Abstract
Curcumol, isolated from the traditional medical plant Rhizoma Curcumae, is the bioactive component of Zedoary oil, whose potential anti-tumor effect has attracted considerable attention in recent years. Though many researchers have reported curcumol and its bioactivity, the potential molecular mechanism for its anti-cancer effect in colorectal cancer LoVo cells still remains unclear. In the present study, we found that curcumol showed growth inhibition and induced apoptosis of LoVo cells in a dose- and time-dependent manner. The occurrence of its proliferation inhibition and apoptosis came with suppression of IGF-1R expression, and then increased the phosphorylation of p38 mitogen activated protein kinase (MAPK), which might result in a cascade response by inhibiting the CREB survival pathway and finally triggered Bax/Bcl-2 and poly(ADP-ribose) polymerase 1 (PARP-1) apoptosis signals. Moreover, curcumol inhibited colorectal cancer in xenograft models of nude mice. Immunohistochemical and Western blot analysis revealed that curcumol could decrease the expression of ki-67, Bcl-2 as well as CREB1, and increase the expression of Bax and the phosphorylation of p38, which were consistent with our in vitro study. Overall, our in vitro and in vivo data confirmed the anti-cancer activity of curcumol, which was related to a significant inhibition of IGF-1R and activation of p38 MAPKs, indicating that curcumol may be a potential anti-tumor agent for colorectal carcinoma therapy.
Keywords: curcumol, colorectal cancer, anti-tumor, IGF-1R, p38 MAPK
1. Introduction
Colorectal cancer is the third most common cancer and the second cause of cancer death in the Unite States and worldwide [1], and more than 1,200,000 cases were diagnosed and about 600,000 deaths in recent years [2]. It has been recognized as a major public health issue in the Western world. Besides surgical treatment, chemotherapy is the most feasible therapy for colorectal cancer patients. Although the therapy targeting colorectal cancer has improved significantly, it has poor response rates, severe toxicities, high recurrence rates [3], and there is drug resistance to the chemotherapy [4,5]. Therefore, there is an urgent need to search for more effective medicine with fewer side effects for colorectal cancer treatment.
In recent years, more and more cancer therapeutics on the market or in preclinical trails turn to natural products with low toxicity and drug resistance. Chinese people have used the medicinal plant Rhizoma Curcumae for thousands of years. Curcumol (Figure 1a) with the structure of a guaiane-type sesquiterpenoid hemiketal, has been reported to possess antitumor, antiproliferation, anti-inflammatory, anti-hepatic fibrosis, antioxidant, and antimicrobial activities with low cytotoxicity [6,7]. Recently, it has been reported that curcumol exhibited growth inhibitory and induced apoptosis activity in several human cancer cell lines in vitro, including cervical carcinoma, breast carcinoma, lung carcinoma, gastric carcinoma and hepatocarcinoma [8,9]. Chen found that 300 μM of curcumol could induce HSC-T6 apoptosis, while showing little toxicity to the normal liver cell line BRL-3A [10]. Tang found that curcumol (60 mg/kg) did not cause notable toxicity to the nude mouse [11]. Despite the increasing interest in the anti-tumor activity of curcumol, the mechanisms and signaling path against cancer are still unclear and no studies have investigated how curcumol induces colorectal cancer cell death in vivo.
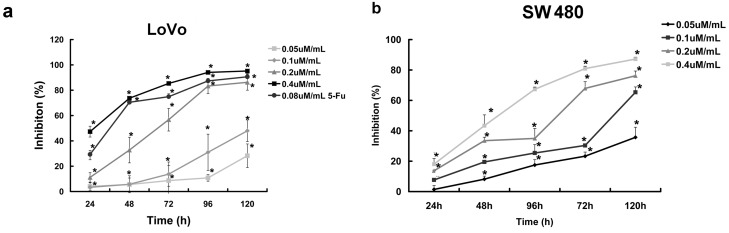
Figure 1.
Curcumol inhibited proliferation of human colorectal cancer cell. (a) Dose- and time-dependent inhibition effect of cucumol on LoVo cells was evaluated by MTT assay; and (b) Dose- and time-dependent inhibition effect of cucumol on SW 480 cells was evaluated by MTT assay. Data represent mean ± SD from at least three independent experiments. * p < 0.05 when compared with the untreated control group.
Insulin-like factor-1 receptor (IGF-1R) is involved in many tissues and mainly regulates growth and survival, and is recognized as a unique factor for malignant cells. Thus, IGF-1R blockade can inhibit tumor growth, angiogenesis and enhance chemotherapy-induced apoptosis. Recent studies have demonstrated that IGF-1R plays a crucial role in the oncogenesis and development of colorectal cancer [12,13,14]. Many studies have shown that the activation of IGF-1R is involved in many cellular signaling pathways [15,16], as a tyrosine kinase-containing transmembrane receptor, up-regulation of IGF-IR will relate to several intracellular second messenger pathways, including the mitogen activated protein kinase (MAPK) and phosphatidylinositol 3-kinase (PI3K) pathways [17,18,19]. MAPK signal pathways also play key roles in a number of biological processes [20,21,22]. It is necessary to clarify the regulating mechanism of curcumol on IGF-1R as well as the downstream signal pathway. In this study, we discovered that the anti-tumor effect of curcumol on colorectal cancer in vitro and in vivo. We found that curcumol inhibited proliferation and induced cell apoptosis in colorectal cancer cells. Moreover, this antitumor activity of curcumol was correlated with the down-regulation of IGF-1R and the up-regulation of p38 MAPK pathways, and finally the activation of PARP-1 cleavage.
2. Result
2.1. Curcumol Inhibited Cell Proliferation of Colorectal Cancer
To investigate the effect of curcumol on colorectal cancer cells viability, we first examined the inhibition effect of different concentrations of curcumol on the growth of LoVo and SW 480 cells at five different points and then cell viabilities were measured by MTT assay (Figure 1a,b). The result showed that curcumol exhibited a significant inhibition of cell viability in a dose- and time-dependent manner. The 50% growth inhibition of LoVo cells (IC50%) at 24, 48, 72, 96 and 120 h were 0.48, 0.31, 0.24, 0.15 and 0.11 μΜ/mL, respectively. Moreover, we have also detected the long-term effects of curcumol on cell survival using colony-formation assays as described below.
