Abstract
Objective
To systematically identify factors associated with participation in social and community activities for adult wheelchair users (WCUs).
Data Sources
Pubmed/MEDLINE, CINAHL, PsycINFO, EMBASE.
Study Selection
Quantitative and qualitative peer-reviewed publications were included which were written in English, reported original research, and investigated factors associated with social and community participation in adult WCUs.
Data Extraction
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were used; factors were organized using the International Classification of Functioning, Disability and Health (ICF).
Data Synthesis
Thirty-five studies were selected: two of power WCUs, 10 of manual WCUs, and 23 of both. Six qualitative studies, ranging in quality from 8/10 to 9/10, and 29 quantitative studies were included, ranging in quality from 4/15 to 11/15. Fifteen Body Function, four Activity, five Participation, 15 Environmental, and 14 Personal Factors were found to be associated with social and community participation.
Conclusions
Social and community participation of wheelchair users is associated with factors from all ICF domains. Wheelchair factors, accessibility, skills with wheelchair use, pain, finances, and education are modifiable factors frequently reported to be associated with participation. Experimental research focusing on modifiable factors is needed to further our understanding of factors influencing participation among wheelchair users.
Keywords: Wheelchairs, Social Participation, Community Integration, Leisure Activities, Experimental Research, Systematic Review
The World Health Organization (WHO) identifies participation in social and community activities as a fundamental right[1]. Participation is defined in the International Classification of Functioning, Disability and Health (ICF) as an individual’s involvement in life situations[2]. There is a general consensus that participation, specific to social activities and community involvement, is an important rehabilitation focus due to its association with subjective quality of life, health[3] and important clinical outcomes. For example, Chang et al. report participation in social and community activities has the strongest association with quality of life in individuals with spinal cord injuries[4]. In addition, social and community participation is shown to be linked to experiences of motivation, competency and self-efficacy, all of which play a vital role in rehabilitation[5] because of their positive effect on health status, and psychological and physical functioning[6]. Furthermore, severity of depressive symptoms is also reported as a factor associated with participation in social roles in individuals who are post stroke[7]. In fact, in a recent systematic review of psychosocial interventions for depressive symptoms, the authors report a statistically significant association with participation in social activities and reduction of depressive symptoms[8]. For these reasons, improving social and community participation is an important clinical focus, especially for those individuals who may be at risk for having less than optimal participation.
Individuals with limited mobility are shown to have reduced opportunity for participation in social and community activities[9, 10]. Fortunately, in many instances, individuals with mobility limitations are prescribed wheelchairs as a means to facilitate both mobility and participation. However, despite evidence that simply acquiring a wheelchair has positive participation implications in individuals with mobility limitations[11–14], research also shows wheelchair users experience lower levels of participation relative to ambulatory individuals[15]. For example, Best and Miller report the rate of physical activity participation of older, community-dwelling wheelchair users as 8.3%, and the rate of age matched ambulatory individuals as 88.9%[16].
In the United States, it is estimated there are 3.6 million wheelchair users[17], with over half above the age of 65[17, 18]. Recent estimates also indicate 360 000 wheelchair users in France[19], and between 640 000 and 710 000 wheelchair users in the United Kingdom[12]. The proportion of individuals requiring a wheelchair increases with age[18, 20], as do the areas of life in which participation is restricted[21]. Chronic conditions such as stroke, and osteo and rheumatoid arthritis are leading causes of activity limitations and wheelchair use. They also increase in prevalence with aging[18, 20, 22]. Therefore, there may be a substantial increase in the number of wheelchair users with participation restrictions resulting from population aging.
Given the potential growth in the number of wheelchair users, and concerns regarding their lowered participation, research in this area has increased to a point where there is now a body of evidence on factors associated with the participation in this population. Although one recent review investigated the impact of powered wheelchairs on activity engagement in adults[23], to our knowledge, there is no published study which has systematically reviewed and consolidated the evidence on all the factors reported to be associated with participation among wheelchair users. Such work will contribute to a better clinical and research understanding of the participation of wheelchair users, and present a platform to advance research in the area.
Clinicians may address the modifiable factors using participation-enhancing interventions, and use a combination of factors to identify those wheelchair users at risk of having less than optimal participation, and who may benefit the most from participation enhancing clinical intervention. Therefore, the purpose of this study is to systematically review both the quantitative and qualitative literature to identify the factors associated with social and community participation in adult wheelchair users, and to organize the factors using the ICF[2] conceptual framework.
Methods
Data Sources
We searched The Cochrane Library for existing relevant reviews, and the PubMed/Medline, EmBase, PsycInfo and CINAHL databases for published articles using keyword and medical subject headings up to November, 2014 (i.e. no lower limit was placed on the search strategy). Search terms were identified through a review of relevant literature and MESH/Subject Headings. Search terms and limits can be found in table 1. Truncation and wildcards were used to promote maximal inclusion (i.e. wheel* mobility includes both wheelchair and wheeled mobility, and associated terms such as wheeled mobility device).
Table 1.
Keywords and Search Limits
| Wheelchair Terms | Participation Terms | |
|---|---|---|
|
| ||
| Keywords | Wheelchairs Wheelchair* Wheelchair user Wheel* Mobility Manual wheelchair* Power wheelchair* |
Participation Community participation Community living Community Integration Social participation Work participation Personal role Social role Instrumental Activities of Daily Living Leisure activities Leisure activit* participation Physical activit* participation |
|
| ||
| Search Limits | Human, English Language, Peer-Reviewed | |
Inclusion and Exclusion Criteria
We collected and reviewed quantitative and qualitative peer-reviewed publications if they were written in English, reported the results of original research, and investigated factors associated with participation in social or community activities, in adult (≥18) wheelchair users (power or manual wheelchairs). For the purposes of this review, we focus on social and community participation, in the following ICF participation domains: community, social and civic life (including community life, political life and citizenship, and recreation and leisure), interpersonal interactions and relationships, and major life areas (including education, and work and employment). Only papers using clearly defined social and/or community participation measures[24–26] were included for review, or qualitative research which focused on participation in social and community activities. We did not include concepts such as frequency of exercise, number of locations visited or mobility, as these measures are more reflective of the ICF definition of activity (‘execution of a task or action’) and do not reflect the complexity inherent in a life situation [27]. Wheelchair users include individuals who use a manual or powered wheelchair for participation in daily activities. Studies reporting on scooter use were not included as they are typically used only for outdoor mobility, and do not reflect the variety of environments in with social and community participation occur. While some scooters may also be wheelchair users, the majority will also be ambulatory, and may not experience the same participation limitations as those who are exclusively manual or power wheelchair users. Conference proceedings, dissertations and/or case studies were excluded from review.
Study Selection
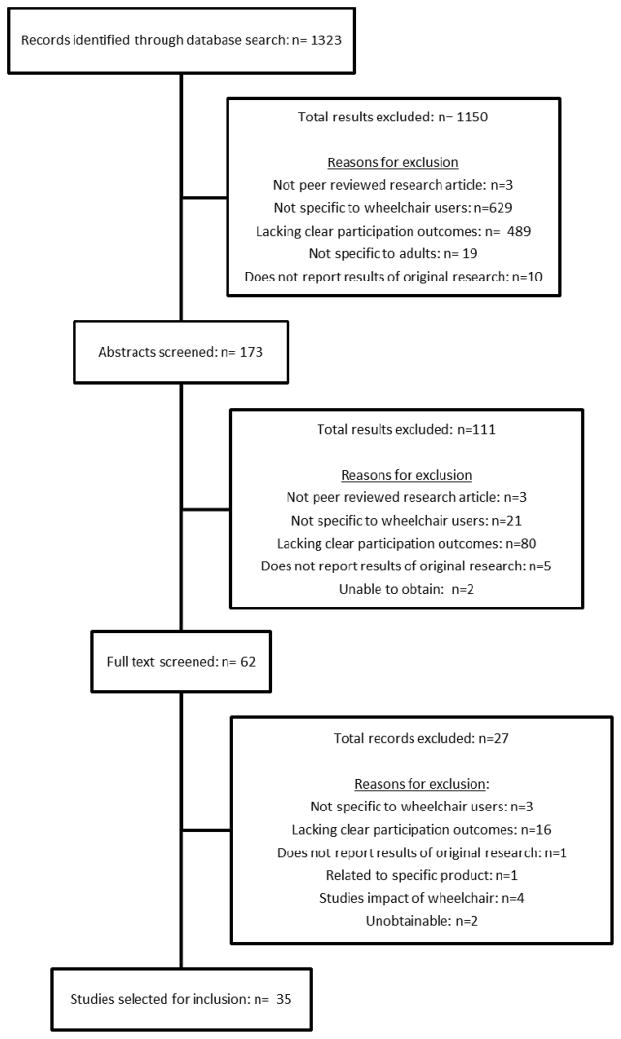
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[28]. Two investigators (EMS and BMS) independently screened all titles resulting from the electronic searches. Those titles of interest were imported into a reference manager, and their abstracts reviewed. After excluding papers not meeting the review’s inclusion criteria, we independently reviewed the full papers of all remaining studies. Disagreements on papers to exclude at all stages were resolved through discussion with a third investigator (WCM). See figure 1 for an account of the selection process, which details the number of papers included/excluded at each step, and reasons for the exclusion of papers.
