Abstract
Herpes zoster is an infectious disease with neurological complications caused by reactivation of varicella zoster virus in dorsal root ganglia of spinal cord which is also known as “Shingles.” Suppression of immune system is the major predisposing factor for reactivation of latent virus. Disease is mainly characterized by rash, vesicles and pain along one or more dermatomes which are innervated from one or more spinal nerve roots. Complications may be present after a while despite of patient treatment. Motor involvement is included. Some previous studies showed segmental zoster paresis as a rare complication, a few weeks after first presentation, among immunocompetent individuals. We present post herpetic motor involvement of C5 and C6 in a 59-year-old woman who underwent chemotherapy and radiotherapy due to breast cancer, manifesting left upper limb weakness and paresis, 6 months after left partial mastectomy. Segmental paresis of zoster virus should be considered as a cause of motor impairment in an immunocompromised person suffering from shingles.
Keywords: Breast cancer, herpes zoster, segmental paresis
INTRODUCTION
Herpes zoster, which is also known as shingles or zona, results from reactivation of latent varicella zoster virus in dorsal root ganglions. The clinical manifestations of herpes zoster are painful unilateral vesicular rashes and acute neuritis that occur in confined dermatomes. The rash of herpes zoster is characterized by erythematous papules, which quickly evolve into vesicles and crust within 7 to 10 days in immunocompetent hosts. Development of new lesions more than a week after the first presentation of disease is seen in immunodeficient patients.[1] The thoracic and lumbar dermatomes are the most common sites which are involved.[2] Pain is the major symptom of disease.[3] Approximately 75% of patients have pain in the dermatome before the appearance of the rashes.[1] Recurrence of zoster in immunocompromised patients is more common than in immunocompetent patients.[4,5] Postherpetic neuralgia is the most common complication of herpes zoster which occurs in about 10% to 15% of patients.[6] Neurologic complications are aseptic meningitis, myelitis, encephalitis, Guillain-Barré syndrome, stroke syndrome and Peripheral motor neuropathy. Approximately 3% of patients with zoster develop peripheral motor paresis which is a rare complication of disease,[7,8] but there are some papers reported zoster paresis in different aspects. Ruppert showed this paresis in a pediatric patient.[8] Tashiro et al. presented zoster paresis of trunk muscles,[9] while Yaszay introduced herpes zoster limb paresis with a review of literature about this topic until 2007.[10]
This case report is about an adult woman who has previously undergone chemotherapy and radiotherapy because of the lung metastasis from breast cancer. She presented with zoster paresis of left upper limb consequently.
CASE REPORT
A 59-year-old woman had noted moderate pruritus in the upper area of her left breast and sensed annoying mass in the same area, 15 months before she was referred to Al Zahra hospital where we took her history notes. One month after the initiation of pruritus, bilateral diagnostic mammography (4 films) showed a 1 cm spherical mass with spiculated edge in the upper zone of the left breast suspected to a malignant lesion and suggested fine-needle aspiration cytology for further studies according to breast imaging-reporting and data system (BIRAD V). Breast sonography revealed normal skin, nipple and subcutaneous fat but a 8.2 × 7.2 mm irregular contour, hypo echo lesion, 1 cm from nipple in the position of eleven o’ clock. Solid mass did not existed in the right breast. Due to these findings the patient underwent partial mastectomy and left axillary dissection 2 month after onset of mass sensation. Post operative pathobiopsy showed an invasive ductal carcinoma. Pruritus subsided immediately after surgery. Lung metastasis and post surgical collection were reported in multi 64-slice CT scan with contrast, 20 days after operation. Lungs were free from any pathologic infiltration. There were multiple pulmonary nodules (one 7 mm in the right upper lobe and three tiny foci in the left lung with mean size of 4 mm) in lung fields. No mediastinal or hilar lymphadenopathy, plural effusion and thickening were seen.
