Abstract
Background
Posttraumatic stress disorder (PTSD) among inpatients with substance use disorders (SUDs) is associated with heightened engagement in a variety of risky, self-destructive, and health-compromising behaviors (e.g., risky sexual behavior, aggression). Extant research provides support for the role of emotion dysregulation in the PTSD-risky behavior relation among inpatients with SUD; however, this research has been limited by a focus on emotion dysregulation involving negative (versus positive) emotions. The goal of the current study was to extend past research on the PTSD-risky behavior relation by examining the potential mediating roles of negative and positive urgency (two domains of emotion dysregulation defined by the tendency to engage in risky behavior in the context of negative and positive emotions, respectively).
Methods
Participants were 158 trauma-exposed inpatients with (n = 91) and without (n = 67) lifetime PTSD consecutively admitted to a residential SUD treatment facility (M age = 34.34; 59.5% White, 50.6% female). Patients were administered diagnostic interviews and completed self-report questionnaires.
Results
Significant positive associations were found among lifetime PTSD symptoms, negative and positive urgency, and risky behaviors. Moreover, findings revealed significant indirect effects of lifetime PTSD symptoms on risky behaviors through the pathways of both negative and positive urgency.
Conclusions
Results provide initial support for the mediating roles of both negative and positive urgency in the PTSD-risky behavior relation, highlighting the potential utility of teaching trauma-exposed inpatients with PTSD-SUD skills for tolerating negative and positive emotional states without engaging in maladaptive behaviors.
Keywords: posttraumatic stress disorder, substance use disorder, risky behaviors, negative urgency, positive urgency, emotion dysregulation
1. Introduction
Posttraumatic stress disorder (PTSD) is a serious psychiatric disorder characterized by symptoms of intrusion, avoidance, negative cognition/mood, and arousal/reactivity following direct or indirect exposure to a traumatic event (American Psychiatric Association [APA], 2013). Whereas 8–14% of the general population will meet criteria for PTSD at some point in their lifetime (e.g., Breslau et al., 1998; Kessler et al., 1995), heightened rates of PTSD have been found among inpatients with a substance use disorders (SUDs), with approximately 36% to 50% of individuals seeking treatment for SUD meeting criteria for lifetime PTSD (see Brady et al., 2004 for a review). The co-occurrence of PTSD and SUD is clinically-relevant. Co-occurring PTSD-SUD (versus SUD alone) has been associated with heightened engagement in a wide range of risky, self-destructive, and health-compromising behaviors, such as risky sexual behavior (e.g., Weiss et al., 2013b), deliberate self-harm (e.g., Gratz and Tull, 2010b), aggressive behavior (e.g., Weiss et al., 2014), and disordered eating (e.g., Cohen et al., 2010). Moreover, inpatients with PTSD-SUD report more severe patterns of substance use than inpatients with SUD alone (e.g., Back et al., 2000). Notably, engagement in these risky behaviors has been linked to numerous deleterious consequences (e.g., disease/injury, crime and criminal justice system costs, decreased worker productivity; Cawley and Ruhm, 2011; Zohrabian and Philipson, 2010), as well as worse SUD outcomes (e.g., SUD treatment dropout; Patkar et al., 2004). However, despite the clear clinical relevance and public health significance of risky behaviors among inpatients with PTSD-SUD, little research has investigated the potential mechanisms underlying the PTSD-risky behavior relation within this population.
An emerging body of literature highlights the role of emotion dysregulation in the development, maintenance, and/or exacerbation of risky behaviors (see Weiss et al., 2015, in press for reviews). Emotion dysregulation is a multi-faceted construct involving maladaptive ways of responding to emotions, regardless of their intensity or reactivity (Gratz and Roemer, 2004; Gratz and Tull, 2010a). The heightened emotion dysregulation reported by inpatients with co-occurring PTSD-SUD (e.g., Weiss et al., 2013a, 2013c, 2012) is theorized to underlie the elevated rates of risky behaviors within this population; however, the precise nature of this relation remains unclear (see Tull et al., in press, for a review). Risky behaviors may have an emotion regulating function, serving to escape or avoid the heightened levels of emotional distress common among individuals with PTSD (e.g., Baker et al., 2004; Khantzian, 1997) or to elicit, maintain, or enhance positive emotional states (e.g., Cox and Klinger, 1988; Nock and Prinstein, 2004). Alternatively, the elevated levels of emotion dysregulation among inpatients with co-occurring PTSD-SUD may interfere with the ability to control behaviors in the context of intense emotions (Baumeister et al., 1998).
Consistent with this theoretical literature, preliminary empirical evidence supports the relevance of emotion dysregulation to risky behaviors within SUD samples. For example, levels of emotion dysregulation among inpatients with SUD have been found to be significantly positively associated with overall risky behaviors (e.g., Weiss et al., 2012), as well as the specific risky behaviors of substance use (e.g., Axelrod et al., 2011), risky sexual behavior (e.g., Tull et al., 2012), deliberate self-harm (e.g., Gratz and Tull, 2010b), aggressive behavior (e.g., Long et al., 2014), and disordered eating (e.g., Lavender et al., 2015). Further, and of particular relevance to the present study, results of Weiss et al. (2012) provide initial support for the mediating role of emotion dysregulation in the PTSD-risky behavior relation among inpatients with SUD. Notably, however, no studies have examined the role of specific dimensions of emotion dysregulation in the association between PTSD and risky behaviors.
Nonetheless, a growing body of research underscores the relevance of the specific dimension of emotion dysregulation involving difficulties controlling behaviors in the context of intense emotions (i.e., urgency) to both PTSD (Weiss et al., 2013a, 2013c) and risky behaviors (see Cyders and Smith, 2007, 2008 for reviews). With regard to the relation between urgency and PTSD among inpatients with SUD, Weiss et al. (2013a) found significantly higher levels of urgency among inpatients with co-occurring PTSD-SUD (vs. SUD only). Moreover, urgency emerged as a unique predictor of PTSD status (present vs. absent) among inpatients with SUD, above and beyond other dimensions of emotion dysregulation (Weiss et al., 2013c). As for the urgency-risky behavior relation, literature reviews focused on the UPPS (the most widely-used measure of urgency; Cyders et al., 2007; Whiteside and Lynam, 2001) suggest that urgency is a stronger predictor of risky behaviors than the other constructs assessed by the UPPS (i.e., sensation seeking, lack of premeditation, and lack of perseverance; Cyders and Smith, 2007, 2008). Similarly, meta-analyses indicate that urgency in particular (relative to sensation seeking, lack of premeditation, and lack of perseverance) is more strongly related to a range of risky behaviors, including substance use and negative alcohol-related outcomes, self-injurious behaviors, disordered eating, and aggression (Berg et al., in press; Coskunpinar et al., 2013). Although studies provide support for the urgency-risky behavior relation, it warrants mention that this research has focused almost exclusively on non-clinical populations, and no studies have explored the precise interrelations among PTSD, urgency, and risky behaviors in general or among inpatients with SUD in particular. Such investigations may elucidate specific treatment targets for reducing risky behaviors within a population at high risk for these behaviors.