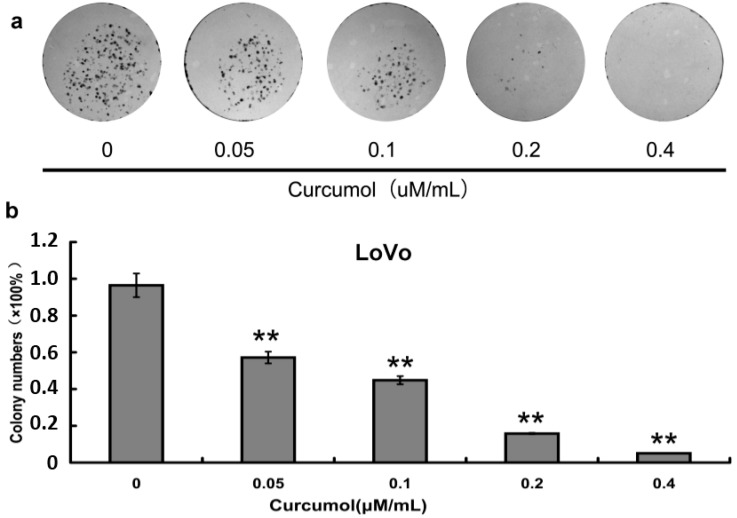
2.2. Inhibition of Cell Survival by Colony-Formation Assay
To further evaluate the inhibition effect of curcumol on cell viability, after curcumol treatment colony-formation assay was performed. As shown in Figure 2a,b, curcumol showed a significant inhibition on colony formation in a dose-dependent manner when compared with control group, and at a concentration of 0.4 μΜ/mL curcumol, nearly no colonies were detected. The results from clonogenic assay demonstrated that curcumol could significantly inhibit the colorectal cancer reproductive potentials compared with the control group, which were consistent with the result from MTT assay.
Figure 2.
Curcumol inhibited human colorectal cancer cell viability. (a) Cell colony formation was evaluated by clonogenic assay; and (b) Statistical results of colony-forming assays presented as surviving colonies (percentage of untreated control). Data are expressed as mean ± SD from at least three independent experiments, ** p < 0.01 when compared with the untreated control group.
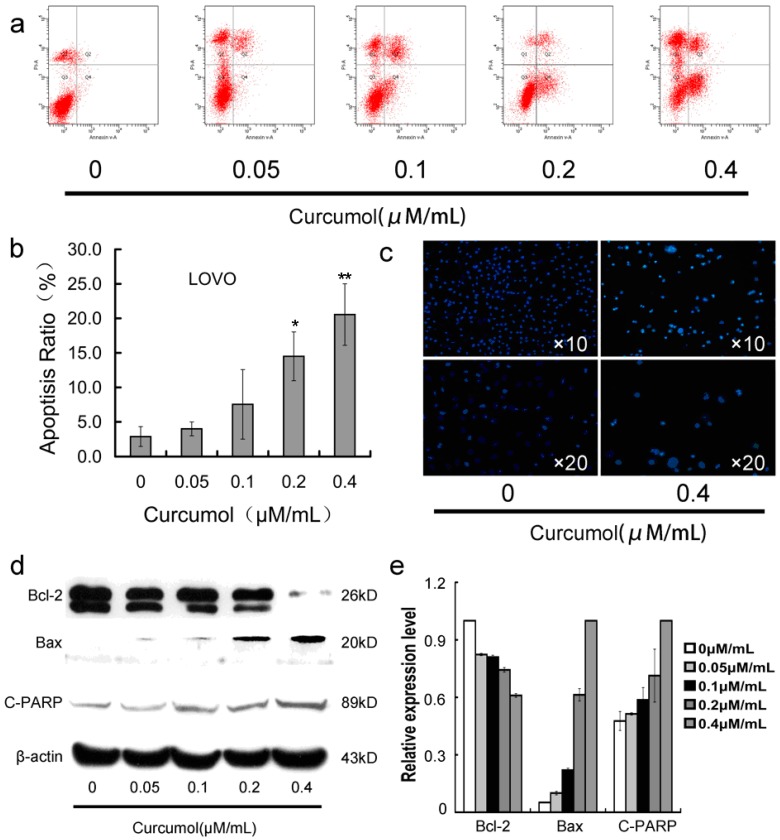
2.3. Curcumol Caused Apoptosis in Colorectal Cancer Cells
Furthermore, in order to determine whether the inhibition effect of curcumol on colorectal cancer cells is associated with triggering the programmed cell death pathways, we then analyzed the apoptosis-induction effect of curcumol in LoVo cells. As shown in Figure 3c, the LoVo cells exhibited apoptotic features after treatment with curcumol by Hoechst 33,258 staining. Cells with bright-blue fluorescent condensed nuclei, reduction of cell volume and nuclear fragmentation were obviously observed at 0.4 μΜ/mL curcumol, however, almost none were found in the control group. To confirm the quantity of cell death, Annexin V-FITC and PI fluorescence staining assay were performed by flow cytometry. As shown in Figure 3a,b, curcumol induced LoVo cells apoptosis in a dose-dependent manner at 48 h. Meanwhile, Western blotting results (Figure 3d,e) showed that curcumol decreased the expression of Bcl-2 in an obvious concentration-dependent manner, while significantly increased the expression of bax and cleaved PARP-1.
Figure 3.
Curcumol induced apoptosis in human colorectal cancer cells. (a) Cells were treated with curcumol for 48 h and analyzed by flow cytometry after AnnexinV-FITC/PI staining; (b) Statistical results of apoptosis assays by FCM presented as surviving cells (percentage of untreated control); (c) Cells were treated with curcumol for 48 h and analyzed after Hoechst 33258 staining; and (d,e) Bax, Bcl-2 and PARP involved in apoptosis were analyzed by Western blotting. Cells were treated with curcumol for 48 h, and total proteins were extracted. Equal protein loading was evaluated by β-actin. Data are represented as means ± SD from at least of three independent experiments. * p < 0.05, ** p < 0.01 when compared with the untreated control group.
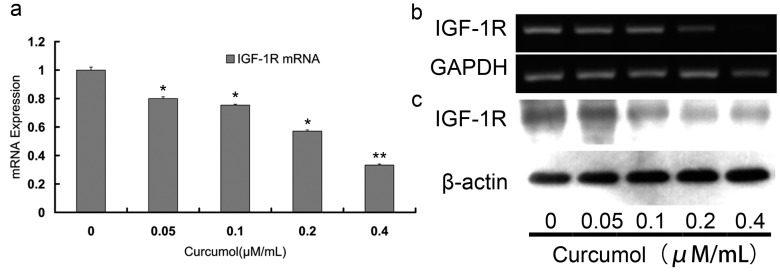
2.4. Curcumol Down-Regulated IGF-1R Levels
A functional IGF-1R caused anchorage-independent growth in various cancers and activated proliferation and survival signaling pathway [12,23,24]. Numerous studies indicated that IGF-1R may be a promising target for tumor therapy. It has been reported that IGF-1R was overexpressed in more than 90% colorectal carcinomas, which contributed to the malignant characteristics of aggressive growth and poor prognosis [14,25]. To investigate IGF-1R activity in colorectal carcinomas cells following curcumol treatment, the transcription level of IGF-1R was analyzed by the RT-PCR and quantitative real time PCR. We found that increasing concentrations of curcumol decreased IGF-1R mRNA level (Figure 4a,b). Furthermore, we examined the IGF-1R changes at protein level by Western blotting (Figure 4c). As shown in Figure 4c, after treatment with curcumol for 48 h, the protein levels of IGF-1R decreased dose-dependently.