Figure 1.
PRISMA Flow Diagram
Data Extraction/Synthesis
Data related to study year, country, sample size, design, population, outcomes, and results were extracted into a study specific data extraction form. We extracted data separately for manual and power wheelchair users where possible, because different factors may affect one group of users differently from the other. In quantitative studies, factors with a statistically significant association (i.e. p <0.05) with participation were reported, including statistical values (odds ratios, regression coefficients, correlation) where available. In qualitative studies, factors associated with participation were those which were identified thematically by the study authors. Once factors were identified, we classified these according to ICF domain by mapping individual factors to the most relevant ICF code[29]. In order to guide future experimental research, and focus for clinical practice, we also categorized factors as either modifiable (i.e. responsive to rehabilitation (OT/PT) intervention) or non-modifiable.
Methodological Quality Assessment
We assessed the methodological quality of quantitative studies using criteria adapted from Chen and Winstein’s Criteria for Rating Quality of Study Methods[30] (Table 2). Each item was scored using: yes (1) if the criterion was met or no (0) if it wasn’t. The total possible scores range from 0 to 15. Any randomized controlled trials were also assessed using the PEDro scale[31]. Methodological quality of qualitative studies was assessed using the Critical Appraisal Skills Program Qualitative Research Checklist[32]. Each item was scored using: yes (1) if the criterion was met or no (0) if it wasn’t, with total possible scores ranging from 0 to 10.
Table 2. Criteria for Rating Methodological Quality of Multivariate Studies.
The rating criteria for methodological quality is adapted from Chen and Winstein.
| Criteria | Each item received a score of 1 if: | |
|---|---|---|
|
| ||
| Internal validity | ||
| 1 2 |
|
Outcome measures and predictor measures were precisely defined. |
| 3 4 |
|
Studies tested the reliability and validity of measures (outcome and predictor) or referenced the literature on the clinimetric properties of each measure. |
| 5 |
|
Blinded testers were specified. |
| 6 |
|
Measures of potential predictors were acquired prior to the measurement of the primary outcome. |
| 7 |
|
Dropouts during observation specified, characteristics of dropouts did not influence conclusion. |
|
| ||
| Statistical validity | ||
| 8 |
|
Rationale for statistical approaches was specified, the relationship between outcome measures and predictor measures was tested for statistical significance. |
| 9 |
|
At least 10 subjects for each predictor variable examined. |
| 10 |
|
Interaction between two or more predictor measures was tested in the prediction model. |
|
| ||
| External validity | ||
| 11 |
|
The study identified if the sample was comprised of manual or power wheelchair users, or both. If both, results were stratified by wheelchair type. |
| 12 |
|
Relevant subject characteristics (eg, age, sex, diagnosis) were specified for patient selection. |
| 13 |
|
Information on rehabilitation treatment was reported. |
| 14 |
|
Prediction models were validated in a second independent group of wheelchair users. |
| 15 |
|
Minimal clinically important differences were considered. |
Results
The electronic database search resulted in 1323 papers. Of these papers, 173 abstracts were reviewed, and subsequently 62 articles were selected to read in their entirety. After reading these papers, 27 were excluded, resulting in 35 studies included for inclusion. The PRISMA Flow Diagram (Figure 1) identifies the numbers of papers excluded at each stage, and reasons for their exclusion.
Description of Included Studies
Twenty-nine studies were quantitative, including 28 cross-sectional designs, and one single-group pre-post study. One study was identified as mixed methods, employing a longitudinal survey with qualitative and quantitative analyses. Of the cross-sectional studies, five were secondary analyses, each using data from large national databases. Fourteen studies used multiple regression analyses. Six studies were qualitative, including five semi-structured, ethnographic or in-depth interviews, and one focus group. The number of wheelchair users in each study ranged from 6[33] to 3726[34]. Seventeen studies were specific to individuals with spinal cord injury and two studies investigated wheelchair users with stroke. The remaining 16 studies were not specific to diagnosis, and included wheelchair users in general. The mean age of the samples ranged from 36.2[35] to 84.0 [36] years. Study specific details and results can be found in table 3.
Table 3.
Study Details and Results
| Author, year, country, sample size. | Study Design; Methodological quality: Quantitative/15, PEDro/11, Qualitative/10 | Population; mean age; sex; Wheelchair (w/c) type (manual/power/ both) | Outcome measure* | Outcome | Reported factors that are statistically significant, or reported as important factors in qualitative studies | Statistic (where available) |
|---|---|---|---|---|---|---|
| Manual and Power Wheelchairs (Quantitative) | ||||||
| Quantitative Studies with Multivariate Analyses | ||||||
| Collins, D., et al., 2006, USA, N=152 | Quantitative (multivariate): Cross-sectional; 9/15 | Wheelchair users; Mean age = 44.4; Sex: 61.8% female; | CHART | Community participation and integration | Depression (fewer symptoms) Sex (female) Marital status (yes) |
β= −0.52 β=9.11 β=12.38 R2=0.26 |
| Ginis, K.A., et al., 2010, Canada, N=695 | Quantitative (multivariate): Cross-Sectional; 10/15 | Spinal Cord injury; Mean age: 47.1; Sex: n = 164 female; | PARA-SCI | Leisure Time Physical Activity | Age Sex (male) Years Since Injury Wheelchair factors Level of Injury Paraplegia Quadriplegia |
β-0.12 β=0.09 β= −0.12 β= −0.14 β= −0.11 β= −0.12 R2=0.09 |
| Liang, H., et al., 2008, USA, N=131 | Quantitative (multivariate): Cross-sectional; 9/15 | Spinal cord injury; Mean age: 39.1; Sex: n= 131 male | LTPA | Physical Activity Participation | Environmental – Neighborhood crime rate | OR 0.14 (95%CI 0.04–0.49) |
| Mortenson, W.B., et al., 2012, Canada, N=264 | Quantitative (multivariate): Cross-sectional; 9/15 | Long term care residents (n= 146 self-report, n= 118 proxy); Mean age = 84; Sex: 69% female | LLDI: Disability Component | Social and Community Participation Frequency | Cognition Depression Mobility Accessibility - Perceived Barriers Wheelchair Skills |
β =0.29 β =−0.23 β =0.20 β =0.20 β =0.18 R2 = 0.53 |
| Norweg, A., et al., 2011, USA, N=3726 | Quantitative (multivariate): Cross-sectional, Secondary analysis; 9/15 | Spinal Cord Injury; Mean age = not given; Sex: n = 808 female | Employment; CHART – Mobility, Occupation and Social Integration subscales. | Employment Total Community Reintegration Social Integration Occupation |
Driving | β=0.62, OR 1.85 (1.50– 2.29) β=0.20 β=0.13 β=0.13 |
| Tsai, I-H., et al., 2014, USA, N=2986 | Quantitative (multivariate): Cross-sectional, secondary analysis; 9/15 | Spinal Cord Injury; Mean age = 40.0; Sex = 19.1% female | CHART-SF; Employment | Social participation Employment |
