Abstract
Background:
Studies show that immunization among migrant children is poor. India has a dropout rate of 17.7% between Bacillus Calmette-Guιrin (BCG) and measles (District Level Household Survey (DLHS)-3). Haridwar district had the highest dropout rate of 27.4% from BCG to diphtheria, pertussis, and tetanus (DPT) 3 (DLHS-3) in Uttarakhand. We evaluated the Universal Immunization Programme (UIP) among migrants in Haridwar in two blocks.
Materials and Methods:
We developed input, process, and output indicators on infrastructure, human resources, and service delivery. A facility, session site and cross-sectional survey of 180 children were done and proportions for various indicators were estimated. We determined factors associated with not taking vaccination using multivariate analysis.
Results:
We surveyed 11 cold chain centers, 25 subcenters, 14 sessions, and interviewed 180 mothers. Dropouts were supposed to be tracked using vaccination card counterfoils and tracking registers. The dropout rate from BCG to DPT3 was 30%. Lack of knowledge (adjusted odds ratio (AOR) 6.6,95% confidence interval (CI) 2.6–16.7), mother not being decision maker (AOR 4.0,95%CI 1.7–9.2), lack of contact by Accredited Social Health Activist (ASHA; AOR 3.0,95%CI 1.1–7.7), not being given four post-vaccination messages (AOR 7.7, 95% CI 2.9–20.2), and longer duration of stay in Haridwar (AOR 3.0 95% 1.9–7.6) were risk factors for nonimmunization. The reasons stated by mothers included lack of awareness of session site location (67%) and belief that child should only be vaccinated in their resident district (43%).
Conclusions:
There was low immunization coverage among migrants within adequate supervision, poor cold chain maintenance, and improper tracking of dropouts. Mobile immunization teams, prelisting of migrant children, and change in incentives of ASHAs for child tracking were needed. A monitoring plan for sessions and cold chain needed enforcement.
Keywords: Dropouts and left outs, Haridwar, immunization coverage, migrants, tracking
Introduction
Globally, 19.3 million infants did not receive diphtheria, pertussis, and tetanus (DPT)3 vaccine in 2010.(1,2) Nearly 70% of these children live in 10 developing countries of Africa and Asia including India.(3) India achieved 61% immunization coverage in 2011.(4) However, the dropout rate from Bacillus Calmette-Guérin (BCG) to measles and BCG and DPT3 is 14.7 and 17.7%, respectively, in India (Coverage Evaluation Survey (CES) 2009 Unicef report).(5) The dropout rates are higher among migrants who have poor service utilization.(6,7) Floating population, overcrowding poor sanitation, and personal hygiene lead to higher transmission of vaccine preventable diseases (VPD).(8) Studies on determinants of immunization have shown that nearly one in three migrant children are unable to complete their course of vaccination.(1) Government of India declared 2012 as “the year of intensification of routine immunization” a campaign-like strategy to reach all children including migrants in remote inaccessible backward areas and urban slums.(9)
Uttarakhand in North India, had a high dropout from BCG to DPT3 at 23% as per the District Level Household Survey (DLHS)-3 report.(4) This hilly state with a population of 10.1 million has a high migrant population from neighboring states in its three Terai region districts.(10) Haridwar district had the highest dropout rate in routine immunization in the state with only 52.4% of the children aged 12–23 months fully immunized. As per the DLHS-3 report, the dropout rate from BCG to measles and from BCG to DPT3 was 12.8 and 27.4%, respectively.(11) The routine immunization monitoring report highlighted that the dropout and left out rate was 70% in migrant sites.(12)
We evaluated the Universal Immunization Programme (UIP) in Haridwar to review the infrastructure, human resources, and service delivery as per the guidelines among migrant population in two blocks.(13,14) We also estimated the immunization coverage among migrant children (in the 12–23 months age group) and identified reasons for dropouts and left outs.
Materials and Methods
Study site and study population
We evaluated the program in two blocks, Bahadarabad and Narsan of Haridwar district in 2012. The target population included 800 children in 146 sites (mainly brick kilns and industrial construction sites) of Narsan block of Haridwar.(13) The block of Bahadarabad included both-the urban slums of Haridwar city and dry river quarries in the tributaries of the Ganga. There were 1,170 children in 101 migrant sites of this block.(13) We surveyed select facilities including three community health centers (CHCs), eight primary health centers (PHCs), and 25 subcenters catering to these migrant populations.