Figure 4.
Curcumol down-regulated the expression of IGF-1R in human colorectal cancer cells. The mRNA expression of IGF-1R was detected by real-time PCR (a) and RT-PCR (b); (c) The expression of IGF-1R was analyzed by Western blot. Cells were treated with curcumol for 48 h, and total proteins were extracted. Equal protein loading was evaluated by β-actin. Data are represented as means ± S.D. from at least of three independent experiments. * p < 0.05, ** p < 0.01 when compared with the untreated control group.
2.5. The p38 MAPK Pathways Were Involved in the Anti-Tumor Effects of Curcumol
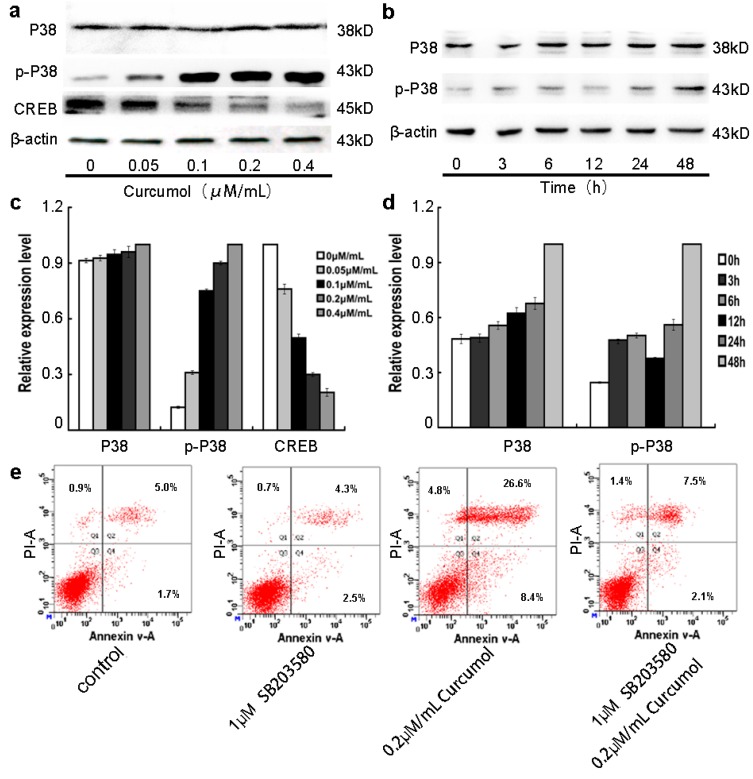
MAPK intracellular signaling cascades are involved in the IGF-1R mediated signals pathways [17,24]. It is reported that p38 MAPK acts as a tumor suppressor in various cancer cells [21,26,27], Liu showed that activation of ERK1/2 and suppression of p38 MAPK pathways might be the molecular mechanisms for the malignant behavior of colon cancer cells [28]. Hui has indicated that activation of p38 MAPK could induce apoptosis in colorectal carcinoma cells [29]. To clearly understand the underlying molecular signaling pathways by which curcumol exerted anti-proliferation effect on colorectal cancer cells, we investigated the effects of curcumol on MAPK pathways by Western blot analysis. As shown in Figure 5a,c, we found that increasing concentrations of curcumol significantly increased the expression of phosphorylated p38 and decreased the CREB expression in a dose-dependent manner, while it had no effect on the total levels of p38. Furthermore, we detected the levels of p38 and phosphorylated p38 at the different points. The increase of phosphorylated p38 was observed over time in curcumol-treated LoVo cells (Figure 5b,d). In addition, LoVo cells were treated with p38 inhibitor SB203580. No obvious cell number changes were found in SB203580-treated groups from 0.5 to 5 μM concentration (according the protocol of SB203580). Then, we performed an apoptotic assay by flow cytometry in LoVo cells upon treatment with SB203580, curcumol, or SB203580 combined with curcumol, and the results show that the presence of apoptotic LoVo cells following curcumol treatment (Figure 5e). Combined with the FCM results, our study demonstrated that curcumol induced LoVo cells apoptosis via activation of p38 MAPK and its downstream signal pathway.
Figure 5.
Involvement of p38 MAPK pathway in the anti-tumor effect of curcumol. (a,c) Cells were treated with curcumol (0, 0.05, 0.1, 0.2 and 0.4 μΜ/mL) for 48 h, and the total proteins were extracted. The expression levels of p38, phospho-p38 and CREB were analyzed by Western blotting; (b,d) Cells were treated with 0.2 μΜ/mL curcumol for 0, 3, 6, 12, 24, and 48 h. The whole cell lysates were prepared to test the expression levels of p38 and phospho-p38. Equal protein loading was evaluated by β-actin; and (e) Cells were treated with SB203580 and curcumol for 48 h after AnnexinV-FITC/PI staining flow cytometry analysis was performed. Representative data are shown from three independent experiments.
