Abstract
Objective
To conduct a systematic review of emergency care in low- and middle-income countries (LMICs).
Methods
We searched PubMed, CINAHL and World Health Organization (WHO) databases for reports describing facility-based emergency care and obtained unpublished data from a network of clinicians and researchers. We screened articles for inclusion based on their titles and abstracts in English or French. We extracted data on patient outcomes and demographics as well as facility and provider characteristics. Analyses were restricted to reports published from 1990 onwards.
Findings
We identified 195 reports concerning 192 facilities in 59 countries. Most were academically-affiliated hospitals in urban areas. The median mortality within emergency departments was 1.8% (interquartile range, IQR: 0.2–5.1%). Mortality was relatively high in paediatric facilities (median: 4.8%; IQR: 2.3–8.4%) and in sub-Saharan Africa (median: 3.4%; IQR: 0.5–6.3%). The median number of patients was 30 000 per year (IQR: 10 296–60 000), most of whom were young (median age: 35 years; IQR: 6.9–41.0) and male (median: 55.7%; IQR: 50.0–59.2%). Most facilities were staffed either by physicians-in-training or by physicians whose level of training was unspecified. Very few of these providers had specialist training in emergency care.
Conclusion
Available data on emergency care in LMICs indicate high patient loads and mortality, particularly in sub-Saharan Africa, where a substantial proportion of all deaths may occur in emergency departments. The combination of high volume and the urgency of treatment make emergency care an important area of focus for interventions aimed at reducing mortality in these settings.
Résumé
Objectif
Réaliser un examen systématique des soins d'urgence dans les pays à revenu faible ou intermédiaire (PRFI).
Méthodes
Nous avons recherché dans les bases de données de PubMed, CINAHL et de l'Organisation mondiale de la Santé des rapports décrivant les soins d'urgence dispensés dans les établissements médicaux et obtenu des données non publiées auprès d'un réseau de cliniciens et de chercheurs. Nous avons sélectionné plusieurs articles à inclure d'après leur titre et leur résumé en anglais ou en français. Nous avons extrait des données liées à l'état de santé des patients, à la démographie et aux caractéristiques des établissements et des prestataires. Les analyses se sont limitées à des rapports publiés à partir de 1990.
Résultats
Nous avons identifié 195 rapports relatifs à 192 établissements implantés dans 59 pays. Il s'agissait pour la plupart d'hôpitaux universitaires situés dans des zones urbaines. La mortalité moyenne au sein des services d'urgence était de 1,8% (intervalle interquartile, IQR: 0,2–5,1%). Elle était relativement élevée dans les centres pédiatriques (moyenne: 4,8%; IQR: 2,3–8,4%) et en Afrique subsaharienne (moyenne: 3,4%; IQR: 0,5–6,3%). Le nombre moyen de patients était de 30 000 par an (IQR: 10 296–60 000), la plupart d'entre eux étant des jeunes (âge médian: 35 ans; IQR: 6,9–41,0) et de sexe masculin (moyenne: 55,7%; IQR: 50,0–59,2%). La majorité des établissements employaient des médecins en formation ou dont le niveau de formation n'était pas précisé. Rares étaient les prestataires à avoir reçu une formation spécialisée en soins d'urgence.
Conclusion
Les données existantes concernant les soins d'urgence dispensés dans les PRFI indiquent un nombre de patients et une mortalité élevés, en particulier en Afrique subsaharienne où une fraction importante de l'ensemble des décès est susceptible de survenir dans les services d'urgence. Compte tenu du nombre élevé et de l'urgence des interventions, les soins d'urgence constituent un domaine d'intérêt important pour les actions visant à réduire la mortalité dans ces lieux.
Resumen
Objetivo
Realizar una revisión sistemática de la atención de emergencia en países de ingresos medios y bajos (PIMB).
Métodos
Se realizaron búsquedas en las bases de datos de PubMed, CINAHL y la Organización Mundial de la Salud (OMS) para encontrar informes que describieran la atención de emergencia en centros sanitarios y se obtuvieron datos sin publicar de una red de clínicos e investigadores. Se seleccionaron artículos para ser incluidos en base a los títulos y resúmenes en inglés o francés. Se recogieron datos de los resultados y demografías de los pacientes, así como características de las instalaciones y los proveedores. Los análisis se redujeron a informes publicados a partir de 1990.
Resultados
Se identificaron 195 informes referentes a 192 instalaciones en 59 países. La mayoría eran hospitales académicamente afiliados en zonas urbanas. La mortalidad media en los servicios de urgencias era de 1,8% (rango intercuartílico, RIC: 0,2–5,1%). La mortalidad era relativamente alta en los centros pediátricos (mediana: 4,8%; RIC: 2,3–8,4%) y en el África subsahariana (mediana: 3,4%; RIC: 0,5–6,3%). La mediana de pacientes era de 30.000 al año (RIC: 10.296–60.000), la mayoría de los cuales eran jóvenes (mediana de edad: 35 años; RIC: 6,9–41,0) y hombres (mediana: 55,7%; RIC: 50,0–59,2%). El personal de la mayoría de los centros eran médicos en formación o médicos cuyo nivel de formación era indeterminado. Muy pocos de estos proveedores tenían una formación especializada en atención de emergencia.
Conclusión
Los datos disponibles en atención de emergencia en PIMB indican una gran carga de pacientes y mortalidad, en especial en el África subsahariana, donde una proporción sustancial de todas las muertes pueden ocurrir en los servicios de urgencias. La combinación entre una gran carga y la urgencia del tratamiento hacen de la atención de emergencia un área importante en la que centrarse de cara a intervenciones dirigidas a reducir la mortalidad en estos escenarios.
ملخص
الغرض
إجراء مراجعة منهجية للرعاية المقدمة في حالات الطوارئ في البلدان منخفضة الدخل والبلدان متوسطة الدخل (LMIC).
الطريقة
لقد بحثنا في قواعد البيانات في موقع PubMed، والدليل التراكمي للنشريات في مجال التمريض والمهن الصحية المساعدة (CINAHL)، ومنظمة الصحة العالمية (WHO) عن تقارير تبين الرعاية المقدمة في حالات الطوارئ داخل المؤسسات الصحية. وقد استطلعنا بعض المقالات لتضمينها في المراجعة حسب العناوين والملخصات الواردة باللغة الإنجليزية أو الفرنسية. واستخلصنا بيانات بشأن النتائج المتعلقة بالمرضى والخصائص الديموغرافية وخصائص المؤسسات والجهات المقدمة للخدمات. واقتصرت التحليلات على التقارير المنشورة منذ عام 1990.
النتائج
توصلنا إلى تحديد 195 تقريرًا يتعلق بـ 192 مؤسسة في 59 دولة. وكان معظم المؤسسات يمثل مستشفيات تابعة لجهات أكاديمية في مناطق حضرية. وبلغ متوسط نسبة الوفيات داخل أقسام الطوارئ 1.8% (المدى الربيعي: 0.2–5.1%). وكانت نسبة الوفيات مرتفعة نسبيًا في مؤسسات علاج الأطفال (المتوسط: 4.8%؛ المدى الربيعي: 2.3 – 8.4%) وفي الدول الواقعة في جنوب الصحراء الأفريقية (المتوسط: 3.4%؛ المدى الربيعي: 0.5–6.3%). وبلغ متوسط عدد المرضى 30,000 في السنة (المدى الربيعي: 10,296 – 60,000)، حيث كان معظمهم من الشباب (متوسط العمر: 35 عامًا؛ المدى الربيعي: 9.6 – 41.0) والذكور (المتوسط: 55.7%؛ المدى الربيعي: 50.0–59.2%). وضم فريق العمل بمعظم المؤسسات إما أطباء في مرحلة التدريب أو أطباء ذوي مستوى غير محدد من التدريب. وتوفر لدى عدد قليل جدًا من هذه الجهات المقدمة للخدمة الصحية تدريب تخصصي في تقديم الرعاية الصحية في حالات الطوارئ.
الاستنتاج
تشير البيانات المتوفرة عن تقديم الرعاية الصحية في حالات الطوارئ في البلدان منخفضة الدخل والبلدان متوسطة الدخل إلى ارتفاع عدد المرضى لدى الأطباء المتدربين وارتفاع عدد الوفيات، خاصةً في الدول الواقعة جنوب الصحراء الأفريقية، حيث يُحتمل وقوع نسبة كبيرة من جميع حالات الوفاة في أقسام الطوارئ. وإن اجتماع عنصر ارتفاع العدد وعنصر الحاجة الملحة للعلاج يجعل تقديم الرعاية الصحية في حالات الطوارئ نقطة هامة تستحق التركيز عليها في التدخلات التي تهدف إلى تقليل نسبة الوفيات في مثل هذه المناطق.
摘要
目的
旨在对中低收入国家 (LMIC) 中的急救护理进行系统评审。
方法
我们从 PubMed、CINAHL 和世界卫生组织 (WHO) 数据库中搜索了描述机构中急救护理的报告,并且从临床医生和研究人员网络中获取了未经发布的数据。 我们根据其英语或法语标题和摘要筛选了所包含的文章。 我们针对患者疗效和人口统计以及机构和提供方的特性提取了数据。 分析仅限于自 1990 年以来发布的报告。
结果
我们确定了涉及 59 个国家中 192 家机构的 195 份报告。 其中大部分为城市地区的学院附属医院。 急诊部内的平均死亡率为 1.8%(四分位差,IQR: 0.2 至 5.1%)。死亡率在儿科也相对较高(平均值: 4.8%;IQR: 2.3 至 8.4%),而且在撒哈拉以南的非洲死亡率也比较高(平均值: 3.4%;IQR: 0.5 至 6.3%)。患者平均为每年 30 000 例(IQR: 10 296 至 60 000),其中大部分为年轻人(平均年龄: 35 岁;IQR: 6.9 至 41.0)和男性(平均值: 55.7%;IQR: 50.0 至 59.2%)。大多数机构中的工作人员为实习医生或未指定培训水平的医生。 这些提供方中仅有非常少的一部分接受过急救护理方面的专业培训。
结论
中低收入国家 (LMIC) 中现有的急救护理数据表明患者数量和死亡率很高,特别是在撒哈拉以南的非洲,所有死亡中有相当大的一部分比例是发生在急诊部。 治疗量大并且具有紧急性这两个特点的结合让急救护理在我们采取以降低这些环境中的死亡率为目的的干预措施时成为关注的重点领域。
Резюме
Цель
Систематизированный анализ неотложной помощи в странах с низким и средним уровнем доходов населения.