During 6 sessions of chemotherapy and 31 sessions of radiotherapy, the patient had no considerable symptom or problem until 1 week after last session of radiotherapy when she presented with severe scattering pain of the whole left upper limb with a radiation to scapula. Multiform blisters appeared 1 week after, when the scattering pain was decreasing. The watery/vesicular blisters were in the distal flexor surface of the arm in different sizes, dominantly in the cubital area lasted for 3 weeks. These clinical manifestations were diagnosed as herpes zoster activation and approved by positive direct fluorescent antibody test for herpes zoster. The patient was hospitalized and intravenous acyclovir was initiated 10 mg/8 hours for 7 days. Gradual improvement of blisters and severe pain was observed during treatment. A few days after completion of treatment, itching and motor involvement including elbow flexion and shoulder abduction appeared suddenly. The range of motion of glenohumeral joint decreased but the patient was able to adduct shoulder, flex and extend wrist and passively extend elbow. Magnetic resonance imaging showed compression of the left nerve root at C4-C5 and C5-C6 levels by protruded disk. No evidence of metastatic brachial plexus was noted [Figure 1]. Acromioclavicular and glenohumeral joint osteoarthritis were found in the left shoulder CT scan. No fracture or dislocation was reported.
Figure 1.
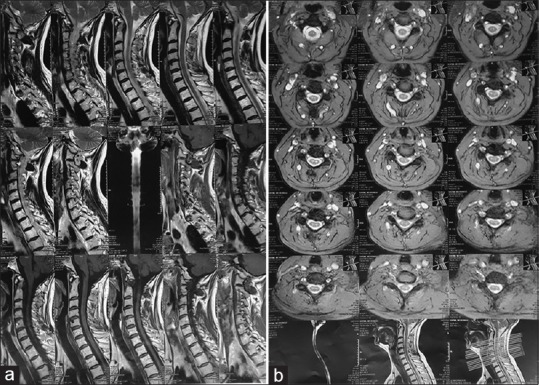
Cervical magnetic resonance imaging 2 month after onset of herpes blisters. (a) Sagittal plane. MRIs were obtained in multiple images with different pulse sequences. Left paracentral-central protruded disk at C4-C5 and C5-C6 levels with compression to epidural space-left nerve root and stenosis of spinal canal and left neuroforamina were found. Central protruded disk was noted at C6-C7 level. Cervical magnetic resonance imaging 2 month after onset of herpes blisters. (b) Axial plane. MRIs were obtained in multiple images with different pulse sequences. Left paracentral-central protruded disk at C4-C5 and C5-C6 levels with compression to epidural space-left nerve root and stenosis of spinal canal and left neuroforamina were found. Central protruded disk was noted at C6-C7 level
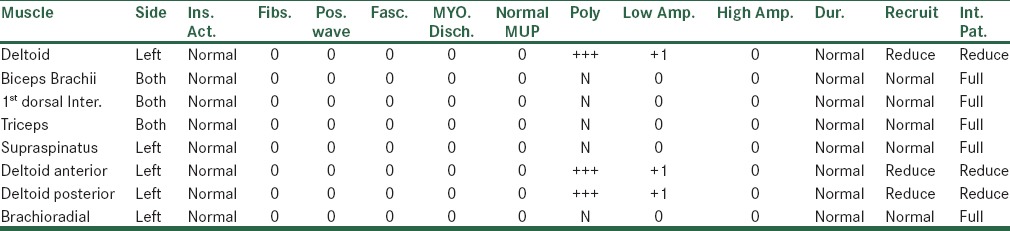
Sensory nerve conduction study and electromyography revealed low amplitude action potentials in left superior radial and median (from thumb and index) SNAPs (sensory neuron action potentials) and nascent MUAPs (motor unit action potentials) in left deltoid muscle [Tables 1 and 2]; also, a low amplitude action potential in left radial nerve was seen. Above findings were compatible with zoster-induced radiculoplexitis considering the MRI results, patient's history and clinic.
Table 1.