2.6. Curcumol Suppressed Tumor Growth in Vivo
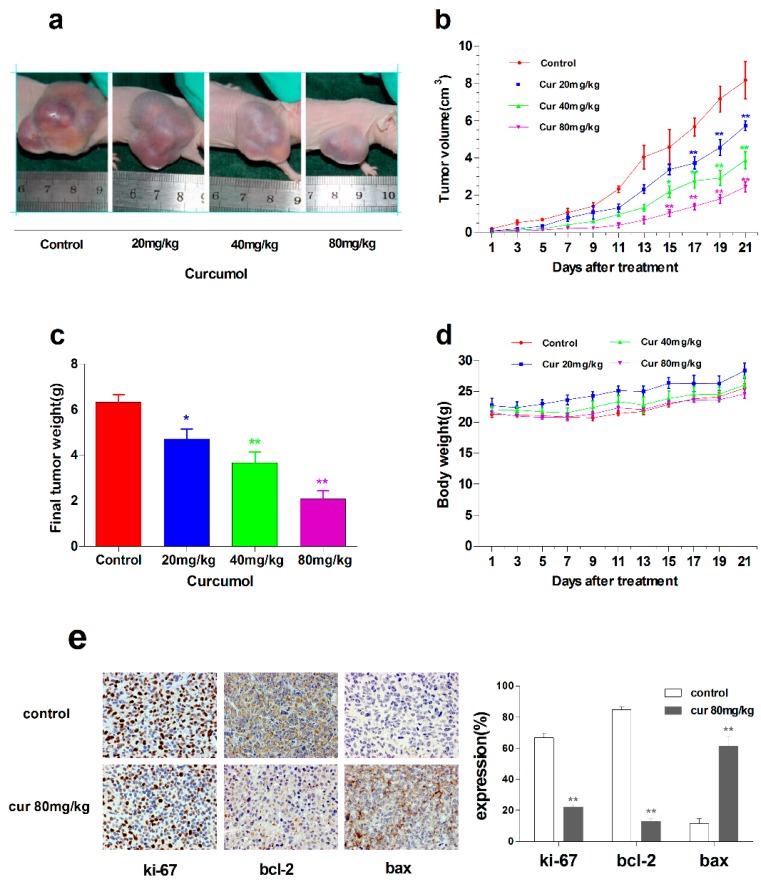
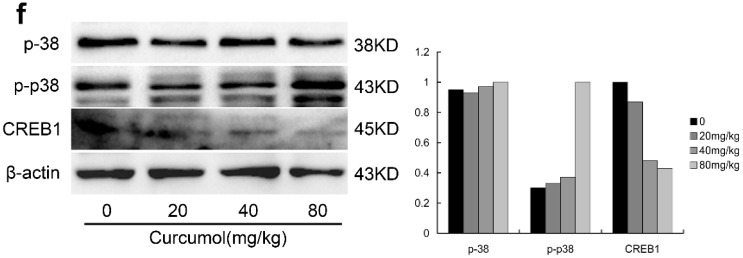
After assessing the anti-tumor activity of curcumol in colorectal cancer in vitro, further study was carried out to investigate the anti-tumor effects of curcumol in vivo. LoVo cells were xenografted subcutaneously into the right flanks of BALB/c nude mice to establish xenografts. Tumor-bearing mice were treated with vehicle or curcumol at a dosage of 20, 40 or 80 mg/kg/day for the LoVo model. Curcumol substantially suppressed tumor growth in a dose-dependent manner (Figure 6a); significant reductions in tumor volume (Figure 6b) and tumor weight (Figure 6c) were observed in the curcumol-treated groups, and, especially, tumor progression inhibition was nearly 70% in 80 mg/kg group. Furthermore, curcumol-treated groups were well tolerated and did not show significant loss in body weight (Figure 6d).
Figure 6.
Curcumol suppressed the growth of human colon tumors in vivo. Nude mice bearing LoVo human colon xenografts were treated with physiological saline or curcumol at three doses (20, 40, 80 mg/kg of body weight) for 21 days. (a) Representative tumor pictures; (b) Tumor volume was recorded every three days; (c) Tumor weight was evaluated on the twenty-first day; (d) Body weight was recorded every three days; (e) Immunohistochemical staining of tumor specimens; and (f) The level of p38, phospho-p38 and CREB was analyzed by Western blot. Data are represented as mean ± SD; n = 6 mice per group. * p < 0.05 ** p < 0.01 when compared with the untreated control group.
Consistent with in vitro results, ki-67, a proliferation marker of tumors was significantly decreased in curcumol-treated groups. Bax, an apoptosis implication of tumors, was remarkably increased, whereas anti-apoptosis factor Bcl-2 was decreased after curcumol treatment. Furthermore, we found that the expression of CREB1 was inhibited and phosphorylated p38 was up-regulated in curcumol-treated groups (Figure 6f).
3. Discussion
A lot of crude medicine has been applied to clinical therapy due to their effectiveness and fewer side effects. Curcumol, a pure monomer, extracted from the traditional Chinese medicine Rhizoma Curcumae, has recently been found to have anti-tumor effect on many cancer cells [8,9,30]. Though Zhang’s study showed that curcumol induced apoptosis in lung cancer ASTC-a-1 cells via caspase-independent pathway, but the anticancer mechanism is still unclear. In this study, we evaluated the anti-tumor effect of curcumol on human colorectal cancer cells and investigated the possible underlying mechanism.
Since uncontrolled cell growth is the main biological behavior of malignant tumor [31], we first investigated whether curcumol inhibited proliferation of colorectal cancer cells. Our results showed that curcumol inhibited LoVo cells proliferation in a time- and dose-dependent manner. Apoptosis is a programmed cell death and is a key target in the development of new anti-cancer therapies [32,33]. Curcumol treatment for 48 h could induce LoVo cells apoptosis. The regulation of pro- and anti-apoptotic factor was involved in the progress of cell apoptosis. In the present study, curcumol showed the apoptosis-induction effect with an increase in the Bax/Bcl-2 ratio, and at the same time, curcumol also caused a remarkable cleavage of PARP, which is a marker of early apoptosis.
Numerous evidences have confirmed that IGF-1R was a promising target for cancer therapy [19,34], which was overexpressed in colorectal cancer (CRC), and mediated anti-apoptosis activity in CRC development [24,35]. Due to the important role of IGF-1R in proliferation and survival, inhibition of IGF-1R has been shown to be an efficient approach for cancer therapy [35]. Our results demonstrated that the increasing concentration of curcumol decreased the level of IGF-1R, indicating that IGF-1R was involved in the anti-cancer mechanism of curcumol in LoVo cells.
Valenciano reported that IGF-1R exerted its main action through MAPK and PI3k pathways [19], then blockade of IGF-1R resulted in the changes of the down-stream signals [36], which was involved in p38 MAPK activation [17]. P38 MAPKs have been reported to mediate apoptosis, proliferation and differentiation [1,37,38]. Activation of p38 MAPK in several tumor cells induces apoptosis depending on the cellular context, cancer stage and the stimuli [39]. Gupta found that p38 MAPK deficiency resulted in tumorigenesis in colon cancer [39]. Many studies suggested that p38 MAPK was a negative regulator of malignant transformation and showed pro-apoptotic effects in tumor cells [22,40,41]. Inhibition of p38 MAPK could enhance tumor development in vivo or induce resistance to chemotherapy [4,38,42]. However, upregulation of p38 MAPK induced cell cycle arrest or apoptosis [43]. Diane demonstrated that PBA could suppress human lung carcinoma cell growth via activation of p38 [44]. In A549, U2OS, BXPC3 and PANC-1 Cell lines, oleanolic acid exerted certain anti-tumor activity by inducing apoptosis which required the p38 activation [45,46]. In human colonic carcinoma, many studies have revealed that activation of p38 by the berberine or garlic-derived compound s-allylmercaptocysteine could cause tumor cells apoptosis [40,47]. However, it is still unknown whether p38 MAPK pathway is involved in the anti-tumor activity of curcumol on CRC cells. Here, we found that the phosphorylated p38 MAPK was enhanced by up-regulation of phosphorylated p38 MAPK in curcumol-treated CRC LoVo cells. However, inactivation of p38 caused the decrease of the pro-apoptosis effect upon curcumol treatment. Moreover, p38 MAPK exerted pro-apoptosis functions by direct or indirect regulating apoptosis-related factors, such as CREB, Bcl-2, Bax, PARP and so on [5,29,35,48,49]. Curcumol treatment resulted in an increased expression of Bax, a decreased expression of CREB1 and Bcl-2 in LoVo cells. Meanwhile, we also found the cleavage of PARP in a dose-dependent manner, which was consistent with our previous study in lung cancer [50]. As we all know, the Bcl-2 family is engaged in the apoptosis progress in nearly all cancer cells. Either inhibiting the expression of Bcl-2 or enhancing the expression of Bax could be an effective approach for cancer therapy. Our previous work indicated that curcumol induced tumor cells apoptosis via down-regulation of Bcl-2, while the mechanism is not very clear [30]. Hui showed that CREB, which is a direct substrate of p38 MAPK, regulated Bcl-2 expression [29]. In our current study, we also found that curcumol inhibited the expression of Bcl-2 as well as CREB, while it is not been verified whether CREB directly regulated expression of Bcl-2, which was involved in the curcumol-induced apoptosis, and then stimulate the downstream apoptosis signal. Thus, more work needed to be performed to find the defined mechanism of curcumol-induced apoptosis, which is a main focus of our further study.