Evaluation indicators
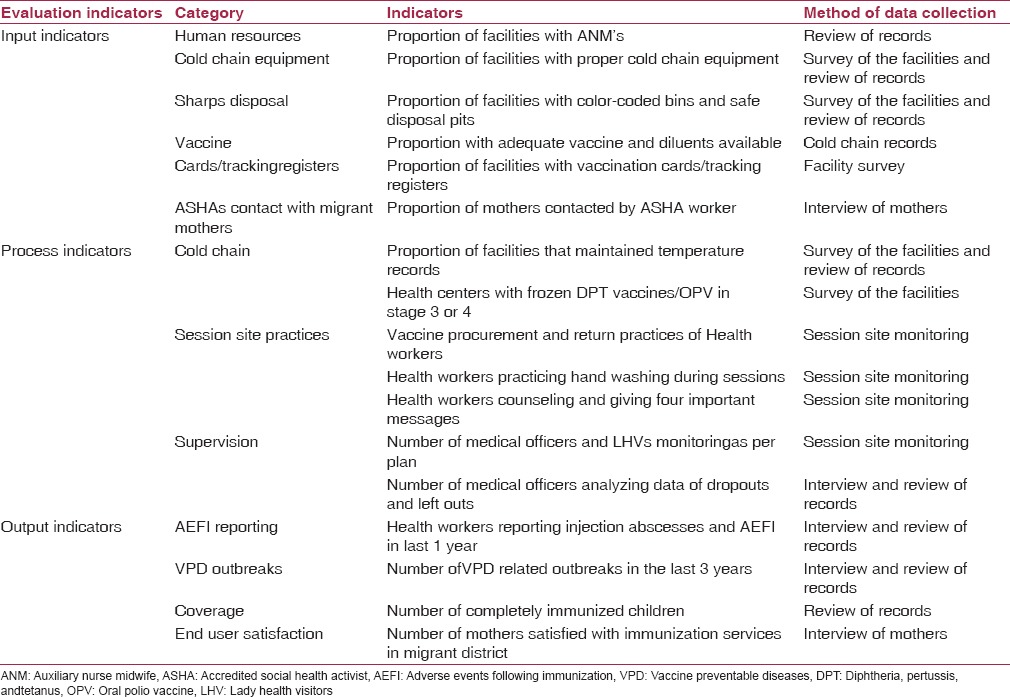
We developed input, process, and output indicators. The input indicators included availability of human resources, cold chain equipment, sharps disposal, vaccine stock, and child tracking documentation. The key process indicators were temperature maintenance recording, session site practices, and supervision. Reporting of adverse events following immunization (AEFI), VPD outbreaks, immunization coverage of migrant children, and end user satisfaction were the output indicators [Table 1].
Table 1.
Key input, process, and output indicators for evaluation of Universal Immunization Progrmme (UIP) in two blocks, Haridwar, Uttarakhand, India, 2012
Evaluation design and data collection
We used multiple methods to evaluate the program. The methods and the data collected using each of the methods was as follows:
Review of records
The guidelines for UIP by the Ministry of Health and Family Welfare, Government of India, New Delhi were reviewed. Various stakeholders including the District Immunization Officer (DIO), medical officers, and auxiliary nurse midwives (ANMs) were interviewed. The available records of last 3 years for routine immunization and routine immunization data management software (RIMS) data were reviewed at the district, CHCs, PHCs, and subcenters of Narsan and Bahadarabad blocks regarding coverage and vaccine utilization.
Facility survey
We surveyed 11 cold chain centers (three CHCs and eight PHCs) and 25 subcenters (six urban slum maternal and child health (MCH) centers and 19 rural subcenters). A standard checklist was used to collect data regarding cold chain equipment, consumables, infrastructure, number of beneficiaries, logistics for immunization, and maintenance of cold chain.