Use of modified vehicle | β= 20.0 OR 3.14 |
| Warner, G., et al., 2010, Canada/USA N=123 | Quantitative (multivariate): Cross Sectional; 7/15 | Non institutionalized wheelchair users; Mean age = 64.8; Sex: 8% female | Physical activity and leisure participation; Questionnaire, | Physical activity and leisure participation (LTPA hours per week) |
Aged 26–64 Level of education Level of assistance Over 64 Living alone |
β= −0.42 β= −0.80 R2 = 0.34 β= −0.27 R2 = 0.11 |
| Additional Quantitative Studies | ||||||
| Akyuz et al. (2014), Turkey, N=100 | Quantitative: Survey; 4/15 | Spinal Cord Injury; Mean age = 37.9; Sex = 30% female | Barrier to Social Integration | Social Integration | Accessibility | % reported 48% |
| Anneken et al. (2010), Germany, N=277 | Quantitative: Cross-Sectional Survey; 4/15 | Spinal Cord Injury; Mean age = 41.8; Sex: = 21% female | Employment; QoL Feedback questionnaire | Employment frequency | Involvement in Sports | Reported as significant, no values provided. |
| Best, K.L. & Miller, W.C. 2011, Canada, N=8301 (149 wheelchair users) | Quantitative: Survey; 5/15 | Older Adults; Mean age = 76.4; Sex: = 52.6% female | Canadian Community Health Survey |
Physical Activity Leisure Participation |
Tobacco Use BMI Sex (male) Level of Education Alcohol Use Tobacco Use BMI Sex (male) Level of Education Alcohol Use |
OR 1.95 1.07 0.72 0.62 0.74 1.81 1.04 1.16 0.61 0.54 |
| Carlson, D., & Myklebust, J., 2002, USA, N=39, 137 | Quantitative: Survey; 5/15 | Wheelchair users; Mean age = not given Sex: n =22,088 female | National Health Institute Survey – Disability | Social participation and community integration | Sex (female) Wheelchair factors Age Employment Level of Education Physical health status |
Reported as significant, no values provided. |
| Chaves, E.S., et al., 2004, USA, N=70 | Quantitative: Cross-sectional questionnaire; 4/15 | Spinal Cord Injury; Mean age = 41; Sex: n = 15 female | PARTS/M | Participation in and outside home Transportation |
Wheelchair factors Fatigue Accessibility - Physical Environment Pain |
Reported as significant, no values provided. |
| Cooper, R.A., et al., 2011, USA N=16 | Quantitative: Cross-sectional; 7/15 | Wheelchair users; Mean age = 49.13; Sex: n = 15 female | PARTS/M |
Manual Community Transportation Socialization Power Community integration/leisure |
Average Speed Travelled |
Rs= 0.84 Rs= 0.77 Rs= −0.64 |
| Leung, V., et al., 2005, Canada, N=5395 | Quantitative: Cross-Sectional; 7/15 | Older adults, Mean age >65; Sex: Not given | Canadian Study of Health and Aging | Recreation and environment Housing Finances Religion |
Pain | chi2=88.0 chi2=16.9 chi2=31.7 chi2=11.1 |
| McVeigh, S.A., et al, 2009, Canada, N=90 | Quantitative: Cross-sectional; 6/15 | Spinal Cord Injury; Mean age = not given; Sex: n = 19 female | CIQ | Community Integration | Involvement in sports | OR 1.36 (95% CI 0.09–1.45) |
| Meyers, A.R., 2002, USA, N=25 | Mixed Methods: Longitudinal Survey; 4/15 | Experienced wheelchair users; Mean age = 47; Sex: n = 13 female | Questionnaire | Community Participation | Age (higher age barrier to participation) | Reported as significant, no values provided |
| Pluym, S., et al., 1997, Netherlands, N=44 | Quantitative: Survey; 4/15 | Wheelchair users; Mean age = 38; Sex: n = 17 female | Self-administered semi-structured questionnaire - |
Work Participation Leisure Participation Relationships and Social Participation |
Accessibility Physical health status Accessibility Dependence on others Finances Accessibility Physical health status |
% reported 54.1% 51.4% 70.5% 59.1% 56.8% 77.3% 59.0% |
| Tasiemski, T., et al., 2000, Poland/UK, N=5 | Quantitative: Postal Survey; 4/15 | Spinal Cord Injury (C5 or lower); Mean age = not given; Sex: n = 9 female | Postal Survey | Participation in Sports, employment | Accessibility Lack of opportunity Finances Fear of injury Transportation access Suitable housing Societal attitudes Dependence on others |
Correlations not reported. |
| Qualitative Studies | ||||||
| Barker, D., et al., 2006, Canada, N=10 | Qualitative: Interview; 9/10 | Stroke; Mean age = 75.5; Sex: n = 2 female | Interviews | Social/community participation | Wheelchair factors Physical Limitations Urinary incontinence Caregiver concerns Accessibility-environmental Psychological factors Comorbidities Societal attitudes |
|
| Hjelle, K., et al., 2011, Norway, N=6 | Qualitative: Focus Group; 9/10 | Persons with Disabilities; Mean age = 48.5; Sex: n = 3 female | Focus Groups | Community and Social Participation |
Being engaged Being a member of society Interacting as a citizen |
|
| Levins, S.M., et al., 2004, Canada, N=8 | Qualitative: Ethnographic Interviews; 9/10 | Spinal Cord Injury; Mean age = 42; Sex: n = 3 female | Interview, thematic analysis | Physical activity participation | Loss of identity Societal attitudes Environmental Characteristics |
|
| Reid, D., et al., 2003, Canada N = 11 | Qualitative: Interview; 8/10 | Wheelchair users engaged in homemaking and parenting; Mean age = 42; Sex: female | Social and home participation; Interviews | Home participation Social participation |
Accessibility - Living Spaces Social Environment Climate Finances |
|
| Rudman, D.L., et al., 2006, Canada, N=16/15 | Qualitative: Interview; 9/10 | Stroke survivors (16) Mean age = 76 Sex: n= 4 female Caregivers (15); Mean age = 68.1; Sex: n = 13 female |
Interviews | Leisure and Social participation, Community Integration | Accessibility – environment Transportation Social Environment Fatigue Motor Involvement Vision Motivation Incontinence Caregiver concerns Personality |
|
| Manual Wheelchair Users Only | ||||||
| Quantitative Studies with Multivariate Analyses | ||||||
| Hosseini, S., et al., 2012, USA, N=214 | Quantitative (multivariate): Cross-sectional; 11/15 | Spinal Cord Injury; Mean age = 38.8; Sex: n = 44 female | CHART total and sub scores | Community participation Mobility Occupation Physical Independence |
Wheelchair skills |
R2= 0.12 R2= 0.05 R2= 0.04 R2= 0.03 |
| Kilkens, O., et al., 2005, Netherland, N=81 | Quantitative (multivariate): Cross-sectional; 10/15 | Spinal Cord Injury; Mean age = 39.3; Sex: n = 25 female | SIPSOC | Impact on Social participation | Age Wheelchair skills Physical Strain |
Rs =0.34 Rs= −0.49 Rs= 0.38 R2=0.34 |
| Phang, S.H., et al., 2012, Canada, N=54 | Quantitative (multivariate): Cross-sectional; 10/15 | Spinal Cord Injury; Mean age = 47.7; Sex: n = 11 female | PARA-SCI | Leisure time physical activity | Wheelchair Skills | β=0.27, R2=0.48 |
| Sakakibara B.M., et al., 2013, Canada, N=124 | Quantitative (multivariate) : Cross-sectional; 10/15 | Community living wheelchair users; Mean age = 59; Sex: n = 50 female | LLDI | Social and personal role participation | Confidence | β=0.44 R2=0.41 |
| Sakakibara, B., et al., 2013, Canada, N=54 | Quantitative (multivariate): Cross-sectional; 10/15 | Community living wheelchair users; Mean age = 59; Sex: n = 19 female | LLDI | Social and personal role participation | Confidence (stronger for men than women) | β=0.83 R2= 0.10 |
