Abstract
African American women suffer higher incidence and mortality of triple negative breast cancer (TNBC) than Caucasian women. TNBC is very aggressive, causing the worst clinical outcome. We previously demonstrated that tumors from these patients express high IGF-II and exhibit high activation of the IGF signaling pathways. IGF-II gene expression is imprinted (monoallelic), promotes tumor progression, and metastasis and regulates Survivin, a TNBC prognostic marker. Since BC mortality has increased among young Vietnamese women, we analyzed 48 (paired) TNBC samples from Vietnamese patients to assess IGF-II expression. We analyzed all samples by qrtPCR for identification of IGF-II heterozygosity and to determine allelic expression of the IGF-II gene. We also analyzed the tissues for proIGF-II and Survivin by RT-PCR and Western blotting. A total of 28 samples displayed IGF-II heterozygosity of which 78% were biallelic. Tumors with biallelic IGF-II gene expression exhibited the highest levels of proIGF-II and Survivin. Although 100% of these tissues corresponding normal samples were biallelic, they expressed significantly lower levels of or no proIGF-II and Survivin. Thus, IGF-II biallelic gene expression is differentially regulated in normal versus tumor tissues. We propose that intratumoral proIGF-II is dependent on the IGF-II gene imprinting status and it will promote a more aggressive TNBC.
1. Introduction
IGF-II is expressed in breast cancer and “free” circulating IGF-II levels in humans are correlated to breast tumor size [1]. The expression of the IGF-II gene is tightly regulated and inhibited by tumor suppressor genes such as PTEN and p53 [2, 3]. IGF-II is positively regulated by estrogen, progesterone, prolactin, and growth hormones in normal breast development and in breast cancer progression [4–6]. Thus, IGF-II expression is important in normal breast development and increased IGF-II levels in the mammary gland contribute to tumor progression.
IGF-II was the first gene discovered to be imprinted and it is expressed exclusively from the paternal allele in humans [7]. Genomic imprinting is an important biological phenomenon defined by allelic-specific epigenetic modifications unique to the parent-of-origin specific gene expression [8]. IGF-II is also the first imprinted gene found to display loss of imprinting (LOI) or aberrant imprinting in human diseases [9]. In addition, LOI of the IGF-II gene is a frequent alteration in breast cancer [10]. The imprinting of the IGF-II gene is tissue specific [11] and it is predominantly monoallelic, except for certain regions in the brain where biallelic expression is normal [12].
Activation of the normally silent maternal allele of IGF-II is considered an early event in tumor development. Other genetic changes in the IGF-II gene such as Single Nucleotide Polymorphisms (SNPs) can influence the risk and/or severity of many diseases and may also be associated with increased risk of cancer. IGF-II ApaI (rs680) has been widely used to assess IGF-II loss of imprinting [13]. In our present study we use IGF-II rs680 SNP to determine loss of imprinting and, in addition, we will assess the effect of this SNP on proIGF-II protein expression.
TNBC patients are usually younger than 40 years old, have lower survival rates, and face worse clinical outcomes when treated with chemotherapy [14, 15]. This aggressive form of BC represents 15% of all invasive BC cases, yet it disproportionally affects AA women, who represent over one-third of this BC group. We have demonstrated that breast cancer tumors from AA patients express significantly higher levels of IGF-II when compared to tumors from Caucasian American women (CA) [16]. Our studies also showed that these tumors display high levels of activation of the IGF signaling pathways and antiapoptotic proteins such as Survivin which are associated with a more aggressive and chemoresistant form of the disease.
TNBC is increasing among younger Vietnamese women; however, it is not known which factors contribute to this condition. Understanding the growing evidence of the critical role of IGF-II in cancer, we thought to determine whether IGF-II gene regulation is present in TNBC among Vietnamese women. We used the IGF-II rs680 SNP to determine the IGF-II imprinting status in these tissues [17] and to determine if this genetic alteration is associated with TNBC in this ethnic group.
With hormone-based therapies, treatment pivots on whether a given hormone is recognized by its receptor [18]. Nevertheless, TNBC tumors do not express the traditional hormone receptors targeted for treatment: estrogen, progesterone, and Her2 receptors. The identification of alternate prognostic markers that can be targeted for therapy may result in new treatment of TNBC [19]. Thus, the present study also assessed how IGF-II imprinting regulates the expression of Survivin and related proteins associated with IGF-II signaling in the development and progression of breast cancer.
2. Materials and Methods
2.1. Patient Samples and Information
Frozen paired TNBC tissue samples (normal/malignant) were commercially obtained from ILSbio (Integrated Laboratory Services-Biotech, 100 Radcliffe Drive, Chestertown, MD 21620 USA) and stored at −80°C. ILSbio randomly obtained the samples from Vietnamese breast cancer patients residing in the USA. Each specimen comes with detailed clinical information and pathological reports. The diagnosis is confirmed by at least three pathologists. The pathology reports contain the basic information of patients and the verified characterization of normal and tumor tissues (Table 1). All ILSbio specimens are collected under Institutional Review Board (IRB) approved protocols, ensuring that strict ethical guidelines are followed to protect patient confidentiality and safety. Each sample has the patients consent for use in a wide range of research including the development of commercial products or services. The samples are identifiable only by barcodes to ensure an unbiased assessment as well as patient confidentiality.
Table 1.
| Sample type | IGF-II ApaI allelic usage | Pathological diagnosis | Surg stage | Grade |
|---|---|---|---|---|
| Tumor | 1M (Het) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 2N (Het) | Normal adjacent tissues | II A | 3 |
|
| ||||
| Tumor | 3M (Hom) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 4N (Hom) | Normal adjacent tissues | II A | 3 |
|
| ||||
| Tumor | 5M (Het) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 6N (Het) | Normal adjacent tissues | II A | 3 |
|
| ||||
| Tumor | 7M (Hom SNP) | Infiltrating ductal carcinoma | III A | |
| Normal | 8N (Hom SNP) | Normal adjacent tissues | III A | |
|
| ||||
| Tumor | 9M (Het) | Intraductal carcinoma with microinvasion | IV | 3 |
| Normal | 10N (Het) | Normal adjacent tissues | IV | 3 |
|
| ||||
| Tumor | 11M (Het) | Infiltrating ductal carcinoma | III A | 2 |
| Normal | 12N (Het) | Normal adjacent tissues | III A | 2 |
|
| ||||
| Tumor | 13M (Het) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 14N (Het) | Normal adjacent tissues | II A | |
|
| ||||
| Tumor | 15M (Het) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 16N (Het) | Normal adjacent tissues (adenosis) | III A | 3 |
|
| ||||
| Tumor | 17M (Het) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 18N (Het) | Normal adjacent tissues | II A | 3 |
|
| ||||
| Tumor | 19M (Hom) | Infiltrating ductal carcinoma | II A | 3 |
| Normal | 20N (Hom) | Normal adjacent tissues | II A | |
|
| ||||
| Tumor | 21M (Het) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 22N (Het) | Normal adjacent tissues | III A | 3 |
|
| ||||
| Tumor | 23M (Hom) | Infiltrating ductal carcinoma | IIB | 3 |
| Normal | 24N (Hom) | Normal adjacent tissues | IIB | 3 |
|
| ||||
