Abstract
Atraumatic splenic rupture is an uncommon complication of acute pancreatitis. This report describes the case of a 30-year-old man with acute pancreatitis and splenic vein thrombosis complicated by splenic rupture. The patient was admitted to the emergency department with pain in the upper abdomen that had been present for six hours and was associated with vomiting and sweating. He was diagnosed with acute pancreatitis of alcoholic etiology. Upon computed tomography (CT) of the abdomen, the pancreatitis was scored as Balthazar C grade, and a suspicious area of necrosis affecting 30% of the pancreas with splenic vein thrombosis was revealed. Seventy-two hours after admission, the patient had significant improvement in symptoms. However, he showed clinical worsening on the sixth day of hospitalization, with increasing abdominal distension and reduced hemoglobin levels. A CT angiography showed a large amount of free fluid in the abdominal cavity, along with a large splenic hematoma and contrast extravasation along the spleen artery. The patient subsequently underwent laparotomy, which showed hemoperitoneum due to rupture of the splenic parenchyma. A splenectomy was then performed, followed by ultrasound-guided percutaneous drainage.
Keywords: Acute pancreatitis, Pancreatitis, Rupture, Splenic rupture, Spontaneous
Core tip: This report describes a rare case of atraumatic splenic rupture that occurred in a 30-year-old male patient with acute pancreatitis and splenic vein thrombosis. A computed tomography angiography showed a large amount of free fluid in the abdominal cavity, along with a large splenic hematoma and contrast extravasation along the spleen artery. The patient underwent a splenectomy followed by ultrasound-guided percutaneous drainage.
INTRODUCTION
Atraumatic splenic rupture is a rarely reported complication of acute pancreatitis[1]. Approximately 10% of atraumatic splenic ruptures are related to local inflammatory processes[2]. These ruptures can be accompanied by other complications, such as perisplenic/intrasplenic pseudocysts, splenic infarction, subcapsular hematomas, and intrasplenic hemorrhage[3-6]. Morbidity and mortality rates for pancreatitis with splenic complications vary from 39% to 79% and 3.5% to 0.8%, respectively[7], demonstrating the importance of prompt recognition. This report describes a rare case involving a patient with acute pancreatitis and splenic vein thrombosis complicated by splenic rupture.
CASE REPORT
A 30-year-old man was admitted to the emergency department with pain in the upper abdomen that had been present for six hours accompanied by vomiting and sweating. He reported chronic alcoholic abuse, including recent consumption prior to the onset of symptoms. He had no other comorbidities. An initial examination showed normal blood pressure, a heart rate of 120 bpm, respiratory rate of 40 ipm, and a distended abdomen that was painful to palpation but with no signs of peritonitis. Laboratory exams showed: amylase, 199 IU/L; lipase, 410 U/L; C-reactive protein, 56 mg/L; WBC, 14.8 × 106/μL, hemoglobin, 18.1 g/dL hematocrit 52% pH7.30 HCO3, 12.7 mmol/L; lactate, 5.0 mmol/L. A diagnosis of alcoholic pancreatitis was confirmed. The Apache II classification was 2 at admission.
A computed tomography (CT) of the abdomen indicated that the pancreatitis was Balthazar grade C, and a suspicious area of necrosis affecting 30% of the pancreas with splenic vein thrombosis was observed (Figure 1). The patient was given antibiotics because of an increased C-reactive protein level (326 mg/L at 48 h after admission) and necrosis of the pancreas. The patient’s symptoms substantially improved after 72 h, with acceptance of an oral diet. However, clinical worsening occurred on the sixth day of hospitalization, with increasing abdominal distension and a reduced hemoglobin level (9.2 g/dL). Diagnostic paracentesis was then conducted on hematic content output. A subsequent CT angiography of the abdomen revealed a large amount of free fluid in the abdominal cavity, a large splenic hematoma, and contrast extravasation along the spleen artery (Figure 2).
Figure 1.
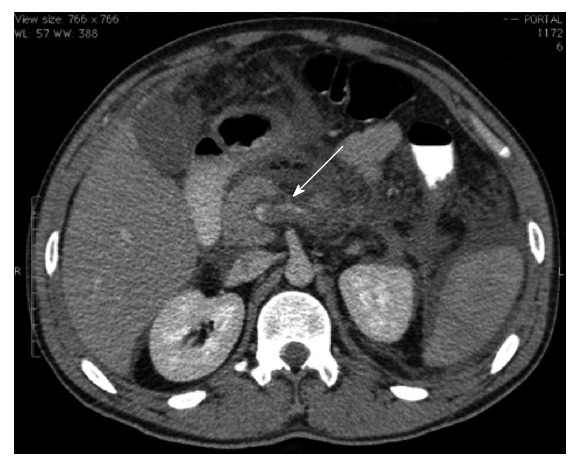
Abdominal computed tomography showing Balthazar C pancreatitis with splenic vein thrombosis (arrow).
