Abstract
The concept of defining essential medicines and establishing a list of them was aimed to improve the availability of affordable medicines for the world's poor. Access to essential medicines is a major determinant of health outcomes. Several countries have made substantial progress towards increasing access to essential medicines, but access to essential medicines in developing countries like India is not adequate. In this review we have tried to present the Indian scenario in respect to availability and accessibility of essential medicines over last one decade. To enhance the credibility of Indian healthcare system, procurement and delivery systems of essential medicines have to be strengthened through government commitment, careful selection, adequate public sector financing, efficient distribution systems, control on taxes and duties, and inculcating a culture of rational use of medicines in current and future prescribers.
Keywords: Essential medicines, health expenditure, National Medicine Policy, primary healthcare, rational drug use
Background
Drugs and other pharmaceuticals constitute up to 40% of the healthcare budget in developing countries, yet a large proportion of the population frequently lack access to the most basic medicines. This can be attributed to poverty levels in the communities, and hence increasingly scarce resources for purchase of these facilities. On the other hand, industrialized countries with more resources are looking for ways to reduce medical expenditures and have embraced the concept of essential medicines. It is widely believed that this concept which advocates for selecting a limited number of drugs from the abundance of pharmaceuticals available in the world market leads to better supply, more rational use, and cost-effectiveness.(1)
Essential Medicine Concept
There are thousands of drugs in the market of which as many as 70% are duplicative or ‘me-too’ drugs and hence nonessential.(1) So it is important to derive a system to facilitate selection of fewer drugs from the numerous that are available.
World Health Organization (WHO) defines essential drugs or medicines as “those drugs that satisfy the healthcare needs of majority of the population; they should therefore be available at all times in adequate amounts and in appropriate dosage forms, at a price the community can afford”.(2) This is the basis of the Essential Medicine Concept that was launched in 1977, and became one of the eight pillars of WHO's “Primary Health Care” strategy. This concept is intended to be flexible and adaptable to many different situations and it is a national responsibility to determine the essential medicines.
This concept of selecting a limited number of essential drugs from the abundance of pharmaceuticals available on the world market leads to:
Improved supply and access of drugs
More rational prescribing and use of drugs, and
Lower drug costs.
Need of Essential Medicines
Forty million deaths have been reported in 1 year alone in developing countries, one-third among children under age 5, yet most leading causes of death and disability can be prevented or treated with cost-effective essential drugs. Ten million die due to acute respiratory infections, diarrheal diseases, tuberculosis, and malaria; for all these conditions safe, inexpensive, essential drugs can be lifesaving. The economic impact of pharmaceuticals is substantial especially in developing countries. While spending on pharmaceuticals represents less than one-fifth of the total public and private health spending in most developed countries, it represents up to 66% in developing countries. In most low income countries pharmaceuticals are the largest public expenditure on health after personnel costs and the largest household health expenditure. Despite this substantial spending on drugs, lack of access to essential drugs, irrational use of drugs, and poor drug quality remain serious global public health problems. Essential medicines are believed to be one of the most cost-effective elements in modern healthcare and their potential health impact is remarkable.(1)
Development
The essential medicines concept arose at a time of great changes in the field of international health cooperation. In May 1975, before representatives of WHO Member States at the World Health Assembly, Dr Halfdan Mahler insisted on the need to develop national pharmaceutical policies based on the affordability, quality, and availability of drugs.(3) The States responded to the report by the Director-General by adopting a resolution in support of national pharmaceutical policies that meet actual health needs and urged the Secretariat of WHO to help States to formulate them.(4,5) Rapidly, the concepts of “essential drugs” and of “National Drug Policy” entered the vocabulary of global public health. After the compilation, in 1976, of national practices based on lists of basic drugs, the first meeting of the Expert Committee on Selection of Essential Drugs was held and, in 1977, WHO adopted the first Model List of Essential Drugs.(6,7,8,9) Within WHO itself, the essential drugs concept was initially implemented by the Drugs Policies and Management Unit, which was setup in 1977 within the Division of Diagnostic, Prophylactic and Therapeutic Substances. In 1977, the World Health Assembly endorsed the “Health for All by the Year 2000” strategy whose purpose, via the new “primary health care” model, was the attainment of a level of health by all citizens of the world to permit them “to lead a socially and economically productive life” by the year 2000. The Health for All Strategy was under pinned by equity, the community dimension and a comprehensive approach to health. Essential medicines are not only crucial to the success of the strategy, and included among the eight basic elements of primary health care, they are also part and parcel of its very philosophy. The concept of essential medicines was quickly taken up by member states and developed their own national lists of essential medicines, often in combination with standard treatment guidelines (STGs) and stratified according to the level of care.(10,11) The “WHO Model List of Essential Medicines” has been updated ever since 1977. The current version, the 17th, was published in 2011. There is also a “WHO Model List of Essential Medicines for Children”, whose third edition was also published in 2011. At the 1978 Alma-Ata conference, provision of essential medicines was identified as one of eight key components of primary health care.(12)
The way in which national lists of essential medicines are being developed has slightly changed over time. The first list was developed as a guideline of procurement of drugs. In recent years, more emphasis has been placed on the development of treatment guidelines as the basis for drug selection and supply, and on the evidence underlying the development of those treatment guidelines. In addition, national lists of essential medicines may need to be stratified to reflect skills and requirements at different levels within the healthcare infrastructure.(13) The selection of essential medicines is a continuing process, which considers changing public health priorities and epidemiological conditions, as well as progress in pharmacological and pharmaceutical knowledge. It should be accompanied by a concomitant effort to supply information and provide education and training to health personnel in the rational use of the drugs.