| Tumor | 25M (Hom SNP) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 26N (Hom SNP) | Normal adjacent tissues | III A | 3 |
|
| ||||
| Tumor | 27M (Hom) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 28N (Hom) | Normal adjacent tissues | III A | 3 |
|
| ||||
| Tumor | 29M (Hom SNP) | Infiltrating ductal carcinoma | II | 3 |
| Normal | 30N (Hom SNP) | Normal adjacent tissues | II | 3 |
|
| ||||
| Tumor | 31M (Hom) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 32N (Hom) | Normal adjacent tissues | III A | 3 |
|
| ||||
| Tumor | 33M (Hom SNP) | Infiltrating ductal carcinoma | II | 3 |
| Normal | 34N (Hom SNP) | Normal adjacent tissues | II | 3 |
|
| ||||
| Tumor | 35M (Het) | Infiltrating ductal carcinoma | III | 3 |
| Normal | 36N (Het) | Normal adjacent tissues | III | 3 |
|
| ||||
| Tumor | 37M (Het) | Infiltrating ductal carcinoma | III B | 2 |
| Normal | 38N (Het) | Normal adjacent tissues | III B | 2 |
|
| ||||
| Tumor | 39M (Het) | Infiltrating ductal carcinoma | II | 3 |
| Normal | 40N (Het) | Normal adjacent tissues | II | 3 |
|
| ||||
| Tumor | 41M (Hom SNP) | Infiltrating ductal carcinoma | I | 3 |
| Normal | 42N (Hom SNP) | Normal adjacent tissues | I | 3 |
|
| ||||
| Tumor | 43M (Het) | Infiltrating ductal carcinoma | III A | 3 |
| Normal | 44N (Het) | Normal adjacent tissues | III A | 3 |
|
| ||||
| Tumor | 45M (Het) | Infiltrating ductal carcinoma | I | 3 |
| Normal | 46N (Het) | Normal adjacent tissues | I | 3 |
|
| ||||
| Tumor | 47M (Het) | Infiltrating ductal carcinoma | III | 3 |
| Normal | 48N (Het) | Normal adjacent tissues | III | 3 |
2.1.1. gDNA qrtPCR to Determine IGF-II Heterozygosity
High molecular weight DNA was extracted by conventional methods using the genomic DNA extraction from Invitrogen. DNA PCR reactions were performed on 100 ng of genomic DNA essentially using forward primer 5′CTTGGACTTTGAGTCAAATTGG-3′ and reverse primer 5′-GGTCGTGCCAATTACATTTCA-3′ which flank a transcribed ApaI polymorphism in Exon 9 of the IGF-II gene to differentiate the distinct IGF-II allelic profile. The resultant 292 bp DNA products were digested with ApaI and electrophoresed in a 3% agarose gel and stained with ethidium bromide. Digested samples yielding bands of 292, 227, and 65 bp were designated Heterozygous (Het), and samples yielding only the 292 bp size band are Homozygous (Hom) while samples yielding 227 and 65 bp are Homozygous with SNP (Hom SNP). IGF-II allelic sequences are checked for and confirmed by applied biosystems sequencing and analyzed by sequence scanners for the IGF-II Exon 9 region. The sequencing is performed by Eton Biosciences for identification of the IGF-II Exon 9.
2.1.2. nPCR to Determine IGF-II Allelic Expression
Total RNA was extracted using TRI Reagent (Molecular Research Center, Cincinnati, OH) in combination with Zymo RNA extraction and purification kit. RNA was purified according to the manufacturer's Direct-zol RNA MiniPrep protocol. To eliminate contaminating DNA, the samples were treated with DNAse prior to reverse transcription and subsequent RT-PCR amplification. One μg of RNA was amplified with high efficiency utilizing random primer to cDNA (Reverse Transcription System, Bio-RAD). A reverse transcription PCR (RT–PCR) was performed in 10 μL of first-strand cDNA with forward primer 5′-TCCTGGAGACGTACTGTGCTA-3′ and reverse primer 5′-GGTCGTGCCAATTACATTTCA-3′. The PCR cycling conditions were the same as described above for gDNA PCR and it yields a 1.12 kb IGF-II product confirmed by agarose gels. DNA-specific PCR product (1.4 kb) could be distinguished from the cDNA-specific product (1.12 kb). None of the RT-PCR preparations yielded a 1.4 kb genomic DNA band, indicating that there was no DNA contamination and that DNAse treatment was successful. To increase the 1.12 kb band we used nested PCR (nPCR) on the 1.12 kb PCR products using forward primer 5′CTTGGACTTTGAGTCAAATTGG-3′ and reverse primer 5′-GGTCGTGCCAATTACATTTCA-3′ to generate a shorter RT-PCR fragment of 292 bp harboring the ApaI polymorphic site as previously determined in the gDNA. The gDNA PCR product for all 48 samples was loaded onto 3% agarose gels and stained with ethidium bromide. The agarose gel bands were visualized under UV light to determine the IGF-II allelic pattern. ApaI restriction digestion enzyme analysis yielding bands of 292, 227, and 65 bp were designated biallelic samples (BA), those that yielded only the 292 bp were designated as monoallelic (MA), and samples yielding 227 and 65 bp are monoallelic with SNP (MAS).
2.1.3. RNA, cDNA, QPCR, and Conventional Gels
Total RNA was extracted using TRI Reagent (Molecular Research Center, Cincinnati, OH) according to the manufacturer's protocol. 50 mg of frozen tissue was cut and homogenized with the next advance motor drive using cool air circulating system. Samples were treated with Ambion DNAse to get rid of genomic DNA contamination. The total RNA stock was kept at −80°C until assayed. The cDNA was synthesized using iScript cDNA Synthesis Kit from Bio-Rad. The genes of interest (GOI) analyzed were IGF-I, IGF-II, Survivin, IGF-IR, IGF-IIR, IRA, IRB, ESR-α, ERBB2/Her2, PRLR, and VEGFR. The primers, forward (F) and reverse (R), for the above GOI were designed using intron spanning assay. 18s rRNA was used as housekeeping reference gene to calculate the fold mRNA change. The analysis was performed using the CFX 1000 QPCR machine. The results were analyzed using the CFX Manager version 1.0. Qbase and GraphPad Prism 5 software were used to quantitate the relative mRNA fold expression change for the above GOI.
2.2. Tissue Protein Extraction and Western Blot
Tissue cell lysates (50–75 mg) were prepared in RIPA buffer (1X TBS, 1% Nonidet P-40, 0.5% sodium deoxycholate, 0.1% SDS, 0.004% sodium azide, 10 μL/mL protease inhibitor cocktail, and 10 μL/mL sodium orthovanadate). A total of 90 μg was loaded into polyacrylamide-SDS gradient gels (4%–12%), transferred to a PVDF membrane (Invitrogen, Carlsbad, CA) using X-cell Sure-Lock electrophoretic transfer module (Invitrogen, Carlsbad, CA). Protein concentration was measured using the BCA Protein Assay Kit from Thermo Scientific (Rockford, IL). PVDF membranes were blocked in PBS/0.05% Tween and 3% milk for 1.5 hr at 4°C followed by 3x washes in PBS during 10 minutes each. Membranes were then incubated with IGF-II monoclonal antibody (Amano, 1 : 2500 dilution) in 3% BSA overnight. Membranes were washed three times for 10 min each in PBS 0.05% Tween. Following the washes, the membranes were incubated with the corresponding biotinylated anti-mouse antibody (IgG (H + L) vector BA-9200). Protein visualization was achieved by using enhanced chemiluminescence (ECL) and autoradiography with Hyperfilm ECL film (Amersham, Arlington Heights, IL). The signals on the X-ray films were quantified using ChemiImager 4000 (Alpha Innotech Corporation). Ponceau red was used to stain the Western blots and to normalize for loading control. Ponceau red stain was chosen among a limited number of alternatives recommended to normalize sample loading [20, 21].
2.3. Statistical Analysis
Statistical differences between mean values were determined by using one-way ANOVA and Wilcoxon Signed Rank Test comparing the paired normal/malignant samples in GraphPad Prism 5. Values are expressed as the mean ± SEM of two or more replicate experiments. A level of ∗ P < 0.05 was considered significant.
3. Results
3.1. IGF-II Allelic Status in TNBC Samples from Vietnamese Patients
A total of 48 informative random samples (24 paired normal/malignant breast tissue samples) of Vietnamese (VIET) TNBC patients are described in Table 1. These samples were analyzed to identify heterozygosity and to select the Heterozygous (Het) samples for further testing to identify the imprinting status of the IGF-II gene.