Методы
В базах данных PubMed, CINAHL и Всемирной организации здравоохранения (ВОЗ) был проведен поиск отчетов по оказанию неотложной помощи в медицинских учреждениях. Кроме того, были получены неопубликованные данные от сети практикующих врачей и исследователей. Статьи отбирались по названию и аннотации на английском или французском языке. Отбирались данные по результатам лечения пациентов и демографические данные, а также информация о характеристиках медицинского учреждения и поставщиков медицинских услуг. Анализировались только отчеты, опубликованные с 1990 года.
Результаты
Было отобрано 195 отчетов по 192 медицинским учреждениям в 59 странах. Большинство из этих учреждений являются академическими больницами, расположенными в городских районах. Средняя смертность в отделениях неотложной помощи составляла 1,8% (межквартильный размах, МКР: 0,2–5,1%). Смертность была относительно высокой в педиатрических медицинских учреждениях (медиана: 4,8%; МКР: 2,3–8,4%) и в Африке к югу от Сахары (медиана: 3,4%; МКР: 0,5–6,3%). Среднее количество пациентов составляло 30 000 человек в год (МКР: 10 296–60 000), большинство из которых были молодого возраста (средний возраст: 35 лет; МКР: 6,9–41,0) и мужского пола (медиана: 55,7%; МКР: 50,0–59,2%). Большинство медицинских учреждений были укомплектованы врачами-стажерами или врачами, уровень подготовки которых не указывался. Лишь небольшое число из рассмотренных поставщиков медицинских услуг обладали специальной подготовкой в области неотложной помощи.
Вывод
Доступные данные по оказанию неотложной помощи в странах с низким и средним уровнем доходов свидетельствуют о большой численности поступающих больных и высоком уровне смертности, особенно в Африке к югу от Сахары, где существенная доля всех смертельных случаев приходится на отделения неотложной помощи. Высокий объем инцидентов и срочность необходимого лечения свидетельствуют о том, что неотложная помощь является одной из важнейших областей, на которую следует направить мероприятия по снижению уровня смертности в указанных условиях.
Introduction
Ebola virus disease,1 cholera,2 armed conflict3 and natural disasters4 have recently strained systems for the provision of emergency care in low- and middle-income countries (LMICs). Expert groups have voiced concern about these systems’ critical lack of surge capacity and resilience.5 Even in non-crisis situations, small surveys6,7 and anecdotal accounts8 hint at high volumes of critically-ill patients seeking emergency care in LMICs. This makes emergency care different from other health settings – including primary care – where doctors typically see only 8–10 ambulatory patients per day.9
In high-income countries, decades of advances in clinical science and care delivery have dramatically improved process efficiency and patient outcomes for a range of acute conditions.10–16 Despite increasingly urgent calls to apply lessons learnt in high-income countries to LMICs,17–19 a lack of data from the field has made it difficult to convince policy-makers to make major new investments in emergency care. Measuring the state of emergency care in LMICs is challenging, because care is delivered through a heterogeneous network of facilities and medical records are often incomplete, even for basic information such as patient identity and diagnosis.19–21
Because of these challenges, studies of emergency care in LMICs have been limited to small, ad hoc efforts, in individual facilities, that were focused on individual acute diseases and conditions.22–28 We systematically reviewed all available evidence on emergency care delivery to guide future research on – and improvements of – emergency health systems in LMICs.
Methods
Systematic search
We did a systematic review (PROSPERO: CRD42014007617) – following PRISMA guidelines29 – to identify quantitative data on the delivery of emergency care to an undifferentiated patient population in all LMICs categorized as such in 2013.30 To increase capture, we also included the names of the autonomous or semi-autonomous geographical areas recognized by the World Bank30 and then disaggregated any relevant data obtained for such areas. For each country or subregion, we searched PubMed, CINAHL and World Health Organization (WHO) regional indices,31 using “emerg*” plus the country or area name as the search term. We wished to identify studies of emergency care, irrespective of location, patient complaint or provider specialty. We performed similar searches in Google Scholar but only searched within article titles. We also identified non-indexed journals that regularly published manuscripts on emergency care (available from the corresponding author) and screened every article in every issue of these journals manually. Searches were conducted between 12 August 2013 and 30 May 2014.
We screened reports based on their titles and abstracts in English or French. The full-text potentially relevant articles were retrieved, irrespective of language or date of publication. Since the purpose of our review was to synthesize recent evidence on emergency care, the findings summarized below relate only to data published after 1989. A summary of our observations on data that were published before 1990 is available from the corresponding author. We retained studies describing the delivery of any emergency care in a health facility to adult or paediatric patients, irrespective of the presenting complaint or condition. For each retained article, we conducted backward and forward reference searches: we screened the references cited and, using Google Scholar, we also identified and screened publications that cited the article. We excluded studies that focused on specific conditions or subsets of emergency patients unless they also provided data on the overall population or facility. We also excluded studies that aggregated data from multiple facilities and general descriptions of the state of emergency care in a country. Despite the assistance of trained medical librarians, the full texts of some potentially relevant manuscripts could not be traced. In these cases, we used data from related abstracts or posters, when available.
Unpublished data
We presented the study protocol and early results at the 2013 African Federation for Emergency Medicine consensus conference. We made use of this presentation and our professional networks to request relevant unpublished data from clinicians in LMICs. Some clinicians, researchers and authors were not authorized to release data that allowed the study health facility or facilities to be identified. In these cases, we identified facilities only by their locations and ownership – i.e. academic, non-profit or for-profit.
Data extraction
We extracted data on the characteristics of each study facility: country, urban or rural setting, bed count, annual patient volume, ownership and highest level of provider training. We considered a provider to be an emergency physician if reference was made to specialty postgraduate training, board certification or practice within an independent department of emergency medicine. We recorded details of the study population – i.e. age, sex, number of subjects included in analysis, number who arrived by ambulance – the sampling method and key patient outcomes. The latter included the inpatient admission and mortality within the emergency department, the percentages of patients recorded as brought in dead, or dead on arrival, and the length of time each patient stayed in the emergency department.
We created a database containing aggregated study data. When multiple publications described a single facility, we merged them to create a single record that, for each variable of interest, contained the most recently published data available. We stratified facilities using World Bank regions30 and considered separately those facilities that only served paediatric populations. If data from a single facility were available disaggregated by age group, we summarized quantitative metrics for adult and paediatric patients separately. Full lists of the included studies and the data extracted and a full description of the study protocol are available from the corresponding author.
Descriptive analysis
We calculated summary statistics for all relevant metrics that were reported consistently across studies: bed count, annual patient volume, admission and mortality within the emergency department. We made an a priori decision not to perform a formal meta-analysis. Instead, our systematic analysis was meant to capture the distribution of metrics across populations – e.g. adult versus paediatric – and World Bank regions – e.g. Africa versus Asia – as well as global patterns. We thus present means – or medians with interquartile ranges (IQR) – disaggregated by country or region, as appropriate. Statistical analyses were performed using Stata/MP (StataCorp. LP, College Station, United States of America).
Results
Fig. 1 shows the results of our literature search. Of the 195 relevant published studies identified (Table 1; available at: http://www.who.int/bulletin/volumes/93/14/07-148338), 170 (87%) were descriptive reports on hospital-based emergency departments whereas the other 25 (13%) described the impact of an intervention. We obtained relevant unpublished data on a further 16 facilities. After combining multiple reports from the same facility and separating paediatric and adult data – for the three facilities with disaggregated data – we had data on 192 individual facilities in 59 countries. Of the 192 facilities, 107 (56%) were academically affiliated, 11 (6%) were in rural areas and 36 (19%) served paediatric patients exclusively; in the remaining 38, facility type could not be identified. Further information on the health facilities is available from the corresponding author.
Fig. 1.
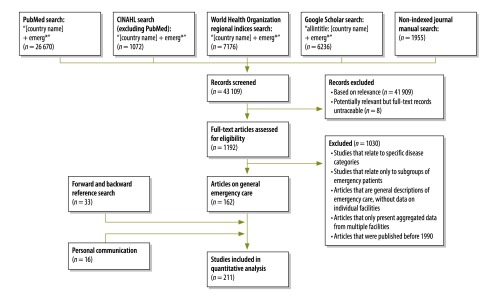
Flowchart for the selection of records on the delivery of emergency care in low- and middle-income countries
Table 1. Identified studies on the delivery of emergency care in low- and middle-income countries.
