Abstract
To provide a better understanding of the local immune system in the face and external genitalia, i.e., the oral floor, lower lip, palpebral conjunctiva, anus and penis, we examined the distribution and density of CD1a-positve Langerhans cells, CD8-positive suppressor T lymphocytes and CD68-positive macrophages using specimens from 8 male elderly cadavers. The density of Langerhans cells showed an individual difference of more than (or almost) 10-fold in the lip (oral floor). In the oral floor, Langerhans cells were often spherical. Submucosal or subcutaneous suppressor lymphocytes, especially rich in the oral floor and penile skin, migrated into the epithelium at 4 sites, except for the anus. In the conjunctiva, macrophage migration into the epithelium was seen in all 8 specimens. The density of suppressor lymphocytes showed a significant correlation between the oral floor and the lip (r=0.78). In contrast, the anal and penile skins showed no positive correlation in the density of all three types of immunoreactive cells examined. Overall, irrespective of the wide individual differences, the oral floor and conjunctiva seemed to be characterized by a rich content of all three cell types, whereas the penile skin was characterized by an abundance of suppressor lymphocytes. Based on the tables, as mean value, the relative abundance of three different cell types were as follows; CD1a-positive Langerhans cells (anus), CD8-positive lymphocytes (penis), and CD68-positive macrophages (lip). The present observations suggest that the local immune response is highly site-dependent, with a tendency for tolerance rather than rejection.
Keywords: Langerhans cells, CD8, CD68, Oral floor, Lip, Conjunctiva, Anal canal, Penis, Human anatomy
Introduction
Although CD1a-positive Langerhans cells in the squamous epithelia play a critical role in antigen presentation, to our knowledge, few studies have quantitatively evaluated regional differences in the density of Langerhans cells. In a rare example, Cruchley et al. [1] reported a regional difference in the oral mucosa: the dorsum of the tongue showed the highest density (28.3 cells per mm epithelial surface length) in comparison with a low density in the buccal mucosa, hard palate and floor of the mouth (16.7-17.6 cells). The first aim of the present study was to examine regional differences in Langerhans cell morphology among the oral mucosa, palpebral conjunctiva, anus and penis.
In contrast to antigen presentation, on the other hand, immune tolerance seems to play an important role in mucosal immunity, especially in the face, since numerous new antigens arrive via the mouth, nose and eye every day. However, there has been little or no information about distribution of CD8-positive suppressor T lymphocytes in the squamous epithelia and associated connective tissues along it. Likewise, little is known about the distribution of CD68-positve macrophages along the normal squamous epithelia, although in association with Langerhans cells, macrophages play an activation role [2,3,4,5] or a suppressor role [6,7] in local defense and inflammation. The latter suppressive role has been reported for alveolar macrophages. Both macrophages and Langerhans cells carry numerous Birbeck granules within the cytoplasm.
The second aim of this study was to examine regional differences in the density of macrophages and suppressor T lymphocytes under an assumption that the number of Langerhans cell correlates with that of the other two cell types. Fortunately, in paraffin sections from formalin-treated cadavers, immunostaining of CD8 and CD68 is much easier than that of other immune system markers such as CD4 and HLA-DR [8]. It is very difficult to obtain frozen specimens from multiple sites in young patients or volunteers. In contrast, specimens from elderly donated cadavers allow examination of multiple sites simultaneously. However, in such cadavers, it is not possible to avoid the influence of epithelial degeneration with aging. Nevertheless, it was expected that this preliminary study would help to clarify the normal morphology of these immunoreactive cells in elderly persons, especially various correlations among Langerhans cells, suppressor T lymphocytes and macrophages in and along the squamous epithelium, thus providing a better understanding of the local immune system at and around the external openings of the mucosal lumen.
Materials and Methods
The study was performed in accordance with the provisions of the Declaration of Helsinki 1995 (as revised in Edinburgh 2000). We examined 80 donated male cadavers ranging in age from 85 to 95 years, with a mean age of 89 years. As shown in Tables 1, 2, 3, the ages at death were 85 years (specimen A), 85 years (B), 86 years (C), 88 years (D), 89 years (E), 91 years (F), 94 years (G), and 95 years (H). The cause of death had been ischemic heart failure or intracranial bleeding. None of the cadavers appeared to have been catheterized during life, as the diameter of the penile urethra was normal in all cases. However, we had no information on whether oral feeding had not been possible. The cadavers had been donated to Tokyo Dental College for research and education on human anatomy, and their use for research had been approved by the university ethics committee. The donated cadavers had been fixed by arterial perfusion of 10% v/v formalin solution and stored in 50% v/v ethanol solution for more than 3 months. From each cadaver, we prepared 5 tissue blocks including (1) the oral floor mucosa near the sublingual gland, (2) the lower lip, (3) the palpebral conjunctiva covering the attachment site between the upper and lower eyelids, (4) the anal canal 2 cm below the columnar-squamous epithelial junction, and (5) the penile skin at the coronary sulcus (a groove of skin under the prepuce).
Table 1. Numbers of CD1a-positive Langerhans cells in a field of ×20 objective.
| Specimen | Oral floor | Lip | Conjunctiva | Anus | Penis |
|---|---|---|---|---|---|
| A | 18 | 88 | 24a) | 50 | 40 |
| B | 69 | 55b) | 36 | 69 | 32 |
| C | 52 | 22 | 25 | 26 | 43c) |
| D | 30 | 14 | 57 | 43 | 38 |
| E | 60 | 12 | 21 | ND | 29 |
| F | 12 | 35 | 32 | 60d) | 25 |
| G | 7 | 8 | 18 | 45 | ND |
| H | 66e) | 51 | 39 | 35 | 35 |
| Mean±SD | 39.3±23.8 | 35.8±26.1 | 31.5±11.8 | 47.0±13.5 | 34.6±5.9 |
The counting was performed at the hot spot (a site with highest density) in the section. Ages of each of the cadavers when he died were 85 (specimen A), 85 (B), 86 (C), 88 (D), 89 (E), 91 (F), 94 (G) and 95 (H), respectively. ND, a failure in the immunostaining or the other histological procedure. a)Fig. 3. b)Fig. 2. c)Fig. 5. d)Fig. 4. e)Fig. 1.