Sensory nerve conduction study
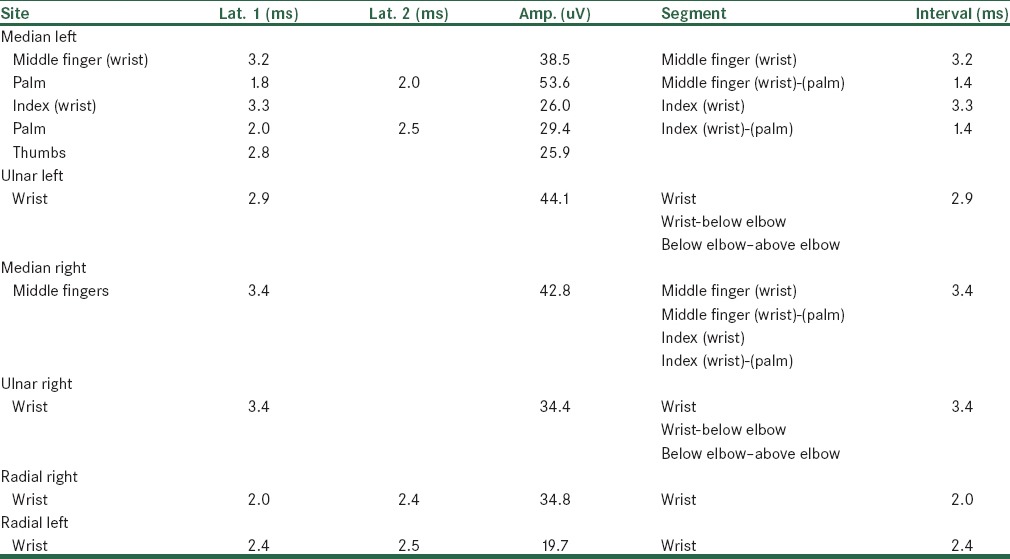
Table 2.
EMG findings summary
We examined the patient 5 months after beginning of pain and rash when 34 sessions of physiotherapy were performed to recover motor activities. The patient's neuropathy and neuroplexitis palliated gradually but pain and itching made poor decrement, suggesting post herpetic neuritis (PHN), as we find in immunocompromised cases.[11] She was able to flex elbow actively and abduct shoulder about 30 degrees while she could not do it before.
At the present time, rehabilitation is supposed to be continued, focusing on biceps brachii and deltoid muscle reinforcement and increasing left upper limb range of motion under supervision of orthopedic physician.
DISCUSSION
Recent studies in immunocompetent patients showed segmental paresis of limbs as a rare complication of herpes zoster virus, characterized by focal unilateral paresis in myotomes associated with involved dermatomes.[12] Viral invasion and inflammation of anterior horn cell motor neurons, in the same time as onset of rashes and vesicles, has been pointed out to be the pathogenesis of motor involvement in herpes zoster virus.[13]
Our case was a 59-year-old woman under treatment of metastatic invasive ductal carcinoma of breast, presented clinical manifestations of shingles, accompanied with acute upper limb paresis, suspected to be herpes zoster neuroplexitis. Confirmatory studies were performed to rule out other conditions and differential diagnoses in which motor neuron pathways were affected such as inflammation, discopathies, spinal neopelasms or even recurrence of previous breast cancer and metastasis. Post chemotherapy follow-up CT scan of thorax and abdomen showed no evidence of pulmonary nodules or metastasis. In addition, whole body Tc-99m-MDP bone scan in routine views was clear. The tumoral compression was ruled out. MRI of cervical and cervical brachial plexus with and without contrast showed protrusion of intervertebral C4-C5 and C5-C6 discs with nerve compression. No evidence of metastatic brachial plexus involvement was found.
The most common symptom in cervical radiculopathy is pain and sensory loss.[14] A herniated disc can cause motor involvement, although in most patients it is not severe. An acute and sudden motor weakness is more expected to result from migration of a fragment of disc into the spinal canal and nerve roots in acute disc herniation.[15] With conservative therapy, motor weakness is expected to improve more than few months.[16] Neurological examination of our patient detected no paresthesia or any sensory loss. According to these findings and clinical course of patient, we didn’t conclude that sudden motor paresis in upper extremity is due to disc protrusion, the primary stage of disc herniation.
