Abstract
Background:
There are many factors that affect the quality of life, for example, stress and the coping strategies. Polycystic ovary syndrome is a common hormonal disorder leading to menstrual disorders, hirsutism, acne, obesity, infertility and abortion. In such cases, the patients suffer from a variety of stresses and face problems in their coping strategies with life's problems which can affect the quality of life and cause psychological distress and low the quality of life. The quality of life is a descriptive term which points to health and emotional, social and physical promotion of individuals as well as their ability to perform daily living tasks. The purpose of this study was to investigate the relationship between quality of life and coping strategies in patients with polycystic ovary syndrome.
Materials and Methods:
To perform this study, randomly 200 women who had inclusion criteria and were referred to Ali Shariati Hospital in Isfahan were selected and responded DLQI questionnaire and Carver coping strategies and form of demographic characteristics.
Results:
The mean score of quality of life in the patients was 4.14 ± 5.57. It was shown that acne has no effective role on quality of life and coping strategies in contrast in hirsute and non-hirsute patients; there was a significant difference in quality of life P value < 0.001). Also there is a significant relationship between the quality of life and coping strategies (problem solving, cognitive, emotional and social support) (P < 0.05) and quality of life has the highest correlation with emotional strategies (r = 0.46).
Conclusion:
According to results of this study, patients with PCOS are at risk pcychologicla disorders that may be led to decrease of quality of life. Thus this patients need to support by oppositions strategies. Also not only physical treatment but also psychological surveillance especially social support must be done for them.
Keywords: Coping strategies, polycystic ovary syndrome, quality of life
INTRODUCTION
Polycystic ovary syndrome (PCOS) is a common endocrine disorder in women which affects approximately 5–10% of them in fertility ages. The name of this disease is caused by lesions in the ovaries in which both ovaries are filled and grow with multiple cysts. These cysts are formed in the outer layer of the ovaries and cause ovaries to appear as cystic.[1] Symptoms of PCOS vary from person to person but generally are infertility due to anovulation, cessation or irregular menstrual periods, hirsutism in face, chest, back and organs, acne, oily skin and dandruff, weight gain and obesity mostly in the waist area, hair loss and baldness, hair growth on the forehead where has been retreated in men, pieces of skin, neck, arms, chest and groin are discolored and darken, skin tags especially in the neck area, pelvic pain, anxiety and depression.[2] Studies have shown that quality of life in women with PCOS compared with healthy subjects and patients of other diseases has been much lower.[3,4] Health-related quality of life is a dynamic and multidimensional concept that includes physical, mental and social aspects associated with a particular disease or its treatment.[5] However, it seems that the presence of biochemical, endocrine and metabolic factors and physical problems is effective in lowering the quality of life of patients with this syndrome, but other issues such as the risks associated with health and appearance changes or psychological symptoms such as anxiety and depression can also cause significant decrease in the area of physical and mental quality of life of these patients.[6,7] Elesenbruch et al. in their study found that PCOS can cause a significant reduction in quality of life and sexual satisfaction.[8] Reduced quality of life in women disrupts the fields such as public health, limitations due to mental health, social functioning, decreased energy levels and mental health feelings.[9] These patients are facing changes in various aspects of their lives, and any kind of change in human life, either pleasant or unpleasant requires re-adjustment. Ways to cope with life changes and stresses resulting from these changes varied in different individuals according to different situations. Coping strategies are a set of individual cognitive and behavioral efforts that are used to change, adjust and interpret a stressful situation and reduce the suffering. Two main strategies to cope are namely emotion-focused coping strategies, including efforts to regulate the emotional consequences and keep emotional balance through the emotion resulting from stressful situations, and problem-focused coping strategies including the constructive measures of an individual in relation to stressful conditions in which the person is trying to remove the source of stress and change it.[10] Researches have shown that in these patients the use of maladaptive coping strategies has been increased due to the reduction in quality of life and vice versa.[11] Benson et al. in a research conducted in German investigated coping strategies in 448 patients with PCO and showed that in these patients in addition to the reduction of quality of life there is a relationship between the use of maladaptive coping strategies with anxiety and depression.[12]
The high prevalence and serious mental consequences of this illness and this fact that it affects the quality of life of patients regarding the less attention to the quality of life of patients and coping strategies in Iran, the present study aimed to investigate the relationship between quality of life and coping strategies and demographic characteristics of patients with PCOS.