| Shechtman, O., et al., 2003, USA, N=13 | Quantitative (multivariate): Cross-sectional; 8/15 | Wheelchair and non-wheelchair users; Mean age = 36.2; Sex: n = 4 female; | CHART | Community participation | Grip strength | r=0.55 R2=0.31 |
| Additional Quantitative Studies | ||||||
| deGroot, S., et al., 2011, USA, N=109 | Quantitative: Cross-sectional; 7/15 | Spinal cord injury; Mean age = 40.4; Sex = 27% female; | PASIPD, SIPSOC | Physical activity participation Social participation |
Satisfaction with: dimensions of wheelchair Satisfaction with simplicity of use, durability, comfort |
Reported as significant, no values provided. |
| Gutierrez, D., et al., 2007, USA, N=80 | Quantitative: Cross-Sectional; 8/15 | Spinal Cord Injury; Mean age=44.7; Sex: n = 22 female; | SQLS, PASIPD, Community Activities Checklist | Physical activity participation | Shoulder Pain | r=−0.42 |
| Kemp, B.J., et al., 2011, USA, N=58 | Quantitative: Randomized Control Trial; 10/15, PEDro:6 | Spinal Cord Injury; Mean age = 45; Sex: Not given; | SII | Social participation | Pain – Decreased Shoulder pain (following 12 week intervention) | (F(1, 25) = 28.78 |
| Oyster, M., et al., 2011, USA, N=132 | Quantitative: Cross-sectional; 8/15 | Spinal Cord Injury; Mean age = 39.38; Sex: n= 26 female; | CHART short form | Social Integration Occupation Community participation |
Race-Caucasian Level of education Marital Status Employment Finances – Income Wheelchair type Years since injury Mobility |
Values not provided R=0.18 R=0.25–0.39 |
| Power Wheelchair Users Only | ||||||
| Quantitative Studies with Multivariate Analyses | ||||||
| Hoenig, H., et al., 2003, USA, N=153 | Quantitative (multivariate): Cross-Sectional; 8/15 | New wheelchair users; Mean age .75; Sex: male | Self-reported nonmedical visits. | Social participation | #Comorbidities Mobility Accessibility - Home |
β= −0.14 β= −0.28 β= −0.32 |
| Qualitative Studies | ||||||
| Blach-Rosen, et al., 2012, Denmark, N=9 | Qualitative: Interview; 9/10 | Power wheelchair users; Mean age = 52; Sex: n = 4 female | Interview | Social participation and community integration | Accessibility – built environment Wheelchair factors Psychological– Being in wheelchair Societal Attitudes |
|
PARA-SCI: Physical Activity Recall Assessment for People with Spinal Cord Injury, CHART: Craig Handicap Assessment and Reporting Technique, LLFDI: Late Life Function and Disability Instrument, LTPA: Leisure Time Physical Activity, PARTS/M: Participation Survey/Mobility Questionnaire, SIPSOC: Sickness Impact Profile, PASIPD: Physical Activity Scale for Individuals with Physical Disabilities, SQLS: Subjective Quality of Life Scale, SII: Social Integration Index
Results by Wheelchair Type
A total of 55 factors were identified from 33 included studies. Of those, 19 were identified from studies employing multivariable analyses. The following results are presented by wheelchair type, privileging those factors which were identified in multivariable studies, as they offer a more robust analysis than those identifying bivariable associations.
Both Manual and Power Wheelchair Users
In studies of both manual and power wheelchair users, 47 factors were identified which are associated with participation. Of these, 15 factors were supported in multivariable analyses from seven studies [34, 36–41], with quality scores ranging from 7–10 of a possible 15 points, all employing cross-sectional designs. Nineteen factors were found in eleven studies employing bivariable analyses [16, 42–51], with quality scores ranging from 4–7 out of a possible 15 points. In qualitative analysis, 22 factors were found in five studies, with quality scores ranging from 8–9 of a possible 10 points, to have an impact on participation [33, 49, 50, 52–55]. See table 3 for factors identified by study. Of those factors identified in all studies pertaining to both manual and power wheelchair users, 13 were categorized as Body Functions, 4 as Activity and 5 as Participation factors, 14 Environmental factors, and 11 Personal factors. See table 4 for categorization of factors by ICF domain.
Table 4.
Modifiable and non-modifiable factors affecting participation, by ICF domain.
| ICF Domain | Modifiable | Non-Modifiable |
|---|---|---|
| Body Functions | Body Mass Index[16]Confidence[56, 57] Depression[36, 37] Fatigue[42, 52] Fear of Injury[50] Grip Strength[35] Motivation[52] Pain (including shoulder pain) Psychological Factors [54, 66] Physical Strain[58] Incontinence[52] Vision[52] Cognition[36] Physical Limitations [54] |
Cognition[36] Level of Injury (SCI)[38] Motor Involvement[52] Vision[52] |
| Activity Factors | Average speed travelled[44] Driving[34] Mobility[36, 63, 65] Wheelchair skills[36, 58–60] |
|
| Participation Factors | Being a member of society[33] Being Engaged (in social/civic pursuits)[33] Involvement in Sports[45, 47] Employment[46, 63] Interacting as a citizen[33] |
|
| Environmental Factors | Caregiver Concerns[52, 54] Dependence on Others[50] Environmental Characteristics (Crime) [39] Lack of opportunity[50] Level of daily assistance[40] Living alone[40] Social environment[52, 55] Suitable Housing[50] Transportation[50, 52] Wheelchair factors[38, 42, 46, 54, 63, 64, 66] Accessibility Home, Living Spaces[55, 65] Driving a Modified Vehicle [41] |
Accessibility (built environment, transit and work)[36, 42, 49–52, 54, 65, 66] Climate[55] Environmental Characteristics[53] Societal Attitudes (incl. Stigma)[50, 53, 54, 66] |
| Personal Factors | Finances[49, 50, 55, 63] Level of Education[16, 40, 46, 63] Loss of Identity[53] Marital Status[37, 63] Personality[52] Physical Health Status[46, 49] Tobacco Use[16] Wheelchair factors - satisfaction[64] Alcohol Use[16] |
Age[38, 46, 48, 58] # Comorbidities[54, 65] Race[63] Sex[16, 37, 38, 46] Years since injury[38, 63] |
Manual Wheelchair Users Only
Ten studies identified fifteen factors in studies specific to manual wheelchair users. Of these, six factors were supported in multivariate analyses from six studies[35, 56–60]. The quality of these studies ranged from 8–11 of a total 15 possible points, and all used a cross-sectional design. Factors which were identified only in manual wheelchair users include confidence[56, 57], grip strength[35], and physical strain[58]. Ten factors were identified in quantitative (bivariable) analysis, in four studies of manual wheelchair users[61–64], with quality of studies ranging from 7–10 of a possible 15 points. One randomized controlled trial was included[62], with a PEDro score of 6. Of these, only satisfaction with the wheelchair[64] and race[63] were not identified in any study comprised of both manual and power wheelchair users. Shoulder pain is the only factor identified in an interventional study[62]. No qualitative studies of only manual wheelchair users were included. See table 3 for factors identified by study. Of those factors identified in all studies pertaining to manual wheelchair users, four were categorized as Body Functions factors, two Activity factors, one Participation factor, one Environmental factor, and seven Personal factors. See table 4 for categorization of factors by ICF domain.