In addition, brachial plexopathy after postoperative radiotherapy should be considered. This type of neuropathy results from formation of dense fibrous connective tissues around nerve fibers,[17] which needs time to proceed and present. In a same case report study as ours, Burns presented three breast cancer patients who underwent radiotherapy treatment and were followed up for developing radiation-induced neuropathy. Brachial plexopathy was detected 8, 15 and 15 years after radiotherapy in these patients.[18] In another long-term cohort study published in 2000, a group of 71 patients operated on for breast cancer with total mastectomy and axillary clearance were given aggressive postoperative telecobalt therapy to the axillary, supraclavicular and parasternal lymph node regions to evaluate the latency of brachial plexus neuropathy from the time of completion of radiotherapy to the first symptoms of plexus injury and to differentiate between the different types and degrees of neurological lesions. After a few years, symptoms and signs of brachial plexus injury appeared in many patients. Motor paresis was one of the scales used to quantify morbidities. High grades of motor impairment were not seen in patients after at least 2 years.[19] In our case, acute limitations in elbow flection (C6) and shoulder abduction (C5) were reported about 1 month after completion of radiotreatment, suggesting zoster-induced plexopathy.
This clinical diagnosis was compatible with available evidence. Cockerell showed that it may be 1 day to 4 months duration between cutaneous manifestations and motor weakness in herpes zoster. A complete recovery in 55-75% of these cases has been mentioned for in <1 year.[20] It is claimed that antiviral therapy for herpes zoster can prevent the occurrence of zoster paresis, although the effect of treatment on the recovery of paresis is uncertain.[21] Final point is that the possible relationship between surgery in the axilla and chemotherapy and brachial plexopathy have been considered in breast cancer patients in a previous study.[22]
CONCLUSION
It seems that reactivation of previous latent varicella zoster virus in dorsal root ganglia, when the natural immune system was impaired by chemotherapy and radiotherapy, resulted in left upper limb segmental paresis in our patient although she did not remember any history of chicken pox in her childhood. We reported this case to clarify common conditions that could present with motor paresis or weakness in old age with a special setting and to show that herpes zoster-induced motor paresis should be considered as an important cause of weakness in clinical decision making and treatment of zona. Nevertheless, we need further literature to investigate whether we can find segmental zoster paresis in congenital or severe immunodeficient patients or not. Also, the answer of this question that “How and when does the combination of chemotherapy and radiotherapy result in paresis in a breast cancer patient?” would be helpful.
Footnotes
Source of Support: This study was supported by Medical Students’ Research Center, Isfahan University of Medical sciences, Isfahan, Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44:S1–26. doi: 10.1086/510206. [DOI] [PubMed] [Google Scholar]
- 2.Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82:1341–9. doi: 10.4065/82.11.1341. [DOI] [PubMed] [Google Scholar]
- 3.Jumaan AO, Yu O, Jackson LA, Bohlke K, Galil K, Seward JF. Incidence of herpes zoster, before and after varicella-vaccination-associated decreases in the incidence of varicella, 1992-2002. J Infect Dis. 2005;191:2002–7. doi: 10.1086/430325. [DOI] [PubMed] [Google Scholar]