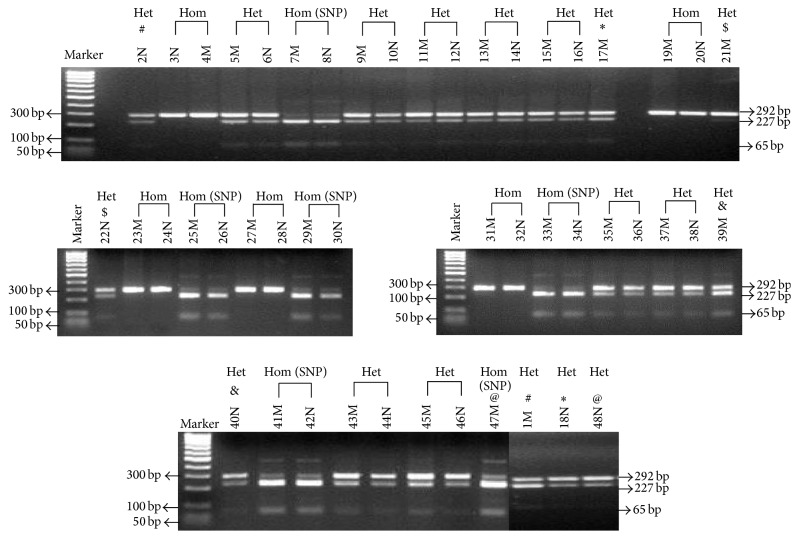
Figure 1 shows a composite of 5 representative 3% agarose gels of all 48 TNBC samples. Symbols #, ∗, $, &, and @ were used to identify paired samples that were not loaded next to each other. The Heterozygous profile for IGF-II was identified by the presence of two polymorphic bands of 292 bp (undigested) and 227 bp + 65 bp if the IGF-II rs680 SNP is present (digested). The Homozygous profile without SNP was identified by the 292 bp single band and Homozygous with SNP yielded two fragments 227 bp + 65 bp, respectively. Samples were further identified by N (normal tissue) and M (malignant tissue). Thus, the gDNA analysis of all 48 TNBC samples resulted in samples characterized as Heterozygous (n = 27), Homozygous (n = 10), and Homozygous with a SNP (n = 11). Thus, approximately 58% of the samples were Het, 21% were Hom, and another 21% were Hom SNP. Therefore, approximately 80% of all samples express the IGF-II rs680 SNP. The parental origin of the SNP was not considered in these experiments since the parental blood samples were not available for analysis.
Figure 1.
3% agarose gel showing ApaI restriction digestion of the 292 gDNA PCR products for the 48 breast normal (N) and malignant (M) samples. The IGF-II allelic pattern determined to be Heterozygous (Het; n = 27) displayed three bands of 292, 227, and 65 bp. The Homozygous with SNP (Hom SNP; n = 11) allelic pattern displayed two bands of 227 and 65 bp. Only one band (292 bp) is seen in the Homozygous without a SNP (Hom; n = 10) IGF-II allelic pattern. Symbols #, ∗, $, &, and @ represent paired samples from normal and malignant that were not next to each other's lane.
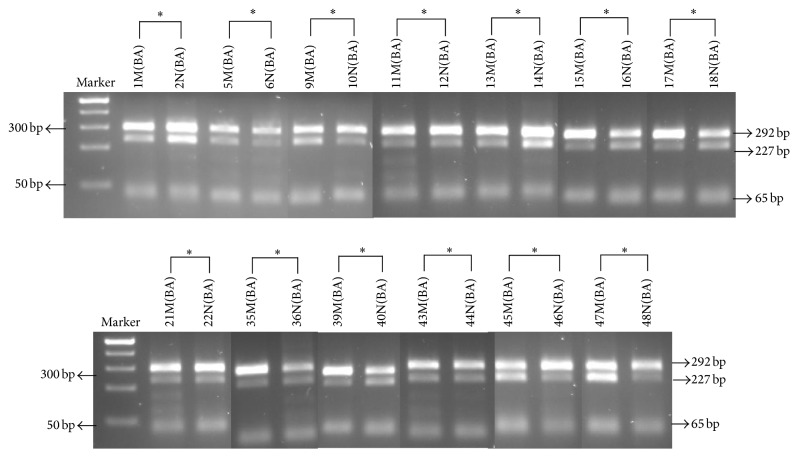
3.2. Biallelic Expression of IGF-II in VIET TNBC Patients
To analyze imprinting of the IGF-II gene, we selected the samples that were Heterozygous (Het) for the transcribed ApaI polymorphism. A total of 26 Het samples were analyzed to identify allelic expression of the IGF-II gene (Figure 2). Surprisingly, all 26 Het samples (13N + 13M) analyzed were biallelic (BA). Thus, 100% of the Het normal paired samples were BA.
Figure 2.
ApaI digestion of the 292 bp nested PCR (QPCR) fragment generated from the fragment of 1.12 RT-PCR reactions. Biallelic expression was identifiable by the presence of each of the 292, 227, and 63 bp restriction fragments. First lane shows Fisher's exACTGene 100 bp DNA Ladder, showing the 500 bp–25 bp respective molecular weight size markers.
3.3. IGF-II rs680 Single Nucleotide Polymorphism (SNP) Sequencing
The gDNA PCR products of the TNBC samples were sequenced to show the rs680 SNP with reference USCS genome browser Feb. 2009 (GRCh37/hg19) released version for IGF-II Exon 9. The sequenced samples show that the BA and the MAS tissues have the (C) cytosine and the MA samples have the (T) Thymidine in reference to the human genome web browser (http://genome.ucsc.edu/). This sequence verified the IGF-II allelic pattern and confirmed the gDNA ApaI restriction enzyme digestion pattern as shown in Figures 1 and 3. The samples were sequenced using the reverse primer 5′-GGTCGTGCCAATTACATTTCA-3′ to identify the allelic pattern for IGF-II at Exon 9 and aligned by EMBI Clustal W software.
Figure 3.
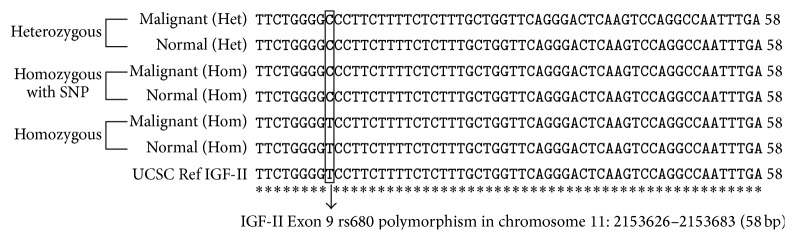
Representative standard sequencing alignment for IGF-II Exon 9 region chromosome 11: 2153626–2153683 (58 bp). The sequenced samples show that the Heterozygous (Het) and the Homozygous with SNP tissues have the (C) cytosine and the Homozygous samples have the (T) Thymidine in reference to the USCS genome Feb. 2009 (GRCh37/hg19) released version as reference gene.