Table 2. Numbers of CD8-positive lymphocytes in a field of ×20 objective.
| Specimen | Oral floor | Lip | Conjunctiva | Anus | Penis |
|---|---|---|---|---|---|
| A | 82 (27) | 38 (4) | 146 (15)a) | 10 | 103 (32) |
| B | 89 (42) | 60 (16)b) | 25 (3) | 5 | 85 (12) |
| C | 98 (15) | 18 (15) | 131 (12) | 6 | 154 (64)c) |
| D | 26 (17) | 18 (5) | 48 (10) | 5 | 115 (35) |
| E | 45 (33) | 12 (3) | 62 (8) | ND | 95 (21) |
| F | 151 (84) | 73 (21) | 106 (7) | 6d) | 120 (45) |
| G | 82 (15) | 25 (9) | 56 (5) | 15 | ND |
| H | 108 (22)e) | 45 (10) | 31 (3) | 12 | 101 (12) |
| Mean±SD | 85.1±35.7 | 36.1±20.5 | 75.6±43.1 | 8.4±3.7 | 110.4±20.8 |
The same specimens as shown in Table 1. The counting was performed at the hot spot (a site with the highest density) in the section. Greater number (smaller number) for the oral mucosa, conjunctiva and penis: the greater number indicates total cell number per mm in the epithelium as well as in the submucosal or subcutaneous tissue within 0.1 mm from the epithelial base. The smaller number indicates cell numbers migrating into the epithelium. In the anus, CD8-positive lymphocytes were not seen in the epithelium. ND, a failure in the immunostainig or the other histological procedure. a)Fig. 3. b)Fig. 2. c)Fig. 5. d)Fig. 4. e)Fig. 1.
Table 3. Numbers of CD68-positive macrophages in a field of ×20 objective.
| Specimen | Oral floor | Lip | Conjunctiva | Anus | Penis |
|---|---|---|---|---|---|
| A | 107 | 142 | 135 (12)a) | 49 | 45 |
| B | 109 (11) | 126b) | 76 (8) | 25 | 25 |
| C | 53 | 84 | 135 (15) | 15 | 50c) |
| D | 132 (21) | 95 (8) | 105 (9) | 56 | 37 |
| E | 65 (3) | 171 (15) | 58 (3) | ND | 32 |
| F | 43 | 66 | 95 (15) | 15d) | 58 |
| G | 104 | 90 | 68 (11) | 12 | ND |
| H | 135e) | 106 | 45 (3) | 37 | 48 |
| Mean±SD | 93.5±33.1 | 110.0±3.1 | 89.6±31.7 | 29.9±16.4 | 42.1±10.6 |
The same specimens as shown in Table 1. The counting was performed at the hot spot (a site with the highest density) in the section. Numbers with parenthesis for the oral floor (specimens B, D, and E), the lip (specimen D and E) and conjunctiva (all specimens): cell numbers migrating into the epithelium. In the anus and penis, CD68-positive macrophages were not seen in the epithelium. ND, a failure in the immunostaining or the other histological procedure. a)Fig. 3. b)Fig. 2. c)Fig. 5. d)Fig. 4. e)Fig. 1.
Most sections were stained with hematoxylin and eosin (H&E), whereas others were used for immunohistochemistry. The primary antibodies used were (1) mouse monoclonal anti-human CD1a (1:100, Dako N1616, Dako, Glostrup, Denmark); (2) mouse monoclonal anti-human CD8 (1:100, Dako N1592); and (3) mouse monoclonal anti-human CD68 KP1 (1:100, Dako M0814). Pretreatment autoclaving was conducted in accordance with the manufacturer's instructions. The secondary antibody (Dako Chem Mate Envison Kit, Dako) was labeled with horseradish peroxidase (HRP), and antigen-antibody reactions were detected via the HRP-catalyzed reaction with diaminobenzidine. All samples were counterstained with hematoxylin. A negative control without a first antibody was set up for each of the specimens. Observations and photography were performed using a Nikon Eclipse 80 (Nikon, Tokyo, Japan).
The density of positive cells (number per visual field) was measured by manual counting under a ×20 objective lens. The field corresponding to a circle 0.8 mm in diameter contained an almost 1-mm surface length of slightly curved epithelium. For measurement, we chose one best section (clearly stained) from each of the three types of immunostainings of an individual structure. As CD8-positive cells and/or CS68-positive cells were often restricted to the submucosal or subcutaneous tissue, we also counted these cells in tissue within 0.2 mm from the base of the epithelium. This counting was performed at a hot spot (a site with the highest density) in each section: this is a routine method for evaluation of metastatic lymph vessels in specimens obtained surgically from cancer patients [9]. However, for convenience of comparison, we prepared the present figures at a single hot spot for one of the 3 cell types examined, such as for CD8-positive cells in Fig. 1. Statistical analyses were carried out using PASW version 18 (SPSS Inc., Chicago, IL, USA). The cell density data were analyzed using Tukey's test (Tables 4, 5, 6).