- 4.Taha Y, Scott FT, Parker SP, Syndercombe Court D, Quinlivan ML, Breuer J. Reactivation of 2 genetically distinct varicella-zoster viruses in the same individual. Clin Infect Dis. 2006;43:1301–3. doi: 10.1086/508539. [DOI] [PubMed] [Google Scholar]
- 5.Gebo KA, Kalyani R, Moore RD, Polydefkis MJ. The incidence of, risk factors for, and sequelae of herpes zoster among HIV patients in the highly active antiretroviral therapy era. J Acquir Immune Defic Syndr. 2005;40:169–74. doi: 10.1097/01.qai.0000178408.62675.b0. [DOI] [PubMed] [Google Scholar]
- 6.Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: A randomized controlled trial. JAMA. 1998;280:1837–42. doi: 10.1001/jama.280.21.1837. [DOI] [PubMed] [Google Scholar]
- 7.Elliott KJ. Other neurological complications of herpes zoster and their management. Ann Neurol. 1994;35:S57–61. doi: 10.1002/ana.410350717. [DOI] [PubMed] [Google Scholar]
- 8.Ruppert LM, Freeland ML, Stubblefield MD. Segmental zoster paresis of the left upper limb in a pediatric patient. Am J Phys Med Rehabil. 2010;89:1024–9. doi: 10.1097/PHM.0b013e3181e7204b. [DOI] [PubMed] [Google Scholar]
- 9.Tashiro S, Akaboshi K, Kobayashi Y, Mori T, Nagata M, Liu M. Herpes zoster-induced trunk muscle paresis presenting with abdominal wall pseudohernia, scoliosis, and gait disturbance and its rehabilitation: A case report. Arch Phys Med Rehabil. 2010;91:321–5. doi: 10.1016/j.apmr.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Yaszay B, Jablecki CK, Safran MR. Zoster paresis of the shoulder. Case report and review of the literature. Clin Orthop Relat Res. 2000;377:112–8. [PubMed] [Google Scholar]
- 11.Choo PW, Galil K, Donahue JG, Walker AM, Spiegelman D, Platt R. Risk factors for postherpetic neuralgia. Arch Intern Med. 1997;157:1217–24. [PubMed] [Google Scholar]
- 12.Gopal KV, Sarvani D, Krishnam Raju PV, Rao GR, Venkateswarlu K. Herpes zoster motor neuropathy: A clinical and electrophysiological study. Indian J Dermatol Venereol Leprol. 2010;76:569–71. doi: 10.4103/0378-6323.69054. [DOI] [PubMed] [Google Scholar]
- 13.Grant BD RC. Motor paralysis of the extremities in herpes zoster. J Bone Joint Surg. 1961;43:885–96. [Google Scholar]
- 14.Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: A review. HSS J. 2011;7:265–72. doi: 10.1007/s11420-011-9218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Postacchini F. Lumbar Disc Herniation. New York: Springer Wien; 1999. [Google Scholar]
- 16.Persson LC, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997;6:256–66. doi: 10.1007/BF01322448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gosk J, Rutowski R, Urban M, Wiecek R, Rabczynski J. Brachial plexus injuries after radiotherapy - analysis of 6 cases. Folia Neuropathol. 2007;45:31–5. [PubMed] [Google Scholar]
- 18.Burns RJ. Delayed radiation-induced damage to the brachial plexus. Clin Exp Neurol. 1978;15:221–7. [PubMed] [Google Scholar]
- 19.Johansson S, Svensson H, Larsson LG, Denekamp J. Brachial plexopathy after postoperative radiotherapy of breast cancer patients–a long-term follow-up. Acta Oncol. 2000;39:373–82. doi: 10.1080/028418600750013140. [DOI] [PubMed] [Google Scholar]
- 20.Cockerell OC, Ormerod IE. Focal weakness following herpes zoster. J Neurol Neurosurg Psychiatry. 1993;56:1001–3. doi: 10.1136/jnnp.56.9.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawajiri S, Tani M, Noda K, Fujishima K, Hattori N, Okuma Y. Segmental zoster paresis of limbs: Report of three cases and review of literature. Neurologist. 2007;13:313–7. doi: 10.1097/NRL.0b013e31811e9d6d. [DOI] [PubMed] [Google Scholar]
- 22.Galecki J, Hicer-Grzenkowicz J, Grudzien-Kowalska M, Michalska T, Zalucki W. Radiation-induced brachial plexopathy and hypofractionated regimens in adjuvant irradiation of patients with breast cancer-a review. Acta Oncol. 2006;45:280–4. doi: 10.1080/02841860500371907. [DOI] [PubMed] [Google Scholar]