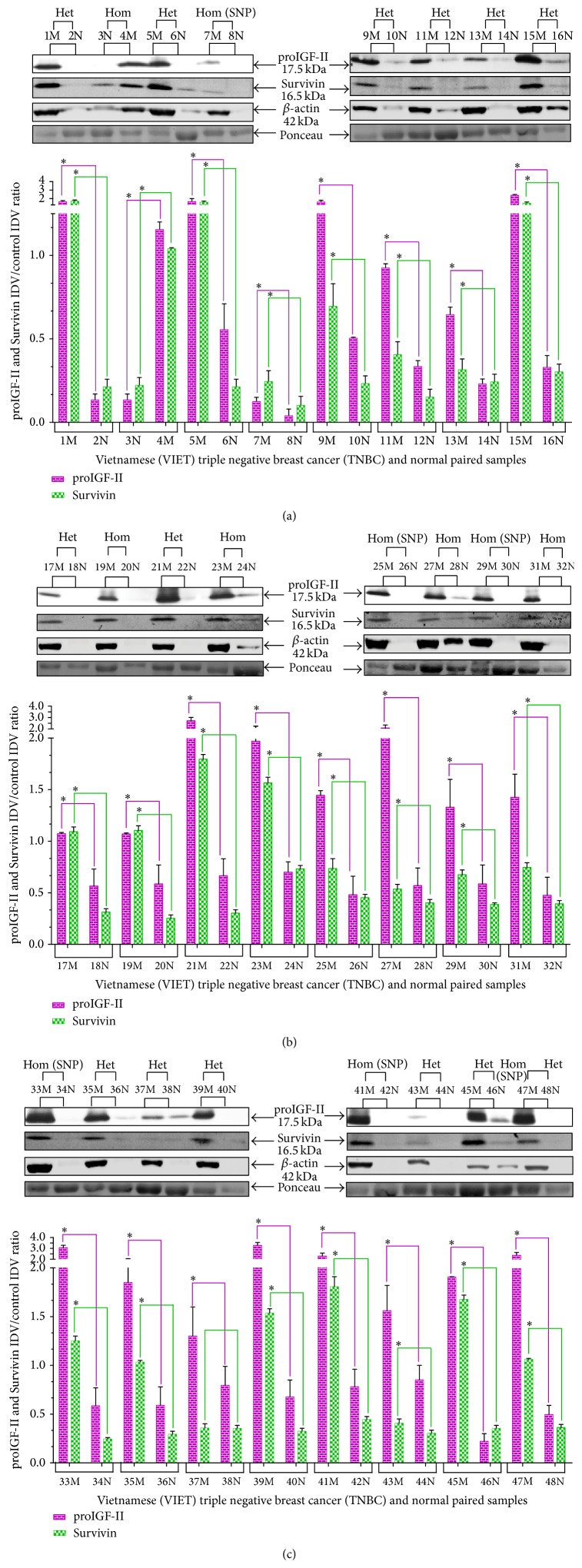
3.4. Expression of proIGF-II (17.5 kDa) and Survivin (16.5 kDa) Proteins
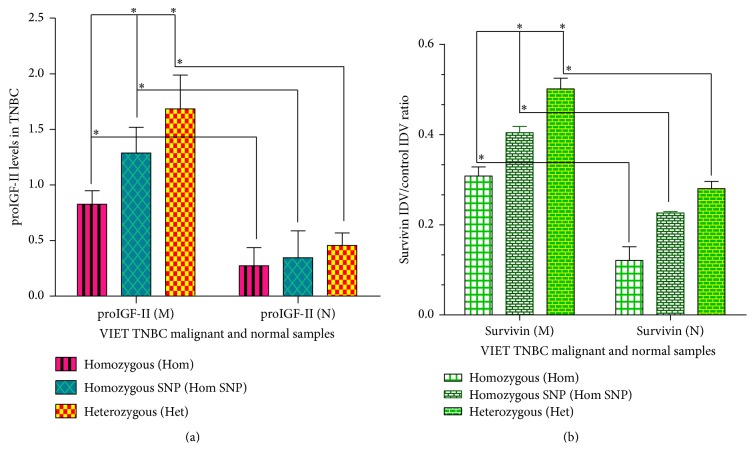
We analyzed the levels of proIGF-II and Survivin protein in all 24 paired informative cases of TNBC by Western blot. Bands were revealed using chemiluminescence followed by exposure to radiography film. Relative protein quantification was determined by using QuantityOne 1-D Analysis Software and data is expressed as IDV proIGF-II and Survivin units/control IDV protein units from Ponceau red stain as seen in the y-axis in Figures 4(a), 4(b), 4(c), 5(a), and 5(b).
Figure 4.
((a), (b), and (c)) Western blot of paired normal/malignant TNBC samples (1–48). Total number of samples (n) analyzed per group was as follows: Heterozygous (Het; n = 27), Homozygous with SNP (Hom SNP; n = 11), and Homozygous (Hom; n = 10). Bar graphs (a–c) of free proIGF-II (17.5 kDa) and Survivin (16.5 kDa). Ponceau red staining was used to normalize for sample loading. Bars represent the mean ± SE of all normalized samples per group. Asterisks indicate values statistically significant ∗(p < 0.05) using the Wilcoxon paired t-test.
Figure 5.
(a) Representative bar graph of proIGF-II (17.5 kDa) in paired malignant and normal TNBC samples in Hom, Hom SNP, and Het. Figure depicts the averages of three separate experiments and each was done in triplicate. Heterozygous (N = 14, M = 13), Homozygous with SNP (N = 5, M = 6), and Homozygous (N = 5, M = 5). Asterisks indicate values statistically significant ∗(p < 0.05) using the Wilcoxon paired t-test. (b) Representative bar graph of Survivin (16.5 kDa) in paired malignant and normal TNBC samples in Hom, Hom SNP, and Het. Figure depicts the averages of three separate experiments and each was done in triplicate. Heterozygous (N = 14, M = 13), Homozygous with SNP (N = 5, M = 6), and Homozygous (N = 5, M = 5). Asterisks indicate values statistically significant ∗(p < 0.05) using the Wilcoxon paired t-test.
The use of β-actin and many other standard control proteins used to normalize loading was attempted unsuccessfully. The housekeeping gene β-Actin (42 kDa) was initially probed to be used as a loading control but, as seen, normal tissues expressed very low β-Actin levels when compared to their respective malignant samples (Figures 4(a) and 5(b)). The Western blot figures show β-actin bands and demonstrate the limitation of its use as a loading control when analyzing normal and tumor tissues. Note that β-actin is almost undetectable in normal (N) breast tissue samples; in contrast, a strong 60 kDa band signal is seen in the same lanes stained with Ponceau red demonstrating the presence of protein. β-actin is essential in cell proliferation and it is a critical component of the cancer cell cytoskeleton [22]; thus it is an unreliable loading control to use in our study. Ponceau red stain was chosen among a limited number of alternatives recommended to normalize sample loading [20, 21].
Overall, as seen in Figures 5(a) and 5(b), the malignant tissue samples (M) expressed higher levels of proIGF-II and Survivin when compared to the normal breast (N) samples that express little or no proIGF-II and Survivin (P ∗ < 0.05). The levels of proIGF-II and Survivin were highest in the Heterozygous (BA) samples (Het; n = 14) ≫ compared to Homozygous with SNP samples (Hom SNP; n = 5) > which were higher than Homozygous tissue samples that have no SNP (Hom; n = 5). Tumors with BA IGF-II gene expression exhibited the highest levels of proIGF-II and Survivin. Although 100% of these tissues corresponding normal samples were BA, they expressed significantly lower levels or no proIGF-II and Survivin. Thus, IGF-II protein expression is differentially regulated in normal versus tumor tissues.