Criteria of Selection of Essential Medicine
Essential medicines are selected based on disease prevalence, evidence on efficacy and safety, and comparative cost-effectiveness.
The following guidelines are used in the selection of drugs for a health facility:(13)
Environment (rural/urban, availability of electricity, facility of cold storage, specialized equipments, etc.) in which the healthcare is provided.
Pattern of prevalent diseases; a facility should not stock anti-leprotic drugs if the area has no case of leprosy.
Level of treatment facilities; a referral hospital should have more medicines than a district hospital, a health center more than a clinic, and so on.
Selection must be based on valid scientific evidence on efficacy and safety profile.
Where two or more medicines have similar properties, the choice should be made on the basis of a comparative evaluation of their relative efficacy, safety, quality, price, and local availability.
In cost comparison between medicines, consideration should be made of the cost of total treatment and not only the unit cost of the medicine. For example, cost of ampicillin capsule may be cheaper than that of amoxicillin, yet the total treatment cost for amoxicillin may be cheaper because it is given three times a day instead of four times a day required for ampicillin.
Most essential medicines should be formulated as single compounds. Fixed-ratio combination products are acceptable only when dosage of each ingredient meets the requirement of a defined population group and when the combination has a proven advantage over single compounds administered separately in therapeutic effect. Single compounds offer flexibility in dosing in various situations.
The number of drugs required is different for a referral hospital, district hospital, health center, and dispensary. The number of drugs should definitely depend on the level and size of the health facility. A referral hospital should have more drugs than a district hospital; a district hospital should have more than a health center; health centers more than a dispensary; and so on.(1)
Indian Scenario
In India first National Essential Medicine List (NEML) was prepared in 1996.(14) This list was neither implemented for procuring drugs nor STGs were drawn up.(15) The first and second revision was published in 2003 and 2011, respectively. NEML 2011 was revised based on the Indian Pharmacopeia 2010 and the National Formulary of India, 4th Edition, 2010.
One of the vital components of the healthcare is medicine, as they account for a substantial part of household expenditure. The overall budget of medicines varies widely in different states in India. The expenditure pattern on medicines of the State Government shows that there are wide-ranging differences across states, from as little as less than 2% in Punjab to as much as 17% in Kerala. The southern states such as Kerala and Tamil Nadu spend over 15% of their health budget on medicines. Many backward states, both in economic and health indicator terms, incurred the lowest expenditure on medicines. States such as Assam, Bihar, UP, and Orissa spent about 5% or less of their health budget on medicines. The Central Government's share of medicines in its total health budget is around 12%. In all, roughly 10% of the health budget goes into procuring medicines in India. Even then, availability of medicines often is a big issue. The non-availability of required medicines jeopardizes the credibility of the public health system. Access to essential medicines is closely linked to health system performance and its utilization. The non-availability of essential medicines in the health facilities is not the only issue; there are problems of affordability and accessibility despite spending a large proportion of resources on medicines. The Essential Medicines List can help countries rationalize the purchasing and distribution of medicines, thereby reducing costs to the health system.(16,17)
Implementation of Essentials Medicine Concept in India
Government initiatives
Government of India has introduced a policy aimed at increasing the availability of essential medicines at affordable prices. In 2011, the government proposed to increase the number of drugs remaining under the purview of the National Pharmaceuticals Pricing Policy 2011 to 348, up from initial 74. This policy has been amended in 2012 to include 652 commonly-used drugs under 27 therapeutic areas. Introduction of this policy is expected to result in a price drop of 10% or more for about two-thirds of essential drugs available in the Indian market.(18)
Industry initiatives
For a pharmaceutical company, establishing a balance between production cost, profitability and affordability of the drug for consumers is a delicate issue, with natural temptation to push the aspect of affordability to the back seat in search for profit maximization. Large pharmaceutical companies have often been criticized for not undertaking sufficient efforts to promote availability and affordability of essential medicines, especially in poor and developing countries. This criticism is slowly yielding positive results-several drug makers, such as GlaxoSmithKline and Johnson and Johnson, are intensifying their initiatives oriented at ensuring the availability and affordability of their drugs in less affluent markets. These efforts are mirrored in the “Access to Medicine Index”, published in 2012 by Access to Medicine Foundation, that clearly indicates drugmakers’ response to rising social pressure to provide affordable drugs. The drugmakers’ initiatives span a range of actions-differential and reduced pricing, technology transfers under license agreements, as well as donations.(18)
Negative repercussions
While these combined corporate and government efforts are likely to boost access to essential medicines, Indian government actions might, ironically, have an adverse impact on the industry. Several pharmaceutical companies operating in the Indian market are already against to these new government policies, citing erosion in both top and bottom line results.(18) There are at least two more negative repercussions potentially arriving from the government's actions:
In a scenario, where the provision of price-capped drugs becomes unprofitable for the drug makers, the pharmaceutical company may decide to discontinue the availability of these medicines in the Indian market. This took place prior to the introduction of the National Pharmaceuticals Pricing Policy 2011, when 27 of the 74 drugs under price control were discontinued. Such a scenario would render these price control efforts counter-productive.