MATERIALS AND METHODS
Participants and research design
The present study was a multiple correlation one. The population consisted of patients with PCOS in Isfahan province in 2013. In the present study for further assurance 200 patients with PCOS were selected as the study population. From all of the patients referred to Shariati Hospital in 2013 and the ones who received a PCO diagnosis and had inclusion criteria, 200 subjects were selected randomly.
Inclusion criteria included female gender, age greater than 16 years, and patient's agreement to participate in the study. In this study, patients with PCOS were examined based on their quality of life, coping strategies and demographic information such as age, marital status, duration and level of education. Dermatology Life Quality Index (DLQI) questionnaire was used to assess the quality of life in these patients. The questionnaires was designed in 1992 by Finalary and Khan to assess the quality of life in patients with skin diseases, it has been widely used in various communities and through various studies which its validity has been proved as 93%.[13] This questionnaire was designed for adults, and patients in a way that can be simply completed within 1–2 min without any additional explanation. It consisted of 10 multiple choice questions and each question had 4 points. Quality of life (QOL) score is obtained by adding the sum of scores. Therefore, the minimum and maximum scores in this questionnaire were 0 and 30. Questions were divided into six main sections, questions 1 and 2 (emotion and symptoms) with a maximum score of 6, questions 3 and 4 (daily activities) with a maximum score of 6, question 5.6 (touring) the maximum score of 6, question 7 (approved education) with a maximum score of 3, 8 and 9 questions about personal relationships with a maximum score of 6 and question 10 (treated) with a maximum score of 3. In this questionnaire, the higher score indicates the lower quality of life. Grading scale is as follows: (1) 0–1 points the impact on the patient's life, (2) 2–5 low impact on the patient's life, (3) 6–10 moderate impact on the patient's life, (4) 11–20 high impact on the patient's life, and (5) 21–30 much more impact on the patient's life.[13] Assessing the coping was done by the use of questionnaire presented by Carver et al., 1989. This questionnaire is a multidimensional instrument which checks the response of people to stress. This has been prepared based on Lazar Weiss model of stress and behavior self-regulation model by Carver, Scheire and Weintraub and has been translated and revised by Zolfaghari et al., according to Iranian culture and using other available coping scales in Iran. Check list contained 28 substances which were scored from 0 to 4. It had 14 subscales which had three scales measuring (active coping, planning, and prevention of nuisance activities) activities focused on problem-solving coping and three scales measuring (seeking instrumental social support, emotional support and focus on feelings and their tools) social support coping activities. The fourth scale measures the emotion-focused coping (denial, lack of emotional involvement, use of alcohol, tobacco and drugs, lack of behavioral engagement) and scale 4 indicates the cognitive coping strategy (reception, positive re-conclusion, taking refuge in religion and continence). The reliability and validity of this instrument have been studied in Iran and the results revealed that this scale is a valid instrument for measuring coping skills. Reliability coefficient obtained by implementing re-test on 10 subjects within 2-week interval has been reported 92%.[14]
In this study 200 PCOS patients who had referred to Shariati Hospital and had the inclusion criteria were selected randomly. After the explanation of study objectives to all participants’ verbal consent was taken, quality of life and coping strategies questionnaire and forms of demographic data including age, sex, educational level and employment were completed by patients and returned. Data were analyzed using Kolmogorov–Smirnov test, Kruskal Wallis, Mann–Whitney, Pearson Correlation Coefficient and regression analysis with a significance level of 0.05.
RESULTS
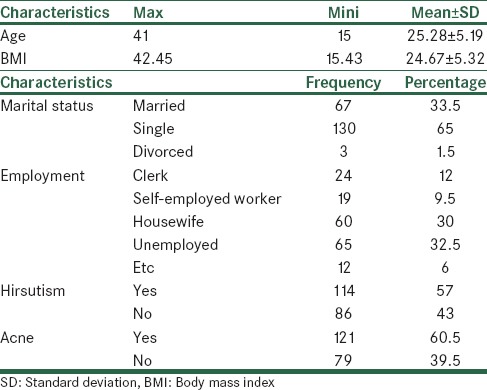
In this study, the mean age of the 200 women with polycystic ovaries was 25.28 ± 5.19 years and 130 of them (65%) were single and 67 (5.33%) were married, and the majority of women were unemployed or housewife. In this study 121 patients (60.5%) were acneic and 79 ones (39.5%) were not. Also, 114 patients (57%) had hirsutism and 86 (43%) did not [Table 1].
Table 1.