Power Wheelchair Users Only
Two studies identified seven factors in studies specific to power wheelchair users. Of these, three factors were supported in multivariate analyses from the same study[65]. This study had a quality score of 8/15, and used a cross-sectional design[65]. All factors associated with the social and community participation of power wheelchair users were also found to be associated with the participation of manual wheelchair users. One qualitative study, with a quality score of 9/10, identified four factors associated with participation of power wheelchair users[66]. No quantitative (bivariable) studies only consisting of power wheelchair users were included. See table 3 for factors identified by study. Of those factors identified in all studies pertaining to only power wheelchair users, one was categorized as a Body Functions factor, one Activity factor, four Environmental factors, and one Personal factor. See table 4 for categorization of factors by ICF domain.
Modifiable and Non-modifiable Factors
Table 4 lists those factors which are modifiable and non-modifiable by ICF domain. Factors which may or may not be modifiable depending on contextual and environmental considerations are listed in both columns. Modifiable factors are found in all domains of the ICF, while non-modifiable factors are found only in body structures/functions, environmental factors, and personal factors. Sixteen factors were categorized as Body Functions, of which 14 were modifiable. Two factors (cognition and vision) were classified as both modifiable and non-modifiable, depending on the condition and context. For example, low vision may be modifiable by improving contrast in the environment, whereas blindness may not be modifiable in rehabilitation, and may require compensation instead.. Four factors were specific to the Activity domain, and five to the Participation domains, of which all were modifiable. Fifteen factors were categorized as Environmental factors, of which 12 were modifiable. One environmental factor (accessibility) was categorized as both modifiable and non-modifiable, depending on environmental and contextual factors. An additional 14 factors were categorized as Personal Factors, of which 9 were modifiable.
Factors Reported Most Often
Accessibility was reported most often (10 studies) followed by wheelchair factors, including comfort, durability, and fit (7 studies). Wheelchair skills, pain, including shoulder pain, finances, societal attitudes (including stigma), level of education, age, and sex were each reported in four studies. Mobility was reported in three studies. Confidence, depression, fatigue, psychological factors, involvement in sports, employment, caregiver concerns, dependence on others, the social environment, transportation, number of comorbidities, physical health status, driving a modified vehicle, marital status and years since injury were reported in two studies each, with all other variables each reported in single studies.
Discussion
This paper systematically reviewed the literature to identify factors associated with social and community participation of adult wheelchair users. Evidence suggests that factors associated with participation differ depending on the type of wheelchair, although some similarities exist. In addition, social and community participation of wheelchair users is associated with factors from all domains of the ICF. Although many of these factors have statistically significant bivariate associations with participation, the majority have not been investigated using multivariable analyses. Those studies modeling participation using multivariable analyses illustrate the complexity of participation by showing how several factors interact to influence social and community participation. This suggests the use of multi-modal interventions in clinical practice may be more effective at improving the participation of wheelchair users than unilateral approaches. For example, Mortenson et al. found mobility, wheelchair skills, perceived environmental barriers, cognition, and depression all contributed to participation in social and community activities, while explaining 53% variance in residential care participants[36]. An intervention which targets two or more factors may demonstrate greater improvements in participation than an intervention which only targets one of these factors. For example, an intervention which focuses on improving wheelchair skills and reducing barriers to accessibility may be more effective than an intervention focusing on either of these factors alone.
Factors Specific to Type of Wheelchair
The majority of studies included for review identified factors associated with participation in wheelchair users in general without stratifying results by type of wheelchair used (i.e. manual or power wheelchair). Of the studies which provide wheelchair-specific results, it is apparent some participation factors are important for manual wheelchair users and not power wheelchair users, and vice-versa. For example, confidence with wheelchair use, grip strength, strain, race, and satisfaction with the wheelchair are reported to influence participation in manual wheelchair users, but are not found in studies pertaining specifically to power wheelchair users. As power and manual wheelchairs require significantly different skill sets, and often are associated with individuals with differing characteristics, such as age, type of injury or illness, cognitive status and physical health, future research should aim to stratify results by type of wheelchair to determine if device-specific participation enhancing interventions are warranted.
Body Structures and Functions factors
Body Structures and Functions are defined by the ICF as physiological and psychological functions, and anatomical parts of the body[67]. Number of depression symptoms was one of two factors within the Body Structures and Functions domain associated with participation in more than one study using multivariable analyses. In a study by Collins et al., depression, marriage status and sex accounted for 27.6% of the variation in social participation scores[37]. The impact of depression was also noted by Mortenson et al. as being negatively correlated with participation, when controlling for other variables[36]. The association of depression and participation is likely bidirectional, given evidence that increased participation reduces depressive symptoms[8], and that limited participation contributes to depression[7]. Interventions designed to improve participation by addressing depression and depressive symptoms in wheelchair users will have beneficial effects on their participation, overall health, and well-being.
Two multivariable studies also identified wheelchair confidence as a statistically significant factor of participation[56, 57]. Given the strong positive association between participation and confidence, it is plausible that improvements to confidence may lead to more participation. In fact, Sakakibara et al. demonstrated the association between confidence and participation is mediated by mobility and participation limitations. This suggests that improvements to confidence may lead to improved mobility and reduced participation limitations, which in turn has a positive effect on participation[54]. Experimental research is needed to corroborate these findings. Interestingly, confidence with wheelchair use has been shown to be modifiable via wheelchair skills training[68]. Therefore, a reasonable next step may be to test the hypothesis that improvements to confidence through wheelchair skills training leads to statistically significant improvements to social and community participation in wheelchair users.
In manual wheelchair users, grip strength[35] was also noted in multivariable analyses to have an impact on participation. There are many reasons why this may be the case. Stronger grip strength may be related to younger age, and overall strength and health, all of which could contribute to increased participation. Alternately, grip strength may be related to wheelchair skills capacity in manual wheelchair use, which has also been shown to have an impact on participation. That is, improved grip strength may lead to greater participation by means of improved wheelchair skills and/or activities of daily living. Interventional research is needed to investigate these hypotheses to develop a further understanding of the relationship between grip strength and participation.
Only one factor was identified in an intervention based study, specifically the treatment of shoulder pain[61, 62]. Pain was identified as a significant factor in four studies using bivariate analyses[42, 43, 61, 62]; two studies identified pain in general as a factor, while the other two studies identified shoulder pain as a limiting factor. Pain as a factor is specific to manual wheelchair users, a finding which is not surprising given the load placed on the shoulders during manual wheelchair propulsion. In a study of individuals with spinal cord injury, Jensen et al. report pain was significantly associated with decreased scores in social functioning and psychological functioning[69]. This supports our findings. Pain may limit an individual’s ability to operate their wheelchair, and hinder community engagement. Clinically, pain is seen as a modifiable factor, which can be improved through a variety of medical and non-medical interventions. For example, Kemp et al. established that a 12-week exercise and movement optimization program to strengthen shoulder muscles and modify upper extremity movements in wheelchair users reduced shoulder pain and improved social participation[62].
Also notable in the Body Structures and Functions domain is fatigue. Although fatigue was noted in two studies[42, 52], neither study investigated fatigue relative to other variables in multivariable analyses. A review of literature exploring fatigue in older adults found fatigue impacted participation in social and daily life due to the constraining effect on the individual’s abilities[70]. In a study of individuals with spinal cord injury, fatigue was noted to be significantly related to physical function, physical role, bodily pain, general health, vitality and social function[71].
Fatigue has also been identified as impacting participation in individuals post-stroke, notably impacting their social participation, employment, and driving[72]. Fatigue may also be related to other factors which were found to be correlates of participation, including factors identified in the activity and participation domain such as wheelchair skills, involvement in sports, and mobility. Intervention based research aiming to reduce the effects of fatigue in wheelchair users is warranted.