An additional limitation of extant research on the relations among PTSD, emotion dysregulation, and risky behaviors is its primary focus on emotion dysregulation involving negative (versus positive) emotions. Individuals can experience dysregulation across both negative and positive emotional systems (e.g., Cyders and Smith, 2008; Gruber et al., 2011; Weiss et al., 2015), and research has identified the relevance of several difficulties in the regulation of positive emotions to PTSD and/or risky behaviors, including nonacceptance of positive emotions, low positive emotion differentiation, and difficulty controlling risky behaviors and engaging in goal-directed behaviors when experiencing positive emotions (e.g., Dixon-Gordon et al., 2014; Roemer et al., 2001; Tull and Roemer, 2007; Weiss et al., 2015). However, no studies have examined the role of difficulties in the regulation of positive emotions in the PTSD-risky behavior relation in general or among inpatients with SUD. In particular, despite past studies both linking difficulties controlling behaviors in the context of intense positive emotions (i.e., positive urgency; see Cyders et al., 2007) to numerous risky behaviors in non-PTSD populations (e.g., substance use, risky sexual behavior, disordered eating, and gambling; Anestis et al., 2007; Cyders et al., 2009; Cyders and Smith, 2008; Cyders et al., 2007; Fischer et al., 2007; Zapolski et al., 2009) and highlighting the relevance of difficulties controlling behaviors in the context of intense negative emotions (i.e., negative urgency; see Whiteside and Lynam, 2001) to PTSD (Weiss et al., 2013a, 2013c), no research has examined the relevance of positive urgency to the PTSD-risky behavior relation in inpatients with SUD.
Thus, the goal of the current study was to examine the potential mediating roles of both negative and positive urgency in the relation between PTSD symptoms and risky behaviors in a sample of trauma-exposed inpatients with SUD. We hypothesized that PTSD symptoms would be significantly positively associated with negative urgency, positive urgency, and risky behaviors. Furthermore, we predicted that negative and positive urgency would be significantly positively associated with risky behaviors. Finally, we hypothesized that both negative and positive urgency would mediate the relation between PTSD symptoms and risky behaviors.
2. METHODS
2.1. Participants
Participants were 158 trauma-exposed inpatients admitted to a residential SUD treatment facility in central Mississippi. Standard treatment at this treatment facility involves a mix of strategies from Alcoholics Anonymous and Narcotics Anonymous, as well as groups that cover a variety of topics, including coping skills and relapse prevention. This treatment center requires complete abstinence from drugs and alcohol, with the exception of nicotine and caffeine. Methadone maintenance is not available at this treatment facility, and no patients were receiving medication-assisted treatment for their SUD at the time of this study. Aside from scheduled activities, residents are not permitted to leave the treatment facility. Participants ranged in age from 18 to 59 (M age = 34.34, SD = 9.99) and just over half were female (n = 80, 50.6%). In terms of racial/ethnic background, 59.5% of participants (n = 94) self-identified as White, 36.7% as Black/African American (n = 58), 1.9% as Latino/a (n = 3), 1.3% as Native American (n = 2), and 0.6% as Asian/Southeast Asian (n = 1). Almost half of the participants reported an annual income under $10,000 (n = 76, 48.7%), and 62.7% (n = 99) had no higher than a high school education. Most participants were single (n = 133; 84.2%).
2.2. Measures
2.2.1. Clinical Interviews
The SUD module of the Structured Clinical Interview for Diagnostic DSM-IV Axis I Disorders (SCID-I/P; First et al., 1996) was used to determine the presence of current substance dependence across a variety of different substances. The SUD module has shown good validity (e.g., Kidorf et al., 1998; Kranzler et al., 1996) and high inter-rater reliability (e.g., Skre et al., 1991).
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990, 1995), the most widely used PTSD measure (Elhai et al., 2005), was used to assess lifetime PTSD symptom severity. This structured diagnostic interview first assesses DSM-IV-TR Criterion A traumatic exposure. The frequency and intensity of the 17 DSM-IV PTSD symptoms are then examined among participants reporting a Criterion A traumatic event. Frequency items are rated from 0 (never or none/not at all) to 4 (daily or almost every day or more than 80%). Intensity items are rated from 0 (none) to 4 (extreme). The CAPS has been found to demonstrate adequate interrater reliability (.92–.99), internal consistency (.73–.85), and convergent validity with the SCID-IV and other established measures of PTSD (Weathers et al., 2001). In addition, the robust psychometric properties of the CAPS have been supported in a variety of combat and civilian (including inpatient SUD) samples, as well as across different racial/ethnic groups (see Weathers et al., 2001 for a review). Internal consistency for lifetime PTSD symptoms in the current sample was excellent (α = .93).