| Author | Year | Title | Journal | Country or area |
|---|---|---|---|---|
| A-Rahman NHA | 2014 | The state of emergency care in the Republic of the Sudan | Afr J Emerg Med | Sudan |
| Abbadi S et al | 1997 | Emergency medicine in Jordan | Ann Emerg Med | Jordan |
| Abd Elaal SAM et al | 2006 | The waiting time at emergency departments at Khartoum State-2005 | Sudan J Public Health | Sudan |
| Abdallat AM et al | 2007 | Frequent attenders to the emergency room at Prince Rashed Bin Al-Hassan Hospital | J R Med Serv | Jordan |
| Abdallat AM et al | 2000 | Who uses the emergency room services? | Eastern Mediterr Health J | Jordan |
| Abhulimhen-Iyoha BI et al | 2012 | Morbidity and mortality of childhood illnesses at the emergency paediatric unit of the University of Benin Teaching Hospital, Benin City | Nigeria J Pediatr | Nigeria |
| Adeboye MAN et al | 2010 | Mortality pattern within twenty-four hours of emergency paediatric admission in a resource-poor nation health facility | West Afr J Med | Nigeria |
| Adesunkanmi ARK et al | 2002 | A five year analysis of death in accident and emergency room of a semi-urban hospital | West Afr J Med | Nigeria |
| Afuwape OO et al | 2009 | An audit of deaths in the emergency department in the University College Hospital Ibadan | Nigeria J Clin Pract | Nigeria |
| Aggarwal P et al | 1995 | Utility of an observation unit in the emergency department of a tertiary care hospital in India | European J Emerg Med | India |
| Akpa MR et al | 2013 | Profile and outcome of medical emergencies in a tertiary health institution in Port Harcourt, Nigeria | Nigeria Health J | Nigeria |
| Al-Hakimi ASA et al | 2004 | Load and pattern of patients visiting general emergency Al-Thawra Hospital, San a'a | Yemen Health Medical Res J | Yemen |
| Alagappan K et al | 1998 | Early development of emergency medicine in Chennai (Madras), India | Ann Emerg Med | India |
| Asumanu E et al | 2009 | Improving emergency attendance and mortality – the case for unit separation | West Afr J Med | Ghana |
| Atanda HL et al | 1994 | Place des urgences medicales pediatriques dans un service medical a Pointe-Noire | Med Afr Noire | Congo |
| Avanzi MP et al | 2005 | Diagnósticos mais freqüentes em serviço de emergência para adulto de um hospital universitário | Rev Ciênc Méd | Brazil |
| Azhar AA et al | 2000 | Patient attendance at a major accident and emergency department: Are public emergency services being abused? | Med J Malaysia | Malaysia |
| Bains HS et al | 2012 | A simple clinical score “TOPRS” to predict outcome in pediatric emergency department in a teaching hospital in India | Iran J Pediatr | India |
| Bamgboye EA et al | 1990 | Mortality pattern at a children’s emergency ward, University College Hospital, Ibadan, Nigeria | Afr J Med Med Sci | Nigeria |
| Basnet B et al | 2012 | Initial resuscitation for Australasian Triage Scale 2 patients in a Nepalese emergency department | Emerg Med Australas | Nepal |
| Batistela S et al | 2008 | Os motivos de procura pelo Pronto Socorro Pediátrico de um Hospital Universitário referidos pelos pais ou responsáveis | Semina: Ciênc Biológicas Saúde | Brazil |
| Bazaraa HM et al | 2012 | Profile of patients visiting the pediatric emergency service in an Egyptian university hospital | Pediatr Emerg Care | Egypt |
| Ben Gobrane HLB et al | 2012 | Motifs du recours aux services d’urgence des principaux hôpitaux du Grand Tunis | East Mediterr Health J | Tunisia |
| Berraho M et al | 2012 | Les consultations non approprieés aux services des urgences: étude dans un hôpital provincial au Maroc | Prat Organ Soins | Morocco |
| Boff JM et al | 2002 | Perfil do Usuário do Setor de Emergência do Hospital Universitário da UFSC | Rev Contexto Saude | Brazil |
| Boros MJ | 2003 | Emergency medical services in St. Vincent and the Grenadines | Prehosp Emerg Care | St. Vincent and the Grenadines |
| Bresnahan KA et al | 1995 | Emergency medical care in Turkey: current status and future directions | Ann Emerg Med | Turkey |
| Brito MVH et al | 1998 | Pronto-atendimento de adultos em serviço de saúde universitário: um estudo de avaliação | Rev Adm Publica | Brazil |
| Brito MVH et al | 2012 | Perfil da demanda do serviço de urgência e emergência do hospital pronto socorro municipal- Mario Pinotti | Rev Paraense Med | Brazil |
| Brown MD | 1999 | Emergency medicine in Eritrea: rebuilding after a 30-year war | Am J Emerg Med | Eritrea |
| Bruijns S et al | 2008 | A prospective evaluation of the Cape triage score in the emergency department of an urban public hospital in South Africa | Emerg Med J | South Africa |
| Burch V et al | 2008 | Modified early warning score predicts the need for hospital admission and inhospital mortality | Emerg Med J | South Africa |
| Buys H et al | 2013 | An adapted triage tool (ETAT) at Red Cross War Memorial Children’s Hospital Medical Emergency Unit, Cape Town: an evaluation | S Afr Med J | South Africa |
| Cander B et al | 2006 | Emergency operation indications in emergency medicine clinic (model of emergency medicine in Turkey) | Adv Ther | Turkey |
| Carret MLV et al | 2007 | Demand for emergency health service: factors associated with inappropriate use | BMC Health Serv Res | Brazil |
| Carret MLV et al | 2011 | Características da demanda do serviço de saúde de emergência no Sul do Brasil | Cien Saude Colet | Brazil |
| Cevik AA et al | 2001 | Update on the development of emergency medicine as a specialty in Turkey | European J Emerg Med | Turkey |
| Chattoraj A et al | 2006 | A study of sickness & admission pattern of patients attending an emergency department in a tertiary care hospital | J AcadHosp Adm | India |
| Chukuezi AB et al | 2010 | Pattern of deaths in the adult accident and emergency department of a sub-urban teaching hospital in Nigeria | Asian J Med Sci | Nigeria |
| Clark M et al | 2012 | Reductions in inpatient mortality following interventions to improve emergency hospital care in Freetown, Sierra Leone | PLoS one | Sierra Leone |
| Clarke ME | 1998 | Emergency medicine in the new South Africa | Ann Emerg Med | South Africa |
| Clem KJ et al | 1998 | United States physician assistance in development of emergency medicine in Hangzhou, China | Ann Emerg Medi | China |
| Coelho MF et al | 2010 | Analysis of the organizational aspects of a clinical emergency department: a study in a general hospital in Ribeirao Preto, SP, Brazil | Rev Lat Am Enfermagem | Brazil |
| Coelho MF et al | 2013 | Urgências clínicas: perfil de atendimentos hospitalares | Rev Lat Am Enfermagem | Brazil |
| Cox M et al | 2007 | Emergency medicine in a developing country: experience from Kilimanjaro Christian Medial Centre, Tanzania, East Africa | Emerg Med Australas | The United Republic of Tanzania |
| Curry C et al | 2004 | The first year of a formal emergency medicine training programme in Papua New Guinea | Emerg Med Australas | Papua New Guinea |
| da Silva GS et al | 2007 | Caracterização do perfil da demanda da emergência de clínica médica do hospital universitário da Universidade Federal de Santa Catarina | Arq Catarinenses Med | Brazil |
| Dalwai M et al | 2013 | Implementation of a triage score system in an emergency room in Timergara, Pakistan | Public Health Action | Pakistan |
| Damghi N et al | 2013 | Patient satisfaction in a Moroccan emergency department | Intl Arch Med | Morocco |
| Dan V et al | 1991 | Prise en charge des urgences du nourrisson et de l'enfant: aspects actuels et perspectives d'avenir | Med Afr Noire | Benin |
| de Souza LM et al | 2011 | Risk classification in an emergency room: agreement level between a Brazilian institutional and the Manchester Protocol | Rev Lat Am Enfermagem | Brazil |
| De Vos P et al | 2008 | Uses of first line emergency services in Cuba | Health Policy | Cuba |
| Derlet RW et al | 2000 | Emergency medicine in Belarus | J Emerg Med | Belarus |
| Dubuc IF et al | 2006 | Adolescentes atendidos num serviço púlico de urgência e emergência: perfil de morbidade e mortalidade | Rev Eletrônica Enfermagem | Brazil |
| Duru C et al | 2013 | Pattern and outcome of admissions as seen in the paediatric emergency ward of the Niger Delta University Teaching Hospital Bayelsa State, Nigeria | Nigeria J Pediatr | Nigeria |
| Ekere AU et al | 2005 | Mortality patterns in the accident and emergency department of an urban hospital in Nigeria | Nigeria J Clinic Pract | Nigeria |
| Enobong EI et al | 2009 | Pattern of paediatric emergencies and outcome as seen in a tertiary hosptial: a five-year review | Sahel Med J | Nigeria |
| Erickson TB et al | 1996 | Emergency medicine education intervention in Rwanda | Ann Emerg Med | Rwanda |
| Eroglu SE et al | 2012 | Evaluation of non-urgent visits to a busy urban emergency department | Saudi Med J | Turkey |
| Fajardo-Oritz G et al | 2000 | Utilización del servicio de urgencias en un hospital de especialidades | Cir Cir | Mexico |
| Fajolu IB et al | 2011 | Childhood mortality in children emergency centre of the Lagos University Teaching hospital | Nigeria J Pediatr | Nigeria |
| Fayyaz J et al | 2013 | Missing the boat: odds for the patients who leave ED without being seen | BMC Emerg Med | Pakistan |
| Furtado BMA et al | 2004 | O perfil da emergência do Hospital da Restauração: uma análise dos possíveis impactos após a municipalização dos serviços de saúde | Revi Bras Epidemiol | Brazil |
| Gaitan M et al | 1998 | Growing pains: status of emergency medicine in Nicaragua | Ann Emerg Med | Nicaragua |
| Garg M et al | 2013 | Study of the relation of clinical and demographic factors with morbidity in a tertiary care teaching hospital in India | Int J Crit Illn Inj Sci | India |
| George IO et al | 2010 | An audit of cases admitted in the children emergency ward in a Nigerian tertiary hospital | Pakistan J Med Sci | Nigeria |
| Gim U et al | 2012 | Pattern and outcome of presentation at the children emergency unit of a tertiary institution in the Niger Delta region of Nigeria: a one year prospective study | J Med | Nigeria |
| Goh AY et al | 2003 | Paediatric utilization of a general emergency department in a developing country | Acta Paediatr | Malaysia |