Descriptive statistics and frequency distribution of demographic and clinical characteristics of ovarian cystic syndrome in women
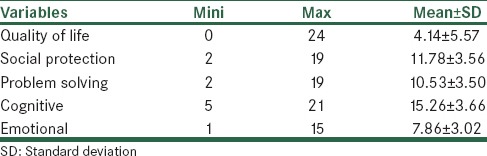
The quality of life mean in patients with PCOS was 4.14 ± 5.57 with the range of 0–24 and based on the obtained results, PCO did not affect the quality of life of 48% patients, had little effect on 28.5%, medium effect on 8.5%, high effect on 13% and very much effect on 2%. The mean range of coping strategies including social support, problem solving, emotional and cognitive coping strategies were social protection mean of women with polycystic 11.78 ± 3.56, problem solving mean 10.53 ± 3.50, mean of cognitive coping strategies 15.26 ± 3.66 and mean of emotional coping strategies 7.86 ± 3.02 [Table 2].
Table 2.
Mean of studied variables in women with polycystic ovary syndrome
The Kolmogorov–Smirnov test was used to examine the distribution of the variables (despite the large sample size), none of the variables followed a normal distribution (P < 0.05), and thus nonparametric test was used in this study.
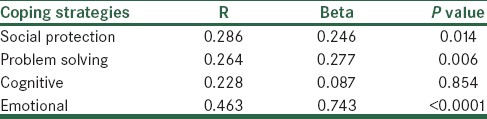
Since comorbid diseases like acne and hirsutism can affect the quality of life and coping strategies, Table 3 provides the comparison searching of patients, quality of life and coping strategies based on acne and hirsutism. According to this table, the average score of quality of life of patients who suffer from acne and who do not was respectively 4.26 ± 0.48 and 3.62 ± 0.61, which statically and according to Mann–Whitney test, was not significant in patients, quality of life score (P = 0.410). On the other hand, the quality of life scores of patients suffering from hirsutisim and who do not were respectively 5.45 ± 0.61 and 2.42 ± 0.37, which according to noted test, the difference between these two groups was significant (P < 0.001). In contrast, acne and hirsutism do not have any special influence on coping strategy and so there is no significant difference between the two groups (P > 0.05) [Table 3]. Examining the relationship between quality of life with each of the four dimensions of coping strategies and also the regression relation between these two factors showed a significant relationship between them (P < 0.05) in which affective strategies correlated much with quality of life (r = 0.46 and β =0.743, P < 0.0001) [Table 4].
Table 3.
Analyzing quality of life comparison based on comorbid diseases like acne and hirsutism
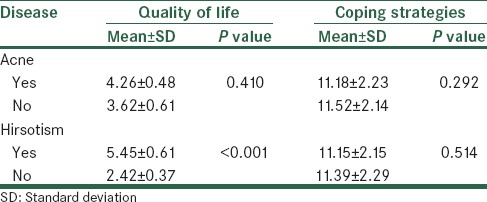
Table 4.
Multiple regressions of coping strategies and quality of life
And finally, analyzing demographic factors influencing quality of life rate and coping strategies and the use of Mann–Whitney and Kruskal–Wallis show that the factor of “age” affected the quality of life and coping strategies (P < 0.05). In another words, with increasing age in women, quality of life and coping strategies will be improved too. The factor of «marital status», although in married women, the amount of considered variables has been more than in single women, had affected just the aspect of cognitive strategy. In addition, the factor of «job» also affects the quality of life and social support (P < 0.05). In addition, the factor of BMI has no influence on none of current research variables (P > 0.05) but as it is seen, the average of quality of life and coping strategies in persons with low BMI is lower than other people; this difference is statistically unknown [Table 5, Figure 1].
Table 5.
Analyzing the role of demographic factors on quality of life and coping strategies
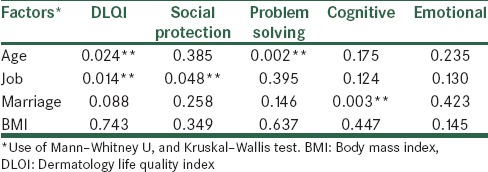
Figure 1.