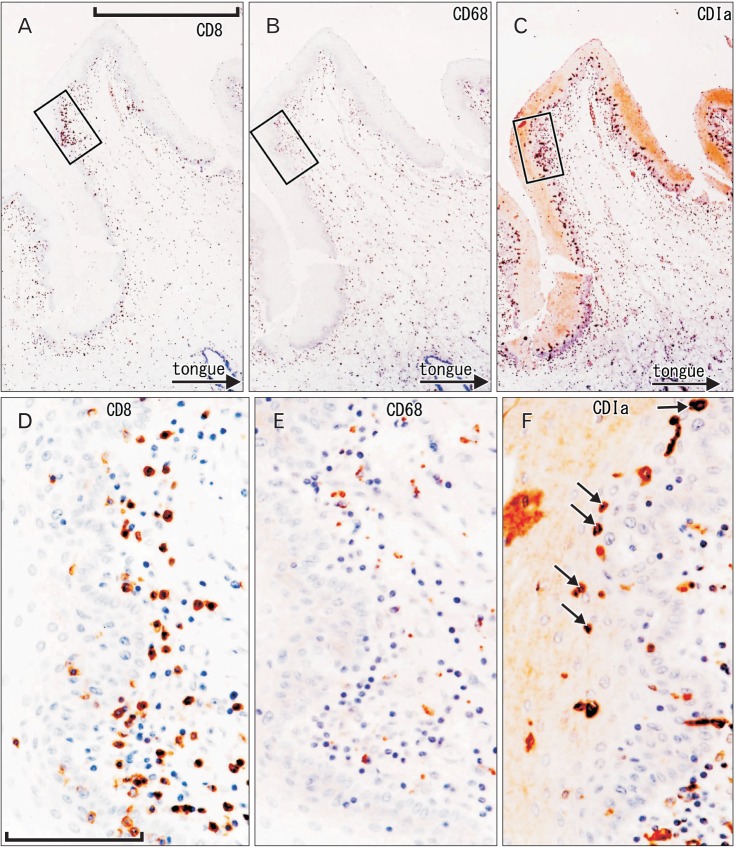
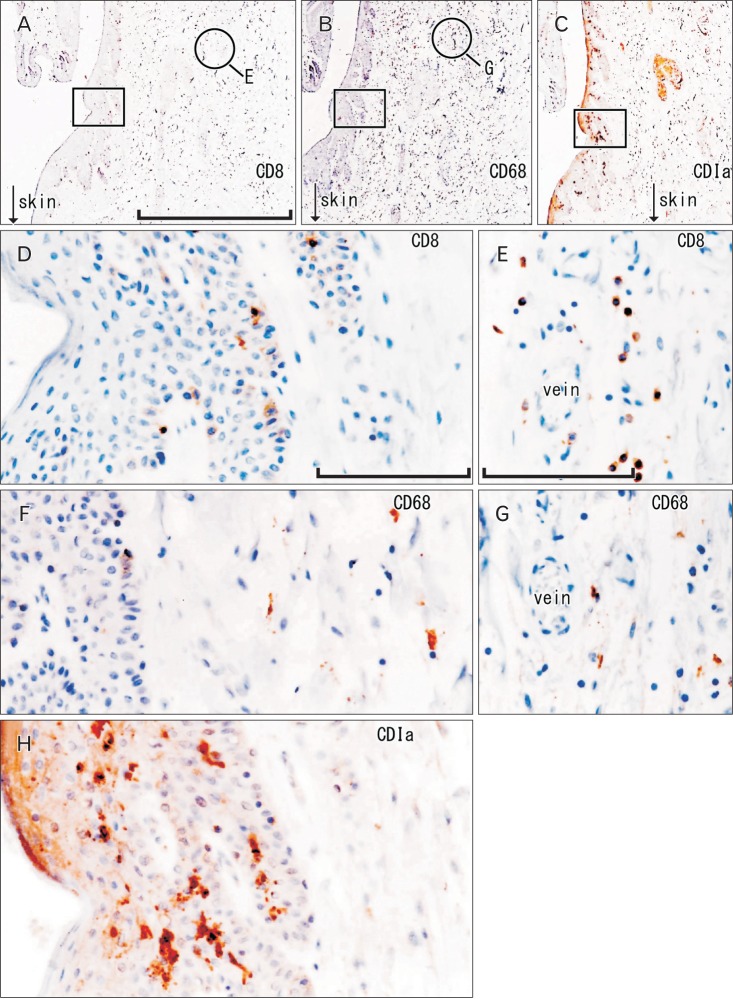
Fig. 1. CD1a-positive Langerhans cells, CD8-positive T lymphocytes, and CD68-positive macrophages in the oral floor mucosa. Immunohistochemistry of CD8 (A, D), CD68 (B, E), and CD1a (C, F). Panel (A-C) display the same mucosal fold using adjacent sections at the same magnification (scale bar in panel A=1 mm), while panels (D-F) correspond to square in panels (A-C), respectively at the same magnification (scale bar in panel D=0.1 mm). Thus, the positive cells do not show maximum density in panels (E) and (F). Some of suppressor lymphocytes have migrated into the epithelium (D), in contrast to macrophages (E). The epithelium contains abundant spherical Langerhans cells (arrows in panel F).
Table 4. Comparison of numbers of CD1a-positive Langerhans cells.
| Oral floor | Lip | Conjunctiva | Anus | Penis | |
|---|---|---|---|---|---|
| Oral floor | - | - | - | - | - |
| Lip | - | - | - | - | - |
| Conjunctiva | - | - | - | - | - |
| Anus | - | - | - | - | - |
| Penis | - | - | - | - | - |
*P<0.05 was considered to be the level of statistical significance.