Given the dearth of empirically-supported measures of risky behaviors, and consistent with Weiss et al. (2012), we utilized the risky behaviors criterion of the borderline personality disorder (BPD) module of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al., 1996) to assess clinically-relevant risky behaviors. The DIPD-IV is a well-established and widely-used diagnostic interview of personality disorders with good inter-rater and test-retest reliability (Zanarini et al., 2000). The BPD module assesses the presence of clear-cut patterns of 12 risky behaviors in the past two years (see Table 1). Only those behaviors endorsed by the participant as occurring regularly over the past two years are considered “present” and scored a 1 (i.e., ≥ 5 incidents of binge drinking, illicit substance use or prescription drug misuse, risky sexual behavior, binge eating, excessive spending, verbal aggression, and reckless driving; ≥ 3 incidents of deliberately damaging property; and ≥ 2 incidents of physical assault, fistfights, and criminal behavior); behaviors that occurred infrequently or never are scored a 0. Scores for each of the 12 behaviors are then summed to create a continuous variable reflecting the total number of risky behaviors the participant has engaged in regularly during the past two years. Although the risky behaviors assessed by this item are considered relevant to a BPD diagnosis, they have also been found to be relevant to PTSD (e.g., Tull et al., in press; Weiss et al., 2012). Internal consistency for this variable within this sample was adequate (α = .81). All interviews were administered by post-baccalaureate or doctoral-level clinical assessors trained to reliability with the principal investigator. All interviews were reviewed by a PhD level clinician, with diagnoses confirmed in consensus meetings.
Table 1.
Percentage of participants reporting clinically-relevant patterns of individual risky behaviors
| A pattern of… | % Endorsed |
|---|---|
| Problematic drug use | 89.2% (n = 141) |
| Problematic alcohol use | 82.9% (n = 131) |
| Verbal aggression | 65.8% (n = 104) |
| Reckless driving | 63.9% (n = 101) |
| Criminal behavior | 61.4% (n = 97) |
| Risky sexual behavior | 50.0% (n = 79) |
| Verbal threats | 43.0% (n = 68) |
| Excessive spending | 43.0% (n = 68) |
| Deliberately damaging property | 36.7% (n = 58) |
| Physical assault or abuse | 36.1% (n = 57) |
| Fistfights | 34.8% (n = 55) |
| Binge eating | 14.6% (n = 23) |
2.2.2. Measure of Negative and Positive Urgency
The Urgency, Premeditation, Perseverance, Sensation Seeking, and Positive Urgency Impulsive Behavior Scale (UPPS-P; Cyders et al., 2007; Whiteside and Lynam, 2001) is a 59-item self-report questionnaire that assesses multiple dimensions of impulsivity, including negative urgency, positive urgency, sensation seeking, lack of premeditation, and lack of perseverance. Participants rate the extent to which each item applies to them on a 4-point Likert-type scale (1 = rarely/never true, 4 = almost always/always true). The negative and positive urgency subscales, which measure the tendency to engage in risky behaviors when experiencing intense negative and positive emotions, respectively, were utilized in the present study given their overlap with the dimension of emotion dysregulation involving difficulties controlling impulsive behaviors in the context of intense emotions (Cyders and Smith, 2008; Weiss et al., 2013), as well evidence that these particular UPPS-P dimensions correlate most strongly with risky behaviors (see Berg et al., 2015; Coskunpinar et al., 2013; Cyders and Smith, 2007, 2008 for literature and meta-analytic reviews). These subscales have been shown to demonstrate adequate psychometric properties (Cyders et al., 2007). Internal consistency in this sample was adequate (αs = .81 and .91 for negative and positive urgency, respectively).
2.2.3. Demographic Information
All participants completed a demographics form assessing gender, age, racial/ethnic background, marital status, education, and income in the past year. These characteristics were examined as potential covariates.
2.2.4. Withdrawal Symptoms
Following the SCID-I/P, participants completed a self-report measure assessing 28 withdrawal symptoms associated with the discontinuation of a variety of different substances (e.g., sedatives, alcohol, opioids, cocaine). The severity of each withdrawal symptom was rated on a 5-point Likert-type scale ranging from 0 (not at all) to 4 (extremely severe). Items were summed to create an overall score reflecting the severity of current withdrawal symptoms, and this score was used to evaluate whether participants were experiencing withdrawal symptoms at a severity level that could interfere with study participation.
2.3. Procedure
All procedures were reviewed and approved by Institutional Review Boards of the University of Mississippi Medical Center and the Mississippi State Hospital. Data were collected as part of a larger study examining risk-taking as a function of PTSD among inpatients with SUD. To be eligible for inclusion in the larger study, participants were required to have: (a) reported dependence on alcohol and/or cocaine; (b) obtained a Mini-Mental Status Exam (Folstein et al., 1975) score of ≥ 24; and (c) exhibited no current psychotic disorders (as determined by the Mini International Neuropsychiatric Interview; Sheehan et al., 1998). Those who met inclusion criteria were provided with information about study procedures and associated risks, following which written informed consent was obtained. Eligible participants were recruited for this study no sooner than 72 hours after entry in the facility to limit the possible interference of withdrawal symptoms on study engagement.
The larger study involved three separate sessions conducted on separate days. The present study uses data from only the first session, during which participants completed a series of diagnostic interviews (including the SUD module of the SCID-I/P, CAPS, and BPD module of the DIPD) and questionnaires. Only participants who reported a DSM-IV-TR Criterion A traumatic event were included in the current study. Participants were reimbursed $25 for completing this session.
2.4. Data Analysis
As recommended by Tabachnick and Fidell (2007), all study variables were examined for assumptions of normality. Pearson product-moment and partial correlations were conducted to examine intercorrelations among the primary study variables. A series of analyses of variance and correlation analyses were conducted to examine the impact of demographic variables (i.e., age, gender, racial/ethnic background, income, education, and relationship status) on the dependent variable (i.e., risky behaviors). Given the small number of participants in several of the income, marital status, education, and racial/ethnic categories, these variables were collapsed into dichotomous variables of over (51.3%) versus under (48.7%) $10,000 per year; not married (84.2%) versus married (15.8%); high school diploma or less (62.7%) versus some education beyond high school (37.3%); and White (59.5%) versus Non-White (40.5%).
Following this, structural equation modeling (SEM) was used to examine negative and positive urgency as mediators of the relation between lifetime PTSD symptoms and risky behaviors. Given theoretical and empirical evidence suggesting considerable overlap between positive and negative urgency (with positive and negative urgency theorized to represent two domains of the larger construct of urgency), a latent variable (i.e., urgency) was utilized in the SEM model to represent these manifest variables (i.e., negative and positive urgency). Of note, SEM calculates indirect effects through all manifest variables individually, thereby facilitating examination of the mediating role of each manifest variable (i.e., negative and positive urgency) in the SEM model. AMOS 20.0 (Arbuckle, 2010), which uses Full Information Maximum Likelihood to deal with missing data, was employed to analyze the path models, obtain maximum-likelihood estimates of model parameters, and provide goodness-of-fit indices (Peters and Enders, 2002). Full information maximum likelihood estimation is robust against violations of normality (Bollen, 1989). Standard measures including χ2, normed fit index (NFI), Tucker-Lewis index (TLI), comparative fit index (CFI), root mean square error of approximation (RMSEA), and p of the close fit (PCLOSE) were used to assess model fit. A nonsignificant χ2, values of NFI, TLI, and CFI ≥ .90, lower RMSEA values (<.05), and higher PCLOSE values (>.05), are considered indicators of good model fit (Browne and Cudeck, 1992; Hu and Bentler, 1999; Lei and Wu, 2007).