At the same time, quite possibly, small domestic generic drug manufacturers are likely to be tempted to raise the prices of their low-cost drugs closer to the designated price-cap level, which in their case would mean an increase in the average price of drugs. This would, without a doubt, negatively impact consumers, particularly in smaller cities across the country.
Essential Medicines in Primary Health Care
Primary health care (PHC) is concerned with the important health problems in the community, promoting preventive and rehabilitative services to the people. Essential medicines are selected with regard to public health relevance and intended to satisfy the priority health care need of the community. The major hurdle to use of essential medicines in India is its low availability within health care facilities. Access to essential medicines is a major determinant of health outcomes. In developing countries, where the proportion of poor economic group is high, economic constraints related to the ability to afford medicines, constitute a major reason for lack of access to essential medicines. The availability of medicines is influenced by several factors like poor medicine supply, insufficient health facilities and staff, low investment in health, and affordability.(19)
Health expenditure in India
The rising prices of drugs is a considerable drain on the pockets of the entire population, but it affects the poor most. It is estimated that each year 20 million Indians fall below the poverty line because of indebtedness due to expenditure on healthcare.(20) The economic constraints related to the ability to afford medicines, constitute a major reason for lack of access to essential medicines. In India both total health expenditure (THE) as percentage of gross domestic product (GDP) and public spending as percentage of THE is low when compared to developed countries.(21) In India THE was 4.5% of GDP in 2004 and has decreased to 4.0% in 2012 [Figure 1]. External resources on health as percentage of THE has dropped to 1.2% in 2012from 2.3% in 2003 [Figure 2]. General Government Expenditure on Health (GGHE) has marginally increased from 22.8% of THE in 2003 to 33.1% in 2012, whereas private expenditure on health (PvtHE) has decreased from 77.2% of THE in 2003 to 66.9% in 2012.(22) In India the drug expenditure also varies state-wise. The THE per capita was as high as Rs. 2,950 in Kerala and as low as Rs.513 in Bihar.(21) Thus, any vision on universalization of access to essential medicines, in such a situation, would have to look at economic constraints that compromise access.
Figure 1.
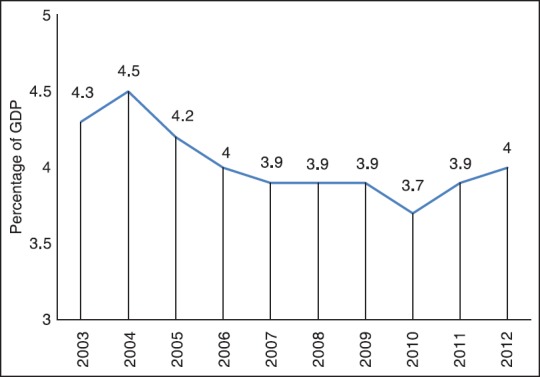
Total expenditure on health (THE) as percentage of GDP (2003-2012)
Figure 2.