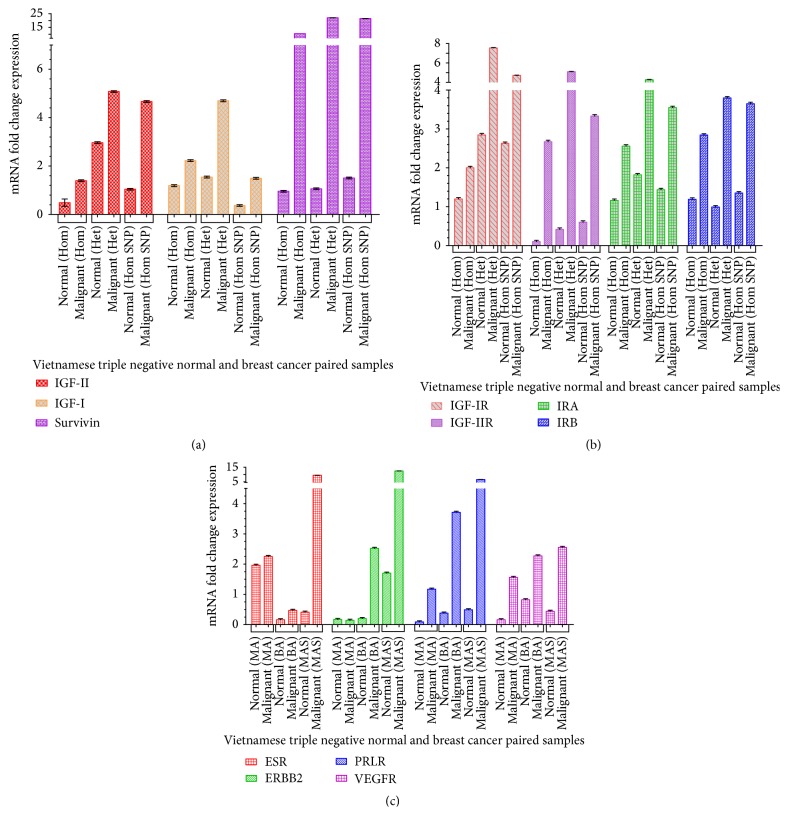
3.5. Quantitative RT-PCR Analysis of Selected Gene Expression in TNBC
Representative 9 paired samples were selected based on their mRNA quality and were analyzed by quantitative RT-PCR to assess the gene expression of IGF-II, IGF-I, Survivin (Figure 6(a)), IGF-IR, IGF-IIR, Insulin Receptor A (IRA), Insulin Receptor B (IRB) (Figure 6(b)), Estrogen Receptor-α (ESR-α), Human Epidermal Growth Factor Receptor 2 (ERBB2/Her2), Prolactin Receptor (PRLR), and the Vascular Endothelial Growth Factor Receptor (VEGFR) (Figure 6(c)). The 18S rRNA was used to normalize mRNA fold change expression (CFX Bio-Rad Manager, qbase software and GraphPad Prism 5). The data show that normal breast tissues (N) have lower levels of IGF-II, IGF-I, Survivin, and related receptors IGF-IIR, IRA, IRB, ESR-α, ERBB2, PRLR, and VEGFR when compared to the malignant breast tissues. The IGF-IIR, IRA, IRB, and VEGFR are higher in Het when compared to the Hom and Hom SNP.
Figure 6.
(a) Representative bar graph of IGF-II, IGF-I, and Survivin mRNA fold levels from 3 different patient samples ran in three separate qrtPCR assays done in triplicate. (b) Representative bar graph of Insulin-Like Growth Factor-I Receptor (IGF-1R), Insulin-Like Growth Factor-II Receptor (IGF-IIR), Insulin Receptor A (IRA) and Insulin Receptor B (IRB) mRNA fold levels from 3 different patient samples ran in three separate qrtPCR assays done in triplicate. (c) Representative bar graph of Estrogen Receptor-α (ESR-α), Human Epidermal Growth factor Receptor 2 (ERBB2/Her2), Prolactin Receptor (PRLR), and Vascular Endothelial Growth Factor Receptor (VEGFR) mRNA fold levels from 3 different patient samples ran in three separate qrtPCR assays done in triplicate.
4. Discussion
African American (AA) women have a lower incidence of BC but they have a higher occurrence of TNBC and increased mortality [23]. We demonstrated that BC tumors from AA patients have high levels of IGF-II and higher activation of the IGF signaling pathways [24]. Since young Vietnamese women are affected by TNBC [25], we designed the present study to determine the allelic regulation and expression of IGF-II in TNBC tumors from Vietnamese women. We examined the genomic imprinting status of IGF-II for specific allele expression to determine if disrupted imprinting, as evidenced by biallelic (BA) expression, is a mechanism of altered gene expression in breast cancer in this population [17, 26].
To our knowledge, this study is the first to identify free intratumoral IGF-II in TNBC paired samples and to demonstrate that BA expression of this growth factor gene results in significantly higher expression of IGF-II mRNA and free proIGF-II protein. The free proIGF-II protein levels were highest in the BA tumors followed by intermediate IGF-II levels in Homozygous (Hom) with SNP tumors and the lowest IGF-II levels were detected in the Hom without SNP tumors. Interestingly, IGF-II level in the BA normal tissues was undetectable or significantly lower than that in the BA paired tumor tissues, indicating that IGF-II expression is differentially regulated in the nontransformed tissues. Thus, loss of IGF-II imprinting precedes the malignant transformation and breast cancer development in the samples analyzed of young Vietnamese TNBC patients.
IGF-II bioavailability is a critical issue because most of the systemic IGF-II is associated with IGFBPs and those circulating levels cannot distinguish between secretion from liver, benign breast lesions, and breast cancer tumors. Therefore, rather than acting in an endocrine fashion, IGF-II produced in tumors is more likely working in a paracrine/autocrine mode. Thus, intratumoral IGF-II levels should be considered a better reflection of its potential actions in cancer growth and a more accurate estimate of IGF-II allelic dosage. Therefore, blood test for IGF-II may be inaccurate since it does not reflect true bioavailable IGF-II for tumor growth. IGF-II imprinting status will not only impact carcinogenesis but also impact critical functions regulated by this growth factor such as fetal development, cell cycle, apoptosis, and diabetes [27–29]. Interestingly, a recent review presents evidence of how loss of IGF-II imprinting can promote “cancer initiating cells” supporting the hypothesis of the epigenetic progenitor model of cancer [30].
Our previous studies of AA paired breast tumor/normal tissues demonstrated that higher levels of intratumoral IGF-II were correlated to Survivin, a critical antiapoptotic protein considered a marker of poor prognosis in TNBC [31–33]. Furthermore, in a breast cancer cell model, we showed that IGF-II stimulated Survivin and that IGF-II siRNA treatment completely abrogated the expression of this TNBC survival prognostic marker. In addition, those studies also showed that decreased IGF-II caused a significant reduction of Survivin resulting in increased sensitivity to resveratrol. Exogenous treatment with IGF-II restored the levels of Survivin in this cell model system and prevented cell apoptosis by inhibiting mitochondrial membrane depolarization [33]. The interaction between IGF-II and Survivin resulted in the protection of the mitochondria and the inhibition of apoptosis, key factors in promoting chemotherapy resistance. Resistance to currently available chemotherapy treatments is a major factor in the increased breast cancer mortality observed in TNBC patients [14, 15]. Thus, LOI of IGF-II will cause higher levels of free IGF-II promoting increased Survivin, among other proteins, and stimulating a more aggressive breast cancer progression and a breast tumor that is less responsive to chemotherapy.
It is well known that the expression of IGF-II is imprinted and regulated by methylation and, normally, only the paternal allele is transcribed [34–36]. Nevertheless, our results demonstrated that biallelic expression of IGF-II was present in 100% of the normal paired samples, thus demonstrating that “loss of imprinting” (LOI) is not the result of carcinogenesis in these samples. Since LOI resulted in higher intratumoral free IGF-II, we can expect, then, that LOI will contribute to an enhanced proliferative cell signaling milieu promoting a fast growing tumor, chemoresistance, and increased breast cancer death [17]. Other studies have also shown that IGF-II allelic dosage matters and that it is not an inconsequential genetic occurrence. Szabó and Mann showed that embryos were less likely to survive when both the paternal and the maternal IGF-II alleles were not expressed [37]. Likewise, if the silent maternal IGF-II allele is activated while the normally expressed paternal allele remains silent, abortion occurs as a result of the trophoblast cells failure to grow. Differentiation of trophoblastic cells is specifically regulated by IGF-II, not IGF-I [38]. LOI of IGF-II also occurs in 25% of Beckwith Wiedemann syndrome (BWS) as well as other tumors [9]. Since our study showed that higher levels of IGF-II are expressed in tumors carrying the rs680 SNP, it will be reasonable to assume that if carriers of this genetic variance develop cancer, they will be at a higher risk of developing a very aggressive disease. The IGF-II rs680 SNP have been associated with exercise induced muscle damage [39]. A higher consumption of dairy products is also associated with increased height depending on the rs680 IGF2 genotype [40]. No associations of the IGF-II SNP rs680 have been previously described with TNBC; thus, our study is the first one to identify this SNP which may impact the aggressiveness of this disease.