Next, and consistent with recommendations (Kline, 2011; Preacher and Hayes, 2004), bootstrapping procedures were utilized to estimate the significance of any indirect effects. Compared to the causal steps approach to testing mediation (e.g., Baron and Kenny, 1986), bootstrap methodology tests indirect effects directly, is more statistically powerful, and does not rely on distributional assumptions (McCartney et al., 2006). Bootstrapping was done with 5,000 random samples generated from the observed covariance matrix to estimate bias-corrected 95% confidence intervals (CIs) and significance values for the standardized indirect effects in the final model.
Finally, given evidence to suggest that negative and positive urgency are distinct traits that evidence differential relations to aspects of risky behaviors (see Cyders and Smith, 2007, 2008 for reviews), analyses were also conducted to explore whether negative and positive urgency independently mediate the relation between PTSD symptoms and risky behaviors.
3. RESULTS
3.1. Preliminary Analyses
On average, participants reported experiencing withdrawal symptoms at a negligible to mild level of severity (M item response = 0.57, SD = 0.68), suggesting that withdrawal symptoms would not interfere with study participation. Based on CAPS data, 91 participants (57.6%) met diagnostic criteria for lifetime PTSD, with PTSD symptom severity scores ranging from 0 to 120 (M = 53.04, SD = 34.55). Participants reported clinically-relevant patterns of risky behavior in 6.23 areas on average (SD = 3.14). The frequencies of endorsement of clinically-relevant patterns of specific risky behaviors are presented in Table 1. Descriptive data and intercorrelations among the primary variables of interest are presented in Table 2.
Table 2.
Descriptive Data for and Intercorrelations among PTSD Symptoms, Risky Behaviors, and Negative and Positive Urgency
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. PTSD Symptoms | -- | .16* | .22** | .24** |
| 2. Risky Behaviors | .15+ | -- | .30*** | .24** |
| 3. Negative Urgency | .21** | .27** | -- | .60*** |
| 4. Positive Urgency | .24** | .23** | .60*** | -- |
|
| ||||
| M | 53.04 | 6.23 | 45.43 | 47.04 |
| SD | 34.55 | 3.14 | 6.16 | 7.03 |
Note. PTSD = posttraumatic stress disorder. Zero-order correlations appear above the diagonal and partial correlations (controlling for age and race/ethnicity) appear below the diagonal.
p < .07.
p < .05.
p < .01.
p < .001.
Results of analyses examining the relations of demographic variables to risky behaviors revealed significant associations between risky behaviors and both age (r = −.16, p < .05) and race/ethnicity (F [1,157] = 4.82, p < .05), with White (M = 6.68, SD = 3.11) versus non-White (M = 5.58, SD = 3.09) participants reporting greater engagement in risky behaviors.
3.2. Primary Analyses
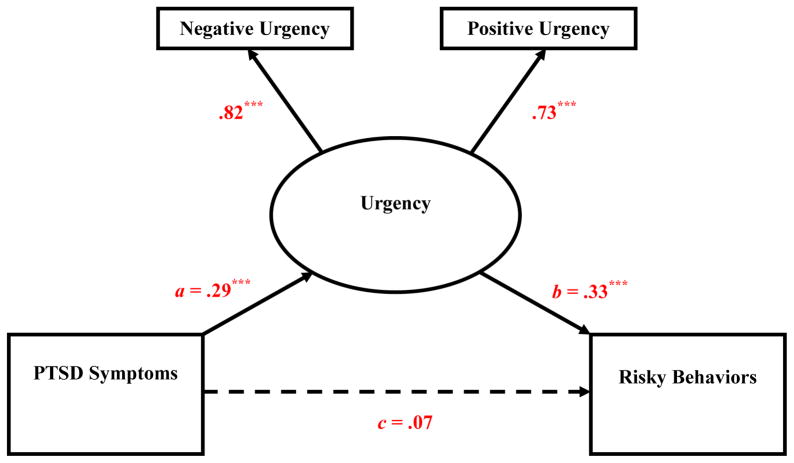
The final model provided an excellent fit to the data, χ2 (1) = 0.66, p = .416, NFI = .993, TLI = 1.022, CFI = 1.000, RMSEA = .000, PCLOSE = .501. (Age and race/ethnicity were included as covariates in the initial model; however, the direct effects linking these demographic variables to the dependent variable (i.e., risky behaviors) were non-significant and the model including age and race/ethnicity provided a poor fit to the data. As such, these variables were excluded from the final model.) Notably, although the zero-order relation between PTSD symptom severity and risky behaviors was significant (r = .16, p < .05), the direct effect of PTSD symptoms on risky behaviors when accounting for its indirect effect through urgency was not significant (β = .07, p = .42; see Figure 1). Rather, results revealed a significant indirect relation of PTSD symptoms to risky behaviors through the pathways of both negative urgency (β = .239, SE = .065, p = .001, 95% CI = 0.109 – 0.367) and positive urgency (β = .213, SE = .072, p = .003, 95% CI = 0.069 – 0.351). These findings provide support for the mediating roles of both negative and positive urgency in the relation between PTSD symptoms and risky behaviors.
Figure 1. Summary of Analyses Examining the Mediating Role of Negative and Positive Urgency in the Relation between Posttraumatic Stress Disorder Symptom Severity and Risky Behaviors (5,000 bootstrap samples; N = 158).
Note. Weights are reported in the figure using standardized estimates. Dashed lines indicate nonsignificant paths. a = effect of independent variable on the mediating variable. b = effect of the mediating variable on the dependent variable. c = direct effect of the independent variable on the dependent variable when accounting for its indirect effect through the mediating variable. *p ≤ .05. **p ≤ .01. ***p ≤ .001. Model Fit: χ2 (1) = 0.66, p = .416, NFI = .993, TLI = 1.022, CFI = 1.000, RMSEA = .000, PCLOSE = .501.