| Gomide MFS et al | 2012 | Perfil de usuários em um serviço de pronto atendimento | Med (Ribeirão Preto) | Brazil |
| Gueguen G | 1995 | Senegal: mise en place d’un mirco ordinateur dans le service d’accueil des urgencies de l’hopital regional de Ziguinchor | Med Trop | Senegal |
| Halasa W | 2013 | Family medicine in the emergency department, Jordan | Br J Gen Pract | Jordan |
| Hanewinckel R et al | 2010 | Emergency medicine in Paarl, South Africa: a cross-sectional descriptive study | Int J Emerg Med | South Africa |
| Hexom B et al | 2012 | A model for emergency medicine education in post-conflict Liberia | Afr J Emerg Medi | Liberia |
| Hodkinson PW et al | 2009 | Cross-sectional suvey of patients presenting to a South African urban emergency centre | Emerg Med J | South Africa |
| House DR et al | 2013 | Descriptive study of an emergency centre in Western Kenya: challenges and opportunities | Afr J Emerg Med | Kenya |
| Huo X | 1994 | Emergency care in China | Accid Emerg Nur | China |
| Ibeziako SN et al | 2002 | Pattern and outcome of admissions in the children's emergency room of the University of Nigeria Teaching Hospital, Enugu | Nigeria J Paediatr | Nigeria |
| Jacobs PC et al | 2005 | Estudo exploratório dos atendimentos em unidade de emergência em Salvador-Bahia | Rev Assoc Méd Bras | Brazil |
| Jafari-Rouhi AH et al | 2013 | The Emergency Severity Index, version 4, for pediatric triage: a reliability study in Tabriz Children’s Hospital, Tabriz, Iran |
Int J Emerg Med | Islamic Republic of Iran |
| Jalili M et al | 2013 | Emergency department nonurgent visits in Iran: prevalence and associated factors | Am J Manag Care | Islamic Republic of Iran |
| Jerius M et al | 2010 | Inappropriate utilization of emergency medical services at Prince Ali Military Hospital | J R Med Serv | Jordan |
| Ka Sall B et al | 2002 | Les urgences dans un centre hospitalier et universitaire en milieu tropical | Méd Trop | Senegal |
| Karabocuoglu M et al | 1995 | Analysis of patients admitted to the emergency unit of a university children's hosptial in Turkey | Turk J Pediatr | Turkey |
| Karim MZ et al | 2009 | A retrospective study of illness and admission pattern of emergency patients utilizing a corporate hospital in Dhaka, Bangladesh: 2006 −2008 | ORION Med J | Bangladesh |
| Khan NU et al | 2011 | Unplanned return visit to emergency department: a descriptive study from a tertiary care hospital in a low-income country | European J Emerg Med | Pakistan |
| Khan NU et al | 2007 | Emergency department deaths despite active management: experience from a tertiary care centre in a low-income country | Emerg Med Australas | Pakistan |
| Khan AN et al | 2003 | International pediatric emergency care: establishment of a new specialty in a developing country | Pediatr Emerg Care | Serbia |
| Kriengsoontornkij W et al | 2010 | Accuracy of pediatric triage at Siriraj Hospital, Bangkok, Thailand | J Medl Ass Thailand | Thailand |
| Krym VF et al | 2009 | International partnerships to foster growth in emergency medicine in Romania | CJEM | Romania |
| Lammers W et al | 2011 | Demographic analysis of emergency department patients at the Ruijin Hospital, Shanghai | Emerg Med Int | China |
| Lasseter JA et al | 1997 | Emergency medicine in Bosnia and Herzegovina | Ann Emerg Med | Bosnia and Herzegovina |
| Lee S | 2011 | Disaster management and emergency medicine in Malaysia | West J Emerg Med | Malaysia |
| Leite JA et al | 2010 | Internaçöes e serviços de urgência e emergência pactuados em hospital geral púlico da Bahia, Brazil | Rev Baiana Saude Publica | Brazil |
| Lima SBS et al | 2013 | Perfil clínico-epidemiológico dos pacientes internados no prontosocorro de um hospital universitário | Saude (Santa Maria) | Brazil |
| Lin JY et al | 2013 | Breadth of emergency medical training in Pakistan | Prehosp Disaster Med | Pakistan |
| Little RM et al | 2013 | Acute care in Tanzania: epidemiology of acute care in a small community medical centre | Afr J Emerg Med | The United Republic of Tanzania |
| Liu Y et al | 1994 | A preliminary epidemiological study of the patient population visiting an urban ED in the Republic of China | Am J Emerg Med | China |
| Lopes SLB et al | 2007 | The implementation of the Medical Regulation Office and Mobile Emergency Attendance System and its impact on the gravity profile of non-traumatic afflictions treated in a University Hospital: a research study | BMC Health Serv Res | Brazil |
| Loria-Castellanos J et al | 2006 | Reanimation unit experience of a second- level hospital in Mexico City | Prehosp Disaster Med | Mexico |
| Loria-Castellanos J et al | 2010 | Frecuencia y factores asociados con el uso inadecuado de la consulta de urgencias de un hospital | Cir Cir | Mexico |
| Mabiala-Babela JR et al | 2007 | Consultations et réadmissions avant l’âge d’un mois aux urgences pédiatriques, Brazzaville (Congo) | Arch Pediatr | Congo |
| Mabiala-Babela JR et al | 2009 | Consultations de nuit aux urgences pédiatriques du CHU de Brazzaville, Congo | Méd Trop | Congo |
| Mahajan V et al | 2013 | Unexpected hospitalisations at a 23-Hour observation unit in a paediatric emergency department of northern India | J Clin Diagn Res | India |
| Maharjan RK | 2011 | Mortality pattern in the emergency department in Tribhuvan University Teaching Hospital, Kathmandu, Nepal | Prehosp Disaster Med | Nepal |
| Malhotra S et al | 1992 | A study of the workload of the casualty department of a large city hospital | Health Popul Perspect Issues | India |
| Martinez RQ et al | 2008 | Padecimientos más frecuentemente atendidos en el Servicio de Urgencias Pediátricas en un hospital de tercer nivel |
Rev Fac Med Univ Auton Mex | Mexico |
| Matoussi N et al | 2007 | Profil epidemiologique et prise en charge des consultants des urgences medicales pediatriques de l’hopital d’enfants de Tunis | Tunis Med | Tunisia |
| Maulen-Radovan I et al | 1996 | PRISM score evaluation to predict outcome in paediatric patients on admission at an emergency department | Arch Med Res | Mexico |
| Mbutiwi Ikwa Ndol F et al | 2013 | Facteurs pre ´dictifs de la mortalite ´ des patients admis aux urgences me ´dicales des cliniques universitaires de Kinshasa | Rev Epidemiol Sante Publique | Democratic Republic of the Congo |
| McDonald A et al | 2005 | Emergency medicine in Jamaica | CJEM | Jamaica |
| McDonald A et al | 2000 | Morbidity pattern of emergency room patients in Jamaica | West Indian Med J | Jamaica |
| Medina J et al | 2007 | Triage: experiencia en un Servicio de Urgencias Pediátricas | Rev Soc Boliv Pediatr | Paraguay |
| Meijas CLA | 2011 | La atención de urgencia y la dispensarización en el Policlínico Universitario Docente de Playa | Rev Cubana Med Gen Integral | Cuba |
| Melo EMC et al | 2007 | O trabalho dos pediatras em um serviço público de urgências: fatores intervenientes no atendimento |
Cad Saude Publica | Brazil |
| Meskin S et al | 1997 | Delivery of emergency medical services in Kathmandu, Nepal | Ann Emerg Med | Nepal |
| Mijinyawa MS | 2010 | Pattern of medical emergency utilisation in a Nigeria tertiary health institution: a preliminary report | Sahel Med J | Nigeria |
| Miranda NA et al | 2012 | Caracterização de crianças atendidas no pronto-socorro de um hospital universitário | Rev Eletrônica Gestão Saúde | Brazil |
| Molyneux E et al | 2006 | Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting | Bull World Health Organ | Malawi |
| Morton TD | 1992 | A perspective on emergency medicine in the developing world | J Emerg Med | Malaysia |
| Mullan PC et al | 2013 | Reduced overtriage and undertriage with a new triage system in an urban accident and emergency department in Botswana: a cohort study | Emerg Med J | Botswana |
| Muluneh D et al | 2007 | Analysis of admissions to the pediatric emergency ward of Tikur Anbessa Hospital in Addis Ababa, Ethiopia | Ethiop J Health Dev | Ethiopia |
| Musharafieh R et al | 1996 | Development of emergency medicine in Lebanon | Ann Emerg Med | Lebanon |
| Naidoo DK et al | 2014 | An evaluation of the Triage Early Warning Score in an urban accident and emergency department in KwaZulu-Natal | S Afr Family Pract | South Africa |
| Nelson BD et al | 2005 | Integrating quantitative and qualitative methodologies for the assessment of health care systems: emergency medicine in post-conflict Serbia | BMC Health Serv Res | Serbia |
| Nemeth J et al | 2001 | Emergency medicine in Eastern Europe: the Hungarian experience | Ann Emerg Med | Hungary |
| Nkombua L | 2008 | The practice of medicine at a district hospital emergency room: Middelburg Hospital, Mpumalanga Province | S Afr Family Pract | South Africa |
| O'Reilly G et al | 2010 | The dawn of emergency medicine in Vietnam | Emerg Med Australas | Viet Nam |
| Ogah OS et al | 2012 | A two-year review of medical admissions at the emergency unit of a Nigerian tertiary health facility | Afr J Biomed Res | Nigeria |
| Ogunmola OO et al | 2013 | Mortality pattern in adult accident and emergency department of a tertiary health centre situated in a rural area of developing country | J Dent Med Sci | Nigeria |
| Ohara K et al | 1994 | Investigación sobre pacientes atendidos en el servicio de emergencia del Hospital Escuela | Rev Med Hondur | Honduras |
| Okolo SN et al | 2002 | Health service auditing and intervention in an emergency paediatric unit | Nigeria J Paediatr | Nigeria |
| Oktay C et al | 2003 | Appropriateness of emergency department visits in a Turkish university hospital | Croat Med J | Turkey |
| Olivati FN et al | 2010 | Perfil da demanda de um pronto-socorro em um município do interior do estado de São Paulo |
Rev Fac Odontol Univ Passo Fundo | Brazil |
| Oliveira GN et al | 2011 | Profile of the population cared for in a referral emergency unit | Rev Lat Am Enfermagem | Brazil |
| Onwuchekwa AC et al | 2008 | Medical mortality in the accident and emergency unit of the University of Port Harcourt Teaching Hospital | Nigeria J Med | Nigeria |
| Orimadegun AE et al | 2008 | Comparison of neonates born outside and inside hospitals in a children emergency unit, southwest of Nigeria | Pediatr Emerg Care | Nigeria |