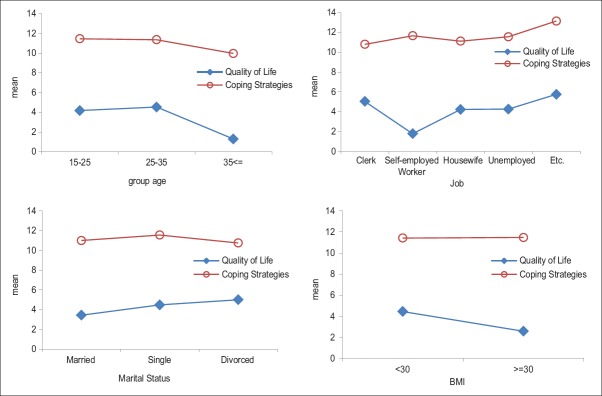
Bar graph of variables average of quality of life and coping strategies based on understudied factors
DISCUSSION
The main objective of this study was to examine the relationship between quality of life and coping strategies. The results showed that quality of life has a significant relationship with a variety of coping strategies (cognitive, problem solving, social support, and emotional) (P < 0.05). These results are consistent with the study results of Ching et al.,[3] Jenz et al.,[4] Alsenbrach et al.,[8] Pirlayne et al.,[11] and Benson et al.,[12] as well as the results of Bilihnger and Mouse, Folkman and Lazarus and Perlin and Sackler, Folkman and Lazarus[15] in which they believe that coping strategies act as a mediator between stress and physical or mental impairment, thus influencing the quality of life. They believed that stress plays a less important role in human welfare compared to the skills and strategies to deal with stress. In explaining these results it can be stated that quality of life was in interaction with coping strategies in which hand selection and the use of effective coping strategies on adjustment or change of stress have an important role in promotion of quality of life. On the other hand, having a good quality of life underlies a healthy psychological space that causes correct understanding and assessment of stressors and choosing effective coping strategies that are effective on physical, psychological health.
Problem-solving coping strategies include actively dealing with the problem, planning and avoiding pesky thoughts; cognitive coping strategies include acceptance, positive re-conclusion, taking refuge in religion and continence; social protection strategies include focus on emotions and their expression and seeking for social and emotional support; given the circumstances and created problem, the selection and utilization of each can have a significant role in promoting the quality of life. Thus, an individual can solve a problem by the use of efficient coping strategies of various cognitive and emotional skills. Accordingly, the ways to cope with problem are dealt directly and often appropriate solutions for psychological satisfaction are achieved. On the other hand, it causes mental discipline and intellectual coherence, thus reducing emotional distress and this helps identifying and assessing sources of stress. Identifying sources of stress on one hand and the evaluation of stress source on the other hand help increase mental health which is effective in improving the quality of life.[16] Folkman and Lazarus have argued that if stress or people are considered as controllable ones, the deal more focused than they used and otherwise deal in turn to focus on the excitement. This trend may explain why problem-focused coping strategies are mostly used in work-related stresses and social interactions and performance but emotion-focused coping are used more about stress and health-related emotional states.[15]
On the other side, the factor of “age” has had influence on the quality of life and problem-solving strategy. The factor of “marital status”, although in married women, the amount of considered variables has been more than in single women, had affected just the aspect of cognitive strategy. The factor of “job” also effects on the quality of life and social support. In a research done by Chan and Yu, factors, like gender, job, and the number of being hospitalized, play a role in quality of life, so that being female, unemployment and high number of being hospitalized relate certainly to the lower quality of living.[17] It is clear that the weaker mental status results in higher number of hospitalization, unemployment and finally problems in social life and coping strategies in society all of which can have effect on the quality of life. In addition, lacking opportunities, discriminations, unemployment and poverty play an important role, along with severe complications, in quality of life of patients. Therefore, comparing the current research to considered research, it can be said that job is an important factor in quality of life and coping strategy in the society, which exist along with each other in this respect.