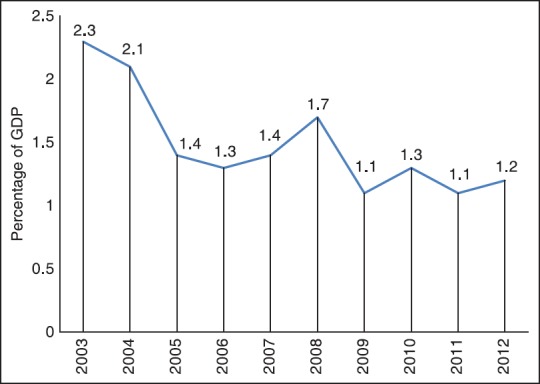
External resources on health as percentage of THE (2003-2012)
Availability and accessibility of essential medicines
The availability of medicines in India is still a big issue. It has been estimated by different sources that 50–80% of the Indian population are not able to access all the medicines they need.(23) Despite having lower prices of medicines in India as compared to the international prices, the availability and affordability is poor.(24)
A six-state survey carried out in 2004-2005, revealed that the median availability of a basket of 27 essential medicines in the public sector outlets was 0–30%.(25)
Similar conditions were also reported in a cross-sectional study carried out in three primary health centers (PHCs), three additional PHCs, and six subcenters in Darbhanga in Bihar.(26)
The results of a recent study done by Dixit et al., at Kunijarla, Khammam district, Andhra Pradesh shows that the people of Kunijarla have full access to essential medicines since the PHC-EML is on par with Andhra Pradesh-EML (AP-EML) and NEML and also the PHC has adequate supply of most of the essential medicines to the community, but they are in need of certain add-on supply of medicines for which suggestion was given for the revision of PHC-EML according to the criteria for identifying medicines for inclusion in the revised list.(27)
A survey was carried out by a bunch of nongovernmental organizations (NGOs) working in the field of healthcare supported by the National Rural Health Mission (NRHM) in 36 PHCs across 12 districts of Maharashtra. Basic medicines like paracetamol, common antibiotics, and essential drugs used post-delivery and lifesaving anti-rabies and anti-snake venom vaccines were found unavailable at a sizeable number of PHCs surveyed in the state. The survey was carried out to check availability of five essential medicines at primary healthcare centers and found that essential medicines were not available in 13% PHCs, while their stock was insufficient in 75% of the PHCs surveyed.(28)
Inadequacy of access to essential medicines is evidential of larger problems related to the way healthcare services are organized, financed, and delivered. Availability of medicines in public sector is lacking in most developing countries including India, and is consistently lower than in the private sector. When medicines are unavailable in the public sector, patients are forced to buy medicines from the higher-priced private sector, or abstain treatment altogether. Since public healthcare facilities usually provide medicines at low cost or free of cost, they are especially important for providing access to medicines for the underprivileged. In addition to the general deficiencies in health systems performance, four drug related factors are obligatory to ensure accessibility of medicines to people whenever and wherever they are needed. Rational selection processes should be in use to choose medicines, based on national or local essential drugs lists and treatment guidelines; prices should be affordable by governments, health care providers and consumers; impartial and continual financing for the medicines of health care should be ensured through adequate funding and unbiased prepayment mechanisms, such as government revenues or social health insurance; and finally, dependable health and supply systems need to be in place, integrating an productive and locally-appropriate blend of public and private service providers. Failure in any one of these processes will imperil people's access to medicines. So, the problems of lack of access to quality drugs that largely affect the developing countries are low-quality and spurious drugs; lack of availability of essential drugs due to varying production or exorbitant cost; and the need to conduct field-based drug research to determine optimum utilization and development for new drugs for the developing world.
India is one of the global leaders in manufacturing generic medicines. However, it is also held that large population is without having access to basic medicines. Most of the studies suggest that unless procurement and delivery systems of essential medicines are strengthened, mere presence of a NEML will largely be futile. Implementation of NEML in procurement of good quality medicines, regular supply as well as price regulation, strengthening indigenous manufacturing capacity should be emphasized. A regular and widespread accessibility of essential medicines needs to be ensured to enhance the credibility of health care system.
Healthcare referral systems
Provision of better healthcare in any healthcare system with different levels necessarily depends on a competent referral system. Generally, this is a pyramidal system with many primary healthcare centers at the base, some secondary centers in the middle, and a fewer number of tertiary care centers at the top. While the primary healthcare centers offer the minimum services on an outpatient care basis, the secondary level centers are able to offer most of the diagnostic tests and treatment facilities, including hospitalization, interventional procedures, and rehabilitation programs. The functioning of tertiary care centers is defined for complicated procedures, prescription of highly advanced and costly investigations, and domiciliary devices and life support systems. National- and state-level utilities should be set up to ensure a transparent system for bulk procurement and supply of adequate, rational, low cost, generic essential medicines down to the lowest referral levels which can be managed through an IT enabled system. Well organized referral systems, improved transportation, expert management of human resources, efficient supply chains and data, and upgraded facilities are essential to ensure availability and accessibility of essential medicines.
Central and State Government initiatives towards health services
National Rural Health Mission (NRHM)
Health system strengthening is a central mandate of the NRHM. Ministry of Health and Family Welfare has cleared Rs. 1,300 crore under the NRHM scheme for states to support their purchase of medicines in September 2012. The NRHM's state program under the Ministry of Health and Family Welfare equips the PHCs and public hospitals in the state with drugs. However, the adequate availability of medicines and other consumables is still not fully ensured in all states. At present, the public sector provides healthcare to 22% of the country's population and it is likely to swell to 52% by 2017 once medicines are provided for free from 1.6 lakh subcenters; 23,000 PHCs; 5,000 community health centers; and 640 district hospitals.(29) NRHM is addressing three critical areas - the access to essential drugs, the affordability of essential drugs, and the rational or appropriate use of drugs. These are three interrelated areas, each of which pose several challenges to the achievement of health for all.