To investigate the effect of curcumol in vivo and find an appropriate dose in cancer therapy, we established colorectal cancer subcutaneous tumor model in nude mice. We treated the mice with three different doses (20, 40 and 80 mg/kg) by intraperitoneal injection every day. We discovered that the tumor volume was markedly attenuated in curcumol-treatment groups, and no adverse effects were observed on body weight and activity compared with the control group. There was no any pathological change in the kidney and liver tissue of curcumol-treated mice compared with the control group by hematoxylin-eosin (HE) staining. Moreover, the level of Bax and phosphorylated p38 were increased by immunohistochemical and Western blot analyses, while the level of Bcl-2 and CREB1 were decreased in curcumol-treated groups, which were consistent with in vitro apoptosis effect of curcumol.
In conclusion, these signaling cascades ultimately contributed to the curcumol-induced apoptosis in LoVo cells. In this paper, we investigated the anti-proliferative effects of curcumol on colorectal cancer in vitro and in vivo, revealing the potential molecular mechanism of curcumol in CRC LoVo cells. The main findings also included the following: (1) Our work presented evidence to demonstrate that curcumol regulated the expression of IGF-1R in colon cancer cells; (2) Curcumol induced LoVo cell apoptosis via an IGF-1R/p38 MAPK signal pathway; (3) Curcumol could suppress the growth of human colorectal cancer xenografts in vivo. All of the above findings suggested that curcumol might be used as a potential anti-cancer agent in colon cancer treatment.
4. Experimental Section
4.1. Ethics Statement
This study was carried out in strict accordance with the institutional guidelines of Guilin medical college (GLMC) Animal Care and Use Committee. The protocol was approved by the Committee on the Ethics of Animal Experiments of GLMC (Permit Number: 35).
4.2. Drugs and Reagents
Curcumol (lot: 100185-200506) was obtained from National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China). 3-(4,5)-dimethylthiahiazo(-z-y1)-2,5-di-phenytetrazolium bromide (MTT) and dimethyl sulfoxide (DMSO) were purchased from Amerso Chemical Co. (Amresco, Cochran Solon, OH, USA). Propidium iodide (PI) and Annexin V-FITC apoptosis detection kit were purchased from BD Biosciences (Bedford, MA, USA). Hoechst 33258 was purchased from Kaiji Biotechnology (Nanjing, China). The antibodies against Bax, PPAR and p-p38 were obtained from Wanlei Biotechnology Company (Shenyang, China), IGF-1R and p38 were purchased from Abcam Company (Cambridge, UK). Antibody β-actin and Bcl-2 were purchased from Santa Cruz Biotechnology Company (Santa Cruz, CA, USA).
4.3. Cell Culture
Human LoVo and SW 480 cell lines were obtained from the Guilin medical university (Guilin, China). Cells were cultured in DMEM medium (Gibco BRL, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS; Gibco, Auckland, New Zealand), 100 units/mL penicillin and 100 units/mL streptomycin under humidified conditions with 5% CO2 at 37 °C. Cells without curcumol treatment served as a control group. Curcumol was dissolved in the absolute ethyl alcohol as a 10 mg/mL, and then diluted by the 10% FBS DMEM medium.
4.4. Cell Proliferation Assay
The sensitivity of cells to curcumol was measured using the MTT assay. Briefly, 800 cells/well were plated in a 96 well plate. The next day, cells were treated with different concentrations of curcumol (0.05, 0.1, 0.2 and 0.4 μΜ/mL), a positive control (0.08 μΜ/mL 5-fu) and negative control (1% of anhydrous alcohol culture medium). After 24, 48, 72, 96 and 120 h, 20 μL/well of 5 mg/mL MTT solution was added to each well and further incubated for 4 h at 37 °C. The formazan crystals formed in the wells were solubilized by adding solubilization solution and incubating the plates at 37 °C 30 min with slight shake. The plates were read at 490 nm on a TECH M200 plate reader (TECH, Switzerland). The percentage cell growth inhibition for each treatment group was calculated by adjusting the untreated control group to 100%. All experiments were repeated at least 3 times.
4.5. Colony Formation Assay
To test the survival of LoVo treated with curcumol, the cells were plated 4 × 104–8 × 104 per well) in a six-well plate and incubated overnight at 37 °C. After 48 h exposure to various concentrations of curcumol, then the cells were trypsinized, and the viable cells were counted and plated in 100 mm Petri dishes in a range of 100 to 1000 cells to determine the plating efficiency as well as assess the effects of treatment on clonogenic survival. The cells were then incubated for 10 to 12 days at 37 °C with 5% CO2. The colonies were fixed by 4% paraformaldehyde solution, stained with Giemsa stain and then counted. The surviving fraction was normalized to untreated control cells with respect to clonogenic efficiency.
4.6. Morphological Analysis after Hoechst Staining
Morphological changes associated with apoptosis in LoVo cells were detected by Hoechst 33258 staining. Briefly, the cells were plated in 6-well plates for 12 h and then treated with various concentrations of curcumol for another 48 h. After treatment, cells were washed with cold PBS and fixed in paraformaldehyde solution for 20 min. The cells were stained with Hoechst 33258 solution (5 μg/mL) followed by PBS washing and examination under fluorescence microscope (olympusIX71FL, Tokyo, Japan) to identify the nuclear morphology of apoptotic cells.
4.7. Apoptosis Analysis by Flow Cytometry (FCM)
To further confirm that curcumol could induce cell apoptosis by flow cytometry using Annexin V-FITC apoptosis detection kit. To put it simply, after treatment with different concentrations of curcumol for 48 h as described above, cells were harvested and washed with cold PBS twice. After centrifugation, cells were stained with Annexin V-FITC and PI, and then analyzed with FCM (Becton Dickinson, San Jose, CA, USA).