Activity Factors
Activities are related to the execution of specific tasks, separate from the context of the environment or personal factors. Multiple activities (i.e. making a telephone call, using transportation) may contribute to involvement in a life situation (i.e. engaging in a social relationship), which is the ICF definition of participation [67]. Within the Activity domain, wheelchair skills are commonly reported as an independent predictor of participation [36, 58–60]. For example, Mortenson et al. showed wheelchair skills to have both direct and indirect effects, through mobility, on frequency of participation[36]. Phang et al. also demonstrated a significant relationship between wheelchair skills and level of leisure time physical activity[60]. After controlling for covariates of sex, level of injury, employment, age at injury and race, Hosseini et al. demonstrated a higher level of wheelchair skills as measured by the Wheelchair Skills Test predicted increased levels of community participation[59]. Kilkens et al. also noted performance time on a Wheelchair Circuit was the only significant predictor of participation, after accounting for demographic variables and level of injury[58]. Level of wheelchair skills is likely associated with participation because it allows for greater mobility and independence. Although research shows the efficacy of wheelchair skills training programs at improving wheelchair skills, the impact of such improvement on participation has yet to be experimentally studied. This represents a key area for future intervention study. In addition, this may be an area where clinicians have an important role. By increasing the amount of wheelchair skills training provided to wheelchair users may also increase their social and community participation.
Environmental Factors
Environmental Factors are defined as those factors which make up the social, physical and attitudinal environment in which a person conducts his/her daily life[67]. Within this domain, the factor of accessibility, or physical barriers was identified in 10 studies [36, 42, 49–52, 54, 55, 65, 66], more than any other factor reported in this review.
Of the 10 studies, 2 reported statistically significant associations between physical barriers and social participation using multivariable analyses with conflicting results [36, 65]. In one study, higher reported environmental barriers were associated with lower levels of social participation[65], whereas the other study reported perceived environmental barriers were associated with higher levels of participation[36], Further research to investigate the impact of accessibility of a variety of environments (home, community, work etc.) is warranted to provide additional understanding about this difference. These studies differed significantly in their populations, and this may relate to the discrepancy. In the first, the sample was comprised of community dwelling wheelchair users, while in the second, the sample came from residential care facilities. Differences in environmental barriers and perceived barriers in these settings, as well as differences in the age, physical, and cognitive capacities of the two populations may have contributed to the difference in results. Interventional research to determine the impact of improved accessibility in home and work environments on participation in wheelchair users could potentially have effects on participation of wheelchair users.
Personal Factors
Personal Factors are contextual factors such as age, sex, gender, social history, education and past experience[67]. In this domain, the only factor identified in multiple studies, including multivariate analysis, which was also modifiable, was level of education, identified as having a significant association with participation in four studies[16, 40, 46, 63]. A study of older adults found those with lower levels of overall education had lower levels of physical activity participation[73]. In addition, level of education also modified the effects of employment status on physical activity participation[73]. It is plausible that level of education may contribute to increased participation through increased access to employment opportunities, identified as a significant factor in two of the same studies[46, 63].
Participation Factors
Interestingly, our results also illustrate associations between different types of participation, which is indicative of interactions between different areas of participation. The ICF identifies multiple areas of participation, including interpersonal interactions and relationships, education, work and employment, community life, recreation and leisure, and political life and citizenship[2]. It seems intuitive that physical activity participation (recreation and leisure) may lead to more social participation (interpersonal relationships), and participation in education may lead to participation in work and employment.
Study Limitations
Lack of precision and unclear definitions of domains in the ICF made it difficult to categorize some variables. Through discussion and debate, we were able to agree on the categorization of factors using the available definitions and additional references, and therefore believe our results are as accurate as possible. We also categorized factors by whether they were modifiable or non-modifiable in the context of an intervention, while recognizing almost any factor may be modifiable given sufficient resources. We categorized those which were modifiable in the context of a rehabilitation intervention to highlight those factors which may be relevant to clinicians and/or researchers investigating interventions to improve social and community participation in wheelchair users. Only English studies from the USA, Canada, and Europe were included for review. Therefore a bias may be introduced by not identifying results of studies conducted or published in other languages. Next, the majority of the studies included both power and manual wheelchair users, without stratifying results by type of wheelchair and therefore may not capture factors which affect one type of user disproportionally to the other. In addition, many of the included studies were specific to individuals with spinal cord injury, which may have biased the results. Finally, because very little experimental research has focused on improving participation in wheelchair users, we were unable to conduct a meta-analysis on the effectiveness of interventions at improving participation in this population. The lack of experimental findings and may enable bias in the findings. However, a body of correlational and qualitative literature exists which can provide direction on future research priorities in this area.
Conclusions
The social and community participation of wheelchair users is complex. It is influenced by all of Body Structures and Functions, Activity and Participation, Environmental, and Personal Factors. Overall, wheelchair factors and accessibility are most frequently reported as factors associated with participation. Wheelchair skills, pain, finances, and level of education are modifiable factors which were also frequently reported. Future intervention-based research focusing on modifiable factors, such as wheelchair skills and accessibility are warranted. Moreover, confidence and depression have not been studied in depth, but show promise in multivariable analyses. Research studying the efficacy of improved confidence and/or lowered depression at enhancing participation is warranted. Such research will enhance our knowledge of the social and community participation of wheelchair users.
Implications for Rehabilitation.
Wheelchair factors, including comfort and durability, are associated with participation, and may be targeted in clinical intervention.
Wheelchair skills are clinically modifiable, and have been shown to improve participation in manual wheelchair users.
Body Functions (i.e. confidence, depression, fatigue) and personal factors (i.e. finances, level of education) may be considered for clinical intervention.
Acknowledgments
We acknowledge the support of the GF Strong Rehabilitation Centre.
Funding Support
This research was supported by the Canadian Institutes of Health Research (Doctoral Scholarship to BMS), Operating Grant (107848-1), the CIHR CanWheel Emerging team in Wheeled Mobility for Older Adults (100925-1), and by the Social Sciences and Humanities Research Council.
Footnotes
Declaration of Interests
The authors report no declaration of interest.
References
- 1.World Health Organization. Active ageing: A policy framework. Geneva: World Health Organization; 2002. [PubMed] [Google Scholar]