Universal Health Coverage (UHC)
The recently launched National Urban Health Mission (NUHM) is a major step towards strengthening primary healthcare in urban areas and is expected to help the health needs of more than 10 crore urban people. To provide UHC, government has announced two schemes-National Urban Health Mission and Free Essential Medicines, which will cost the country approximately Rs.50,000 crore. Government of India has taken an initiative for free supply of essential medicines in public healthcare facilities in the country aiming to provide affordable health care to the people by reducing out of pocket expenses for medicines. This initiative has been undertaken to promote rational use of medicines and reduce the consumption of unscientific and hazardous medicines. The government estimates that the percentage of Indian population accessing public healthcare will be around 52% by 2017 from present value of 22%.
State Government initiatives
To provide universal access to essential medicines, Rajasthan government has launched Mukhyamantri Nishulk Dava Yojana. For its successful implementation, Rajasthan Medical Services Corporation (RMSC) was constituted in 2011 to procure generic medicines and surgical and diagnostic equipments for the department of Medical, Health and Family Welfare, Medical Education, Ayurveda, and Medical Relief Societies. RMSC has developed its drug procurement list following the framework of WHO-EDL which has been approved as the state EDL and has been modified according to the different level of healthcare system, that is, primary, secondary, and tertiary centers. Gujarat government has doubled its expenditure for the procurement of medicine under the Central Medical Stores Organization (CMSO) for establishing better healthcare facilities in the state. In Tamil Nadu, free medicines are procured in generic name by Tamil Nadu Medical Services Corporation (TNMSC), directly from the manufacturing company and are supplied to the public through an IT-enabled supply chain management system. Many state governments have started health insurance schemes named Arogyasri. The insurance claim ratio is said to be rising but ironically, the money is not going into improving health care, but used in purchasing it. In Andhra Pradesh, where Arogyasri covers a large population, a huge amount of money cannot be used to improve the public health system.
Role of Essential Medicines in framing National Medicine Policy (NMP)
A NMP is an obligation to goals and to monitor action. Irrespective of a nation's specific settings, a complete NMP considers all the components of the pharmaceutical segment and all relevant shareholders. WHO endorses all the countries to frame and implement a comprehensive NMP. A NMP provides a mutual framework to resolve problems in pharmaceuticals. A NMP, presented and printed as an official government proclamation, is imperative because it acts as a formal record of aims, goals, decisions, and promises. The main objectives of a national drug policy are to ensure access, quality, and rational use to medicines.(30)
The essence of essential medicines underlies in satisfying the health care needs of the population. The selection of essential medicines is one of the core principles of a NMP which helps to set primacies for all the aspects of the pharmaceutical system and helps in the maintenance of a proficient healthcare system globally. Devising of essential medicines and NMP is fast emerging as global concept of high relevance to the public irrespective of their nationalities. The prevalence of dreaded diseases like acquired immunodeficiency syndrome (AIDS), cancer, and a worldwide increase in case of malaria, tuberculosis, and other infectious diseases with an added problem of multidrug resistance has further augmented the relevance of essential medicines and formulation of a rigid comprehensive national drug policy under the endorsement of WHO medicine strategy and implementing the same under a complete implementation plan or master plan.(30)
Essential medicines to promote rational drug use
The selection of essential medicines is only the first step to improve the quality of health care. It should be followed by the appropriate use of the selected medicines. Each individual should receive the right medicine, in an adequate dose for an adequate duration, with appropriate information, planning of treatment follow-up, and at an affordable cost. In each country and setting, this is influenced by a number of factors, such as regulatory decisions, procurement, information, training, and the context where medicines are prescribed or recommended.(16)
Strategies to promote rational use of medicines(16)
A multidisciplinary national body to coordinate medicine use policies.
Clinical guidelines.
Essential medicines list for different therapeutic domains.
Drugs and therapeutics committees in hospitals.
Problem-based pharmacotherapy training in undergraduate curriculum.
Continuing medical education as a licensure requirement.
Supervision, audit, and feedback.
Independent information on medicines.
Public education and awareness about medicines.
Avoidance of perverse financial incentives.
Appropriate and enforced regulation.
Sufficient government expenditure to ensure availability of medicines and staff.