4.8. RT-PCR and Real-Time PCR Analysis
Total RNA was extracted from LoVo cells with Trizol reagent (TIANGEN, China), followed by being reversely transcribed into cDNA via M-MLV first strand RT Kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. QPCR was performed using SYBR premix Ex Taq (ABI) on 7500 fast Real-Time PCR Detection System (ABI, Foster, CA, USA) supplied with analytical software. The following primers were used: upper IGF-1R 5′-CCATTCTCATGCCTTGGTCT-3′; lower IGF-1R 5′-TGCAAGTTCTGGTTGTCGAG-3′ [23]; upper GAPDH 5′-ACCACAGTCCATGCCATCAC-3′; lower GAPDH 5′-TCCACCACCCTGTTGCTGTA-3′ [15].
4.9. Western Blot Analysis
After treatment with the different concentrations of curcumol for 48 h, cells were lysed in RIPA lysis buffer (Beyotime, Shanghai, China) with protease and phosphatase inhibitor cocktail tablets (Roche, Mannheim, Germany). Then, lysates were centrifuged at 12,000× g for 25 min at 4 °C. The supernatant was harvested and the protein concentration was measured by the BCA protein assay kit (Beyotime). An equivalent amount of protein was resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a nitrocellulose membrane. Membranes were blocked for 1 h in 5% (w/v) skim milk in PBST (with 0.1% Tween 20) at room temperature, and then incubated at 4 °C overnight with primary antibodies in PBST with 5% skim milk. Horseradish peroxidase-labeled anti-mouse or anti-rabbit secondary antibodies were added for 1 h at 37 °C and detected with enhanced chemiluminescence (ECL) reagent (BIO-RAD, Hercules, CA, USA), and exposed to medical X-ray film. The optical density of protein bands was measured using Image J software (BIO-RAD). The optical density of each band was normalized by β-actin optical density.
4.10. Xenograft Tumor Models
Five-week-old BALB/c athymic nude mice weighting approximately 20 g were purchased from Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai, China) and were caged in standard laboratory conditions. LoVo tumor cells resuspended in 200 μL PBS and were injected subcutaneously in the right flanks of nude mice. When tumors reached an average volume of 100 mm3, the mice were randomly assigned to four groups. Curcumol was dissolved in 90% propylene glycol. Three groups of nude mice were treated with 200 μL curcumol in 90% propylene glycol by intraperitoneal injection at a series dose of 20, 40, 80 mg/kg per day, respectively, and 200 μL 90% propylene glycol were injected into the last group and used as the control. Tumor size and body weight were measured by periodic measurements with calipers every three days, and clinical symptoms were observed daily. Tumor volume was calculated using the following formulae: V = (length × width2/2) [3]. After 3 weeks treatment, mice were killed and tumor tissues were embedded in paraffin for further analysis. All surgery was performed under sodium pentobarbital anesthesia, and all efforts were made to minimize suffering.
4.11. Statistical Analysis
All data are presented as mean ± SD of at least three independent experiments. ANOVA, followed by multiple comparison post hoc test, or Kruskal–Wallis, was used to assess the statistical significance in difference groups. p < 0.05 indicated a statistically significant difference.
Acknowledgments
The work was supported by a grant from the National Natural Science Foundation of China (31460029), a grant from the Science Research and Technology Development Program of Guangxi (Guikezhong 1355001-5-7), a grant from the Scientific Research and Technology Development Projects of Guilin (20140105-8) and a grant from the Small Talent Highland Fund in Guangxi (1415).
Abbreviations
- CRC
colorectal cancer
- IGF-1R
insulin-like factor-1 receptor
- CREB
cAMP-response element binding protein
- PARP-1
Poly (ADPribose) polymerase 1
- MAPK
mitogen activated protein kinase
- P13k
phosphatidylinositol 3-kinase.
Author Contributions
Conceived and designed the experiments: Xu Chen and Jiacai Wu; Performed the experiments: Zhun Bai, Juan Wang, Bixia Chi and Fengxiang Huang; Analyzed the data: Juan Wang and Zhun Bai; Contributed reagents/materials/analysis tools: Xu Chen and Fengxiang Huang; Wrote the paper: Juan Wang.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Grossi V., Peserico A., Tezil T., Simone C. p38α MAPK pathway: A key factor in colorectal cancer therapy and chemoresistance. World J. Gastroenterol. 2014;20:9744–9758. doi: 10.3748/wjg.v20.i29.9744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R., Naishadham D., Jemal A. Cancer statistics, 2013. CA Cancer J. Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 3.Song X.J., Xia Y., Wang N.Y., Zhang L.D., Shi X.H., Xu Y.Z., Ye T.H., Shi Y.J., Zhu Y., Yu L.T. A Novel benzothiazole derivative YLT322 induces apoptosis via the mitochondrial apoptosis pathway in vitro with anti-tumor activity in solid malignancies. PLoS ONE. 2013;8:e63900. doi: 10.1371/journal.pone.0063900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang W., Su G., Li J., Liao J., Chen S., Huang C., Liu F., Chen Q., Ye Y. Enhanced anti-colorectal cancer effects of carfilzomib combined with CPT-11 via downregulation of nuclear factor-κB in vitro and in vivo. Int. J. Oncol. 2014;45:995–1010. doi: 10.3892/ijo.2014.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seitz S.J., Schleithoff E.S., Koch A., Schuster A., Teufel A., Staib F., Stremmel W., Melino G., Krammer P.H., Schilling T., et al. Chemotherapy-induced apoptosis in hepatocellular carcinoma involves the p53 family and is mediated via the extrinsic and the intrinsic pathway. Int. J. Cancer. 2010;126:2049–2066. doi: 10.1002/ijc.24861. [DOI] [PubMed] [Google Scholar]
- 6.Dang Y.Y., Li X.C., Zhang Q.W., Li S.P., Wang Y. Preparative isolation and purification of six volatile compounds from essential oil of Curcuma wenyujin using high-performance centrifugal partition chromatography. J. Sep. Sci. 2010;33:1658–1664. doi: 10.1002/jssc.200900453. [DOI] [PubMed] [Google Scholar]