Likewise, separate models examining negative and positive urgency as mediators revealed a significant indirect effect of PTSD symptoms on risky behaviors through the pathway of negative urgency in the first model (β = .062, SE = .028, p = .001, 95% CI = 0.018 – 0.126) and positive urgency in the second model (β = .050, SE = .026, p = .005, 95% CI = 0.012 – 0.113). These results provide further support for the mediating roles of both negative and positive urgency in the relation between PTSD symptoms and risky behaviors.
4. DISCUSSION
The goal of the present study was to extend past literature by examining the mediating roles of negative and positive urgency in the association between PTSD symptoms and risky behaviors among trauma-exposed inpatients with SUD. Consistent with hypotheses, significant positive associations were found among PTSD symptoms, negative and positive urgency, and risky behaviors. Moreover, negative and positive urgency mediated the relation of PTSD symptoms to risky behaviors. This study is the first to document both a relation between PTSD symptoms and positive emotion dysregulation in the form of positive urgency and the mediating roles of negative and positive urgency in the association between PTSD symptoms and risky behaviors among an at-risk clinical sample of inpatients with SUD and a history of traumatic exposure. These findings are consistent with past research highlighting the independent contributions of positive and negative emotional dysfunction to both PTSD (e.g., Litz et al., 2000; Tull et al., 2007; Weiss et al., 2013a, 2012) and risky behaviors (see Cyders and Smith, 2007, 2008 for reviews), and suggest that difficulties controlling behaviors in the context of intense emotional arousal (both positive and negative) may explain the relation between PTSD and risky behaviors.
Future research should examine whether PTSD symptoms and/or risky behaviors among inpatients with PTSD-SUD are associated with other dimensions of emotion dysregulation (e.g., nonacceptance of negative and positive emotions and difficulties engaging in goal-directed behavior when experiencing negative and positive emotions, as measured by the Difficulties in Emotion Regulation Scale [Gratz and Roemer, 2004] and the Difficulties in Emotion Regulation Scale – Positive [Weiss et al., 2015], respectively). Such findings may speak to the utility of incorporating existing empirically-supported emotion regulation treatments, such as Emotion Regulation Group Therapy (Gratz et al., 2014), into standard SUD treatment for inpatients with co-occurring PTSD-SUD. Indeed, research provides support for the utility of this treatment in reducing risky behaviors among women with borderline personality disorder (Gratz and Tull, 2011; Gratz et al., 2014).
Although results of the present study add to the literature on the role of emotion dysregulation in risky behaviors among inpatients with co-occurring PTSD-SUD, several limitations warrant mention. First, the cross-sectional and correlational nature of the data precludes determination of the precise nature and direction of the relations examined. In particular, the extent to which risky behaviors emerge as a consequence of PTSD symptoms and subsequent negative and positive urgency as hypothesized, or contribute to PTSD symptoms and negative and positive urgency, remains unknown. Future research is needed to investigate the nature and direction of these relations through prospective, longitudinal investigations. Additionally, theory suggests that emotion dysregulation may also occur in response to low levels of positive emotional arousal (e.g., Cox and Klinger, 1988; Nock and Prinstein, 2004), and research suggests a link between low levels of positive affect and risky behaviors (e.g., Muehlenkamp et al., 2009; Smyth et al., 2007). As such, future research would benefit from clarifying the role of emotion dysregulation stemming from both low and high intensity negative and positive emotions in risky behaviors.
An additional limitation is the exclusive reliance on self-report measures of negative and positive urgency, responses to which may be influenced by an individual’s willingness and/or ability to report accurately on emotional responses. Future studies would benefit from the integration of behavioral and physiological measures of negative and positive urgency. Moreover, although our measure of risky behaviors was drawn from a well-established and empirically validated diagnostic interview for BPD and has been utilized in past research (see Weiss et al., 2012), the use of this item as a measure of risky behaviors has limited empirical support. Nonetheless, it is important to note that this item assesses a wide range of risky behaviors and allows for the determination of clinically-relevant levels of each behavior. Nevertheless, future research examining the psychometric properties of this and other more comprehensive measures of risky behaviors is needed. It also warrants mention that our measure of PTSD in the present study was based on the DSM-IV-TR classification of PTSD. Thus, research is needed to replicate these findings using DSM-5 guidelines for the assessment of PTSD. In addition, we examined lifetime versus current PTSD. Although individuals with past (but not current) PTSD exhibit less functional impairment than those with current PTSD, there is evidence that individuals with past PTSD continue to exhibit clinically-significant deficits across a variety of domains (e.g., addiction severity, mental health quality of life, distress, physiological reactivity) consistent with those observed among individuals with current PTSD (e.g., Carson et al., 2007; Reynolds et al., 2005; Parslow et al., 2000; Westphal et al., 2011). Likewise, previous studies have found that patients with substance dependence and lifetime PTSD exhibit significantly greater impairment than those without PTSD (Mills et al., 2005). Consequently, our examination of lifetime PTSD may not necessarily be a limitation. Nonetheless, future research is needed to replicate these findings and examine the utility of the proposed model among inpatients with current PTSD.
Further, although our focus on a high-risk sample of inpatients with SUD and a history of traumatic exposure is arguably a strength of this study, findings cannot be assumed to generalize to non-SUD populations and require replication across a more diverse group of patients with PTSD. For instance, our sample was comprised primarily of individuals who identified as White or African American. Consistent with extant research on some of the specific forms of risky behavior assessed here (e.g., substance use [Smith et al., 2006] and risky sexual behavior [Douglas et al., 1997]), risky behaviors varied as a function of race/ethnicity, with White versus non-White participants reporting more risky behaviors. However, other forms of risky behavior (e.g., interpersonal aggression [Caetano et al., 2000] and binge eating [Pike et al., in press]) have been found to be heightened among non-White versus White individuals. Indeed, research suggests that there may be differences in contextual- (e.g., access to opportunities for risky behaviors) and personality-oriented (e.g., attitudes towards risky behaviors, sensation seeking) risk factors for engagement in different risky behaviors across different racial/ethnic groups (e.g., Kurtz and Zuckerman, 1978; Wallace and Muroff, 2002). Thus, future research would benefit from examining moderated mediational models wherein these various risk factors are taken into account. Such research may assist in clarifying the specific factors that increase or decrease risk for risky behaviors among different racial/ethnic groups with PTSD and SUD, thereby contributing to the development of more personalized treatments for these behaviors.