Role of Medical Council of India (MCI) to promote rational drug use
The MCI has issued circulars to the deans of all medical colleges, directors of Post Graduate Institutes, and presidents of state medical councils to give wide publicity to ensure compliance by doctors to the clause 1.5 of the Indian Medical Council (Professional Conduct, Etiquette, and Ethics) Regulations, 2002. The clause contains provisions that every physician should, as far as possible, prescribe drugs with generic names and he/she shall ensure that there is a rational prescription and use of drugs.(31) Additionally, MCI brought a new rule that doctors must attend 30 h of continuing medical education every 5years to maintain their licenses will help encourage such courses.(32)
The China Experience
To provide universal health care coverage, large-scale health care reforms were brought in by China government. One of the major reform components focuses on improving access to essential medicines to reduce high out-of-pocket medicines expenditure. The reform policies were comprehensive, and included systematic selection of essential medicines to improve availability, centralized procurement and tendering at provincial levels, price controlling policies, and stronger quality and safety standards. The national health care reform announced in 2009 was focused on strengthening public health services, service delivery, public hospitals, and supply of essential medicines. The Ministry of Health first published its EML in 1982. In 2004, the EML was revised to include 1,260 Chinese herbal preparations and 773 medicines products. To increase their availability, essential medicines were subjected to price controls. After health care reform was announced, the government revised the first part of the EML to make it suitable for primary care facilities. The current EML is composed of 307 medicines, including 102 traditional medicines.
The main areas of national health care reform in China were social security and insurance, service delivery, public health, and public hospital reform on pilot basis. These reforms showed a huge impact on access to and utilization of essential medicines. There is a considerable increase in the number of people covered under insurance programs, from 294 million in 2003 to 1.28 billion by 2011. Inpatient insurance reimbursement rates rose steadily, averaging 46.9% in 2011, including medicines and service fees. Reconstruction of the primary care system, including some 2,200 country hospitals and 33,000 urban and rural primary care facilities was done. Different categories of basic public health services have been implemented by introducing a per capita subsidy of 25 Yuan to primary care facilities and the subsidy is expected to increase to 40 Yuan by 2015. Hospital reform on a pilot basis was carried out at some municipalities and provincial cities to reduce the dependence on medicine sales as a major source of revenues.
The major impacts due to several activities under the reform of the essential medicines system are:
Essential medicines available at primary care facilities at cost.
Inpatients are reimbursed for essential medicines at higher rates than nonessential medicines.
Prices for essential medicines have been reduced primarily through greater efficiencies.
Through release of pricing data, greater price transparency is possible.
Prescribing and physician remuneration/facility operational costs have been delinked at many primary care facilities, thus reducing the incentives for over-prescription.
Consumers have greater protection through quality standards and more confidence in the quality of medicines.
Increased knowledge of rational medicines use.
Though some challenges still remain, China's health care reforms set an example of a comprehensive approach that other countries could follow in reforming their health care systems for achieving universal coverage. (33)
The Millennium Development Goals (MDGs)
The MDGs are eight international development goals that were established following the Millennium Summit of the United Nations in 2000, following the adoption of the United Nations Millennium Declaration. Target 8e of the MDGs acknowledges the need to improve the availability of affordable medicines for the world's poor. Recent progress in a number of countries shows that access to essential medicines can be improved through stronger partnership among governments; pharmaceutical companies; and civil society, including consumers, working together to ensure universal access to essential medicines. The role of pharmaceutical companies, ranging from multinationals to generic manufacturers to national distributors, is critical in this effort. The indicator used for measuring Target 8e is proportion of population with access to affordable, essential drugs on a sustainable basis. No doubt the MDG target to provide, in cooperation with pharmaceutical companies, access to affordable essential drugs in developing countries has served to mobilize resources and improve coordination aimed at increasing access to essential medicines and treatments to fight human immunodeficiency virus (HIV)/AIDS, malaria, and tuberculosis in many countries. Part of the difficulty in assessing progress towards this commitment has been the lack of a quantitative target. Recent efforts to develop reliable indicators to measure access (namely, those related to availability and price) will improve accountability in respect of global actions to expand sustainable access to essential medicines. In recent years, India has enjoyed consistently high rates of growth and steady improvement in human development. The imperative of faster, more inclusive, and sustainable growth is central to the Government of India's 12th Five-Year Plan (2012–2017) as well as to the United Nations Development Action Framework (UNDAF 2013–2017).
The Constraints and Recommendations
The major hurdle to use of essential medicines in India is its low availability within health care facilities. In India, where the proportion of poor economic group is high, economic constraints related to the ability to afford medicines, constitute a major reason for lack of access to essential medicines. The poor availability of medicines is influenced by several factors like poor medicine supply, insufficient health facilities and staff, low investment in health, and affordability.
The following recommendations can be considered for overcoming the constraints to implement Essential Medicine Concept in India:
The current list (2011) has been revised after 8 years. Like WHO EML, regular revisions are necessary at least once in 2 years.
Regarding health financing and financial protection, government should increase expenditures on public health.
General taxation can be used as the key source of health care financing; complemented by additional compulsory deductions for health care from salaried individuals and tax payers.