Session-site survey
We did a cross-sectional survey of 14immunization sessions and interviewed ANMs using a semistructured questionnaire to assess the status of immunization records, status of cold chain at field level, information education and communication (IEC), injection safety measures, VPD, and AEFI reporting, and existing monitoring and supervision activities. The practices of health workers during vaccination, child tracking methods adopted, efforts made for reimmunization of dropouts by Accredited Social Health Activists (ASHAs) were observed using checklist during the sessions.
Community survey
We did a cross-sectional survey of 180 migrant children (12–23-months-old). The mothers of these 12–23-months-old children were interviewed using pretested semistructured questionnaires. We collected data about their sociodemographic characteristics, knowledge, attitude, perceptions regarding immunization, and the immunization status of the child by recall as well as vaccination card if available.
Operational definitions
Fully vaccinated child
Any child who had received one dose of BCG, three doses of DPT, three doses of OPV, and one dose of measles by 1 year of age was considered fully vaccinated.
Dropouts or partially vaccinated child
Any child who received at least one dose of vaccination by 1 year of life, but did not complete all doses.
Leftouts or unvaccinated child
If child had never received any of the vaccines by 1st year of life.
Overall dropout rate
The percentage difference between the vaccines of maximum and minimum antigen received expressed as a percentage of the maximum antigen.
Migrant site/colony
The sites included brick kilns, slums, construction sites, or temporary settlements having more than 10 households with families coming from other states and residing within Haridwar for more than 1 month prior to the date of interview.
Resident district
The district of residence where migrants resided prior to migrating to current location.
Sampling strategy and sample size
Facility and session site survey
All 11 cold chain centers in the two blocks were surveyed and the medical officer in charge of immunization was interviewed. Twenty-five subcenters catering to the migrant clusters were surveyed. We interviewed all 25 ANMs of these subcenters and monitored 14 immunization sessions held during a 3-monthstudy period.
Community survey
We used the cluster sampling technique for the community survey and selected the clusters using the Population Proportion to Size (PPS) method. One migrant site was considered as cluster. We calculated the sample size of 180 children (12–23-months-old) with an estimated proportion of 44% migrant children being completely immunized,(1) 95% CI, ± 8% precision, and design effect of 1.9. We interviewed 10 children from each of the 18 selected migrant clusters.
Data analysis
Data was analyzed using Epi-info software. We calculated the proportions for various indicators. We computed proportion with 95% confidence intervals (CIs) for antigen wise coverage. We also determined factors associated with partial/nonimmunization using univariate and multivariate analysis.
Human subject protection
The Institutional Ethics Committee of National Institute of Epidemiology, Chennai approved the study. We obtained written consent from the respondents after providing the information regarding the study.
Results
Input indicators
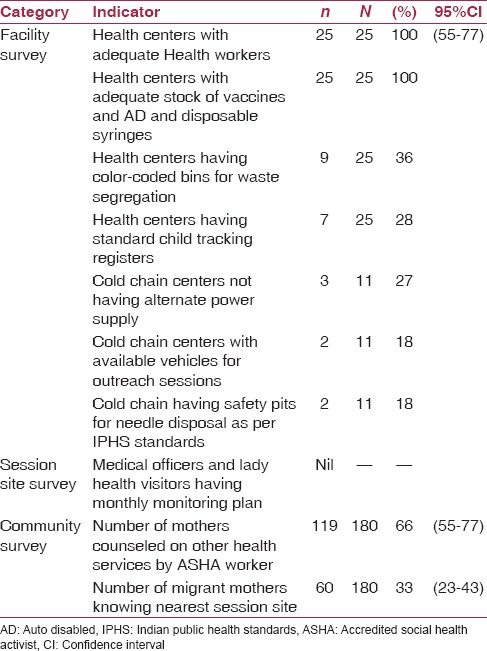
In the health facilities, 94% of the sanctioned medical officers, 90% of lady health visitors (LHVs), and 100% of ANMs were in position. All cold chains had functional ice-lined refrigerators (ILRs) and deep freezers, but there were no separate stabilizers for each equipment. Three of the 11 cold chain centers had no alternate electricity supply (diesel run generators) and only two had vehicles for vaccine supply. All the cold chain points were supplied with adequate number of auto disabled (AD) syringes of 0.1and 0.5ml, and had 1 month vaccine stock. There was no shortage of vaccines except vitamin A in the past 1 year. Only 36% (9/25) of the subcenters were equipped with color-coded bins. Both the CHCs had disposal pits, but none of the PHCs had pits for disposal of sharps. Among mothers 66% had been contacted by ASHA for general health problems and 33% knew the nearest session site [Table 2].