- 2.World Health Organization. International classification of functioning, disability and health. Geneva: World Health Organization; 2001. [Google Scholar]
- 3.Levasseur M, Desrosiers J, Tribble DC. Subjective quality-of-life predictors for older adults with physical disabilities. Am J Phys Med Rehabil. 2008;87:10–830. doi: 10.1097/PHM.0b013e318186b5bd. [DOI] [PubMed] [Google Scholar]
- 4.Chang FH, Wang YH, Jang Y, Wang CW. Factors associated with quality of life among people with spinal cord injury: Application of the international classification of functioning, disability and health model. Arch Phys Med Rehabil. 2012 Dec;93(12):2264–70. doi: 10.1016/j.apmr.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Baum CM. Fulfilling the promise: Supporting participation in daily life. Arch Phys Med Rehabil. 2011 Feb;92(2):169–75. doi: 10.1016/j.apmr.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, Schulz R. Association of enjoyable leisure activities with psychological and physical well-being. Psychosom Med. 2009 Sep;71(7):725–32. doi: 10.1097/PSY.0b013e3181ad7978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmid AA, Damush T, Tu W, Bakas T, Kroenke K, Hendrie HC, Williams LS. Depression improvement is related to social role functioning after stroke. Arch Phys Med Rehabil. 2012;93:6–978. doi: 10.1016/j.apmr.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Forsman AK, Nordmyr J, Wahlbeck K. Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. HEALTH PROMOT INT. 2011 Dec-Feb;26:i85–i107. doi: 10.1093/heapro/dar074. [DOI] [PubMed] [Google Scholar]
- 9.Williams G, Willmott C. Higher levels of mobility are associated with greater societal participation and better quality-of-life. Brain Inj. 2012;26(9):1065–71. doi: 10.3109/02699052.2012.667586. [DOI] [PubMed] [Google Scholar]
- 10.Riggins MS, Kankipati P, Oyster ML, Cooper RA, Boninger ML. The relationship between quality of life and change in mobility 1 year postinjury in individuals with spinal cord injury. Arch Phys Med Rehabil. 2011 Jul;92(7):1027–33. doi: 10.1016/j.apmr.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Rousseau-Harrison K, Rochette A. Impacts of wheelchair acquisition on children from a person-occupation-environment interactional perspective. Disability and Rehabilitation: Assistive Technology 2013. 2013 Jan;8(1):1–10. doi: 10.3109/17483107.2012.670867. [DOI] [PubMed] [Google Scholar]
- 12.Sapey B, Stewart J, Donaldson G. Increases in wheelchair use and perceptions of disablement. DISABIL SOC. 2005;20(5):489. [Google Scholar]
- 13.Shore S, Juillerat S. The impact of a low cost wheelchair on the quality of life of the disabled in the developing world. Med Sci Monit. 2012 Sep;18(9):533–42. doi: 10.12659/MSM.883348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salminen AL, Brandt A, Samuelsson K, Töytäri O, Malmivaara A. Mobility devices to promote activity and participation: A systematic review. J Rehabil Med. 2009;41:9–697. doi: 10.2340/16501977-0427. [DOI] [PubMed] [Google Scholar]
- 15.Best KL, Routhier F, Miller WC. A description of manual wheelchair skills training: Current practices in canadian rehabilitation centers. Disabil Rehabil Assist Technol. 2014 Apr 7; doi: 10.3109/17483107.2014.907367. [DOI] [PubMed] [Google Scholar]
- 16.Best KL, Miller WC. Physical and leisure activity in older community-dwelling canadians who use wheelchairs: A population study. Journal of Aging Research. 2011;2011:2011. doi: 10.4061/2011/147929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brault MW. Americans with disabilities: 2010. Washington: U.S. Census Bureau; 2012. [Google Scholar]
- 18.LaPlante MP, Kaye HS. Demographics and trends in wheeled mobility equipment use and accessibility in the community. Assist Technol 2010. 2010;22(1):3–17. doi: 10.1080/10400430903501413. [DOI] [PubMed] [Google Scholar]
- 19.Vignier N, Ravaud JF, Winance M, Lepoutre FX, Ville I. Demographics of wheelchair users in france: Results of national community-based handicaps-incapacites-dependance surveys. J Rehabil Med. 2008 Mar;40(3):231–9. doi: 10.2340/16501977-0159. [DOI] [PubMed] [Google Scholar]
- 20.Kaye HS, Kang T, LaPlante MP. Mobility device use in the united states. Washington, D.C: U.S. Department of Education, National Institute on Disability and Rehabilitation Research; 2000. [Google Scholar]
- 21.Wilkie R, Peat G, Thomas E, Croft P. The prevalence of person-perceived participation restriction in community-dwelling older adults. Qual Life Res. 2006 Nov;15(9):1471–9. doi: 10.1007/s11136-006-0017-9. [DOI] [PubMed] [Google Scholar]
- 22.Kaye HS, Kang T, LaPlante MP. Disability statistics abstract: Wheelchair use in the united states. Washington, D.C: U.S. Department of Education; 2002. Report nr 23. [Google Scholar]
- 23.Fomiatti R, Richmond J, Moir L, Millsteed J. A systematic review of the impact of powered mobility devices on older adults’ activity engagement. PHYS OCCUP THER GERIATR. 2013;31:4–297. [Google Scholar]
- 24.Perenboom R, Chorus A. Measuring participation according to the international classification of functioning, disability and health (ICF) Disabil Rehabil. 2003 Jun-Mar;25(11):577–87. doi: 10.1080/0963828031000137081. [DOI] [PubMed] [Google Scholar]
- 25.Chung P, Sarah Jin HY, Khan F. A comparison of participation outcome measures and the international classification of functioning, disability and health core sets for traumatic brain injury. J REHABIL MED (16501977) 2014;46:2–108. doi: 10.2340/16501977-1257. [DOI] [PubMed] [Google Scholar]
- 26.Resnik L, Plow MA. Measuring participation as defined by the international classification of functioning, disability and health: An evaluation of existing measures. Arch Phys Med Rehabil. 2009;90:5–856. doi: 10.1016/j.apmr.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Jette AM, Haley SM, Kooyoomjian JT. Are the ICF activity and participation dimensions distinct? J Rehabil Med. 2003;35:3–145. doi: 10.1080/16501970310010501. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009 Aug-18;151(4):264. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 29.Cieza A, Geyh S, Chatterji S, Kostanjsek N, Üstün B, Stucki G. ICF linking rules: An update based on lessons learned. J Rehabil Med. 2005;37:4–212. doi: 10.1080/16501970510040263. [DOI] [PubMed] [Google Scholar]
- 30.Chen S, Winstein CJ. A systematic review of voluntary arm recovery in hemiparetic stroke: Critical predictors for meaningful outcomes using the international classification of functioning, disability, and health. Journal of Neurologic Physical Therapy. 2009 Mar;33(1):2–13. doi: 10.1097/NPT.0b013e318198a010. [DOI] [PubMed] [Google Scholar]
- 31.PEDro Scale [Internet] Australia: Physiotherapy Evidence Database; p. c1999. Available from: www.pedro.org.au. [Google Scholar]
- 32.Qualitative Research Checklist [Internet] United Kingdom: Critical Appraisal Skills Program; p. c2013. Available from: www.casp-uk.net. [Google Scholar]
- 33.Hjelle KM, Vik K. The ups and downs of social participation: Experiences of wheelchair users in norway. Disabil Rehabil. 2011;33(25–26):2479–89. doi: 10.3109/09638288.2011.575525. [DOI] [PubMed] [Google Scholar]
- 34.Norweg A, Jette AM, Houlihan B, Ni P, Boninger ML. Patterns, predictors, and associated benefits of driving a modified vehicle after spinal cord injury: Findings from the national spinal cord injury model systems. Arch Phys Med Rehabil. 2011 Mar;92(3):477–83. doi: 10.1016/j.apmr.2010.07.234. [DOI] [PubMed] [Google Scholar]
- 35.Shechtman O, Locklear C, MacKinnon L, Hanson C. The relationship between strength, pain, and community integration in wheelchair users: A pilot study. Occup Ther Health Care. 2003;17:1–5. doi: 10.1080/J003v17n01_02. [DOI] [PubMed] [Google Scholar]
- 36.Mortenson WB, Miller WC, Backman CL, Oliffe JL. Association between mobility, participation, and wheelchair-related factors in long-term care residents who use wheelchairs as their primary means of mobility. J Am Geriatr Soc. 2012;60:7–1310. doi: 10.1111/j.1532-5415.2012.04038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Collins DM, Fitzgerald SG, Sachs-Ericsson N, Scherer M, Cooper RA, Boninger ML. Psychosocial well-being and community participation of service dog partners. Disability and Rehabilitation. Assistive Technology 2006. 2006 Jan-Jun;1(1–2):41–8. doi: 10.1080/09638280500167183. [DOI] [PubMed] [Google Scholar]