Availability of free essential medicines should be ensured by increasing public expenditure on drug procurement. User fees of all forms can be waived as a source of government revenue for health.
Elimination of taxes and duties on essential medicines.
Regular monitoring of medicine prices and availability.
Encouraging pharmaceutical companies to apply differential pricing practices to reduce prices of essential medicines in India where generic equivalents are not available.
Independent agencies in the private sector and insurance companies such as Rashtriya Swasthya Bima Yojana (RSBY) are supposed to achieve expected enrolment, utilization levels, and fraud control.
Key requirement to ensure availability and accessibility of essential medicines is the provision of adequate human resources. Sufficient numbers of trained and competent health care providers and technical health care workers at different referral levels should be recruited.
Adoption of generic substitution policies for essential medicines. Here it is essential to expedite the introduction of a scientifically powerful system of interchangeability of generic medicines, which would ease comprehensive policies to promote the use of generic medicines.
Ensuring adequate availability of essential medicines in public health care facilities.
Updating of national policy on medicines.
The evolution of objective and evidence-based STGs remains an important yet neglected part. Information required for developing evidence-based guidelines includes current utilization patterns for services and medicines.
Enhance the promotion of the production of generic medicines and remove barriers to uptake.
Increase funding for research and development in areas of medicines relevant to developing countries, including children's dosage forms and most neglected diseases.
Conclusion
The Essential Medicine Concept is needed now more than ever because of the rapidly changing global economic situation and the limited available resources. A limited range of carefully selected medicines can cater for most health care needs. The Essential Medicine Concept is globally applicable and offers the most cost-effective solution to healthcare needs. Government, universities, and professional associations have a critical role to play with regard to the improvement of undergraduate, postgraduate, and continuing medical education in clinical pharmacology, therapeutics, and medicines information issues. Although many people in the world still lack effective access to essential medicines, the work done by WHO and its partners has done much to bridge this gap. The original insight that a restricted list of well-chosen medicines could meet the needs of most of the world remains as valid now as it did in 1977. However, the fundamental human right to access to these medicines remains a challenge and will require further action at the national and international levels.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Masiga J. Essential drugs concept: Is it still relevant in our situation today? Meds Update. 2010;17:2–8. [Google Scholar]
- 2.Report of a WHO Expert Committee. Geneva: World Health Organization; 2002. The Selection and Use of Essential Medicines. (WHO Technical Report Series, No. 914). [PubMed] [Google Scholar]
- 3.WHO, WHO Offficial Records, Prophylactic and therapeutic substances. In: Twenty-eighth World Health Assembly, Geneva, 13–30 May 1975. Part 1. Resolutions and decisions, annexes. Geneva, World Health Organization, 1975 (Official Records of the World Health Organization, No, 226), Annex. 13:96–110. [Google Scholar]
- 4.WHA 28.66 - Prophylactic and Therapeutic Substances. WHA Resolution; Twenty-eighth World Health Assembly, 1975. [Last accessed on 2013 May 12]. Available at: http://apps.who.int/medicinedocs/en/d/Js21447en .
- 5.WHA54.11 - WHO Medicines Strategy. WHA Resolution; Fiftyfourth World Health Assembly, 2001. [Last accessed on 2013 May 12]. Available at: http://apps.who.int/medicinedocs/en/m/abstract/Js16336e .
- 6.Laing R, Waning B, Gray A, Ford N, ’t Hoen E. 25 years of the WHO essential medicines lists: Progress and challenges. Lancet. 2003;361:1723–9. doi: 10.1016/S0140-6736(03)13375-2. [DOI] [PubMed] [Google Scholar]
- 7.Helling-Borda M. Memories of the First Expert Committee Meeting and Celebrating 25 years later. Essent Drugs Monit. 2003;32:14–5. [Google Scholar]
- 8.The selection of essential drugs. Report of a WHO expert committee. Geneva: World Health Organization; 1977. (WHO Technical Report Series, No. 615). [PubMed] [Google Scholar]
- 9.WHO, The Selection of essential drugs. Report of a WHO Expert Committee, op. cit. :20–30. [Google Scholar]
- 10.WHO. The use of essential drugs: Report of a WHO expert committee. Geneva: World Health Organization; 2000. (Technical report series no 895). [Google Scholar]
- 11.WHO. The rational use of drugs: Report. Geneva: World Health Organization; 1987. [Google Scholar]
- 12.WHO/UNICEF. Primary health care: Report of the International Conference on Primary Health Care, Alma-Alta, USSR, Sept 6–12, 1978. Geneva: World Health Organization; 1978. (Health for all, series 1). [Google Scholar]
- 13.WHO. Essential Medicines. [Last accessed on 2013 May 02]. Available from: www.who.int/medicines/services/essmedicines_def/en/index.html .