| Osuigwe AN et al | 2002 | Mortalty in the accident and emergency unit of Nnamdi Azikiwe University Teaching Hospital, NNEWI: patterns and factors involved | Nigeria J Clin Pract | Nigeria |
| Parekh KP et al | 2013 | Who leaves the emergency department without being seen? A public hospital experience in Georgetown, Guyana | BMC Emerg Med | Guyana |
| Partridge RA | 1998 | Emergency medicine in West Kazakhstan, CIS | Ann Emerg Med | Kazakhstan |
| Patil A | 2013 | Analysis of pattern of emergency cases in the casualty of a university | Indian J Forensic Med Toxicol | India |
| Peixoto BV et al | 2013 | The harsh reality of children and youth emergency care showing the health status of a city | Rev Paul Pediatr | Brazil |
| Pekdemir M et al | 2010 | No significant alteration in admissions to emergency departments during Ramadan | J Emerg Med | Turkey |
| Periyanayagam U et al | 2012 | Acute care needs in a rural Sub-Saharan African emergency centre: a retrospective analysis | Afr J Emerg Med | Uganda |
| Pinilla MMA et al | 2009 | Demandas inadecuadas en urgencias e identificación del uso inapropriado de la hospitalización en el Centro Piloto de ASSBASALUD ESE. en Manizales. año 2008 | Arch Med | Colombia |
| PoSaw LL et al | 1998 | Emergency medicine in the new Delhi Area, India | Ann Emerg Med | India |
| Raftery KA | 1996 | Emergency medicine in southern Pakistan | Ann Emerg Med | Pakistan |
| Ramalanjaona G | 1998 | Emergency medicine in Madagascar | Ann Emerg Med | Madagascar |
| Rashidi A et al | 2009 | Demographic and clinical characteristics of red tag patients and their one-week mortality rate from the emergency department of the Hospital Universiti Sains Malaysia | South-east Asian J Trop Med Public Health | Malaysia |
| Rehmani R | 2004 | Emergency section and overcrowding in a university hospital of Karachi, Pakistan | J Pak Med Assoc | Pakistan |
| Reynolds TA et al | 2012 | Most frequent adult and pediatric diagnoses among 60 000 patients seen in a new urban emergency department in Dar es Salaam, Tanzania | Ann Emerg Med | The United Republic of Tanzania |
| Reynolds TA et al | 2012 | Emergency care capacity in Africa: a clinical and educational initiative in Tanzania | J Public Health Policy | The United Republic of Tanzania |
| Ribeiro RCH et al | 2013 | Stay and outcome of the clinical and surgical patient in the emergency service | Rev Enfermagem | Brazil |
| Riccetto AGL et al | 2007 | Sala de emergência em pediatria: casuística de um hospital universitário | Revi Paul Pediatr | Brazil |
| Richards JR | 1997 | Emergency medicine in Vietnam | Ann Emerg Med | Viet Nam |
| Robison JA et al | 2012 | Decreased pediatric hospital mortality after an intervention to improve emergency care in Lilongwe, Malawi | Pediatr | Malawi |
| Rodriguez JCM et al | 2012 | Aplicación de los criterios de ingreso a la unidad de reanimación en el servicio de urgencias de adultos del Hospital General «La Raza» | Arch Medi Urg Méx | Mexico |
| Rodriguez JP et al | 2001 | “Filtro Sanitario” en las urgencias médicas. Un problema a reajustar | Rev Cubana Med | Cuba |
| Rosa TP et al | 2011 | Perfil dos pacientes atendidos na sala de emergência do pronto Socorro de um hospital universitário | Rev Enfermagem UFSM | Brazil |
| Rosedale K et al | 2011 | The effectiveness of the South African Triage Score (SATS) in a rural emergency department | S Afr Med J | South Africa |
| Rytter MJH et al | 2006 | Effects of armed conflict on access to emergency health care in Palestinian West Bank: systematic collection of data in emergency departments | BMJ | West Bank and Gaza Strip |
| Salaria M et al | 2003 | Profile of patients attending pediatric emergency service at Chandigarh | Indian J Pediatr | India |
| Salgado RMP et al | 2010 | Perfil dos pacientes pediátricos atendidos na emergência de um hospital universitário |
Pediatr (Sao Paulo) | Brazil |
| Santhanam I et al | 2002 | Mortality after admission in the pediatric emergency department: a prospective study from a referral children’s hospital in southern India | Pediatr Critical Care Med | India |
| Savitsky E et al | 2000 | Emergency medical services development in the Seychelles Islands | Am J Emerg Med | Seychelles |
| Selasawati HG et al | 2004 | Inappropriate utilization of emergency department services in Universiti Sains Malaysia Hospital | Med J Malaysia | Malaysia |
| Sentilhes-Monkam A | 2011 | Les services d’accueil des urgences ont-ils un avenir en Afrique de l’ouest? Exemple à l’hôpital principal de Dakar | Sante Publique | Senegal |
| Shakhatreh H et al | 2009 | Patient satisfaction in emergency department at King Hussein Medical Center | J R Med Serv | Jordan |
| Shakhatreh H et al | 2003 | Use and misuse of accident and emergency services at Queen Alia Military Hospital | J R Med Serv | Jordan |
| Simons DA et al | 2010 | Adequação da demanda de crianças e adolescentes atendidos na Unidade de Emergência em Maceió, Alagoas, Brasil | Rev Bras Saúde Matern Infant | Brazil |
| Singhi S et al | 2004 | Comparison of pediatric emergency patients in a tertiary care hospital vs a community hospital | Indian Pediatr | India |
| Singhi S et al | 2003 | Pediatric emergencies at a tertiary care hospital in India | J Trop Pediatr | India |
| Smadi BY et al | 2005 | Inappropriate use of emergency department at Prince Zeid Ben Al-Hussein Hospital | J R Med Serv | Jordan |
| Soleimanpour H et al | 2011 | Emergency department patient satisfaction survey in Imam Reza Hospital, Tabriz, Iran | Int J Emerg Med | Islamic Republic of Iran |
| Souza BC et al | 2009 | Perfil da Demanda do Departamento de Emergência do Hospital Nossa Senhora da Conceição – Tubarão – SC | Arq Catarinenses Med | Brazil |
| Tannebaum RD et al | 2001 | Emergency Medicine in Southern Brazil | Ann Emerg Med | Brazil |
| Taye BW et al | 2014 | Quality of emergency medical care in Gondar University Referral Hospital, north-west Ethiopia: a survey of patient's perspectives: a survey of patients’ perspectives | BMC Emerg Med | Ethiopia |
| Tiemeier K et al | 2013 | The effect of geography and demography on outcomes of emergency department patients in rural Uganda | Ann Emerg Med | Uganda |
| Tinaude O et al | 2010 | Health-care-seeking behaviour for childhood illnesses in a resource-poor setting | J Paediatr Child Health | Nigeria |
| Tintinalli J et al | 1998 | Emergency care in Namibia | Ann Emerg Med | Namibia |
| Topacoglu H et al | 2004 | Analysis of factors affecting satisfaction in the emergency department: a survey of 1 019 patients | Adv Ther | Turkey |
| Traoré A et al | 2002 | Les urgences médicales au Centre hospitalier national Yalgado Ouédraogo de Ouagadougou : profil et prise en charge des patients | Cah Etud Rech Francophones / Santé | Burkina Faso |
| Trejo JA et al | 1999 | El servicio de urgencias en un hospital de tercer nivel. Su comportamiento durante cinco años: estudio preliminar | Med Interna Mex | Mexico |
| Tsiperau J et al | 2010 | The management of paediatric patients in a general emergency department in Papua New Guinea | P N G Med J | Papua New Guinea |
| Ugare GU et al | 2012 | Epidemiology of death in the emergency department of a tertiary health centre south-south of Nigeria | Afr Health Sc | Nigeria |
| Veras JEG et al | 2011 | Profile of children attended in emergency according to the risk classification: a documental study | Online Bras J Nurs | Brazil |
| Veras JEG et al | 2009 | Analise das causas de atendimento de crianças e adolescentes menores de 15 anos em pronto-atendimento de um hospital secundário de Fortaleza | Congr Bras Enfermagem | Brazil |
| Wang L et al | 2011 | Application of emergency severity index in pediatric emergency department | World J Emerg Med | China |
| Webb HR et al | 2001 | Emergency medicine in Ecuador | Am J Emerg Med | Ecuador |
| Williams EW et al | 2008 | The evolution of emergency medicine in Jamaica | West Indian Med J | Jamaica |
| Wright SW et al | 2000 | Emergency medicine in Ukraine: challenges in the post-Soviet era | Am J Emerg Med | Ukraine |
| Yaffee AQ et al | 2012 | Bypassing proximal health care facilities for acute care: a survey of patients in a Ghanaian accident and emergency centre | Trop Med Int Health | Ghana |
| Yildirim C et al | 2005 | Patient satisfaction in a university hospital emergency department in Turkey | Acta Med | Turkey |
| Zhou JC et al | 2012 | High hospital occupancy is associated with increased risk for patients boarding in the emergency department | Am J Med | China |
Notes: Further information about the studies can be obtained from corresponding author. Additional data were obtained through personal communications from: Botswana (1), Cameroon (1), Ghana (1), Lebanon (1), Liberia (1), Madagascar (1) and South Africa (10).
Table 2 presents the key metrics for the facilities. Median mortality within the emergency departments – of the 65 facilities that reported the relevant data – was 1.8% overall and higher in the 19 paediatric facilities (4.8%) than in the 46 adult or general facilities (0.7%). Across World Bank regions that we investigated, mortality was highest in sub-Saharan Africa (3.4%; IQR: 0.5–6.3%; n = 44), especially in east, central or west Africa (4.8%; IQR: 3.3–8.4%; n = 30). Paediatric facilities in sub-Saharan Africa had a median mortality of 5.1% (IQR: 3.5–11.1%; n = 15). Mortality in emergency facilities was also high in Latin America. Two facilities in Brazil were major contributors to this high rate, with mortality of 7.4%32 and 3.9%.33 These centres also reported long inpatient stays: one facility reported a median length of stay of three days,32 whereas the other reported that 21% of patients stayed in the emergency department for more than five days.33 Lengths of stay were only reported for 15 facilities and for these, the median value was 7.7 hours (IQR: 3.3–40.8). As mortality data were only available for nine of these 15 facilities, it was not possible to formally investigate the relationship between length of stay and mortality. The five sub-Saharan African facilities that recorded length of stay reported a median stay of 17 hours (IQR: 16.9–18.0). Additional data comparing mortality, patient volumes and admission are available from the corresponding author.