- 38.Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, Hayes KC, Hicks AL, McColl MA, Potter PJ, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: Demographic and injury-related correlates. Arch Phys Med Rehabil. 2010 May;91(5):722–8. doi: 10.1016/j.apmr.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 39.Liang H, Tomey K, Chen D, Savar NL, Rimmer JH, Braunschweig CL. Objective measures of neighborhood environment and self-reported physical activity in spinal cord injured men. Arch Phys Med Rehabil. 2008 Aug;89(8):1468–73. doi: 10.1016/j.apmr.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 40.Warner G, Basiletti M, Hoenig H. Age differences in leisure physical activity by adult wheelchair users. PHYS OCCUP THER GERIATR. 2010;28:4–410. [Google Scholar]
- 41.Tsai I, Graves DE, Lai C. The association of assistive mobility devices and social participation in people with spinal cord injuries. Spinal Cord 2014. 2014 Mar;52(3):209–15. doi: 10.1038/sc.2013.178. [DOI] [PubMed] [Google Scholar]
- 42.Chaves ES, Boninger ML, Cooper R, Fitzgerald SG, Gray DB, Cooper RA. Assessing the influence of wheelchair technology on perception of participation in spinal cord injury. Arch Phys Med Rehabil. 2004;85:11–1854. doi: 10.1016/j.apmr.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 43.Leung V, Colantonio A, Santaguida PL. Wheelchair use pain, and satisfaction with life in a national sample of older adults. Gerontechnology. 2005;3:3–159. [Google Scholar]
- 44.Cooper RA, Ferretti E, Oyster M, Kelleher A, Cooper R. The relationship between wheelchair mobility patterns and community participation among individuals with spinal cord injury. Assistive Technology. 2011;23:3–177. [Google Scholar]
- 45.Anneken V, Hanssen-Doose A, Hirschfeld S, Scheuer T, Thietje R. Influence of physical exercise on quality of life in individuals with spinal cord injury. Spinal Cord. 2010 May;48(5):393–9. doi: 10.1038/sc.2009.137. [DOI] [PubMed] [Google Scholar]
- 46.Carlson D, Myklebust J. Wheelchair use and social integration. Top Spinal Cord Inj Rehabil 2002. 2002;7(3):28–46. [Google Scholar]
- 47.McVeigh SA, Hitzig SL, Craven BC. Influence of sport participation on community integration and quality of life: A comparison between sport participants and non-sport participants with spinal cord injury. J Spinal Cord Med. 2009;32:2–115. doi: 10.1080/10790268.2009.11760762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meyers AR, Anderson JJ, Miller DR, Shipp K, Hoenig H. Barriers, facilitators, and access for wheelchair users: Substantive and methodologic lessons from a pilot study of environmental effects. Soc Sci Med. 2002 Oct-15;55(8):1435–46. doi: 10.1016/s0277-9536(01)00269-6. [DOI] [PubMed] [Google Scholar]
- 49.Pluym SM, Keur TJ, Gerritsen J, Post MW. Community integration of wheelchair-bound athletes: A comparison before and after onset of disability. Clin Rehabil. 1997 Aug;11(3):227–35. doi: 10.1177/026921559701100306. [DOI] [PubMed] [Google Scholar]
- 50.Tasiemski T, Bergström E, Savic G, Gardner BP. Sports, recreation and employment following spinal cord injury -- a pilot study. Spinal Cord. 2000;38:3–173. doi: 10.1038/sj.sc.3100981. [DOI] [PubMed] [Google Scholar]
- 51.Akyuz M, Yalcin E, Selcuk B, Degirmenci I. The barriers limiting the social integration of wheelchair users with spinal cord injury in turkish society. Neurosurgery Quarterly 2014. 2014 Aug;24(3):225–8. [Google Scholar]
- 52.Rudman DL, Hebert D, Reid D. Living in a restricted occupational world: The occupational experiences of stroke survivors who are wheelchair users and their caregivers. Can J Occup Ther. 2006;73:3–141. doi: 10.2182/cjot.05.0014. [DOI] [PubMed] [Google Scholar]
- 53.Levins SM, Redenbach DM, Dyck I. Individual and societal influences on participation in physical activity following spinal cord injury: A qualitative study. Phys Ther. 2004 Jun;84(6):496–509. [PubMed] [Google Scholar]
- 54.Barker DJ, Reid D, Cott C. The experience of senior stroke survivors: Factors in community participation among wheelchair users. Can J Occup Ther. 2006;73:1–18. doi: 10.2182/cjot.05.0002. [DOI] [PubMed] [Google Scholar]
- 55.Reid D, Angus J, McKeever P, Miller KL. Home is where their wheels are: Experiences of women wheelchair users. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association 2003. 2003;57(2):186–95. doi: 10.5014/ajot.57.2.186. [DOI] [PubMed] [Google Scholar]
- 56.Sakakibara BM, Miller WC, Routhier F, Backman CL, Eng JJ. The association between self-efficacy and participation in community-dwelling manual wheelchair users, aged 50 and over. Phys Ther. 2014 doi: 10.2522/ptj.20130308. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sakakibara BM, Miller WC, Eng JJ, Backman CL, Routhier F. Preliminary examination of the relation between participation and confidence in older manual wheelchair users. Arch Phys Med Rehabil 2013. 2013 Apr;94(4):791–4. doi: 10.1016/j.apmr.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kilkens OJ, Post MW, Dallmeijer AJ, van Asbeck FW, van der Woude LH. Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 year after discharge from inpatient rehabilitation. Journal of Rehabilitation Research and Development. 2005;42(3 Suppl 1)(65–73):65–74. doi: 10.1682/jrrd.2004.08.0093. [DOI] [PubMed] [Google Scholar]
- 59.Hosseini SM, Oyster ML, Kirby RL, Harrington AL, Boninger ML. Manual wheelchair skills capacity predicts quality of life and community integration in persons with spinal cord injury. Arch Phys Med Rehabil. 2012 Dec;93(12):2237–43. doi: 10.1016/j.apmr.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 60.Phang SH, Martin Ginis KA, Routhier F, Lemay V. The role of self-efficacy in the wheelchair skills-physical activity relationship among manual wheelchair users with spinal cord injury. Disabil Rehabil. 2012;34(8):625–32. doi: 10.3109/09638288.2011.613516. [DOI] [PubMed] [Google Scholar]
- 61.Gutierrez DD, Thompson L, Kemp B, Mulroy SJ Physical Therapy Clinical Research Network, Rehabilitation Research and Training Center on Aging-Related Changes in Impairment for Persons Living with Physical Disabilities. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30(3):251–5. doi: 10.1080/10790268.2007.11753933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kemp BJ, Bateham AL, Mulroy SJ, Thompson L, Adkins RH, Kahan JS. Effects of reduction in shoulder pain on quality of life and community activities among people living long-term with SCI paraplegia: A randomized control trial. J Spinal Cord Med. 2011 May;34(3):278–84. doi: 10.1179/107902611X12972448729486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oyster ML, Karmarkar AM, Patrick M, Read MS, Nicolini L, Boninger ML. Investigation of factors associated with manual wheelchair mobility in persons with spinal cord injury. Arch Phys Med Rehabil 2011. 2011 Mar;92(3):484–90. doi: 10.1016/j.apmr.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 64.de Groot S, Post MW, Bongers-Janssen HM, Bloemen-Vrencken JH, van der Woude LH. Is manual wheelchair satisfaction related to active lifestyle and participation in people with a spinal cord injury? Spinal Cord. 2011 Apr;49(4):560–5. doi: 10.1038/sc.2010.150. [DOI] [PubMed] [Google Scholar]
- 65.Hoenig H, Landerman LR, Shipp KM, George L. Activity restriction among wheelchair users. J Am Geriatr Soc. 2003;51:9–1244. doi: 10.1046/j.1532-5415.2003.51408.x. [DOI] [PubMed] [Google Scholar]
- 66.Blach Rossen C, Sørensen B, Würtz Jochumsen B, Wind G. Everyday life for users of electric wheelchairs - a qualitative interview study. Disabil Rehabil Assist Technol. 2012;7:5–399. doi: 10.3109/17483107.2012.665976. [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization. ICF beginner’s guide. Genva: World Health Organization; 2002. [Google Scholar]
- 68.Sakakibara BM, Miller WC, Souza M, Nikolova V, Best KL. Wheelchair skills training to improve confidence with using a manual wheelchair among older adults: A pilot study. Arch Phys Med Rehabil. 2013 Jun;94(6):1031–7. doi: 10.1016/j.apmr.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jensen MP, Kuehn CM, Amtmann D, Cardenas DD. Symptom burden in persons with spinal cord injury. Arch Phys Med Rehabil. 2007;88:5–638. doi: 10.1016/j.apmr.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu D, Lee D, Man NW. Fatigue among older people: A review of the research literature. Int J Nurs Stud. 2010;47:2–216. doi: 10.1016/j.ijnurstu.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 71.Wijesuriya N, Tran Y, Middleton J, Craig A. Impact of fatigue on the health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:2–319. doi: 10.1016/j.apmr.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 72.Flinn NA, Stube JE. Post-stroke fatigue: Qualitative study of three focus groups. OCCUP THER INT. 2010;17:2–81. doi: 10.1002/oti.286. [DOI] [PubMed] [Google Scholar]
- 73.Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health. 2008;20:7–767. doi: 10.1177/0898264308321081. [DOI] [PMC free article] [PubMed] [Google Scholar]