The use of emotional coping strategies, for example, denial, lack of mental and behavioral-psychological involvement, tobacco use, alcohol and drugs, can be effective in reducing mental health and lower quality of life which is also true about PCOS patients, since denial or avoidance have been known as short-term strategies, but in the long term psychologically hinder psychological adaptation and increase symptoms of distress, such as increase in depression, and affect the quality of life of individuals.[18] Given the high prevalence and serious mental consequences of this illness the use of inefficient coping strategies severely affects the quality of life of these patients; in order to provide more comprehensive care to women with PCOS, doctors and health care providers should pay much attention to the psychological-social aspects of this illness, irrespective of the severity of its symptoms or response to treatment and be aware and understand it better.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Banaszewska B, Duleba AJ, Spaczynski RZ, Pawelczyk L. Lipid in polycystic ovary syndrome: Role of hyperinsulinumia and effects of metformin. Am J Obstet Gynecol. 2006;194:1266–72. doi: 10.1016/j.ajog.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 2.Glueck CJ, Morrison JA, Friedman LA, Goldenberg N, Stroop DM, Wang P. Obesity, free testosterone, and cardiovascular risk factors in adolescents with polycystic ovary syndrome and regularly cycling adolescents. Metabolism. 2006;55:508–14. doi: 10.1016/j.metabol.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Ching HL, Burke V, Stuckey BG. Quality of like and psychological morbidity in woman with polycystic ovary syndrome: Body mass index, age and the provision of patient information are significant modifiers. Clin Endocrinol (Oxf) 2007;66:373–9. doi: 10.1111/j.1365-2265.2007.02742.x. [DOI] [PubMed] [Google Scholar]
- 4.Jones GL, Palep-Singh M, Ledger WL, Balen AH, Jenkinson C, Campbell MJ, et al. Do South Asian woman with PCOS have poorer health-related quality of life than Caucasian woman with DCOS? A comparative cross-sectional study. Health Qual Life Outcomes. 2010:8–149. doi: 10.1186/1477-7525-8-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amini L, Sydfatmy N, Montazeri A, Mahmoodi Z, Arefi S, Hosseini F, et al. Quality of life in women with polycystic ovary syndrome. Quarterly Monitoring, 2011;6:862–57. [In Persian] [Google Scholar]
- 6.Upadhya K, Treat M. Effects of polycystic ovary syndrome on health-related quality of life. Expert Rev Pharmacoecon Outcomes Res. 2007;7:597–603. doi: 10.1586/14737167.7.6.597. [DOI] [PubMed] [Google Scholar]
- 7.Benson S, Hahn S, Tan S, Mann K, Janssen OE, Schedlowski M, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: Results of an internet-based survey in Germany. Hum Reprod. 2009;24:1466–51. doi: 10.1093/humrep/dep031. [DOI] [PubMed] [Google Scholar]
- 8.Elsenbruch S, Hahn S, Kowalsky D, Offner AH, Schedlowski M, Mann K, et al. Quality of life, psychosocial well-being, and sexual satisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88:5801–7. doi: 10.1210/jc.2003-030562. [DOI] [PubMed] [Google Scholar]
- 9.Drosdzol A, Skrzypulec V, Mazur B, Pawliñska-Chmara R. Quality of life and marital sexual satisfaction in women with polycystic ovary syadrome. Folia Histochem Cytobiol. 2007;45(Suppl 1):S93–7. [PubMed] [Google Scholar]
- 10.Carver CS, Pozo C, Harris SD, Noriega V, Scheier MF, Robinson DS, et al. How coping mediates the effect of optimism and distress: A study of women with early stage breast cancer. J Pers Soc Psychol. 1993;65:375–90. doi: 10.1037//0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- 11.Pearlin LI, Schooler C. The structure of copying. J Health Soc Behav. 1987;19:2–21. [PubMed] [Google Scholar]
- 12.Benson S, Hahn S, Tan S, Janssen OE, Schedlowski M, Elsenbruch S. Maladaptive coping with illness in women with polycyetic ovary syndrome. J Obstet Gynecol Neonatal Nurs. 2010;39:37–45. doi: 10.1111/j.1552-6909.2009.01086.x. [DOI] [PubMed] [Google Scholar]
- 13.Finlay AY, Khan GK. Dermatology life quality index (DLQI) - a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210–6. doi: 10.1111/j.1365-2230.1994.tb01167.x. [DOI] [PubMed] [Google Scholar]
- 14.Carver CS. You want to measure coping but your protocol's too long: Consider the Brief CODE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 15.Lazarus RS, Folkman S. New York: Springer publishing; 1984. Stress, appraisal and coping: Pp 445 illastrated. [Google Scholar]
- 16.Ghazanfari F, Ghadampour E. Investigate the relationship between coping and mental health of the residents of the city of Khorramabad. J Ment Health. 2009;37:47–54. [In Persian] [Google Scholar]
- 17.Chan S, Yu IuW. Quality of life of clients with schizophrenia. J Adv Nurs. 2004;45:72–83. doi: 10.1046/j.1365-2648.2003.02863.x. [DOI] [PubMed] [Google Scholar]
- 18.Mohammadi F, Sahebi A. Reviews styles and problem-solving in depressed patients compared with normal subjects. The Journal Psychological Science. 2002;1:42–24. [In Persian] [Google Scholar]