Despite limitations, results of the present study extend extant research on the role of emotion dysregulation in the PTSD-risky behavior relation among inpatients with SUD and a history of traumatic exposure, highlighting the relevance of both negative and positive urgency to this relation. Although preliminary, these findings provide support for the potential utility of teaching inpatients with co-occurring PTSD-SUD skills for tolerating negative and positive emotional states without acting impulsively. For example, distress tolerance skills (see, e.g., Distress Tolerance Treatment [Brown et al., 2008] and Dialectical Behavior Therapy [Linehan, 1993]) may facilitate behavioral control in the context of negative and positive emotional states by redirecting attention to non-emotional stimuli and promoting more adaptive actions in the face of emotional arousal. Likewise, treatments that emphasize emotional acceptance and willingness (e.g., Acceptance and Commitment Therapy [Hayes et al., 1999]; Emotion Regulation Group Therapy [Gratz et al., 2014]) may reduce urgency stemming from negative and positive emotions by decreasing secondary emotional responses and increasing tolerance for previously-avoided emotions. Notably, treatments that target urgency and/or emotional avoidance have been found to result in reductions in distress intolerance and risky behaviors among inpatients with SUD (e.g., Brown et al., 2008, 2013; Dimeff et al., 2000; Gifford et al., 2004; Hayes et al., 2004; Linehan et al., 1999). Future research would benefit from examining whether these treatments result in improvements in both negative and positive urgency, as well as whether these improvements relate to reductions in risky behaviors. The utility of these treatments for inpatients with co-occurring PTSD-SUD in particular also needs to be examined. Likewise, it will be important to identify whether prevention efforts focused on teaching individuals with a history of traumatic exposure strategies for improving negative and positive urgency prevent the development of risky behaviors. Finally, given recent evidence to suggest that neurocognitive exercises to enhance working memory lead to improvements in delay discounting among inpatients with SUD (Bickel et al., 2011), future research would benefit from examining the impact of computerized cognitive remediation on risky behaviors.
Highlights.
Substance use disorder patients with PTSD exhibit heightened risky behaviors
PTSD symptoms are associated with clinically-relevant patterns of risky behaviors
Negative and positive urgency are mediators of the PTSD-risky behavior relation
Treatments targeting negative and positive urgency may reduce risky behaviors
Acknowledgments
Role of Funding Source
This study was funded by R21DA030587 of the National Institute on Drug Abuse of the National Institutes of Health, awarded to the second author (MTT). Work on this paper by the first author (NHW) was supported by National Institute on Drug Abuse Grant T32DA019426. The NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare.
Contributors
Authors NHW and MTT designed the study. NHW and KLDG wrote the first draft of the manuscript and completed statistical analyses. MTT, TPS, and KLG assisted in the completion of the final manuscript. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nicole H. Weiss, Email: nhweiss7@gmail.com, Yale University School of Medicine, 389 Whitney Avenue, New Haven, CT 06511
Matthew T. Tull, Email: mtull@umc.edu, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216
Tami P. Sullivan, Email: tami.sullivan@yale.edu, Yale University School of Medicine, 389 Whitney Avenue, New Haven, CT 06511
Katherine L. Dixon-Gordon, Email: katiedg@gmail.com, University of Massachusetts Amherst, 135 Hicks Way, Amherst, MA 01003-9271
Kim L. Gratz, Email: klgratz@aol.com, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216
References
- American Psychiatric Association [APA] Diagnostic And Statistical Manual Of Mental Disorders. APA; Washington, DC: 2013. [Google Scholar]
- Anestis MD, Selby EA, Joiner TE. The role of urgency in maladaptive behaviors. Behav Res Ther. 2007;45:3018–3029. doi: 10.1016/j.brat.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Amos (Vers. 19.0) SPSS Inc; Chicago, IL: 2010. [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. Am J Drug Alcohol Abuse. 2011;37:37–42. doi: 10.3109/00952990.2010.535582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without posttraumatic stress disorder: a comparison of substance use, trauma history and psychiatric comorbidity. Am J Addict. 2000;9:51–62. doi: 10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Person Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: is the active self a limited resource? J Person Soc Psychol. 1998;74:1252–1265. doi: 10.1037//0022-3514.74.5.1252. [DOI] [PubMed] [Google Scholar]
- Berg JM, Latzman RD, Bliwise NG, Lilienfeld SO. Parsing the heterogenity of impulsivity: A meta-analyttic review of the behavioral implications of the UPPS for psychopathology. Psychol Assess. doi: 10.1037/pas0000111. in press. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69:260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LN, Kaloupek DG, Klauminser G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. Behav Ther. 1990;18:187–188. [Google Scholar]
- Bollen KA. Structural Equations With Latent Variables. Wiley; New York, NY: 1989. [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Curr Dir Psychol Sci. 2004;13:206–209. [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brown RA, Palm KM, Strong DR, Lejuez CW, Kahler CW, Zvolensky MJ, Hayes SC, Wilson KG, Gifford EV. Distress tolerance treatment for early-lapse smokers: rationale, program description, and preliminary findings. Behav Modif. 2008;32:302–332. doi: 10.1177/0145445507309024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Reed KMP, Bloom EL, Minami H, Strong DR, Lejuez CW, Kahler CW, Zvolensky MJ, Gifford EV, Hayes SC. Development and preliminary randomized controlled trial of a distress tolerance treatment for smokers with a history of early lapse. Nicotine Tob Res. 2013;15:2005–2015. doi: 10.1093/ntr/ntt093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. 1992;21:230–258. [Google Scholar]
- Caetano R, Cunradi CB, Schafer J, Clark CL. Intimate partner violence and drinking patterns among White, Black, and Hispanic couples in the US. J Subst Abuse. 2000;11:123–138. doi: 10.1016/s0899-3289(00)00015-8. [DOI] [PubMed] [Google Scholar]
- Carson MA, Metzger LJ, Lasko NB, Paulus LA, Morse AE, Pitman RK, Orr SP. Physiologic reactivity to startling tones in female Vietnam nurse veterans with PTSD. J Trauma Stress. 2007;20:657–666. doi: 10.1002/jts.20218. [DOI] [PubMed] [Google Scholar]
- Cawley J, Ruhm C. The Economics Of Risky Health Behaviors. Elsevier; New York, NY: 2011. [Google Scholar]