Table 5. Comparison of numbers of CD8-positive lymphocytes.
| Oral floor | Lip | Conjunctiva | Anus | Penis | |
|---|---|---|---|---|---|
| Oral floor | - | * | - | * | - |
| Lip | * | - | - | - | * |
| Conjunctiva | - | - | - | * | - |
| Anus | * | - | * | - | * |
| Penis | - | * | - | * | - |
*P<0.05 was considered to be the level of statistical significance.
Table 6. Comparison of numbers of CD68-posirive macrophages.
| Oral floor | Lip | Conjunctiva | Anus | Penis | |
|---|---|---|---|---|---|
| Oral floor | - | - | - | * | * |
| Lip | - | - | - | * | * |
| Conjunctiva | - | - | - | * | * |
| Anus | * | * | * | - | - |
| Penis | * | * | * | - | - |
*P<0.05 was considered to be the level of statistical significance.
Results
Oral floor
The oral floor was characterized by a rich content of immunoreactive cells in the epithelium as well as the submucosal tissue (Fig. 1). CD1a-positive Langerhans cells were usually the least numerous among the three cell types examined (Tables 1, 2, 3). They were evenly distributed in the thick stratum spinosum of the squamous epithelium. The oral floor epithelium contained abundant type 2 Langerhans cells that were spherical rather than pyramidal in shape (Fig. 1F). This classification was made according to Jaitley and Saraswathi [10]. Thus, cells with long dendritic processes were few in number. The density of Langerhans cells showed almost a 10-fold individual difference in the oral floor (Table 1). CD8-positive suppressor lymphocytes were concentrated along the basal layer of the epithelium and some of them were seen to have migrated into the epithelium (Fig. 1D). CD68-positive macrophages were not evident in the epithelium. The epithelial thickness varied considerably between specimens (0.15-0.5 mm). Suppressor lymphocyte density showed a difference of more than 5-fold between individuals, but macrophages did not show such a large difference (Tables 2, 3).
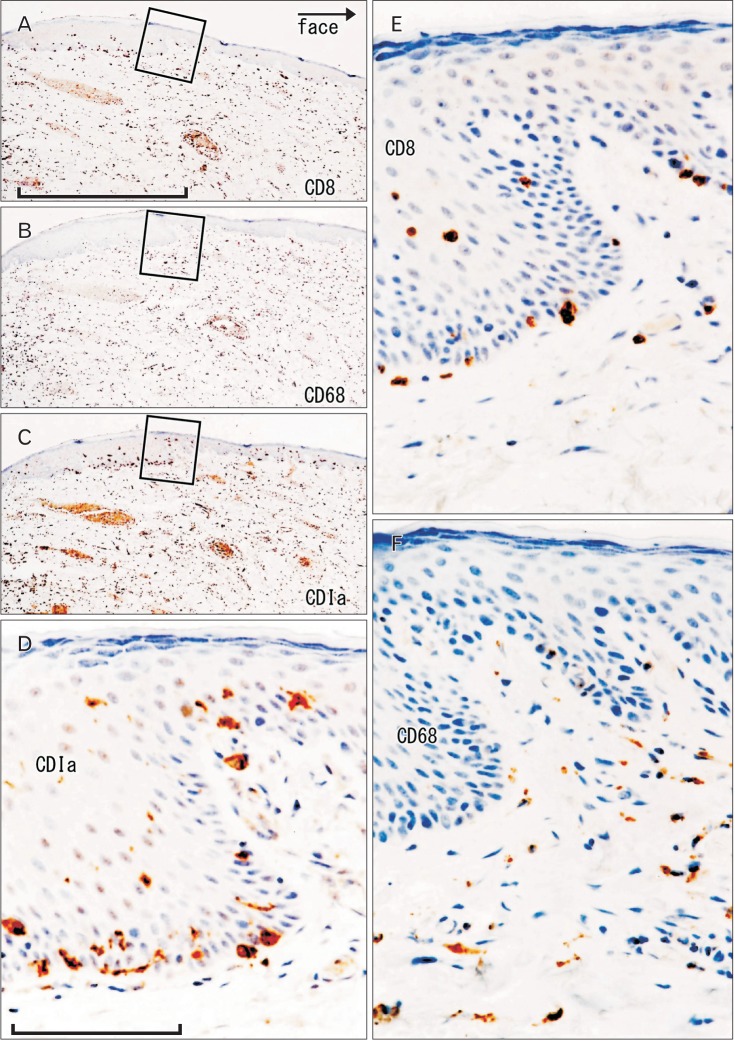
Lower lip
The lip of the mouth was also characterized by a rich content of immunoreactive cells (Fig. 2) despite the fact that the epithelial thickness (0.1-0.2 mm) was almost half that of the oral mucosa. Langerhans cells, most of which were highly dendritic, tended to be concentrated along the papilla. Langerhans cell density in the lip showed more than a 10-fold individual difference (Table 1). Suppressor lymphocytes always and macrophages sometimes were seen to have migrated into the epithelium, especially along the papilla. These cells were also richly distributed along thin subcutaneous vessels. Suppressor lymphocytes tended to be arranged along the basal layer of the epithelium. Cell-cell junctions in the stratum spinosum of the epithelium sometimes expressed CD8 reactivity (figure not shown). Suppressor lymphocytes were consistently fewer in number than on the oral floor of the same specimen. The density of suppressor lymphocytes showed more than a 5-fold difference between individuals, but macrophages did not exhibit such a great difference (Tables 2, 3).
Fig. 2. CD1a-positive Langerhans cells, CD8-positive T lymphocytes and CD68-positive macrophages in the lower lip. Immunohistochemistry of CD8 (A, E), CD68 (B, F), and CD1a (C, D). Panels (A-C) display the same site using adjacent sections at the same magnification (scale bar in panel A=1 mm), while panels (D-F) correspond to square in panels (A-C), respectively at the same magnification (scale bar in panel D=0.1 mm). Thus, the positive cells do not show maximum density (E, F).
