Am J Roentgenol. 195, 1051–1056. ( 10.2214/AJR.10.4600) [DOI] [PubMed] [Google Scholar]
- 27.Ebert LC, Ptacek W, Naether S, Fürst M, Ross S, Buck U, Weber S, Thali M. 2010. Virtobot—a multi-functional robotic system for 3D surface scanning and automatic post mortem biopsy. Int. J. Med. Robot. 6, 18–27. ( 10.1002/rcs.285) [DOI] [PubMed] [Google Scholar]
- 28.Martinez RM, Ptacek W, Schweitzer W, Kronreif G, Fürst M, Thali MJ, Ebert LC. 2014. CT-guided, minimally invasive, postmortem needle biopsy using the B-Rob II needle-positioning robot. J. Forensic Sci. 59, 517–521. ( 10.1111/1556-4029.12329) [DOI] [PubMed] [Google Scholar]
- 29.Ebert LC, Ptacek W, Breitbeck R, Fürst M, Kronreif G, Martinez RM, Thali M, Flach PM. 2014. Virtobot 2.0: the future of automated surface documentation and CT-guided needle placement in forensic medicine. Forensic Sci. Med. Pathol. 10, 179–186. ( 10.1007/s12024-013-9520-9) [DOI] [PubMed] [Google Scholar]
- 30.Buck U, et al. 2007. Application of 3D documentation and geometric reconstruction methods in traffic accident analysis: with high resolution surface scanning, radiological MSCT/MRI scanning and real data based animation. Forensic Sci. Int. 170, 20–28. ( 10.1016/j.forsciint.2006.08.024) [DOI] [PubMed] [Google Scholar]
- 31.Bolliger MJ, Buck U, Thali MJ, Bolliger SA. 2012. Reconstruction and 3D visualisation based on objective real 3D based documentation. Forensic Sci. Med. Pathol. 8, 208–217. ( 10.1007/s12024-011-9288-8) [DOI] [PubMed] [Google Scholar]
- 32.Dedouit F, Savall F, Mokrane FZ, Rousseau H, Crubézy E, Rougé D, Telmon N. 2014. Virtual anthropology and forensic identification using multidetector CT. Br. J. Radiol. 87, 20130468 ( 10.1259/bjr.20130468) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim DI, Lee UY, Park SO, Kwak DS, Han SH. 2013. Identification using frontal sinus by three-dimensional reconstruction from computed tomography. J. Forensic Sci. 58, 5–12. ( 10.1111/j.1556-4029.2012.02185.x) [DOI] [PubMed] [Google Scholar]
- 34.Ruder TD, Kraehenbuehl M, Gotsmy WF, Mathier S, Ebert LC, Thali MJ, Hatch GM. 2012. Radiologic identification of disaster victims: a simple and reliable method using CT of the paranasal sinuses. Eur. J. Radiol. 81, e132–e138. ( 10.1016/j.ejrad.2011.01.060) [DOI] [PubMed] [Google Scholar]
- 35.Leditschke J, Collett S, Ellen R. 2011. Mortuary operations in the aftermath of the 2009 Victorian bushfires. Forensic Sci. Int. 205, 8–14. ( 10.1016/j.forsciint.2010.11.002) [DOI] [PubMed] [Google Scholar]
- 36.Rutty GN, Robinson C, Morgan B, Black S, Adams C, Webster P. 2009. Fimag: the United Kingdom disaster victim/forensic identification imaging system. J. Forensic Sci. 54, 1438–1442. ( 10.1111/j.1556-4029.2009.01175.x) [DOI] [PubMed] [Google Scholar]
- 37.Ruder TD, Thali Y, Bolliger SA, Somaini-Mathier S, Thali MJ, Hatch GM, Schindera ST. 2013. Material differentiation in forensic radiology with single-source dual-energy computed tomography. Forensic Sci. Med. Pathol. 9, 163–169. ( 10.1007/s12024-012-9398-y) [DOI] [PubMed] [Google Scholar]
- 38.Thali MJ, Yen K, Schweitzer W, Vock P, Ozdoba C, Dirnhofer R. 2003. Into the decomposed body-forensic digital autopsy using multislice-computed tomography. Forensic Sci. Int. 134, 109–114. ( 10.1016/S0379-0738(03)00137-3) [DOI] [PubMed] [Google Scholar]
- 39.Bolliger SA, Thali MJ. 2010. Decomposition. In The Virtopsy approach: 3D optical and radiological scanning and reconstruction in forensic medicine (eds Thali M, Dirnhofer R, Vock P.). Boca Raton, FL: CRC Press, Taylor & Francis. [Google Scholar]
- 40.Jackowski C, Thali M, Sonnenschein M, Aghayev E, Yen K, Dirnhofer R, Vock P. 2004. Visualization and quantification of air embolism structure by processing postmortem MSCT data. J. Forensic Sci. 49, 1339–1342. ( 10.1520/JFS2004047) [DOI] [PubMed] [Google Scholar]