Table 2.
Key input indicators for universal immunization programme in Narsan and Bahadarabad blocks, Haridwar, Uttarakhand, India, 2012
Process indicators
Cold chain maintenance
Twice a day temperature monitoring was being done in 4/11 cold chain centers. Two frozen DPT vials and 10 vials of polio vaccine were in stage 3 and 4 of (vaccine vial monitor (VVM)) in two PHCs of one block. Six of the 25 (24%) ANMs were taking vaccine 1 day prior to the vaccination day and storing vaccine and ice packs overnight in their domestic refrigerators. Five (40%) ANMs procured the vaccine early in the morning on vaccination day without simultaneous entries in the stock register due to nonavailability of cold chain staff and unused vials were being returned after 1–2 days of the session [Table 3].
Table 3.
Key process and output indictors for Universal Immunization Programme in Narsan and Bahadarabad blocks, Haridwar, Uttarakhand, India 2012
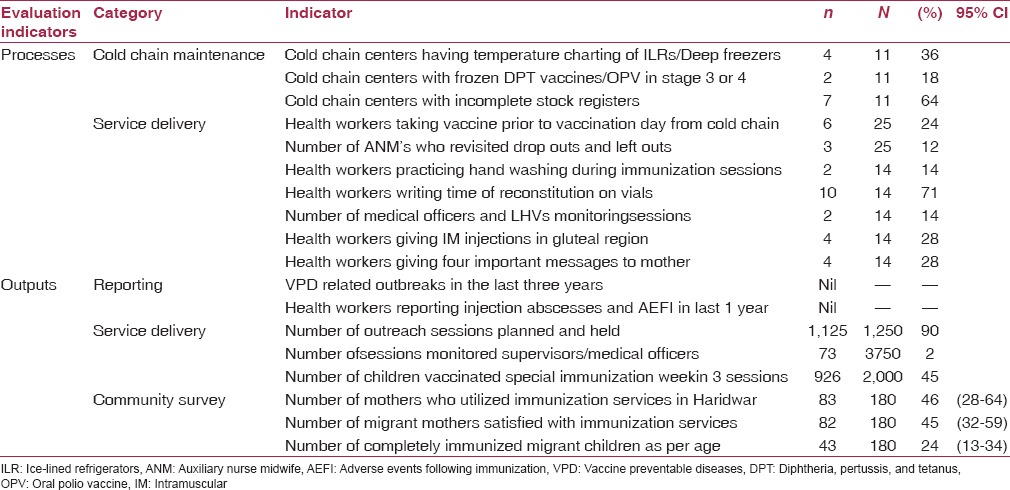
Service delivery
All the three CHCs, eight PHCs, and 25 subcenters conducted weekly “fixed day” immunization and biweekly outreach sessions as per the microplan. Special immunization week was being organized every alternate month in 2012 to monitor and follow-up newborns and children among migrants in the district. All the health workers demonstrated correct knowledge of the revised vaccination schedule and sites of vaccination administration.
The key observations during the session site monitoring (14 sessions) included lack of hand washing (86%), practice of giving intramuscular (IM) injection in gluteal region (28%), and poor counseling of mothers with key four messages (28%). The four messages were information about vaccine given, possible post vaccination complications, next date for vaccination, and instructions to keep the immunization card properly and to bring it in the next visit. All ANMs informed the mother about not massaging the site of injection and to apply vicks or ice in case of local swelling in the area. The mothers of children who had been given DPT were advised to give the child one-fourth of paracetamol tablet for fever. However, there was no supply of the paracetamol syrup or tablets in the subcenters.