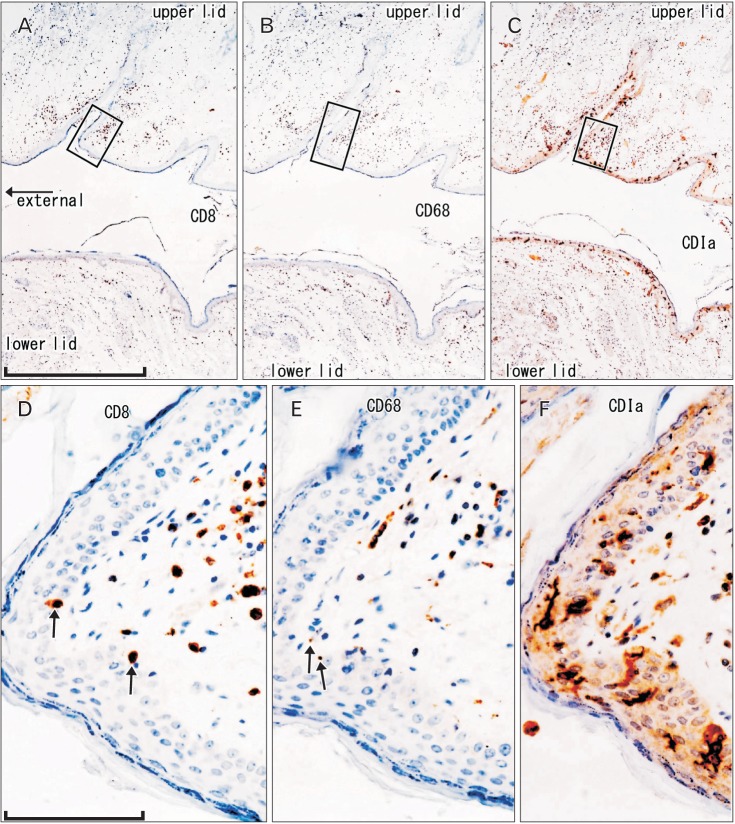
Palpebral conjunctiva
At a lower magnification, the palpebral conjunctiva usually exhibited a diffuse and dense distribution of the cells examined (Fig. 3). Langerhans cells were consistently less numerous than suppressor lymphocytes or macrophages (Tables 1, 2, 3). Especially in the upper eyelid, the conjunctiva usually contained abundant Langerhans cells with highly developed dendritic processes toward the epithelial surface (Fig. 3C, F). They were evenly distributed in the thin stratum spinosum of the squamous epithelium. In contrast, far fewer immunoreactive cells were seen in the bulbar conjunctiva (figure not shown). Short grooves of the palpebral conjunctiva tended to be covered by immunereactive cell-poor epithelium (Fig. 3A, B). In the conjunctiva, the highest cell density was usually seen at the attachment site between the upper and lower eyelids (Fig. 3A-C). Suppressor lymphocytes and/or macrophages were sometimes seen to have migrated into the squamous epithelium (Fig. 3D, E). The density of suppressor lymphocytes varied more than 5-fold between individuals, but macrophages did not show such a large difference (Tables 2, 3).
Fig. 3. CD1a-positive Langerhans cells, CD8-positive T lymphocytes, and CD68-positive macrophages in the palpebral conjunctiva. Immunohistochemistry of CD8 (A, D), CD68 (B, E), and CD1a (C, F). Panel (A-C) display the same mucosal grooves using adjacent sections at the same magnification (scale bar in panel A=1 mm), while panels (D-F) correspond to square in panels (A-C), respectively at the same magnification (scale bar in panel D=0.1 mm). Thus, the positive cells do not have maximum density (D, E). A few suppressor lymphocytes and macrophages have migrated into the epithelium (arrows in panels D and E). The epithelium contains abundant pyramidal or dendritic Langerhans cells (F).
Anal canal
The anal squamous epithelium was characterized by a low content of immunoreactive cells (Fig. 4). Among the three types of cells examined, Langerhans cells were usually th greatest in number, followed by macrophages, whereas suppressor lymphocytes were fewest (Tables 1, 2, 3, Fig. 4C). They tended to be concentrated in thick finger-like protrusions of the stratum spinosum between dermal papillae. Macrophages and lymphocytes were more richly distributed along the submucosal vessels than along the basal layer of the epithelium (Fig. 4E, G). The dendritic processes of Langerhans cells tended to extend in parallel with (not toward) the epithelial surface (Fig. 4H). In the anal canal, lymphocytes as well as macrophages were much more numerous in the columnar epithelium than in the squamous epithelium (figure not shown). The densities of all three cell types examined did not show great individual differences.
Fig. 4. CD1a-positive Langerhans cells, CD8-positive T lymphocytes, and CD68-positive macrophages in the anal canal. Immunohistochemistry of CD8 (A, D, E), CD68 (B, F, G), and CD1a (C, H). Panel (A-C) display the same mucosal groove using near sections at the same magnification (scale bar in panel A=1 mm), while panels (D), (F), and (H) correspond to square in panels (A-C) at the same magnification (scale bar in panel D=0.1 mm). Thus, the positive cells do not show maximum density (D, F). Panels (E) and (G) (scale bar in panel E=0.1 mm) show submucosal tissue around a vein (corresponding to circle in panels A and B, respectively). Suppressor lymphocytes as well as macrophages are concentrated not in and along the epithelium, but near the submucosal vessels (D-G). Langerhans cells extend in parallel with (not toward) the epithelial surface (H).