Our study also shows that increased level of IGF-II in BA and Hom SNP breast tissues correlates with higher expression of receptors important in breast cancer development and progression. Specifically, the mRNA for the receptors IRA, IRB, VEGFR, ER-α, PRLR, and ERBB2 expression correlate with the allelic dosage of IGF-II. This suggests the genomic imprinting of IGF-II; that is, IGF-II allelic dosage may play a critical role in tumorigenesis by triggering the progression of cells already harboring an oncogenic insult. IGF-II binds the IGF-IR and the Insulin Receptor A (IRA) to activate a series of mitogenic and antiapoptotic signaling pathways that includes AKT, MAPK, and NFKB [24, 41–43]. In addition, IGF-II binds the IGF-II receptor resulting in activation of the g protein signaling cascade and modulation of the lysosomal enzyme trafficking to regulate apoptosis, metastasis, proliferation, and motility [44–46]. Furthermore, IGF-II engages in cross talk signaling with other receptors such as the estrogen receptor [47, 48]. Indeed, our laboratory previously demonstrated that IGF-II binding to the IGF-IR and IRA promoted the phosphorylation of ER-α and ER-β independent of estrogen [49]. Of great significance, IGF-II is regulated by estrogen and progesterone and, in turn, IGF-II stimulates these steroid receptor's expression and activation [50]. These reciprocal interactions result in a positive stimulatory feedback that also amplifies the respective receptors signaling cascade [51].
High IGF-II levels are also an important factor in other endocrine conditions associated with a higher risk of breast cancer such as diabetes, metabolic syndrome, and obesity. Epidemiological studies looking at the development of type 2 diabetes and the metabolic syndrome, which are diseases highly prevalent among African American (AA) women, have shown that both diseases are strongly associated with increased breast cancer risk [52, 53]. Interestingly, we showed that significantly higher IGF-II levels and Insulin Receptor A were present in normal breast tissues of AA women leading us to propose that IGF-II was a common important link between breast cancer and diabetes in this ethnic group [41]. Overexpression of IGF-II leads to type 2 diabetes in a transgenic mouse model through a direct effect of IGF-II on β-cell proliferation [54]. These transgenic mice overexpressing IGF-II in β-cells were hyperinsulinemic early in life and showed altered glucose and insulin tolerance tests, as well as insulin resistance. Of great significance, the IGF-II E-peptide derived from the cleavage of proIGF-II regulates insulin secretion in the pancreas [55]. IGF-II is also an important factor in obesity [56]. In contrast to our observations among AA, the IGF-II levels in the normal breast tissues of Vietnamese women in the present study were low or undetectable. Likewise, there is no IGF-II relationship with diabetes and breast cancer among Vietnamese women.
LOI of IGF-II in 100% of the normal breast tissues paired to BA tumors in this study was unexpected as well as surprising. In addition to the effect of IGF-II allelic dosage, our study also showed that the presence of the rs680 IGF-II SNP occurred in approximately 80% of the Vietnamese breast tissue samples. We acknowledge that our Vietnamese paired breast sample number is small (n = 48); however, we have compared the allele count for the rs680 SNP in our paired breast samples from other ethnic groups (African American n = 36, Caucasian n = 32, and South Korean n = 42) to the 1000-Human Genome Ensembl for the same populations (http://uswest.ensembl.org) and the published percentage allele count is almost identical to ours (Supplementary Figures 1-2 in Supplementary Material available online at http://dx.doi.org/10.1155/2015/401851). Thus, the allele count of the IGF-II rs680 in our small sample size is comparable to the allele count in the reference populations where the samples range from 181 to 379 (Supplementary Figure 2).
5. Conclusions
Thus, we have demonstrated that LOI and the occurrence of the rs680 IGF-II SNP result in higher levels of intratumoral free IGF-II in breast cancer tumors of young Vietnamese women affected with TNBC. Given the pleiotropic effects of IGF-II and its multiple interactions with so many receptors, we propose that IGF-II be considered a potential molecular marker in the differential diagnosis and treatment of TNBC patients. Moreover, understanding how IGF-II promotes the development of a hormone-independent tumor and its progression into TNBC will be critical for designing novel and more effective targeted therapies badly needed to reduce the breast cancer survival disparity of this disease.
Supplementary Material
Since our breast cancer samples from Vietnamese patients is limited (n=48), we provided Supplementary Figure 1 which represents the results of the IGF-II rs680 C/T allele count from the 1000 Human Genome Ensemble () from different ethnic groups.
Supplementary Figure 2 represents unpublished data from our own IGF-II rs680 C/T allele count from paired breast cancer samples from Caucasian American (n=32), South Korean (n=42) and African American (n=36).
Please note that when we compared the allele count for the rs680 SNP in our paired breast sample analysis from Caucasian American, South Korean and African American (Supplementary figure 2) to the 1000 Human Genome Ensemble for the same populations () it shows that the published percentage allele count is almost identical to ours (Supplementary Figure 1). Thus, the allele count of the IGF-II rs680 in our sample size is comparable to the allele count in the reference populations where the samples range from 181-379. This is important, because it strengthen the significance of our results even though our sample size is limited.
Acknowledgment
This research was supported by Grants National Institutes of Health P20MD001632 and National Institutes of Health P20MD006988.
Abbreviations
- AA:
African American
- CA:
Caucasian American
- VIET:
Vietnamese
- TNBC:
Triple negative breast cancer
- BC:
Breast cancer
- Hom:
Homozygous
- Het:
Heterozygous
- Hom SNP:
Homozygous with SNP
- BA:
Biallelic
- MA:
Monoallelic with no SNP
- MAS:
Monoallelic with SNP
- IGF-I:
Insulin-Like Growth Factor-I
- IGF-II:
Insulin-Like Growth Factor-II
- ESR-α:
Estrogen Receptor-α
- ERBB2:
Human Epidermal Growth Factor Receptor 2 (Her2)
- VEGFR:
Vascular Endothelial Growth Factor Receptors
- PRLR:
Prolactin Receptors
- IRA:
Insulin Receptor A Isoform
- IRB:
Insulin Receptor B Isoform
- SNP:
Single Nucleotide Polymorphism
- HSK:
Housekeeping gene.
Conflict of Interests
The authors declare no conflict of interests.