Figure 2.
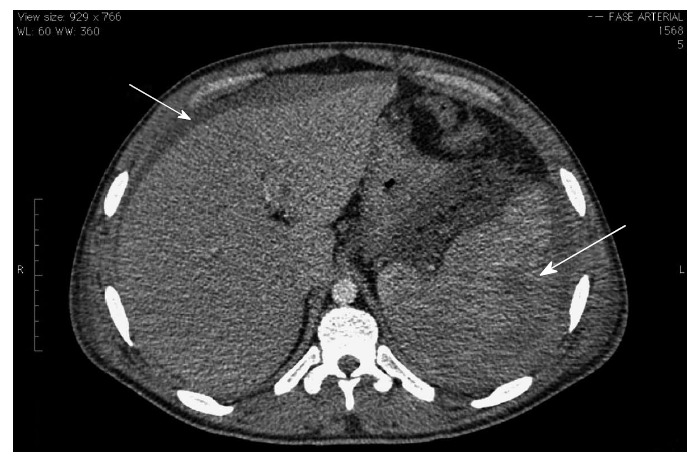
Abdominal computed tomography angiography showing a large amount of free fluid and a splenic hematoma (arrows).
The patient underwent a laparotomy, which showed hemoperitoneum due to the rupture of the splenic parenchyma and surrounding hematoma. A splenectomy was thus performed with cavity drainage. The patient was administered norepinephrine and blood components replacement. Six days after the operation, he was hemodynamically stable without vasoactive drugs and extubated; he showed acceptance of enteral nutrition and no signs of pancreatic fistula.
Forty-eight hours after withdrawal of antibiotics, on postoperative day 20, the patient exhibited a fever. Abdominal CT revealed peripancreatic collection of liquefied content and gas. He subsequently underwent ultrasound-guided percutaneous drainage with a Shiley catheter, which provided purulent content. CT performed after the procedure showed a significant decrease in the collection volume. Seven days after drainage, the fever returned and a second percutaneous procedure was performed, which resolved the fluid collection. The patient was subsequently discharged, with no complaints at a 30-d follow-up.
DISCUSSION
Splenic complications are considered rare events during the course of acute and chronic pancreatitis and have varied descriptions, including pseudocyst, subcapsular hematoma, splenic infarction, intrasplenic hemorrhage, and splenic rupture. Subcapsular hematomas, pseudocysts, and splenic rupture are more common in chronic pancreatitis[8], whereas splenic infarctions and intrasplenic hemorrhage tend to be more frequent in acute pancreatitis[9].
The anatomic relationship between the pancreatic tail and the splenic hilum contributes to the pathology of splenic complications[10]. For example, splenic rupture is more often described as a complication of chronic pancreatitis, where it occurs secondary to the enzymatic erosion of pseudocysts or as a result of direct action in the splenic parenchyma. In contrast, it has been reported in acute pancreatitis following splenic vein thrombosis, perisplenic adhesions, and acute inflammation of ectopic intrasplenic pancreatic tissue[3,8]. The cause of the splenic rupture in the present case was likely the splenic vein thrombosis observed in the first CT scan, as the histopathologic finding was sinusoidal hypertension in the spleen.
The diagnosis of splenic complications is challenging due to the absence of specific symptoms and signs. However, the presence of pain in the left upper quadrant and referred pain in the left shoulder are indications. Thus, CT is valuable for identifying splenic complications, as well as for patient follow-up, as demonstrated in the case presented here. Magnetic resonance imaging may also be useful, as it allows for better characterization of the various soft tissues and vascular alterations compared to CT[8]. Furthermore, the case presented here suggests that worsening of abdominal pain and distension followed by acute anemia are clinical indicators for diagnosis. A diagnostic paracentesis was also performed on the patient in this case, followed by CT angiography, which was used to locate the hemorrhage.
The treatment of splenic complications depends upon the hemodynamic status of the patient. A variety of treatments can be considered for patients who are hemodynamically stable, including a conservative approach, percutaneous drainage, angiography study, embolization, or even surgery. However, use of a conservative approach requires strict follow-up with serial ultrasound or CT. In contrast, surgical intervention with splenectomy or distal pancreatosplenectomy is convenient for patients who are hemodynamically unstable[8,9]. As the patient in the present case was hemodynamically stable, the first choice was angiography study followed by embolization. However, technical problems and clinical worsening of the patient led to the need for a laparotomy followed by splenectomy and drainage of the abdominal cavity. Importantly, despite signs of pancreatic necrosis, no necrosectomy was performed as the patient was treated for hemorrhagic complications rather than the pancreatitis. Indeed, necrosectomy is not recommended in the early phase of the disease[10], and thus, the maximal procedure recommended for this patient was drainage.