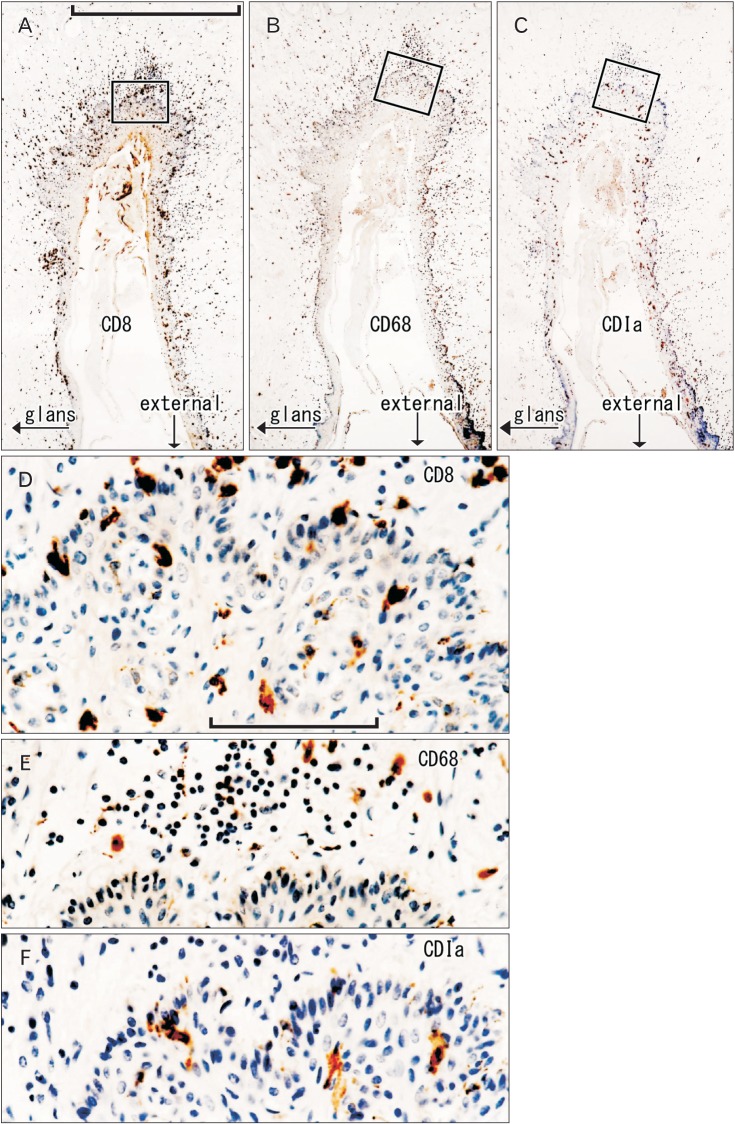
Penis
The distribution of immunoreactive cells in the penile skin was characterized by abundant suppressor lymphocytes migrating into the squamous epithelium (Fig. 5). The lymphocytes tended to be arranged along the basal layer of the epithelium. The density of suppressor lymphocytes was consistently greatest among the three cell types examined (Tables 1, 2, 3). Notably, intra-epithelial suppressor lymphocytes were pyramidal in shape, in contrast to their spherical form in the subcutaneous tissue (Fig. 5D). Observations using adjacent sections suggested that these pyramidal cells were unlikely to be double-positive for CD1a. The subcutaneous suppressor lymphocytes were more numerous at the bottom of the coronary sulci or grooves than in the skin around the sulci (Fig. 5A). Langerhans cells were also concentrated at the bottom of the sulci, and their dendritic processes were directed toward the epithelial surface (Fig. 5C, F). Macrophages in the penile skin were restricted to the subcutaneous tissue (Fig. 5B, E). The squamous epithelium at the urethral opening (i.e., the navicular fossa) also contained abundant suppressor lymphocytes and macrophages, but Langerhans cells were very sparse at the opening (figure not shown). The densities of all three cell types examined did not show a great individual difference such as that evident in the oral floor and lip.
Fig. 5. CD1a-positive Langerhans cells, CD8-positive T lymphocytes and CD68-positive macrophages in the penile skin. Immunohistochemistry of CD8 (A, D), CD68 (B, E), and CD1a (C, F). Panel (A-C) display the bottom of the coronary sulcus or groove under the penile prepuce using adjacent sections at the same magnification (scale bar in panel A=1 mm), while panels (D-F) correspond to square in panels (A-C), respectively at the same magnification (scale bar in panel D=0.1 mm). Thus, the positive cells do not show maximum density (E, F). Abundant suppressor lymphocytes have migrated into the epithelium (D), in contrast to macrophages (E). The epithelium contains pyramidal Langerhans cells (F).
Comparison among the five sites and statistical analysis
Table 7 summarizes the site-specific morphology of Langerhans cells, suppressor lymphocytes, and macrophages in and along the squamous epithelium. In the face, Langerhans cells were evenly distributed along the epithelium, whereas in the anus and penis they were concentrated. Abundant lymphocytes and macrophages, especially those showing migration into the epithelium, characterized the conjunctiva and penile skin.