- 7.Jiang Y., Li Z.S., Jiang F.S., Deng X., Yao C.S., Nie G. Effects of different ingredients of zedoary on gene expression of HSC-T6 cells. World J. Gastroenterol. 2005;11:6780–6786. doi: 10.3748/wjg.v11.i43.6780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu L.C., Bian K.M., Liu Z.M., Zhou J., Wang G. The inhibitory effect of the curcumol on women cancer cells and synthesis of RNA. Tumor. 2005;25:570–572. [Google Scholar]
- 9.Zhang W.W., Wang Z.P., Chen T. Curcumol induces apoptosis via caspases-independent mitochondrial pathway in human lung adenocarcinoma ASTC-a-1 cells. Med. Oncol. 2011;28:307–314. doi: 10.1007/s12032-010-9431-5. [DOI] [PubMed] [Google Scholar]
- 10.Chen G., Wang Y., Li M., Xu T., Wang X., Hong B., Niu Y. Curcumol induces HSC-T6 cell death through suppression of Bcl-2: Involvement of PI3K and NF-κB pathways. Eur. J. Pharm. Sci. 2014;65:21–28. doi: 10.1016/j.ejps.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Tang Q.L., Guo J.Q., Wang Q.Y., Lin H.S., Yang Z.P., Peng T., Pan X.D., Liu B., Wang S.J., Zang L.Q. Curcumol induces apoptosis in SPC-A-1 human lung adenocarcinoma cells and displays anti-neoplastic effects in tumor bearing mice. Asian Pac. J. Cancer Prev. 2015;16:2307–2312. doi: 10.7314/apjcp.2015.16.6.2307. [DOI] [PubMed] [Google Scholar]
- 12.Larsson O., Girnita A., Girnita L. Role of insulin-like growth factor 1 receptor signalling in cancer. Br. J. Cancer. 2005;92:2097–2101. doi: 10.1038/sj.bjc.6602627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitsiades C.S., Mitsiades N.S., McMullan C.J., Poulaki V., Shringarpure R., Akiyama M., Hideshima T., Chauhan D., Joseph M., Libermann T.A., et al. Inhibition of the insulin-like growth factor receptor-1 tyrosine kinase activity as a therapeutic strategy for multiple myeloma, other hematologic malignancies, and solid tumors. Cancer Cell. 2004;5:221–230. doi: 10.1016/S1535-6108(04)00050-9. [DOI] [PubMed] [Google Scholar]
- 14.Weber M.M., Fottner C., Liu S.B., Jung M.C., Engelhardt D., Baretton G.B. Overexpression of the insulin-like growth factor I receptor in human colon carcinomas. Cancer. 2002;95:2086–2095. doi: 10.1002/cncr.10945. [DOI] [PubMed] [Google Scholar]
- 15.Attias Z., Werner H., Vaisman N. Folic acid and its metabolites modulate IGF-I receptor gene expression in colon cancer cells in a p53-dependent manner. Endocr. Relat. Cancer. 2006;13:571–581. doi: 10.1677/erc.1.01156. [DOI] [PubMed] [Google Scholar]
- 16.Rive S., Yael F., Zohar A.G., Ami F., Ilan B., Haim W. Metformin downregulates the insulin/IGF-I signaling pathway and inhibits different Uterine Serous Carcinoma (USC) Cells proliferation and migration in p53-dependent or -independent manners. PLoS ONE. 2013;8:e61537. doi: 10.1371/journal.pone.0061537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen J., Hou R., Zhang X., Ye Y., Wang Y., Tian J. Calycosin suppresses breast cancer cell growth via ERβ-dependent regulation of IGF-1R, p38 MAPK and PI3K/Akt pathways. PLoS ONE. 2014;9:e91245. doi: 10.1371/journal.pone.0091245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heller G., Zöchbauer-Müller S. Insulin-like growth factor type I receptor: A new target in the treatment of non-small cell lung cancer patients. memo-Mag. Eur. Med. Oncol. 2010;3:81–84. doi: 10.1007/s12254-010-0192-9. [DOI] [Google Scholar]
- 19.Valenciano A., Henríquez-Hernández L.A., Moreno M., Lloret M., Lara P.C. Role of IGF-1 receptor in radiation response. Transl. Oncol. 2012;5:1–9. doi: 10.1593/tlo.11265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhillon A.S., Hagan S., Rath O., Kolch W. MAP kinase signalling pathways in cancer. Oncogene. 2007;26:3279–3290. doi: 10.1038/sj.onc.1210421. [DOI] [PubMed] [Google Scholar]
- 21.Wagner E.F., Nebreda A.R. Signal integration by JNK and p38 MAPK pathways in cancer development. Nat. Rev. Cancer. 2009;9:537–549. doi: 10.1038/nrc2694. [DOI] [PubMed] [Google Scholar]
- 22.Hui L., Bakiri L., Mairhorfer A., Schweifer N., Haslinger C., Kenner L., Komnenovic V., Scheuch H., Beug H., Wagner E.F. p38α suppresses normal and cancer cell proliferation by antagonizing the JNK-c-Jun pathway. Nat. Genet. 2007;39:741–749. doi: 10.1038/ng2033. [DOI] [PubMed] [Google Scholar]
- 23.Di Conza G., Buttarelli M., Monti O., Pellegrino M., Mancini F., Pontecorvi A., Scotlandi K., Moretti F. IGF-1R/MDM2 relationship confers enhanced sensitivity to RITA in ewing sarcoma cells. Mol. Cancer Ther. 2012;11:1247–1256. doi: 10.1158/1535-7163.MCT-11-0913. [DOI] [PubMed] [Google Scholar]
- 24.Gombos A., Metzger-Filho O., Dal Lago L., Awada-Hussein A. Clinical development of insulin-like growth factor receptor-1 (IGF-1R) inhibitors: At the crossroad? Investig. New Drugs. 2012;30:2433–2442. doi: 10.1007/s10637-012-9811-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hakam A., Yeatman T.J., Lu L., Mora L., Marcet G., Nicosia S.V., Karl R.C., Coppola D. Expression of insulin-like growth factor-1 receptor in human colorectal cancer. Hum. Pathol. 1999;30:1128–1133. doi: 10.1016/S0046-8177(99)90027-8. [DOI] [PubMed] [Google Scholar]
- 26.Hui L.J., Bakiri L., Stepniak E., Wagner E. p38α: A suppressor of cell proliferation and tumorigenesis. Cell Cycle. 2007;6:2429–2433. doi: 10.4161/cc.6.20.4774. [DOI] [PubMed] [Google Scholar]
- 27.Pal S., Li S., Priceman S.J., Xin H., Zhang W., Deng J., Liu Y., Huang J., Zhu W., Chen M., et al. Icaritin inhibits JAK/STAT3 signaling and growth of renal cell carcinoma. PLoS ONE. 2013;8:e81657. doi: 10.1371/journal.pone.0081657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S.Q., Huang J.A., Qin M.B., Su Y.J., Lai M.Y., Jiang H.X., Tang G.D. Sphingosine kinase 1 enhances colon cancer cell proliferation and invasion by upregulating the production of MMP-2/9 and uPA via MAPK pathways. Int. J. Colorectal Dis. 2012;27:1569–1578. doi: 10.1007/s00384-012-1510-y. [DOI] [PubMed] [Google Scholar]
- 29.Hui K., Yang Y., Shi K., Luo H., Duan J., An J., Wu P., Ci Y., Shi L., Xu C. The p38 MAPK-regulated PKD1/CREB/Bcl-2 pathway contributes to selenite-induced colorectal cancer cell apoptosis in vitro and in vivo. Cancer Lett. 2014;354:189–199. doi: 10.1016/j.canlet.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 30.Wang J., Chen X., Zeng J.H. Effect of curcumolon proliferation and apoptosis of nasopharyngeal carcinoma cellline CNE-2. Chin. J. Cell. Mol. Immunol. 2011;27:790–792. [PubMed] [Google Scholar]