References
- 1.Singer C. F., Mogg M., Koestler W., et al. Insulin-like growth factor (IGF)-I and IGF-II serum concentrations in patients with benign and malignant breast lesions: free IGF-II is correlated with breast cancer size. Clinical Cancer Research. 2004;10(12):4003–4009. doi: 10.1158/1078-0432.ccr-03-0093. [DOI] [PubMed] [Google Scholar]
- 2.Perks C. M., Vernon E. G., Rosendahl A. H., Tonge D., Holly J. M. P. IGF-II and IGFBP-2 differentially regulate PTEN in human breast cancer cells. Oncogene. 2007;26(40):5966–5972. doi: 10.1038/sj.onc.1210397. [DOI] [PubMed] [Google Scholar]
- 3.Zhang L., Zhan Q., Zhan S., et al. p53 regulates human insulin-like growth factor II gene expression through active P4 promoter in rhabdomyosarcoma cells. DNA and Cell Biology. 1998;17(2):125–131. doi: 10.1089/dna.1998.17.125. [DOI] [PubMed] [Google Scholar]
- 4.Brisken C., Ayyannan A., Nguyen C., et al. IGF-2 is a mediator of prolactin-induced morphogenesis in the breast. Developmental Cell. 2002;3(6):877–887. doi: 10.1016/S1534-5807(02)00365-9. [DOI] [PubMed] [Google Scholar]
- 5.Goldfine I. D., Papa V., Vigneri R., Siiteri P., Rosenthal S. Progestin regulation of insulin and insulin-like growth factor I receptors in cultured human breast cancer cells. Breast Cancer Research and Treatment. 1992;22(1):69–79. doi: 10.1007/BF01833335. [DOI] [PubMed] [Google Scholar]
- 6.Hamelers I. H. L., Steenbergh P. H. Interactions between estrogen and insulin-like growth factor signaling pathways in human breast tumor cells. Endocrine-Related Cancer. 2003;10(2):331–345. doi: 10.1677/erc.0.0100331. [DOI] [PubMed] [Google Scholar]
- 7.Steenman M. J. C., Rainier S., Dobry C. J., Grundy P., Horon I. L., Feinberg A. P. Loss of imprinting of IGF2 is linked to reduced expression and abnormal methylation of H19 in Wilms' tumour. Nature Genetics. 1994;7(3):433–439. doi: 10.1038/ng0794-433. [DOI] [PubMed] [Google Scholar]
- 8.Henckel A., Arnaud P. Genome-wide identification of new imprinted genes. Briefings in Functional Genomics and Proteomics. 2010;9(4):304–314. doi: 10.1093/bfgp/elq016. [DOI] [PubMed] [Google Scholar]
- 9.Feinberg A. P. Imprinting of a genomic domain of 11p15 and loss of imprinting in cancer: an introduction. Cancer Research. 1999;59(7, supplement):1743s–1746s. [PubMed] [Google Scholar]
- 10.Van Roozendaal C. E. P., Gillis A. J. M., Klijn J. G. M., et al. Loss of imprinting of IGF2 and not H19 in breast cancer, adjacent normal tissue and derived fibroblast cultures. FEBS Letters. 1998;437(1-2):107–111. doi: 10.1016/S0014-5793(98)01211-3. [DOI] [PubMed] [Google Scholar]
- 11.Ravenel J. D., Broman K. W., Perlman E. J., et al. Loss of imprinting of insulin-like growth factor-II (IGF2) gene in distinguishing specific biologic subtypes of Wilms tumor. Journal of the National Cancer Institute. 2001;93(22):1698–1703. doi: 10.1093/jnci/93.22.1698. [DOI] [PubMed] [Google Scholar]
- 12.Hu J.-F., Vu T. H., Hoffman A. R. Differential biallelic activation of three insulin-like growth factor II promoters in the mouse central nervous system. Molecular Endocrinology. 1995;9(5):628–636. doi: 10.1210/mend.9.5.7565809. [DOI] [PubMed] [Google Scholar]
- 13.Ogawa O., Eccles M. R., Szeto J., et al. Relaxation of insulin-like growth factor II gene imprinting implicated in Wilms' tumour. Nature. 1993;362(6422):749–751. doi: 10.1038/362749a0. [DOI] [PubMed] [Google Scholar]
- 14.Bauer K. R., Brown M., Cress R. D., Parise C. A., Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype. Cancer. 2007;109(9):1721–1728. doi: 10.1002/cncr.22618. [DOI] [PubMed] [Google Scholar]
- 15.Gucalp A., Traina T. A. Triple-negative breast cancer: adjuvant therapeutic options. Chemotherapy Research and Practice. 2011;2011:13. doi: 10.1155/2011/696208.696208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalla Singh S., Tan Q. W., Brito C., De León M., Garberoglio C., De León D. Differential insulin-like growth factor II (IGF-II) expression: a potential role for breast cancer survival disparity. Growth Hormone & IGF Research. 2010;20(2):162–170. doi: 10.1016/j.ghir.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCann A. H., Miller N., O'Meara A., et al. Biallelic expression of the IGF2 gene in human breast disease. Human Molecular Genetics. 1996;5(8):1123–1127. doi: 10.1093/hmg/5.8.1123. [DOI] [PubMed] [Google Scholar]
- 18.Chlebowski R. T. Changing concepts of hormone receptor-positive advanced breast cancer therapy. Clinical Breast Cancer. 2013;13(3):159–166. doi: 10.1016/j.clbc.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Cleator S., Heller W., Coombes R. C. Triple-negative breast cancer: therapeutic options. The Lancet Oncology. 2007;8(3):235–244. doi: 10.1016/s1470-2045(07)70074-8. [DOI] [PubMed] [Google Scholar]
- 20.Dittmer A., Dittmer J. β-Actin is not a reliable loading control in Western blot analysis. Electrophoresis. 2006;27(14):2844–2845. doi: 10.1002/elps.200500785. [DOI] [PubMed] [Google Scholar]
- 21.Romero-Calvo I., Ocón B., Martínez-Moya P., et al. Reversible Ponceau staining as a loading control alternative to actin in Western blots. Analytical Biochemistry. 2010;401(2):318–320. doi: 10.1016/j.ab.2010.02.036. [DOI] [PubMed] [Google Scholar]
- 22.Bunnell T. M., Burbach B. J., Shimizu Y., Ervasti J. M. β-actin specifically controls cell growth, migration, and the G-actin pool. Molecular Biology of the Cell. 2011;22(21):4047–4058. doi: 10.1091/mbc.e11-06-0582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amirikia K. C., Mills P., Bush J., Newman L. A. Higher population-based incidence rates of triple-negative breast cancer among young African-American women. Cancer. 2011;117(12):2747–2753. doi: 10.1002/cncr.25862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalla Singh S., Tan Q. W., Brito C., De León M., De León D. Insulin-like growth factors I and II receptors in the breast cancer survival disparity among African-American women. Growth Hormone & IGF Research. 2010;20(3):245–254. doi: 10.1016/j.ghir.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams D. J., Cohen C., To T. V., et al. Triple-negative breast carcinoma in women from Vietnam and the United States: characterization of differential marker expression by tissue microarray. Human Pathology. 2009;40(8):1176–1181. doi: 10.1016/j.humpath.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Yang R., Wang Y., Zhu X., Gao X. Study on genomic imprinting of IGF2 in breast cancer. Journal of Hygiene Research. 2009;38(4):423–425. [PubMed] [Google Scholar]
- 27.Evan G. I., Vousden K. H. Proliferation, cell cycle and apoptosis in cancer. Nature. 2001;411(6835):342–348. doi: 10.1038/35077213. [DOI] [PubMed] [Google Scholar]
- 28.Constância M., Hemberger M., Hughes J., et al. Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature. 2002;417(6892):945–948. doi: 10.1038/nature00819. [DOI] [PubMed] [Google Scholar]
- 29.Dupont J., Pierre A., Froment P., Moreau C. The insulin-like growth factor axis in cell cycle progression. Hormone and Metabolic Research. 2003;35(11-12):740–750. doi: 10.1055/s-2004-814162. [DOI] [PubMed] [Google Scholar]
- 30.Leick M. B., Shoff C. J., Wang E. C., Congress J. L., Gallicano G. I. Loss of imprinting of IGF2 and the epigenetic progenitor model of cancer. American Journal of Stem Cells. 2012;1(1):59–74. [PMC free article] [PubMed] [Google Scholar]
- 31.Jha K., Shukla M., Pandey M. Survivin expression and targeting in breast cancer. Surgical Oncology. 2012;21(2):125–131. doi: 10.1016/j.suronc.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Dogu G. G., Ozkan M., Ozturk F., Dikilitas M., Er O., Ozturk A. Triple-negative breast cancer: immunohistochemical correlation with basaloid markers and prognostic value of survivin. Medical Oncology. 2010;27(1):34–39. doi: 10.1007/s12032-009-9166-3. [DOI] [PubMed] [Google Scholar]