Tracking the dropouts
The program had three mechanisms to track the dropouts, namely tracking by ANM/ASHA based on the information in card counterfoil/MCH registers, defaulter tracking bags, and SMS reminders. ANMs issued immunization cards to mothers and retained one counterfoil with them. According to program guidelines, ANM's and ASHA'srole was to track the dropout and leftout children to complete their immunization.(14,15) However, feedback meetings with ASHAs were being held only in two (18%) cold chain centers on a quarterly basis. There was lack of monitoring of revisits by ASHAs for the dropouts. Only three (16%) subcenters had the standard printed MCH registers. The rest were using an ordinary register and data regarding left outs and dropouts was incomplete. Only three of 25 (12%) ANMs could produce records of community child tracking activities (dates of revisits were confirmed by the families). Second mechanism namely defaulter tracking bags were distributed to all subcenters 3 years back; however with the use of the new immunization cards, they have been rendered useless as the size of their pockets does not match the size of the cards. The third mechanism was SMS reminders to ANMs regarding dropouts in the recently introduced Mother and Child Tracking System software; however, none had received messages regarding migrant children.(15)
All six of the urban MCH centers had child tracking records and efforts for tracking were being documented by both ASHA and ANM. However, house-to-house immunization was being done in slums contrary to the fixed session site norm. The combined effort of the ASHA and ANM ensured 70% successful immunization of leftout/dropout children. All other cold chain and injection safety guidelines were being followed. There was evidence of session monitoring by nongovernmental organization (NGO) coordinators.
Key output indicators
There were no AEFI and no VPD outbreaks reported in the previous 3 years. Majority (90%) of the planned sessions was held; however, only 2% were monitored by medical officer/LHV in the previous year. Only 46% migrant mothers utilized immunization services in Haridwar [Table 3].
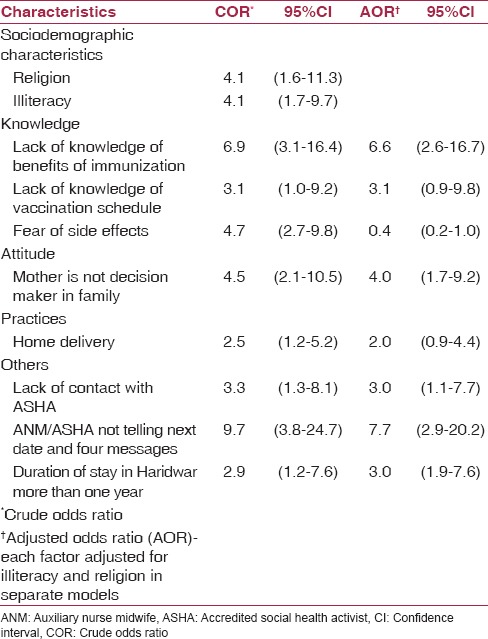
In the community survey, majority of mothers were Hindus (66%), illiterate (85%), and had a duration of stay in Haridwar of more than a year (86%). Of the 180 children surveyed, only 24% were fully vaccinated [Table 4]. The leading reason for partial/non vaccination were lack of awareness of the need to vaccinate (92%) and fear of side-effects (74%) [Figure 1]. In univariate analysis, we identified seven risk factors significantly associated with non/partial immunization. Among them, illiteracy (odds ratio (OR): 4.1 95%CI 1.7–9.7) and Muslim religion (OR 4.1, 95% CI 1.6–11.3) were the sociodemographic factors. Five modifiable risk factors namely lack of knowledge of benefits of immunization (adjusted OR (AOR) 6.6, 95% CI 2.6–16.7), mother not being decision maker for immunization (AOR 4.0, 95%CI 1.7–9.2), lack of contact with ASHA (AOR 3.0, 95%CI 1.1–7.7), not being informed by ANM/ASHA about next date and four messages (AOR 7.7,95% CI 2.9–20.2), and duration of stay for more than 1year (AOR3.0,95% CI 1.9–7.6) were significant after adjusting for illiteracy and Muslim religion in separate models [Table 5].
Table 4.