Table 2. Key quantitative data for emergency departments, 59 low- and-middle-income countries, 1990–2014.
| Metric | Facility type | Unitsa | All regions | Sub-Saharan Africa | South Asia, East Asia & Pacific | Middle East & North Africa | Latin America & Caribbean | Europe & Central Asia |
|---|---|---|---|---|---|---|---|---|
| No. of beds | All | n | 60 | 24 | 20 | 4 | 9 | 3 |
| All | Median (IQR) | 14 (8–22) | 9 (8–14) | 21 (15–23) | 11 (8–25) | 17 (12–22) | 16 (16–27) | |
| Annual patient volume (thousands) | All | n | 173 | 64 | 35 | 24 | 42 | 8 |
| All | Median (IQR) | 30.0 (10.3–60.0) | 13.6 (3.4–29.8) | 36.5 (8.3–70.0) | 49.0 (34.0–68.8) | 52.4 (26.0–87.0) | 33.8 (15.3–72.1) | |
| General and adult | Median (IQR) | 36.9 (15.8–64.2) | 16.7 (5.1–35.3) | 50.0 (29.2–81.2) | 53.6 (34.0–79.0) | 59.7 (31.0–89.1) | 36.5 (14.6–82.1) | |
| Paediatric | Median (IQR) | 7.2 (2.3–31.6) | 3.1 (2.0–7.5) | 5.6 (2.2–7.6) | 43.0 (22.1–44.3) | 27.5 (13.5–68.1) | 31.0 (NA) | |
| Admission, % | All | n | 78 | 26 | 16 | 15 | 20 | 1 |
| All | Median (IQR) | 20.0 (10.1–42.8) | 24.5 (16.5–46.9) | 26.0 (15.0–38.7) | 18.2 (10.1–22.2) | 11.1 (3.9–20.7) | 50.0 (NA) | |
| General and adult | Median (IQR) | 18.8 (9.4–40.1) | 24.5 (15.8–46.5) | 24.2 (15.0–36.3) | 14.9 (7.7–18.9) | 10.2 (3.9–19.5) | 50.0 (NA) | |
| Paediatric | Median (IQR) | 22.2 (10.7–44.3) | 33.2 (20.6–65.2) | 32.5 (14.0–43.0) | 21.8 (15.7–28.6) | 14.3 (6.4–35.4) | NA (NA) | |
| Mortality,%b | All | n | 65 | 44 | 9 | 5 | 7 | NA |
| All | Median (IQR) | 1.8 (0.2–5.1) | 3.4 (0.5–6.3) | 0.3 (0.2–0.8) | 0.7 (0.2–2.1) | 2.0 (0.1–7.4) | NA (NA) | |
| General and adult | Median (IQR | 0.7 (0.2–3.9) | 0.9 (0.2–4.8) | 0.3 (0.2–0.5) | 0.5 (0.2–1.4) | 2.0 (0.1–7.4) | NA (NA) | |
| Paediatric | Median (IQR) | 4.8 (2.3–8.4) | 5.1 (3.5–11.1) | 0.8 (< 0.1–2.7) | 7.8 (NA) | NA (NA) | NA (NA) |
IQR: interquartile range; NA: not available.
a For each metric and region, the number of facilities for which the relevant data were available (n) is indicated.
b Within the emergency department.
Data sources listed in Table 1, (available at: http://www.who.int/bulletin/volumes/93/14/07-148338).
Median annual patient volume was 30 021 (IQR: 10 296–60 000) among 173 facilities reporting these data. Volume was lower in the nine rural facilities (16 468; IQR: 3429–44 395) than in the 164 urban ones (31 000; IQR: 10 994–61 313). The 17 paediatric facilities in Sub-Saharan Africa had relatively low patient volumes with a median annual patient volume of 3129 (IQR: 2009–7479). The median inpatient admission was 20% (IQR: 10–43%; n = 78) and the median number of beds in the emergency department was 14 (IQR: 8–22; n = 60). The median age of patients attending non-paediatric facilities was 35 years (IQR: 6.9–41.0; n = 51) and a median of 55.7% (IQR: 50.0–59.2%; n = 93) were male. The corresponding values for paediatric facilities were 3.2 years (IQR: 2.8–3.4; n = 13) and 58.3% (IQR: 55.4–60.1%; n = 27), respectively.
Table 3 summarizes the training of providers staffing the 102 facilities for which provider data were available. Care in 67 (66%) of these facilities was provided either by trainees or by physicians whose level of training was not specified. In only 29 (28%) of facilities were attending or consultant-level physicians available full-time; in 19 other facilities, physicians were only available in daytime hours. Eighteen facilities were staffed by specialty-trained emergency physicians, but in only four facilities were emergency physicians available at all times – one in the United Republic of Tanzania (unpublished observations, 2014), one in Pakistan34 and two in Nicaragua.35 One facility provided specialized emergency training to non-physician providers staffing the emergency department.36 In another facility, medical students practising alone were primarily responsible for providing emergency care during most of the day.37 Patients had to navigate through a wide range of options to obtain emergency care and financial factors played a major role in determining what kind of care they received (details available from the corresponding author).
Table 3. Training of providers of emergency care included in systematic analysis, 49 low- and-middle-income countries, 1991–2014.
| Region,a country | No. of facilities |
|||
|---|---|---|---|---|
| Non-physician or medical student | Physician in training or with unspecified level of training | Attending physician or consultant | Emergency physician | |
| Sub-Saharan Africa | ||||
| Botswana | – | 1 | – | 1b |
| Burkina Faso | – | 1 | – | – |
| Cameroon | – | 1 | 1b | – |
| Congo | 1 | – | 1b | – |
| Eritrea | – | 1 | – | – |
| Ghana | – | 2 | – | – |
| Kenya | – | 1 | – | – |
| Liberia | – | 1 | 1b | – |
| Madagascar | – | 1 | 1 | – |
| Malawi | – | – | 2 | – |
| Namibia | – | 1 | – | – |
| Nigeria | – | 4 | 2 | 1b |
| Rwanda | – | 1 | – | – |
| Seychelles | – | 1 | – | – |
| Sierra Leone | – | 1 | – | – |
| South Africa | – | 8 | 4 | 1b |
| Sudan | – | 2 | – | 2c |
| Uganda | 1b | – | – | – |
| United Republic of Tanzania | – | 2 | – | 1 |
| South Asia, East Asia & Pacific | ||||
| China | – | 2 | 2b | – |
| India | – | 3 | 7c | – |
| Kazakhstan | – | 1 | – | – |
| Malaysia | – | 2 | – | 1b |
| Nepal | – | 4 | 3d | 1b |
| Pakistan | – | 2 | 1 | 1 |
| Papua New Guinea | – | 1 | – | – |
| Viet Nam | – | 2 | – | – |
| Latin America & Caribbean | ||||
| Brazil | – | 1 | 3 | – |
| Cuba | – | – | 2 | – |
| Ecuador | – | 3 | 1b | – |
| Guyana | – | 1 | – | – |
| Jamaica | – | – | 1 | 1b |
| Mexico | – | 1 | – | 1b |
| Nicaragua | – | – | – | 2 |
| Paraguay | – | 1 | – | 1 |
| Saint Vincent and the Grenadines | – | 1 | – | – |
| Middle East & North Africa | ||||
| Egypt | – | 1 | 1b | – |
| Islamic Republic of Iran | – | 1 | – | – |
| Jordan | – | 4 | 3d | 1b |
| Lebanon | – | – | 1 | 1b |
| Morocco | – | 1 | 1b | – |
| Tunisia | – | 1 | 1b | – |
| Europe & Central Asia | ||||
| Belarus | – | 1 | 1b | – |
| Bosnia and Herzegovina | – | 2 | – | 1b |
| Hungary | – | – | 1 | – |
| Romania | – | – | 1 | 1b |
| Serbia | – | – | 1 | – |
| Turkey | – | 1 | 2b | 1b |
| Ukraine | – | 1 | 3b | – |
a Regions according to the World Bank.30
b Provider only available part-time in the facility or one of the facilities.
c Provider only available part-time in two of the facilities.
d Provider only available part-time in three of the facilities.
Data sources listed in Table 1, (available at: http://www.who.int/bulletin/volumes/93/14/07-148338).
Discussion
While only a small set of metrics on the delivery of emergency care were reported consistently across facilities, we were able to draw some conclusions on the state of emergency care in low-resource settings.
First, large numbers of patients presented to health facilities seeking emergency care. While there was a wide range in annual patient volumes – from just 451 in a paediatric emergency department in Nigeria38 to 273 182 in a general emergency department in Turkey39 – they were approximately 10 times higher than the corresponding caseloads observed in primary care settings in sub-Saharan Africa and Asia.9
Second, patients seeking emergency care were generally young and free of chronic conditions. This is in contrast to the growing burden of elderly patients with multiple chronic conditions seen in the emergency departments of high-income countries.40 Therefore, interventions to decrease mortality and morbidity in emergency settings of LMICs could dramatically increase life-years saved and productivity.
Third, the mortality recorded in emergency departments in LMICs was many times higher than generally reported in high-income countries.40–42 A recent report on emergency departments in the USA documented a mean mortality within the departments of 0.04%.40
Fourth, most providers of emergency care in LMICs had no specialty training in emergency care. This observation was expected given the general shortages in human resources for health in most of these countries.43 Such shortages may be particularly pronounced in emergency settings, where the work is demanding and salaries are often poor. Most governments do not include emergency medicine in their medical education priorities.
What implications do these results have for LMICs? We made a rough calculation for Nigeria, where we identified relevant studies in 21 facilities and mean annual patient volume of 3000 and 5–7% mortality. If we assume that the approximately 1000 teaching and general hospitals44 in the country have the same mean annual patient volume and mortality, then out of the 1.6 million deaths recorded annually in Nigeria45 an estimated 10–15% occur in emergency departments. This estimate – and the observation that most emergency departments in LMICs are run by providers with no speciality training in emergency care – illustrates the opportunity to improve emergency care in LMICs. It is likely that relatively simple interventions to facilitate triage and improve patient flow, communication and the supervision of junior providers (Box 1) could lead to reductions in the mortality associated with emergency care.46–49
Box 1. Interventions to reduce mortality from medical emergencies in four low- or middle-income countries.
Rural districts in Cambodia and northern Iraq
Local paramedics and lay first responders were trained to provide field care for trauma. After the intervention, the trauma mortality decreased from 40% to 15%.46
Queen Elizabeth Hospital, Malawi
The paediatric clinic was physically restructured to streamline operations, clinical staff were trained in emergency care and triage and cooperation between the inpatient and outpatient services was improved. After the intervention, mortality within 24 hours of presentation decreased from 36% to 13%.47
Ola During Children’s Hospital, Sierra Leone
A triage unit was established in the outpatient department and the emergency and intensive care units were combined. Clinical staff were trained in emergency care and triage, with experienced nursing and medical officers required to be present at all times. Equipment and record keeping were also enhanced. After the intervention, inpatient mortality decreased from 12% to 6%.48
Kamuzu Central Hospital, Malawi
The paediatric clinic allocated senior medical staff to supervise emergency care and implemented formal triage procedures, with an emphasis on early patient treatment and stabilization before transfer to the inpatient ward. Inpatient mortality within two days of admission decreased, from 5% to 4%.49
Our data illustrate the unique cost–benefit profile of investments in emergency care. Although disease and injury prevention are key functions of all health systems, acute health problems – e.g. myocardial infarction, sepsis and trauma – continue to occur in all countries. With the same amount of resources, it is likely that more lives could be saved in a paediatric emergency facility with mortality between 12% and 21%50–52 than in paediatric primary-care clinics in similar settings – which generally see just a few critically-ill children per clinic per week (unpublished observations, 2015). There is thus a clear case for investing in emergency care in LMICs, to complement existing efforts to strengthen primary and preventive care.