Even though splenic complications are rare conditions in both acute and chronic pancreatitis, clinical suspicion and prompt diagnosis using CT or other imaging methods are important for the patient’s prognosis. As this condition can change in a short period of time, early diagnosis followed by appropriate treatment can dramatically alter the morbidity and mortality associated with splenic rupture.
COMMENTS
Case characteristics
Thirty years old man with pain in the upper abdomen that had been present for six hours and associated with vomiting and sweating.
Clinical diagnosis
Acute pancreatitis.
Differential diagnosis
Subcapsular hematoma, intrasplenic haemorrhage, and necrotizing hemorrhagic pancreatitis.
Laboratory diagnosis
Amylase, 199 IU/L; Lipase, 410 U/L; C-reactive protein, 56 mg/L; WBC, 14.8 × 106/μL; hemoglobin, 18.1 g/dL hematocrit 52% pH7.30, HCO3, 12.7 mmol/L; lactate, 5.0 mmol/L.
Imaging diagnosis
Computed tomography (CT) of the abdomen showed Balthazar grade C with pancreatic necrosis and CT angiography revealed a large amount of free fluid in the abdominal cavity, a large splenic hematoma, and contrast extravasation along the spleen artery.
Treatment
Splenectomy was performed with cavity drainage.
Related reports
Atraumatic splenic rupture is a very rare complication of acute pancreatitis, with few reports in the literature.
Experiences and lessons
Even though splenic complications are rare, a clinical suspicion and prompt diagnosis are critically important for a positive patient prognosis; because this condition can change in a short period of time, an early diagnosis followed by appropriate treatment was helpful in this case.
Peer-review
The case report by Hernani et al presents a case of a young adult male who developed a splenic rupture associated with an episode acute pancreatitis. The authors briefly discuss the relationship of this complication to pancreatic inflammation, its presenting signs and symptoms, and recommended therapy.
Footnotes
Institutional review board statement: Approval was obtained from the local ethical committee for the publication of this report.
Informed consent statement: Written informed consent was obtained from the patient for the publication of this report.
Conflict-of-interest statement: The authors declare that they have no competing interests.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: April 12, 2015
First decision: May 13, 2015
Article in press: July 14, 2015
P- Reviewer: Kamer E, Poma EM, Sferra TJ
S- Editor: Ji FF L- Editor: A E- Editor: Li D
References
- 1.Toussi HR, Cross KS, Sheehan SJ, Bouchier-Hayes D, Leahy AL. Spontaneous splenic rupture: a rare complication of acute pancreatitis. Br J Surg. 1996;83:632. doi: 10.1002/bjs.1800830513. [DOI] [PubMed] [Google Scholar]
- 2.Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96:1114–1121. doi: 10.1002/bjs.6737. [DOI] [PubMed] [Google Scholar]
- 3.Patil PV, Khalil A, Thaha MA. Splenic parenchymal complications in pancreatitis. JOP. 2011;12:287–291. [PubMed] [Google Scholar]
- 4.Tseng CW, Chen CC, Chiang JH, Chang FY, Lin HC, Lee SD. Percutaneous drainage of large subcapsular hematoma of the spleen complicating acute pancreatitis. J Chin Med Assoc. 2008;71:92–95. doi: 10.1016/S1726-4901(08)70081-9. [DOI] [PubMed] [Google Scholar]
- 5.Gandhi V, Philip S, Maydeo A, Doctor N. Ruptured subcapsular giant haematoma of the spleen--a rare complication of acute pancreatitis. Trop Gastroenterol. 2010;31:123–124. [PubMed] [Google Scholar]
- 6.Mujtaba G, Josmi J, Arya M, Anand S. Spontaneous splenic rupture: a rare complication of acute pancreatitis in a patient with Crohn’s disease. Case Rep Gastroenterol. 2011;5:179–182. doi: 10.1159/000327215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lankisch PG. The spleen in inflammatory pancreatic disease. Gastroenterology. 1990;98:509–516. doi: 10.1016/0016-5085(90)90848-u. [DOI] [PubMed] [Google Scholar]
- 8.Heider R, Behrns KE. Pancreatic pseudocysts complicated by splenic parenchymal involvement: results of operative and percutaneous management. Pancreas. 2001;23:20–25. doi: 10.1097/00006676-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Mortelé KJ, Mergo PJ, Taylor HM, Ernst MD, Ros PR. Splenic and perisplenic involvement in acute pancreatitis: determination of prevalence and morphologic helical CT features. J Comput Assist Tomogr. 2001;25:50–54. doi: 10.1097/00004728-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Werner J, Hartwig W, Hackert T, Büchler MW. Surgery in the treatment of acute pancreatitis--open pancreatic necrosectomy. Scand J Surg. 2005;94:130–134. doi: 10.1177/145749690509400209. [DOI] [PubMed] [Google Scholar]