- Cohen LR, Greenfield SF, Gordon S, Killeen T, Jiang H, Zhang Y, Hien DA. Survey of eating disorder symptoms among women in treatment for substance abuse. Am J Addict. 2010;19:245–251. doi: 10.1111/j.1521-0391.2010.00038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol Use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res. 2013;37:1441–1450. doi: 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox WM, Klinger E. A motivational model of alcohol use. J Abnorm Psychol. 1988;97:168–180. doi: 10.1037//0021-843x.97.2.168. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Flory K, Rainer S, Smith GT. The role of personality dispositions to risky behavior in predicting first-year college drinking. Addiction. 2009;104:193–202. doi: 10.1111/j.1360-0443.2008.02434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: positive and negative urgency. Person Individ Diff. 2007;43:839–850. [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Rizvi SL, Brown MZ, Linehan MM. Dialectical behavior therapy for substance abuse: a pilot application to methamphetamine-dependent women with borderline personality disorder. Cogn Behav Pract. 2000;7:457–468. [Google Scholar]
- Dixon-Gordon KL, Chapman AL, Weiss NH, Rosenthal MZ. A preliminary examination of the role of emotion differentiation in the relationship between borderline personality and urges for maladaptive behaviors. J Psychopathol Behav Assess. 2014;36:616–625. doi: 10.1007/s10862-014-9423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas KA, Collins JL, Warren C, Kann L, Gold R, Clayton S, Ross JG, Kolbe LJ. Results from the 1995 National College Health Risk Behavior Survey. J Am Coll Health. 1997;46:55–67. doi: 10.1080/07448489709595589. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, Williams TJ. Alcohol use and alcohol-related consequences: associations with emotion regulation difficulties. Am J Drug Alcohol Abuse. 2014;40:125–130. doi: 10.3109/00952990.2013.877920. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects? A survey of traumatic stress professionals. J Trauma Stress. 2005;18:541–545. doi: 10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition. New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- Fischer S, Smith GT, Annus A, Hendricks M. The relationship of neuroticism and urgency to negative consequences of alcohol use in women with bulimic symptoms. Person Individ Diff. 2007;43:1199–1209. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state:” A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behav Ther. 2004;35:689–705. [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychol Med. 2014;44:2099–2112. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54. [Google Scholar]
- Gratz KL, Tull MT. Emotion regulation as a mechanism of change in acceptance-and mindfulness-based treatments. In: Baer RA, editor. Assessing Mindfulness and Acceptance: Illuminating the Theory and Practice of Change. New Harbinger Publications; Oakland, CA: 2010a. pp. 105–133. [Google Scholar]
- Gratz KL, Tull MT. The relationship between emotion dysregulation and deliberate self-harm among inpatients with substance use disorders. Cogn Ther Res. 2010b;34:544–553. doi: 10.1007/s10608-009-9268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT. Extending research on the utility of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Personality Disorders: Theory, Research, and Treatment. 2011;2:316–326. doi: 10.1037/a0022144. [DOI] [PubMed] [Google Scholar]
- Gruber J, Mauss IB, Tamir M. A dark side of happiness? How, when, and why happiness is not always good. Perspect Psychol Sci. 2011;6:222–233. doi: 10.1177/1745691611406927. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance And Commitment Therapy: An Experiential Approach To Behavior Change. Guilford Press; New York, NY: 1999. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Bissett R, Piasecki M, Batten SV, Byrd M, Gregg J. A preliminary trial of twelve-step facilitation and acceptance and commitment therapy with polysubstance-abusing methadone-maintained opiate addicts. Behav Ther. 2004;35:667–688. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model. 1999;6:1–55. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Brooner RK, King VL, Stoller KB, Wertz J. Predictive validity of cocaine, sedative, and alcohol dependence diagnoses. J Consult Clin Psychol. 1998;66:168–173. doi: 10.1037//0022-006x.66.1.168. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles And Practice Of Structural Equation Modeling. Guilford Press; New York, NY: 2011. [Google Scholar]
- Kranzler HR, Kadden RM, Babor TF, Tennen H, Rounsaville BJ. Validity of the SCID in substance abuse patients. Addiction. 1996;91:859–868. [PubMed] [Google Scholar]
- Kurtz JP, Zuckerman M. Race and sex differences on the sensation seeking scales. Psychol Rep. 1978;43:529–530. [Google Scholar]
- Lavender JM, Happel K, Anestis MD, Tull MT, Gratz KL. The interactive role of distress tolerance and eating expectancies in bulimic symptoms among substance abusers. Eat Behav. 2015;16:88–91. doi: 10.1016/j.eatbeh.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Peterson CB, Crosby RD, Engel SG, Mitchell JE, Crow SJ, Smith TL, Klein MH, Goldschmidt AB. Dimensions of emotion dysregulation in bulimia nervosa. Eur Eat Disord Rev. 2014;22:212–216. doi: 10.1002/erv.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei P, Wu Q. Introduction to structural equation modeling: issues and practical considerations. Educational Measurement: Issues and Practice. 2007;26:33–43. [Google Scholar]
- Linehan MM. Cognitive Behavioral Treatment Of Borderline Personality Disorder. Guilford Press; New York, NY: 1993. [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical Behavior Therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, Weathers F. Emotional processing in posttraumatic stress disorder. J Abnorm Psychol. 2000;109:26–39. doi: 10.1037//0021-843x.109.1.26. [DOI] [PubMed] [Google Scholar]
- Long K, Felton JW, Lilienfeld SO, Lejuez CW. The role of emotion regulation in the relations between psychopathy factors and impulsive and premeditated aggression. Personality Disorders: Theory, Research, and Treatment. 2014;5:390–396. doi: 10.1037/per0000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCartney K, Burchinal MR, Bub KL. Best practices in quantitative methods for developmentalists. Monogr Soc Res Child Dev. 2006;71:1–145. doi: 10.1111/j.1540-5834.2006.07103001.x. [DOI] [PubMed] [Google Scholar]