Implications for policy
What is needed to strengthen emergency care in LMICs? First, a better understanding of the conditions that drive patients to seek such care is crucial. We documented high patient volumes and mortality but did not identify the diseases or the conditions that drive these metrics. While useful estimates of the burden of acute conditions may be produced in mathematical models,53 the setting of specific clinical and policy priorities remains difficult because of the scarcity of relevant data.
Second, once we have a better understanding of the burden of acute disease, interventions known to be effective in high-income settings – e.g. trauma resuscitation training – must be adapted to LMICs and critically assessed. Some effective interventions to decrease mortality in emergencies (Box 1) may only require the improved use of existing system components, with the minimal input of new material resources. However, assessing the effectiveness of such interventions by rigorous experimental or quasi-experimental methods requires additional funding. Although before-and-after comparisons may be easier, they are also vulnerable to a range of biases.54
Third, international organizations must accelerate efforts to develop consensus on the essential components of systems for emergency care. Policy-makers who wish to assess their emergency systems and set priorities for development need technical guidance. WHO’s framework on systems of trauma care is one useful model for this broad agenda.55
Finally, improvements to emergency care in LMICs will require advances in data collection. The development of a minimum set of indicators for emergency care in LMICs would facilitate research and quality improvement.21 Several actors are improving platforms for data collection in LMICs. For example, the African Federation for Emergency Medicine is building consensus around a medical chart that has been purpose-designed to capture data for clinicians, administrators and researchers in LMICs. A novel data collection platform has been implemented for trauma care in a large teaching hospital in the United Republic of Tanzania, with promising early results. The systematic integration of routine data collection into care delivery settings should help ensure that interventions are – and remain – effective.
Limitations
The most important limitation of our study is the general paucity of data on emergency care. After screening over 40 000 published reports, we identified relevant data from only 192 facilities spread across 59 LMICs. For comparison, there are about 5000 emergency departments in the USA.56 The facilities we identified were largely urban and academic – as might be expected given that our search strategy relied mainly on published reports. Broader reporting biases may also have affected our results. For example, facilities with fewer resources may be relatively unlikely to collect and publish data and facilities with exceptionally high levels of mortality may be relatively unlikely to publish those levels. Thus, our results are likely to present an optimistic view of the state of emergency care in LMICs.
Regional comparisons must be viewed with caution, given the geographical variation in facility characteristics and reporting practices. For example, emergency departments in which patients have exceptionally long lengths of stay will probably also have exceptionally high mortality – since patients who stay longer in the department are more likely to die in the department. Although a lack of relevant data prevented us from investigating this relationship, the median length of stay in our sample – albeit in the small number of facilities that reported lengths of stay – was only 7.7 hours. It therefore seems unlikely that prolonged stays alone could have accounted for the high levels of mortality that we observed.
Other limitations were our search strategy, which relied on the presence of at least one word that began with “emerg” in the title, keywords or abstract of an article. While this made a difficult search problem tractable, it may also have excluded some relevant studies. Also, lack of data standardization across facilities and countries probably biased our results. For example, standardized measures of mortality – e.g. the percentage of patients that died with 24 hours of their presentation – were seldom reported, probably because of the difficulties of following-up patients after they leave the emergency department. The maximum age for a so-called paediatric patient also varied widely across studies, from five to 19 years.57,58
Conclusion
Emergency facilities in LMICs serve a large, young patient population with high levels of critical illnesses and mortality. This suggests that emergency care should be a global health priority. The cost–benefit ratio for improvements in emergency care is likely to be highly favourable, given the high volume of patients for whom high-quality care could be the difference between life and death. There are likely to be substantial opportunities to improve care and impact outcomes, in ways that could be rigorously evaluated with manageable sample sizes.
Acknowledgements
Ziad Obermeyer and Stephanie Kayden are also affiliated with Brigham and Women’s Hospital, Boston. Other members of the Acute Care Development Consortium: Mark Bisanzo (Global Emergency Care Collaborative, Uganda), Amit Chandra (Princess Marina Hospital, Gaborone, Botswana), Cindy Y. Chang (Harvard Affiliated Emergency Medicine Residency Boston, USA), Kirsten Cohen (New Somerset Hospital, Cape Town, South Africa), Joshua J Gagne (Brigham and Women’s Hospital, Boston, USA), Eveline Hitti (American University of Beirut Medical Center, Beirut, Lebanon), Bonaventure Hollong (University of Cape Town, Cape Town, South Africa), Steven Holt (ER Consulting Inc, Johannesburg, South Africa), Vijay Kannan (University of Texas Southwestern Medical Center, Dallas, USA), Roshen Maharaj (King Dinuzulu Hospital Complex, Durban, South Africa), Roseda Marshall (John F. Kennedy Medical Center, Monrovia, Liberia), Hani Mowafi (Yale University School of Medicine, New Haven, USA), Michelle Niescierenko (Boston Children’s Hospital, Boston, USA), Maxwell Osei-Ampofo (Komfo Anokye Teaching Hospital, Kumasi, Ghana), Junaid Razzak (Aga Khan University Hospital, Karachi, Pakistan), Rasha Sawaya (Childrens National Medical Center, Washington, USA), Hendry R Sawe (Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania), Stefan Smuts (Mediclinic Southern Africa, South Africa), Sukhjit Takhar (Brigham and Women’s Hospital, Boston, USA), Eva Tovar-Hirashima (Harvard Affiliated Emergency Medicine Residency, Boston, USA), Benjamin Wachira (Aga Khan University Hospital, Nairobi, Kenya)
Funding:
This research was supported financially by a United States National Institutes of Health grant (DP5-OD012161) awarded to Brigham and Women’s Hospital, Boston.
Competing interests:
None declared.
References
- 1.Lamontagne F, Clément C, Fletcher T, Jacob ST, Fischer WA 2nd, Fowler RA. Doing today’s work superbly well–treating Ebola with current tools. N Engl J Med. 2014. October 23;371(17):1565–6. 10.1056/NEJMp1411310 [DOI] [PubMed] [Google Scholar]
- 2.Ali M, Lopez AL, Ae You Y, Eun Kim Y, Sah B, Maskery B, et al. The global burden of cholera. Bull World Health Organ. 2012. March 1;90(3):209–18. 10.2471/BLT.11.093427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coghlan B, Brennan RJ, Ngoy P, Dofara D, Otto B, Clements M, et al. Mortality in the Democratic Republic of Congo: a nationwide survey. Lancet. 2006. January 7;367(9504):44–51. 10.1016/S0140-6736(06)67923-3 [DOI] [PubMed] [Google Scholar]
- 4.Sharma D. Nepal earthquake exposes gaps in disaster preparedness. Lancet. 2015;385(9980):1819–20. Available from: http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(15)60913-8.pdf [cited 2015 May 25]. [DOI] [PubMed] [Google Scholar]
- 5.High level meeting on building resilient systems for health in Ebola-affected countries, 2014 Dec 10–11, Geneva, Switzerland. Geneva: World Health Organization; 2015. Available from: http://www.who.int/csr/resources/publications/ebola/hs-meeting.pdf?ua=1 [cited 2015 Jan 5].