Coverage of each antigen among the migrants in Narsan and Bahadarabad blocks of Haridwar, Uttarakhand, India, 2012
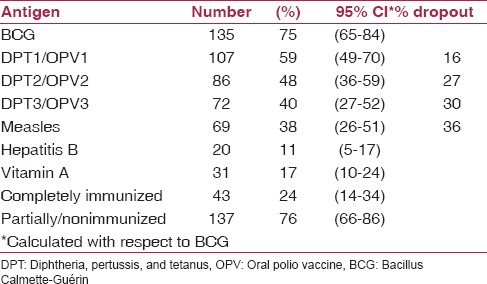
Figure 1.
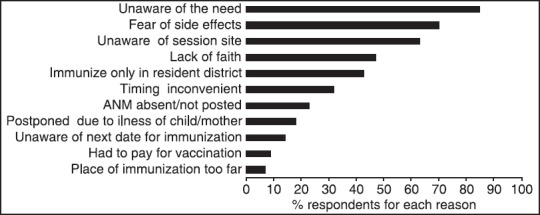
Reasons for non/partial immunization among migrant children in two blocks of Haridwar, Uttarakhand, India, 2012 (as per multiple responses given by respondents). ANM: Auxiliary nurse midwife
Table 5.
Factors associated with partial/non immunization in two blocks of Haridwar, Uttarakhand, India
Discussion
Our evaluation indicated low immunization coverage with gaps in the health system in terms of inadequate cold chain maintenance, inadequate monitoring, and poor implementation of systems for tracking dropouts. The community did not adequately utilize the services due to lack of counseling from the health staff, lack of awareness, and social determinants such as low literacy level.
We observed gaps in the cold chain maintenance and lack of adequate training of the staff regarding maintaining the temperatures at all points. This emphasis on cold chain quality checks for ensuring vaccine potency especially in outreach sessions has been suggested in a multistate study done on quality of cold chain supervision in India.(16) Programme managers need to be sensitized to cross verify temperature records at both storage point and during transit from center to field regularly and a suboptimal temperature should prompt a rapid corrective response.
Migration is an important determinant of child immunization.(17) Mothers despite long stay preferred vaccination in their resident district as the awareness and utilization of local health facilities was poor. Health-seeking behavior was similar to a study among migrants in Nigeria.(17) Complete immunization coverage in our study (24%) was lower than studies done in slums of Delhi and Lucknow, which showed 64 and 44%, respectively; but BCG to measles dropout rate of 36% was comparable.(1,7) Low awareness was one of the reasons in Lucknow study as well as our study.(1) This is in contrast to a study done in Delhi slums which showed that health services were better utilized by settled migrants in contrast to recent migrants due to their better adaptability to the sociocultural environment and better social networking.(7)
The health system was not adequately adapted to the needs of this special population of migrants. ANM/ASHAs who are the key personnel in ensuring immunization did not have adequate interaction with the mothers. Similar studies from Surat (India), Dhaka, and Nairobi showed that in spite of illiteracy amongst mothers, frequent contacts with community health workers with effective interpersonal communication can improve utilization of immunization services.(8,18,19) Migrant populations might require tailored strategies as used in an intervention study from slums of Dhaka. The interventions included user-friendly immunization outreach sites adjacent to large migrant clusters and at-home immunization in small clusters (maintaining proper cold chain) that led to improved coverage.(18) Another strategy could be timings of the immunization beyond the working hours with immunization booth locations in the vicinity to avoid loss of wages as suggested in a study in East China as well as a comprehensive review from India.(9,20)
The limitation of the study was the nonavailability of vaccination cards in the community. Vaccination had to be mostly verbally confirmed by mothers leading to recall bias. The strength of the study is that both programmatic factors and community level determinants have been evaluated to study risk factors for low immunization coverage among migrants.