- 14.Sharma S, Kh R, Chaudhury RR. Attitude and opinion towards essential medicine formulary. Indian J Pharmacol. 2010;42:150–2. doi: 10.4103/0253-7613.66837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Better medicines for children in India. WHO. [Last accessed on 2013 May 05]. Available from: http://apps.who.int/medicinedocs/documents/s17812en/s17812en.pdf .
- 16.Kar SS, Pradhan HS, Mohanta GP. Concept of essential medicines and rational use in public health. Indian J Community Med. 2010;35:10–3. doi: 10.4103/0970-0218.62546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sakthivel S. Access to Essential Drugs and Medicines. In: Lal PE, Byword, editors. NCMH: Background papers on Financing and delivery of Health Care Services in India. New Delhi: Cirrus Graphics Private Limited; 2005. pp. 185–212. [Google Scholar]
- 18.Essential Drugs in India: Is it all About Affordability? [Last accessed on 2013 May 05]. Available from: http://www.eos-intelligence.com/perspectives/?p=36 .
- 19.Geneva, World Health Organization, 1999 (unpublished document WHO/EDM/PAR/99.4; available on request from Essential Drugs and Medicines Policy. Geneva: World Health Organization; Guidelines for drug donations. [Google Scholar]
- 20.Promoting Rational Drug Use under NRHM. [Last accessed on 2013 May 05]. Available from: http://nhsrcindia.org/pdf_files/resources_thematic/Medicine_and_Technology/NHSRC_Contribution/Others/Promoting_Rational_Drug_use_under_NRHM_NHSRC_WHO.pdf .
- 21.National health accounts India 2004–2005. WHO. [Last accessed on 2013 May 07]. Available from: http://www.who.int/nha/country/ind/en/
- 22.Global Health Expenditure Database. Geneva: WHO; [Last accessed on 2013 May 07]. India-national expenditure on health. Table of key indicators and sources by country. Available from: http://apps.who.int/nha/database/StandardReport.aspx?ID=REP_WEB_MINI_TEMPLATE_WEB_VERSION&COUNTRYKEY=84678 . [Google Scholar]
- 23.Economic constraint to access to essential medicines in India. WHO. [Last accessed on 2013 May 07]. Available from: www.healthpolicy.cn/rdfx/jbywzd/gjjy2/yd/yjwx/201002/P020100227571385215688.pdf .
- 24.Thawani V. Rational use of medicines: Achievements and challenges. Indian J Pharmacol. 2010;42:63–4. doi: 10.4103/0253-7613.64486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotwani A. Commentary: Will generic drug stores improve access to essential medicines for the poor in India? J Public Health Policy. 2010;31:178–84. doi: 10.1057/jphp.2010.2. [DOI] [PubMed] [Google Scholar]
- 26.Roy C, Das JK, Jha HK, Bhattacharya V, Shivdasani JP, Nandan D. Logistics and supply management system of drugs at different levels in Darbhanga District of Bihar. Indian J Public Health. 2009;53:147–50. [PubMed] [Google Scholar]
- 27.Dixit R, Vinay M, Jayasree T, Ubedulla S, Manohar VS, Chandrasekhar N. Availability of essential medicines: A primary health care perspective. Indian J Pharmacol. 2011;43:599–600. doi: 10.4103/0253-7613.84981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Isalkar U. Basic medicines unavailable in several state PHCs. [Last accessed on 2013 May 09]. Available from: http://articles.timesofindia.indiatimes.com/2013-02-20/pune/37199579_1_phcs-essential-medicinesrural-health-mission .
- 29.Sinha K. Free medicine scheme gets Rs 1,300 crore boost under NRHM. [Last accessed on 2013 May 09]. Available from: http://articles.economictimes.indiatimes.com/2012-09-20/news/33977207_1_freemedicines-generic-drugs-health-centres .
- 30.Chauhan A. Role of Essential Medicines in framing National Medicine Policy - An Approach from Concept to Clinic. [Last accessed on 2013 May 09]. Available from: www.pharmatutor.org/articles/role-of-essential-medicines-in-making-national-medicine-policies .
- 31.Code of Ethics Regulations, 2002. [Last accessed on 2013 Oct 26]. Available from: www.mciindia.org/RulesandRegulations/CodeofMedicalEthicsRegulations2002.aspx .
- 32.Sinha K. MCI plans to send docs back to lecture halls. Times of India. 2011 Apr 5. [Last accessed on 2013 April 26]. Available from: www.educationtimes.com/index.aspx?page=article&secid=1&conid=201104052011040517292973386030ada .
- 33.Barber SL, Huang B, Santoso B, Laing R, Paris V, Wu C. The reform of the essential medicines system in China: A comprehensive approach to universal coverage. J Global Health. 2013;3:010303. doi: 10.7189/jogh.03.010303. [DOI] [PMC free article] [PubMed] [Google Scholar]