- 6.Wen LS, Xu J, Steptoe AP, Sullivan AF, Walline JH, Yu X, et al. Emergency department characteristics and capabilities in Beijing, China. J Emerg Med. 2013. June;44(6):1174–1179.e4. 10.1016/j.jemermed.2012.07.083 [DOI] [PubMed] [Google Scholar]
- 7.Wen LS, Oshiomogho JI, Eluwa GI, Steptoe AP, Sullivan AF, Camargo CA Jr. Characteristics and capabilities of emergency departments in Abuja, Nigeria. Emerg Med J. 2012. October;29(10):798–801. 10.1136/emermed-2011-200695 [DOI] [PubMed] [Google Scholar]
- 8.Gawande A. Dispatch from India. N Engl J Med. 2003. December 18;349(25):2383–6. 10.1056/NEJMp038180 [DOI] [PubMed] [Google Scholar]
- 9.Das J, Hammer J. Quality of primary care in low-income countries: Facts and economics. Annu Rev Econ. 2014;6(1):525–53. [Google Scholar]
- 10.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999. J Am Coll Cardiol. 2000. December;36(7):2056–63. 10.1016/S0735-1097(00)00996-7 [DOI] [PubMed] [Google Scholar]
- 11.Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012. January 5;366(1):54–63. 10.1056/NEJMra1112570 [DOI] [PubMed] [Google Scholar]
- 12.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000. April 19;283(15):1990–4. 10.1001/jama.283.15.1990 [DOI] [PubMed] [Google Scholar]
- 13.Riopelle RJ, Howse DC, Bolton C, Elson S, Groll DL, Holtom D, et al. Regional access to acute ischemic stroke intervention. Stroke. 2001. March;32(3):652–5. 10.1161/01.STR.32.3.652 [DOI] [PubMed] [Google Scholar]
- 14.Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014. March;42(3):625–31. 10.1097/CCM.0000000000000026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyle AA, Ahmed V, Palmer CR, Bennett TJ, Robinson SM. Reductions in hospital admissions and mortality rates observed after integrating emergency care: a natural experiment. BMJ Open. 2012;2(4):e000930. 10.1136/bmjopen-2012-000930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kellermann AL, Hsia RY, Yeh C, Morganti KG. Emergency care: then, now, and next. Health Aff (Millwood). 2013. December;32(12):2069–74. 10.1377/hlthaff.2013.0683 [DOI] [PubMed] [Google Scholar]
- 17.Anderson PD, Suter RE, Mulligan T, Bodiwala G, Razzak JA, Mock C; International Federation for Emergency Medicine (IFEM) Task Force on Access and Availability of Emergency Care. World Health Assembly Resolution 60.22 and its importance as a health care policy tool for improving emergency care access and availability globally. Ann Emerg Med. 2012. July;60(1):35–44.e3. 10.1016/j.annemergmed.2011.10.018 [DOI] [PubMed] [Google Scholar]
- 18.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–5. [PMC free article] [PubMed] [Google Scholar]
- 19.Hsia R, Razzak J, Tsai AC, Hirshon JM. Placing emergency care on the global agenda. Ann Emerg Med. 2010. August;56(2):142–9. 10.1016/j.annemergmed.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 20.Hsia RY, Carr BG. Measuring emergency care systems: the path forward. Ann Emerg Med. 2011. September;58(3):267–9. 10.1016/j.annemergmed.2011.03.048 [DOI] [PubMed] [Google Scholar]
- 21.Mowafi H, Dworkis D, Bisanzo M, Hansoti B, Seidenberg P, Obermeyer Z, et al. Making recording and analysis of chief complaint a priority for global emergency care research in low-income countries. Acad Emerg Med. 2013. December;20(12):1241–5. 10.1111/acem.12262 [DOI] [PubMed] [Google Scholar]
- 22.Robison J, Ahmed Z, Durand C, Nosek C, Namathanga A, Milazi R, et al. Implementation of ETAT (Emergency Triage Assessment And Treatment) in a central hospital in Malawi. Arch Dis Child. 2011;96 Suppl 1:A74–5. 10.1136/adc.2011.212563.174 [DOI] [Google Scholar]
- 23.Ahmad S, Ellis JC, Kamwendo H, Molyneux EM. Impact of HIV infection and exposure on survival in critically ill children who attend a paediatric emergency department in a resource-constrained setting. Emerg Med J. 2010. October;27(10):746–9. 10.1136/emj.2009.085191 [DOI] [PubMed] [Google Scholar]
- 24.Fournier P, Dumont A, Tourigny C, Dunkley G, Dramé S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural Mali. Bull World Health Organ. 2009. January;87(1):30–8. 10.2471/BLT.07.047076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mock CN, Jurkovich GJ, nii-Amon-Kotei D, Arreola-Risa C, Maier RV. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998. May;44(5):804–14. 10.1097/00005373-199805000-00011 [DOI] [PubMed] [Google Scholar]
- 26.Mock CN, Tiska M, Adu-Ampofo M, Boakye G. Improvements in prehospital trauma care in an African country with no formal emergency medical services. J Trauma. 2002. July;53(1):90–7. 10.1097/00005373-200207000-00018 [DOI] [PubMed] [Google Scholar]
- 27.Creamer KM, Edwards MJ, Shields CH, Thompson MW, Yu CE, Adelman W. Pediatric wartime admissions to US military combat support hospitals in Afghanistan and Iraq: learning from the first 2,000 admissions. J Trauma. 2009. October;67(4):762–8. 10.1097/TA.0b013e31818b1e15 [DOI] [PubMed] [Google Scholar]
- 28.Wen LS, Geduld HI, Nagurney JT, Wallis LA. Africa’s first emergency medicine training program at the University of Cape Town/Stellenbosch University: history, progress, and lessons learned. Acad Emerg Med. 2011. August;18(8):868–71. 10.1111/j.1553-2712.2011.01131.x [DOI] [PubMed] [Google Scholar]
- 29.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009. July 21;6(7):e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Data: country and lending groups [Internet]. Washington: World Bank; 2013. Available from: http://data.worldbank.org/about/country-classifications/country-and-lending-groups [cited 2013 Aug 20].
- 31.Global health library [Internet]. Geneva: World Health Organization; 2014. Available from: http://www.globalhealthlibrary.net/php/index.php [cited 2014 May 1].
- 32.Peres RR, Lima SBS, de Souza Magnago TSB, Shardong AC, da Silva Ceron MD, Prochnow A, et al. Perfil clinico-epidemiologico dos pacientes internados no pronto-socorro de um hospital universitario. Rev Saúde (Santa Maria). 2013;39(1):77–86. Available from: http://cascavel.ufsm.br/revistas/ojs-2.2.2/index.php/revistasaude/article/view/5518 [cited 2014 Jan 10]. Portuguese.
- 33.Ribeiro RCHM, Rodrigues CC, Canova JCM, Rodrigues CDS, Cesarino CB, Júnior OLS. Stay and outcome of the clinical and surgical patient in the emergency service. Rev Enferm (Lisboa). 2013;7(9):5426–32. Available from: http://www.revista.ufpe.br/revistaenfermagem/index.php/revista/article/view/4886/pdf_3390 [cited 2014 Jan 10]. [Google Scholar]
- 34.Rehmani R. Emergency section and overcrowding in a university hospital of Karachi, Pakistan. J Pak Med Assoc. 2004. May;54(5):233–7.http://Error! Hyperlink reference not valid. [PubMed] [Google Scholar]
- 35.Gaitan M, Mendez W, Sirker NE, Green GB. Growing pains: status of emergency medicine in Nicaragua. Ann Emerg Med. 1998. March;31(3):402–5. 10.1016/S0196-0644(98)70355-5 [DOI] [PubMed] [Google Scholar]
- 36.Tiemeier K, Bisanzo M, Dreifuss B, Ward KC.; Global Emergency Care Collaborative. Ward KC. The effect of geography and demography on outcomes of emergency department patients in rural Uganda. Ann Emerg Med. 2013;62(4):S99–99. 10.1016/j.annemergmed.2013.07.096 [DOI] [Google Scholar]
- 37.Mabiala-Babela JR, Senga P. Consultations de nuit aux urgences pédiatriques du CHU de Brazzaville, Congo. (Nighttime attendance at the Pediatric Emergency Room of the University Hospital Centre in Brazzaville, Congo). Med Trop. 2009. June;69(3):281–5. [PubMed] [Google Scholar]
- 38.Duru C, Peterside O, Akinbami F. Pattern and outcome of admissions as seen in the paediatric emergency ward of the Niger Delta University Teaching Hospital Bayelsa State, Nigeria. Niger J Paediatr. 2013;40(3):232–7. Available from http://www.ajol.info/index.php/njp/article/view/89985 [cited 2015 May 2]. [Google Scholar]
- 39.Eroglu SE, Toprak SN, Urgan O, Onur OE, Denizbasi A, Akoglu H, et al. Evaluation of non-urgent visits to a busy urban emergency department. Saudi Med J. 2012. September;33(9):967–72.http:// [PubMed] [Google Scholar]
- 40.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010. August 11;304(6):664–70. 10.1001/jama.2010.1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baker M, Clancy M. Can mortality rates for patients who die within the emergency department, within 30 days of discharge from the emergency department, or within 30 days of admission from the emergency department be easily measured? Emerg Med J. 2006. August;23(8):601–3. 10.1136/emj.2005.028134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Health, United States, 2012: with special feature on emergency care. Hyattsville: National Center for Health Statistics; 2013. Available from: http://www.cdc.gov/nchs/data/hus/hus12.pdf [cited 2014 Jan 15]. [PubMed]
- 43.Crisp N, Chen L. Global supply of health professionals. N Engl J Med. 2014. March 6;370(10):950–7. 10.1056/NEJMra1111610 [DOI] [PubMed] [Google Scholar]
- 44.Nwakeze NM, Kandala N-B. The spatial distribution of health establishments in Nigeria. Afr Popul Stud. 2011;25(2):680–96.
- 45.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012. December 15;380(9859):2095–128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Husum H, Gilbert M, Wisborg T, Van Heng Y, Murad M. Rural prehospital trauma systems improve trauma outcome in low-income countries: a prospective study from North Iraq and Cambodia. J Trauma. 2003. June;54(6):1188–96. 10.1097/01.TA.0000073609.12530.19 [DOI] [PubMed] [Google Scholar]
- 47.Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ. 2006. April;84(4):314–9. 10.2471/BLT.04.019505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Clark M, Spry E, Daoh K, Baion D, Skordis-Worrall J. Reductions in inpatient mortality following interventions to improve emergency hospital care in Freetown, Sierra Leone. PLoS ONE. 2012;7(9):e41458. 10.1371/journal.pone.0041458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robison JA, Ahmad ZP, Nosek CA, Durand C, Namathanga A, Milazi R, et al. Decreased pediatric hospital mortality after an intervention to improve emergency care in Lilongwe, Malawi. Pediatrics. 2012. September;130(3):e676–82. 10.1542/peds.2012-0026 [DOI] [PubMed] [Google Scholar]
- 50.Okolo SN, Ogbonna C, Bode-Thomas F. Healthcare service auditing and intervention in an emergency paediatric unit. Niger J Paediatr. 2002;29(3):71–4. 10.4314/njp.v29i3.12026 [DOI] [Google Scholar]
- 51.Muluneh D, Shimelis D, Benti D. Analysis of admissions to the pediatric emergency ward of Tikur Anbessa Hospital in Addis Ababa, Ethiopia. Ethiopian J Health Dev. 2007;21(1):48–53. Available from: http://www.ajol.info/index.php/ejhd/article/view/10031/2283 [cited 2015 May 2].
- 52.Bamgboye EA, Familusi JB. Mortality pattern at a children’s emergency ward, University College Hospital, Ibadan, Nigeria. Afr J Med Med Sci. 1990. June;19(2):127–32.http:// [PubMed] [Google Scholar]
- 53.Kobusingye OC, Hyder AA, Bishai D, Joshipura M, Romero Hicks E, Mock C. Emergency Medical Services. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al. , editors. Disease control priorities in developing countries. 2nd ed. Washington: World Bank; 2006. pp. 1261–79. [Google Scholar]
- 54.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014. December 10;312(22):2401–2. 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- 55.Guidelines for essential trauma care. Geneva: World Health Organization; 2004. Available from: http://whqlibdoc.who.int/publications/2004/9241546409.pdf?ua=1 [cited 2015 May 11].
- 56.Muelleman RL, Sullivan AF, Espinola JA, Ginde AA, Wadman MC, Camargo CA Jr. Distribution of emergency departments according to annual visit volume and urban-rural status: implications for access and staffing. Acad Emerg Med. 2010. December;17(12):1390–7. 10.1111/j.1553-2712.2010.00924.x [DOI] [PubMed] [Google Scholar]
- 57.Miranda NA, Rezende BD, Oliveira J de SF, Franco MBS, Kawata LS. Caracterização de crianças atendidas no pronto-socorro de um hospital universitário. Gestão Saude. 2012;4(1):1631–45. [Portuguese.] [Google Scholar]
- 58.Peixoto B de V, Piazzetta E, Rischini FA, Guimarães MN, Cuziol M, Lodo PB, et al. [The harsh reality of children and youth emergency care showing the health status of a city.] Rev Paul Pediatr. 2013. June;31(2):231–6. Portuguese. 10.1590/S0103-05822013000200015 [DOI] [PubMed] [Google Scholar]