We recommended mobile immunization teams comprising ANMs and ASHAs to cover widespread rural migrant clusters. Interventions such as counseling of parents, prelisting of migrant children with the help of local brickkiln managers/contractors at construction sites, and incentivizing ASHAs for these activities could be considered. All injection safety and cold chain guidelines were to be stringently implemented. Mechanisms to track dropouts and supervision needed to be strengthened to improve the coverage. In October 2013, Government of Uttarakhand, sanctioned a special “Brick Kiln Plan” which covers 200 kilns in Haridwar wherein every Tuesday 11 mobile immunization teams covered five brick kilns each. Three field supervisors were recruited for monitoring and microplanning. An “ASHA reward” scheme was initiated to encourage ASHAs working in migrant clusters for mobilizing the dropouts and left-outs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Nath B, Singh JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization coverage among 12–23 months old children in urban slums of Lucknow district, India. Indian J Med Sci. 2007;61:598–606. [PubMed] [Google Scholar]
- 2.World Health Organization. Global Immunization Data. 2012. Mar,
- 3.World Health Organization. Progress towards Global Immunization coverage-Summary presentation of key indicators. 2011. Aug,
- 4.International Institute of Population Sciences Mumbai, District Level Household Survey 3 Uttarakhand, India. Mumbai: Ministry of Health and family Welfare Government of India; 2007-2008. [Google Scholar]
- 5.United Nations Children's Fund (UNICEF) and Government of India - Ministry of Health and family Welfare, Coverage Evaluation Survey. New Delhi: National fact Sheet; 2011. [Google Scholar]
- 6.Sharma S. Immunization coverage in India. Institute of Economic growth. 2007-2008 [Google Scholar]
- 7.Kusuma YS, Kumari R, Pandav CS, Gupta SK. Migration and immunization: Determinants of childhood immunization uptake among socioeconomically disadvantaged migrants in Delhi, India. Trop Med Int Health. 2010;15:1326–32. doi: 10.1111/j.1365-3156.2010.02628.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma R, Desai VK, Kavishvar A. Assessment of immunization status in the slums of Surat by 15 clusters multi indicators cluster survey technique. Indian J Community Med. 2009;34:152–5. doi: 10.4103/0970-0218.51222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vashishtha VM, Kumar P. 50 years of immunization in India: Progress and future. Indian Pediatr. 2013;50:111–8. doi: 10.1007/s13312-013-0025-0. [DOI] [PubMed] [Google Scholar]
- 10.Government of India, Office of the Registrar General and Census commissioner of India, Delhi; Uttarakhand State data. Delhi: 2011. [Google Scholar]
- 11.International Institute of Population Sciences Mumbai, District Level Household Survey 3 District Haridwar, Uttarakhand, India. Mumbai: Ministry of Health and family Welfare Government of India; 2007-2008. [Google Scholar]
- 12.National Polio Surveillance Project (WHO-GOI collaboration), Routine Immunization monitoring report of Haridwar, NPSP office Haridwar, Uttarakhand. 2010.
- 13.Sub National immunization day (SNID) report of district Haridwar, Uttarakhand, India. 2012. Jun,
- 14.Facilitators Guide for medical officers—Handbook. New Delhi: 2009. Ministry of Health and family Welfare, Government of India. [Google Scholar]
- 15.Immunization handbook for health workers Handbook. New Delhi: 2009. Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- 16.Murhekar MV, Dutta S, Kapoor AN, Bitragunta S, Dodum R, Ghosh P, et al. Frequent exposure to suboptimal temperatures in vaccine cold-chain system in India: Results of temperature monitoring in 10 states. Bull World Health Organ. 2013;91:906–13. doi: 10.2471/BLT.13.119974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Antai D. Migration and child immunization in Nigeria: Individual and community level contexts. BMC Public Health. 2010;10:116. doi: 10.1186/1471-2458-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perry H, Weierbach R, Hossain I. Childhood immunization coverage in zone 3 of Dhaka City: The challenge of reaching impoverished households in urban Bangladesh. Bull World Health Organ. 1998;76:565–73. [PMC free article] [PubMed] [Google Scholar]
- 19.Mutua MK, Kimani-Murage E, Ettarh RR. Childhood vaccination in informal urban settlements in Nairobi, Kenya: Who gets vaccinated? BMC Public Health. 2011;11:6. doi: 10.1186/1471-2458-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu Y, Li Q, Chen E, Chen Y, Qi X. Determinants of childhood immunization uptake among socio-economically disadvantaged migrants in East China. Int J Environ Res Public Health. 2013;10:2845–56. doi: 10.3390/ijerph10072845. [DOI] [PMC free article] [PubMed] [Google Scholar]