- 31.Evan G.I., Vousden K. Proliferation, cell cycleand apoptosis in cancer. Nature. 2001;411:342–348. doi: 10.1038/35077213. [DOI] [PubMed] [Google Scholar]
- 32.Yin X., Zhang J., Li X., Liu D., Feng C., Liang R., Zhuang K., Cai C., Xue X., Jing F., et al. DADS suppresses human esophageal xenograft tumors through RAF/MEK/ERK and mitochondria-dependent pathways. Int. J. Mol. Sci. 2014;15:12422–12441. doi: 10.3390/ijms150712422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayeenuddin L.H., Yu Y., Kang Z., Helman L.J., Cao L. Insulin-like growth factor 1 receptor antibody induces rhabdomyosarcoma cell death via a process involving AKT and Bcl-xL. Oncogene. 2010;29:6367–6377. doi: 10.1038/onc.2010.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peiro G., Lohse P., Mayr D., Diebold J. Insulin-like growth factor-i receptor and PTEN protein expression in endometrial carcinoma: correlation with Bax and Bcl-2 expression, microsatellite instability status, and outcome. Am. J. Clin. Pathol. 2003;120:78–85. doi: 10.1309/C1KAH1PRL1UBW798. [DOI] [PubMed] [Google Scholar]
- 35.Michael Höpfner, Andreas P. Sutter, Alexander Huether, Viola Baradari, Scherübl H. Tyrosine kinase of insulin-like growth factor receptor as target for novel treatment and prevention strategies of colorectal cancer. World J. Gastroenterol. 2006;12:5635–5643. doi: 10.3748/wjg.v12.i35.5635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sophie G., Robert B., Alinel K.-C., Sophie T., Emmanuel V.O. The insulin and insulin-like growth factor-I receptor substrate IRS-1 associates with and activates phosphatidylinositol 3-kinase in vitro. J. Biol. Chem. 1993;268:7358–7364. [PubMed] [Google Scholar]
- 37.Koul H.K., Pal M., Koul S. Role of p38 MAP kinase signal transduction in solid tumors. Genes Cancer. 2013;4:342–359. doi: 10.1177/1947601913507951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Porras A., Zuluaga S., Black E., Valladares A., Alvarez A.M., Ambrosino C., Benito M., Nebreda A.R. p38α mitogen-activated protein kinase sensitizes cells to apoptosis induced by different stimuli. Mol. Biol. Cell. 2004;15:922–933. doi: 10.1091/mbc.E03-08-0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta J., del Barco Barrantes I., Igea A., Sakellariou S., Pateras I.S., Gorgoulis V.G., Nebreda A.R. Dual function of p38α MAPK in colon cancer: Suppression of colitis-associated tumor initiation but requirement for cancer cell survival. Cancer Cell. 2014;25:484–500. doi: 10.1016/j.ccr.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Y., Li H.Y., Zhang Z.H., Bian H.L., Lin G. Garlic-derived compound S-allylmercaptocysteine inhibits cell growth and induces apoptosis via the JNK and p38 pathways in human colorectal carcinoma cells. Oncol. Lett. 2014;8:2591–2596. doi: 10.3892/ol.2014.2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dolado I., Swat A., Ajenjo N., de Vita G., Cuadrado A., Nebreda A.R. p38α MAP kinase as a sensor of reactive oxygen species in tumorigenesis. Cancer Cell. 2007;11:191–205. doi: 10.1016/j.ccr.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 42.De Zutter G.S., Davis R.J. Pro-apoptotic gene expression mediated by the p38 mitogen-activated protein kinase signal transduction pathway. Proc. Natl. Acad. Sci. USA. 2001;98:6168–6173. doi: 10.1073/pnas.111027698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li X., Wang K., Ren Y., Zhang L., Tang X.J., Zhang H.M., Zhao C.Q., Liu P.J., Zhang J.M., He J.J. MAPK signaling mediates sinomenine hydrochloride-induced human breast cancer cell death via both reactive oxygen species-dependent and -independent pathways: An in vitro and in vivo study. Cell Death Dis. 2014;5 doi: 10.1038/cddis.2014.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matesic D.F., Sidorova T.S., Burns T.J., Bell A.M., Tran P.L., Ruch R.J., May S.W. p38 MAPK activation, JNK inhibition, neoplastic growth inhibition, and increased gap junction communication in human lung carcinoma and Ras-transformed cells by 4-phenyl-3-butenoic acid. J. Cell. Biochem. 2012;113:269–281. doi: 10.1002/jcb.23353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu J., Wu N., Ma L.N., Zhong J.T., Liu G., Zheng L.H., Lin X.K. p38 MAPK signaling mediates mitochondrial apoptosis in cancer cells induced by oleanolic acid. Asian Pac. J. Cancer Prev. 2014;15:4519–4525. doi: 10.7314/APJCP.2014.15.11.4519. [DOI] [PubMed] [Google Scholar]
- 46.Guo G.C., Yang W.C., Zhang Q.Q., Bo Y.L. Oleanolic acid suppresses migration and invasion of malignant glioma cells by inactivating MAPK/ERK signaling pathway. PLoS ONE. 2013;8:e72079. doi: 10.1371/journal.pone.0072079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hsu W.H., Hsieh Y.S., Kuo H.C., Teng C.Y., Huang H.I., Wang C.J., Yang S.F., Liou Y.S., Kuo W.H. Berberine induces apoptosis in SW620 human colonic carcinoma cells through generation of reactive oxygen species and activation of JNK/p38 MAPK and FasL. Arch. Toxicol. 2007;81:719–728. doi: 10.1007/s00204-006-0169-y. [DOI] [PubMed] [Google Scholar]
- 48.Chiacchiera F., Matrone A., Ferrari E., Ingravallo G., Lo Sasso G., Murzilli S., Petruzzelli M., Salvatore L., Moschetta A., Simone C. p38α blockade inhibits colorectal cancer growth in vivo by inducing a switch from HIF1α- to FoxO-dependent transcription. Cell Death Differ. 2009;16:1203–11214. doi: 10.1038/cdd.2009.36. [DOI] [PubMed] [Google Scholar]
- 49.Vanamala J., Reddivari L., Radhakrishnan S., Tarver C. Resveratrol suppresses IGF-1 induced human colon cancer cell proliferation and elevates apoptosis via suppression of IGF-1R/Wnt and activation of p53 signaling pathways. BMC Cancer. 2010;10 doi: 10.1186/1471-2407-10-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen X., Wang J., Jiang X.S., Zeng J.H., Huang F.X. Effects of curcumol on apoptosis induce factor, poly ADP-ribose polymerase and caspase-3 in lung cancer cell line A549. J. Exp. Tradit. Med. Formulae. 2011;19:157–159. [Google Scholar]