- Mills KL, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): prevalence and correlates. Drug Alcohol Depend. 2005;77:243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Engel SG, Wadeson A, Crosby RD, Wonderlich SA, Simonich H, Mitchell JE. Emotional states preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. Behav Res Ther. 2009;47:83–87. doi: 10.1016/j.brat.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraven M, Tice DM, Baumeister RF. Self-control as a limited resource: regulatory depletion patterns. J Person Soc Psychol. 1998;74:774–789. doi: 10.1037//0022-3514.74.3.774. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. 2004;72:885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- Parslow RA, Jorm AF, O’Toole BI, Marshall RP, Grayson DA. Distress experienced by participants during an epidemiological survey of posttraumatic stress disorder. J Trauma Stress. 2000;13:465–471. doi: 10.1023/A:1007785308422. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Murray HW, Mannelli P, Gottheil E, Weinstein SP, Vergare MJ. Pre-treatment measures of impulsivity, aggression and sensation seeking are associated with treatment outcome for African-American cocaine-dependent patients. J Addict Dis. 2004;23:109–122. doi: 10.1300/J069v23n02_08. [DOI] [PubMed] [Google Scholar]
- Peters CLO, Enders C. A primer for the estimation of structural equation models in the presence of missing data: Maximum likelihood algorithms. Journal of Targeting, Measurement and Analysis for Marketing. 2002;11:81–95. [Google Scholar]
- Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, Fairburn CG. A comparison of Black and White women with binge eating disorder. Am J Psychiatry. doi: 10.1176/appi.ajp.158.9.1455. in press. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, Wagner AW. A preliminary investigation of the role of strategic withholding of emotions in PTSD. J Trauma Stress. 2001;14:149–156. [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Herqueta T, Baker R, Dunbar GC. The Mini International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Shorey RC, Brasfield H, Febres J, Stuart GL. An examination of the association between difficulties with emotion regulation and dating violence perpetration. J Aggress Maltreat Trauma. 2011;20:870–885. doi: 10.1080/10926771.2011.629342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skre I, Onstad S, Torgersen S, Kringlen E. High interrater reliability for the Structured Clinical Interview for DSM-III-R Axis I (SCID-I) Acta Psychiatr Scand. 1991;84:167–173. doi: 10.1111/j.1600-0447.1991.tb03123.x. [DOI] [PubMed] [Google Scholar]
- Smith SM, Stinson FS, Dawson DA, Goldstein R, Huang B, Grant BF. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:987–998. doi: 10.1017/S0033291706007690. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Tull MT, Jakupcak M, McFadden ME, Roemer L. The role of negative affect intensity and the fear of emotions in posttraumatic stress symptom severity among victims of childhood interpersonal violence. J Nerv Ment Dis. 2007;195:580–587. doi: 10.1097/NMD.0b013e318093ed5f. [DOI] [PubMed] [Google Scholar]
- Tull MT, Roemer L. Emotion regulation difficulties associated with the experience of uncued panic attacks: evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behav Ther. 2007;38:378–391. doi: 10.1016/j.beth.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Tull MT, Weiss NH, Adams CE, Gratz KL. The contribution of emotion regulation difficulties to risky sexual behavior within a sample of patients in residential substance abuse treatment. Addict Behav. 2012;37:1084–1092. doi: 10.1016/j.addbeh.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Weiss NH, McDermott MJ. Posttraumatic Stress Disorder And Impulsive And Risky Behavior: An Overview And Discussion Of Potential Mechanisms. Springer; New York, NY: in press. [Google Scholar]
- Wallace JM, Muroff JR. Preventing substance abuse among African American children and youth: Race differences in risk factor exposure and vulnerability. J Prim Prev. 2002;22:235–261. [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD Scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Duke AA, Sullivan TP. Probable posttraumatic stress disorder and women’s use of aggression in intimate relationships: the moderating role of alcohol dependence. J Trauma Stress. 2014;27:550–557. doi: 10.1002/jts.21960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, Lavender J. Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: the DERS-Positive. Behav Modif. 2015;39:431–453. doi: 10.1177/0145445514566504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, Tull MT. Explicating the role of emotion dysregulation in risky behaviors: a review and synthesis of the literature with directions for future research. Curr Opin Psychol. 2015;3:22–29. doi: 10.1016/j.copsyc.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, Tull MT. Emotion Regulation: Processes, Cognitive Effects And Social Consequences. Nova Science Publishers; Hauppauge, NY: Emotion Dysregulation And Risky, Self-Destructive, And Health Compromising Behaviors: A Review Of The Literature. in press. [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, Gratz KL. The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug Alcohol Depend. 2013a;128:45–51. doi: 10.1016/j.drugalcdep.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Borne ME, Gratz KL. Posttraumatic stress disorder symptom severity and HIV-risk behaviors among substance-dependent inpatients. AIDS Care. 2013b;25:1219–1226. doi: 10.1080/09540121.2013.764381. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Lavender J, Gratz KL. Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse Negl. 2013c;37:944–954. doi: 10.1016/j.chiabu.2013.03.014. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. J Anxiety Disord. 2012;26:453–458. doi: 10.1016/j.janxdis.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R, Neria Y. Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depress Anxiety. 2011;28:686–695. doi: 10.1002/da.20842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Person Individ Diff. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS Impulsive Behaviour Scale: a four-factor model of impulsivity. Eur J Person. 2005;19:559–574. [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Young L. Diagnostic Interview For DSM-IV personality Disorders. McLean Hospital; Boston, MA: 1996. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH. The collaborative longitudinal personality disorders study: reliability of axis I and II diagnoses. J Person Disord. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zapolski TCB, Cyders MA, Smith GT. Positive urgency predicts illegal drug use and risky sexual behavior. Psychol Addict Behav. 2009;23:348–354. doi: 10.1037/a0014684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zohrabian A, Philipson TJ. External costs of risky health behaviors associated with leading actual causes of death in the US: a review of the evidence and implications for future research. Int J Environ Res Public Health. 2010;7:2460–2472. doi: 10.3390/ijerph7062460. [DOI] [PMC free article] [PubMed] [Google Scholar]