Table 7. Summary of the distribution of CD1a-positive Langerhans cells, CD8-positive T lymphocytes, and CD68-positive macrophages.
| Langerhans cell | Other 2 cells | Migration to the epithelium | |
|---|---|---|---|
| Oral floor | Evenly, spherical | Rich | Lymphocyte ++, macrophage ± |
| Lower lip | Evenly, dendritic | Rich | Lymphocyte +, macrophage ± |
| Conjunctiva | Evenly, dendritic | Very rich | Lymphocyte +, macrophage ± |
| Anal canal | Concentrated, dendritica) | Few | Lymphocyte -, macrophage - |
| Penile skin | Concentrated, dendritic | Very rich | Lymphocyte ++, macrophage - |
Langerhans cell, CD1a-postivie cell; lymphocyte, CD8-positive cell; macrophage, CD68-posiive cell. Evenly or concentrated: they were evenly distributed along the epithelium or concentrated at the bottom of the skin groove (penile skin) or in finger-like protrusions of the stratum spinosum between papillae (anal canal). a)The dendritic cells were not directing toward the epithelial surface but lay in parallel with the epithelial surface.
The density of suppressor lymphocytes showed a significant correlation between the oral floor and the lip (r=0.78). In contrast, the anal and penile skins exhibited no positive correlation in the density of any of the three types of immunoreactive cells examined. The data for the oral floor and lip did not correlate with those for the anus and penis. In addition, the density of either suppressor lymphocytes or macrophages showed a weak correlation between the conjunctiva and the penis (r=0.59). At each of the five sites, there was no evident correlation between the density of Langerhans cells and that of coexisting macrophages or suppressor T lymphocytes.
Discussion
Because langerin, a specific marker of Langerhans cells, is a human immunodeficiency virus 1 receptor of epithelia [11], many researchers have been interested in the distribution of Langerhans cells in the oral mucosa and external genitalia. Another aspect of research on cell distribution has focused on a possible change in immunity after circumcision [12,13,14,15] reported details of this change in the microbiome of the penis. However, to our knowledge, no group has described the morphology of CD8-positive lymphocytes and CD68-positive macrophages in the same section, as used for observations of Langerhans cells. In the present study, the data suggested that a high density of Langerhans cells was often unlikely to correlate with the co-presence of abundant macrophages and/or suppressor lymphocytes.
The present study provided comparative data for Langerhans cells, suppressor lymphocytes and macrophages at five sites around external openings in the human body, although data for the penis were not based on observations of the urethral orifice but of the penile skin under the prepuce. Langerhans cells, dendritic in shape, were consistently abundant in the conjunctiva, anus and penis, but were sometimes few in the oral floor and lip. Notably, in the oral floor, Langerhans cells were often spherical, suggesting an inactive status. Submucosal or subcutaneous suppressor lymphocytes, especially rich in the oral floor and penile skin, were found to have migrated into the epithelium at four sites, with the exception of the anus. In the conjunctiva, macrophage migration into the epithelium was seen in all 8 specimens. The density of Langerhans cells displayed great individual variation in the lip and oral floor, although we could not rule out the possibility of degeneration due to reduction or loss of oral feeding. Irrespective of this great inter-individual difference, the oral floor and conjunctiva were characterized by rich contents of all three cell types, whereas the penile skin had abundant suppressor lymphocytes.
One of the striking features in the present observations was the migration of suppressor lymphocytes and/or macrophages into the epithelium. It was evident at four sites, with the exception of the anus, and the maximum proportion of migrating cells reached 50% (oral floor). We did not consider this rich infiltration to represent evidence of a possible allergic or inflammatory reaction, because the cell density was usually much higher in the epithelium than along and around the submucosal or subcutaneous vessels. We did not use CD4 antibody because of difficulty with immunostaining using specimens from fixed cadavers [8]. However, most of the round cells scattered in the epithelium were probably positive for CD8 or CD68. Conversely, we speculated that the proportion of other leukocytes was much lower than that of these positive cells. Since suppressor lymphocytes tended to be arranged along the basal layer of the epithelium, an interaction between the lymphocytes and Langerhans cells to create tolerance seemed likely [16]. Macrophages in the penis usually had a lower density than in the oral floor, in spite of usual exposure to rich antigens at both sites. In contrast, penile epithelial lymphocytes bore dendritic processes similar to those of Langerhans cells. Such differences might depend on the bacterial population at each site.
In the palpebral conjunctiva, we noted cell accumulation at the attachment site between the upper and lower eyelids. This site consistently receives mechanical stress due to blinking. The thin epithelium seemed to be an adaptation for the quick blinking movement. The rich content of intra-epithelial macrophages in the conjunctiva seemed to be necessary for recovery of tissues damage resulting from blinking. This hypothesis might also be applicable to the lip, with its high density of macrophages as well as thin epithelium. In contrast, in spite of the mechanical pressure resulting from defecation, the anus had relatively few macrophages. At the beginning of this study, we speculated that the density of macrophages would simply depend on the amount of foreign substances present at the site, and thus the anus and penis would have heavy exposure to such antigens. Surprisingly, however, the anal and penile skins exhibited no positive correlation in the density of all three types of immunoreactive cells examined. Thus a local immune response might occur in a highly site-dependent and individual manner, tending to favor tolerance rather than rejection.
The present study provided that the density of suppressor lymphocytes showed a significant correlation between the oral floor and the lip (r=0.78). This is attributed to the fact that the bacterial groups are similar in the oral floor and the lip. On the other hand, the density of either suppressor lymphocytes or macrophages showed a weak correlation between the conjunctiva and the penis (r=0.59). The penis and conjunctiva are touch frequently in daily life. Therefore, this is result from the fact that normal inhabitants in skin easily adhere to the penis and conjunctiva.
One great limitation may have been the fact that we had no information about the daily life and physiological status of the studied individuals, such as the regularity of eating and evacuation. The present data for Langerhans cell density in the oral mucosa (per ×20 objective field) were generally 2-3 times greater than those reported by Cruchley et al. [1] (per mm epithelial surface), largely due to the difference in the size of the field examined. However, the results of 2-dimensional counting of highly pyramidal cells appeared to depend on how many were spotted by the observer because of their long dendritic processes.