- 33.Kalla Singh S., Moretta D., Almaguel F., Wall N. R., De León M., De León D. Differential effect of proIGF-II and IGF-II on resveratrol induced cell death by regulating survivin cellular localization and mitochondrial depolarization in breast cancer cells. Growth Factors. 2007;25(6):363–372. doi: 10.1080/08977190801886905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee D.-H., Tran D. A., Singh P., et al. MIRA-SNuPE, a quantitative, multiplex method for measuring allele-specific DNA methylation. Epigenetics. 2011;6(2):212–223. doi: 10.4161/epi.6.2.13699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Monk D., Sanches R., Arnaud P., et al. Imprinting of IGF2 P0 transcript and novel alternatively spliced INS-IGF2 isoforms show differences between mouse and human. Human Molecular Genetics. 2006;15(8):1259–1269. doi: 10.1093/hmg/ddl041. [DOI] [PubMed] [Google Scholar]
- 36.Shetty P. J., Movva S., Pasupuleti N., et al. Regulation of IGF2 transcript and protein expression by altered methylation in breast cancer. Journal of Cancer Research and Clinical Oncology. 2011;137(2):339–345. doi: 10.1007/s00432-010-0890-z. [DOI] [PubMed] [Google Scholar]
- 37.Szabó P., Mann J. R. Expression and methylation of imprinted genes during in vitro differentiation of mouse parthenogenetic and androgenetic embryonic stem cell lines. Development. 1994;120(6):1651–1660. doi: 10.1242/dev.120.6.1651. [DOI] [PubMed] [Google Scholar]
- 38.Kanai-Azuma M., Kanai Y., Kurohmaru M., Sakai S., Hayashi Y. Insulin-like growth factor (IGF)-I stimulates proliferation and migration of mouse ectoplacental cone cells, while IGF-II transforms them into trophoblastic giant cells in vitro. Biology of Reproduction. 1993;48(2):252–261. doi: 10.1095/biolreprod48.2.252. [DOI] [PubMed] [Google Scholar]
- 39.Devaney J. M., Hoffman E. P., Gordish-Dressman H., Kearns A., Zambraski E., Clarkson P. M. IGF-II gene region polymorphisms related to exertional muscle damage. Journal of Applied Physiology. 2007;102(5):1815–1823. doi: 10.1152/japplphysiol.01165.2006. [DOI] [PubMed] [Google Scholar]
- 40.Dedoussis G. V., Louizou E., Papoutsakis C., Skenderi K. P., Yannakoulia M. Dairy intake associates with the IGF rs680 polymorphism to height variation in periadolescent children. European Journal of Clinical Nutrition. 2010;64(3):253–258. doi: 10.1038/ejcn.2009.124. [DOI] [PubMed] [Google Scholar]
- 41.Kalla Singh S., Brito C., Tan Q. W., De León M., De León D. Differential expression and signaling activation of insulin receptor isoforms A and B: a link between breast cancer and diabetes. Growth Factors. 2011;29(6):278–289. doi: 10.3109/08977194.2011.616200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Frasca F., Pandini G., Vigneri R., Goldfine I. D. Insulin and hybrid insulin/IGF receptors are major regulators of breast cancer cells. Breast Disease. 2003;17(1):73–89. doi: 10.3233/bd-2003-17108. [DOI] [PubMed] [Google Scholar]
- 43.Belfiore A., Frasca F. IGF and insulin receptor signaling in breast cancer. Journal of Mammary Gland Biology and Neoplasia. 2008;13(4):381–406. doi: 10.1007/s10911-008-9099-z. [DOI] [PubMed] [Google Scholar]
- 44.Okamoto T., Katada T., Murayama Y., Ui M., Ogata E., Nishimoto I. A simple structure encodes G protein-activating function of the IGF-II/mannose 6-phosphate receptor. Cell. 1990;62(4):709–717. doi: 10.1016/0092-8674(90)90116-V. [DOI] [PubMed] [Google Scholar]
- 45.Kang J. X., Li Y., Leaf A. Mannose-6-phosphate/insulin-like growth factor-II receptor is a receptor for retinoic acid. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(25):13671–13676. doi: 10.1073/pnas.94.25.13671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen Z., Ge Y., Kang J. X. Down-regulation of the M6P/IGF-II receptor increases cell proliferation and reduces apoptosis in neonatal rat cardiac myocytes. BMC Cell Biology. 2004;5(1, article 15) doi: 10.1186/1471-2121-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Osborne C. K., Schiff R. Growth factor receptor cross-talk with estrogen receptor as a mechanism for tamoxifen resistance in breast cancer. The Breast. 2003;12(6):362–367. doi: 10.1016/s0960-9776(03)00137-1. [DOI] [PubMed] [Google Scholar]
- 48.Surmacz E., Bartucci M. Role of estrogen receptor alpha in modulating IGF-I receptor signaling and function in breast cancer. Journal of Experimental and Clinical Cancer Research. 2004;23(3):385–394. [PubMed] [Google Scholar]
- 49.Richardson A. E., Hamilton N., Davis W., Brito C., De León D. Insulin-like growth factor-2 (IGF-2) activates estrogen receptor-α and-β via the IGF-1 and the insulin receptors in breast cancer cells. Growth Factors. 2011;29(2-3):82–93. doi: 10.3109/08977194.2011.565003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oehler M. K., Rees M. C. P., Bicknell R. Steroids and the endometrium. Current Medicinal Chemistry. 2000;7(5):543–560. doi: 10.2174/0929867003374958. [DOI] [PubMed] [Google Scholar]
- 51.Sachdev D., Yee D. The IGF system and breast cancer. Endocrine-Related Cancer. 2001;8(3):197–209. doi: 10.1677/erc.0.0080197. [DOI] [PubMed] [Google Scholar]
- 52.Rose D. P., Haffner S. M., Baillargeon J. Adiposity, the metabolic syndrome, and breast cancer in African-American and white American women. Endocrine Reviews. 2007;28(7):763–777. doi: 10.1210/er.2006-0019. [DOI] [PubMed] [Google Scholar]
- 53.Wolf I., Sadetzki S., Catane R., Karasik A., Kaufman B. Diabetes mellitus and breast cancer. The Lancet Oncology. 2005;6(2):103–111. doi: 10.1016/s1470-2045(05)01736-5. [DOI] [PubMed] [Google Scholar]
- 54.Devedjian J.-C., George M., Casellas A., et al. Transgenic mice overexpressing insulin-like growth factor-II in β cells develop type 2 diabetes. The Journal of Clinical Investigation. 2000;105(6):731–740. doi: 10.1172/jci5656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Buchanan C. M., Phillips A. R. J., Cooper G. J. S. Preptin derived from proinsulin-like growth factor II (proIGF-II) is secreted from pancreatic islet β-cells and enhances insulin secretion. Biochemical Journal. 2001;360(2):431–439. doi: 10.1042/0264-6021:3600431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sandhu M. S., Gibson J. M., Heald A. H., Dunger D. B., Wareham N. J. Low circulating IGF-II concentrations predict weight gain and obesity in humans. Diabetes. 2003;52(6):1403–1408. doi: 10.2337/diabetes.52.6.1403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Since our breast cancer samples from Vietnamese patients is limited (n=48), we provided Supplementary Figure 1 which represents the results of the IGF-II rs680 C/T allele count from the 1000 Human Genome Ensemble () from different ethnic groups.
Supplementary Figure 2 represents unpublished data from our own IGF-II rs680 C/T allele count from paired breast cancer samples from Caucasian American (n=32), South Korean (n=42) and African American (n=36).
Please note that when we compared the allele count for the rs680 SNP in our paired breast sample analysis from Caucasian American, South Korean and African American (Supplementary figure 2) to the 1000 Human Genome Ensemble for the same populations () it shows that the published percentage allele count is almost identical to ours (Supplementary Figure 1). Thus, the allele count of the IGF-II rs680 in our sample size is comparable to the allele count in the reference populations where the samples range from 181-379. This is important, because it strengthen the significance of our results even though our sample size is limited.