Acknowledgements
We are grateful to the individuals who donated their bodies after death to Tokyo Dental College for research and education on human anatomy without receiving any economic benefit. We also thank their families for agreeing to the donation, as well as their patience for waiting for the return of their remains after study.
References
- 1.Cruchley AT, Williams DM, Farthing PM, Lesch CA, Squier CA. Regional variation in Langerhans cell distribution and density in normal human oral mucosa determined using monoclonal antibodies against CD1, HLADR, HLADQ and HLADP. J Oral Pathol Med. 1989;18:510–516. doi: 10.1111/j.1600-0714.1989.tb01353.x. [DOI] [PubMed] [Google Scholar]
- 2.Linde N, Lederle W, Depner S, van Rooijen N, Gutschalk CM, Mueller MM. Vascular endothelial growth factor-induced skin carcinogenesis depends on recruitment and alternative activation of macrophages. J Pathol. 2012;227:17–28. doi: 10.1002/path.3989. [DOI] [PubMed] [Google Scholar]
- 3.Muthupalani S, Ge Z, Feng Y, Rickman B, Mobley M, McCabe A, Van Rooijen N, Fox JG. Systemic macrophage depletion inhibits Helicobacter bilis-induced proinflammatory cytokine-mediated typhlocolitis and impairs bacterial colonization dynamics in a BALB/c Rag2-/- mouse model of inflammatory bowel disease. Infect Immun. 2012;80:4388–4397. doi: 10.1128/IAI.00530-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou D, Chen YT, Chen F, Gallup M, Vijmasi T, Bahrami AF, Noble LB, van Rooijen N, McNamara NA. Critical involvement of macrophage infiltration in the development of Sjogren's syndrome-associated dry eye. Am J Pathol. 2012;181:753–760. doi: 10.1016/j.ajpath.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam RS, O'Brien-Simpson NM, Lenzo JC, Holden JA, Brammar GC, Walsh KA, McNaughtan JE, Rowler DK, Van Rooijen N, Reynolds EC. Macrophage depletion abates Porphyromonas gingivalis-induced alveolar bone resorption in mice. J Immunol. 2014;193:2349–2362. doi: 10.4049/jimmunol.1400853. [DOI] [PubMed] [Google Scholar]
- 6.Schneider C, Nobs SP, Heer AK, Kurrer M, Klinke G, van Rooijen N, Vogel J, Kopf M. Alveolar macrophages are essential for protection from respiratory failure and associated morbidity following influenza virus infection. PLoS Pathog. 2014;10:e1004053. doi: 10.1371/journal.ppat.1004053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaslona Z, Przybranowski S, Wilke C, van Rooijen N, Teitz-Tennenbaum S, Osterholzer JJ, Wilkinson JE, Moore BB, Peters-Golden M. Resident alveolar macrophages suppress, whereas recruited monocytes promote, allergic lung inflammation in murine models of asthma. J Immunol. 2014;193:4245–4253. doi: 10.4049/jimmunol.1400580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang SE, Kim JH, Yu HC, Murakami G, Cho BH. Lymphocyte subpopulations in the liver, spleen, intestines, and mesenteric nodes: an immunohistochemical study using human fetuses at 15-16 weeks. Anat Rec (Hoboken) 2014;297:1478–1489. doi: 10.1002/ar.22940. [DOI] [PubMed] [Google Scholar]
- 9.Weidner N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis: correlation in invasive breast carcinoma. N Engl J Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 10.Jaitley S, Saraswathi T. Pathophysiology of Langerhans cells. J Oral Maxillofac Pathol. 2012;16:239–244. doi: 10.4103/0973-029X.99077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Witte L, Nabatov A, Pion M, Fluitsma D, de Jong MA, de Gruijl T, Piguet V, van Kooyk Y, Geijtenbeek TB. Langerin is a natural barrier to HIV-1 transmission by Langerhans cells. Nat Med. 2007;13:367–371. doi: 10.1038/nm1541. [DOI] [PubMed] [Google Scholar]
- 12.Morelli AE, Ronchetti RD, Secchi AD, Cufré MA, Paredes A, Fainboim L. Assessment by planimetry of Langerhans' cell density in penile epithelium with human papillomavirus infection: changes observed after topical treatment. J Urol. 1992;147:1268–1273. doi: 10.1016/s0022-5347(17)37538-9. [DOI] [PubMed] [Google Scholar]
- 13.Balat A, Karakök M, Güler E, Uçaner N, Kibar Y. Local defense systems in the prepuce. Scand J Urol Nephrol. 2008;42:63–65. doi: 10.1080/00365590701472663. [DOI] [PubMed] [Google Scholar]
- 14.Qin Q, Zheng XY, Wang YY, Shen HF, Sun F, Ding W. Langerhans' cell density and degree of keratinization in foreskins of Chinese preschool boys and adults. Int Urol Nephrol. 2009;41:747–753. doi: 10.1007/s11255-008-9521-x. [DOI] [PubMed] [Google Scholar]
- 15.Price LB, Liu CM, Johnson KE, Aziz M, Lau MK, Bowers J, Ravel J, Keim PS, Serwadda D, Wawer MJ, Gray RH. The effects of circumcision on the penis microbiome. PLoS One. 2010;5:e8422. doi: 10.1371/journal.pone.0008422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polak ME, Newell L, Taraban VY, Pickard C, Healy E, Friedmann PS, Al-Shamkhani A, Ardern-Jones MR. CD70-CD27 interaction augments CD8+ T-cell activation by human epidermal Langerhans cells. J Invest Dermatol. 2012;132:1636–1644. doi: 10.1038/jid.2012.26. [DOI] [PubMed] [Google Scholar]