Mammography screening is controversial and systematic reviews conducted by organisations with no conflicts of interest, such as the Nordic Cochrane Centre, the US and the Canadian Task Forces, the Independent UK Panel and the Swiss Medical Board have found substantial problems with the randomised trials.1–5 It is therefore difficult to know what the true effect is.
An additional problem is that trials are old. All but one started between 1963 and 1982,1 and back then, women did not receive much adjuvant therapy such as anti-hormonal treatment and chemotherapy.1 The introduction of effective drugs has reduced substantially the potential for screening to work. Screening can have no effect for women who, thanks to improved therapy, now live so much longer that they die of a heart attack before their breast cancer becomes life-threatening. Furthermore, as the effect of adjuvant therapy is largely independent of nodal status and other tumour characteristics,6 it works whether or not the cancer is detected ‘early’.
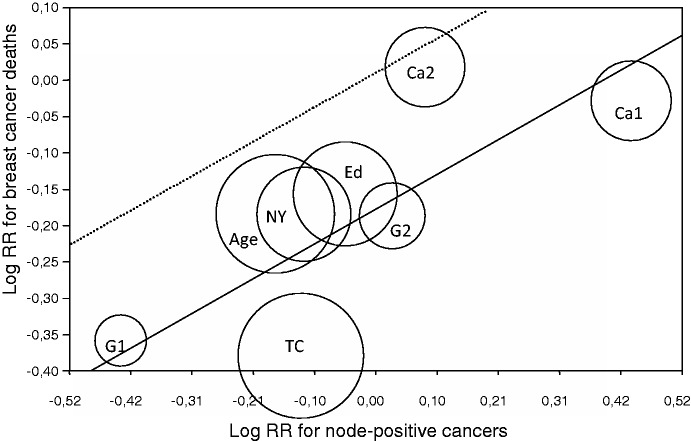
An additional, crucial problem is that the assessment of cause of death is biased in favour of screening. I documented this in our Cochrane review,1 and more recently also in a meta-regression analysis of the trials (Figure 1).7 One would expect to see the greatest reduction in breast cancer mortality in those trials that were most effective in lowering the rate of node-positive cancers in the screened group. This was indeed the case, but the regression predicts that a screening effectiveness of zero (i.e. the rate of node-positive cancers is the same in the screened group as in the control group) results in a 16% reduction in breast cancer mortality (95% confidence interval 9–23% reduction). This could only happen if there is bias, and further analyses showed that assessment of cause of death and of the number of cancers in advanced stages were both biased in favour of screening.7
Figure 1.
Meta-regression of the risk ratio for dying from breast cancer after 13 years in relation to the risk ratio for detecting node-positive breast cancer. The circled areas are proportional in size to the weights. The hatched line represents an unbiased regression line that crosses (0.0) and has the same slope as the calculated regression line. RR: risk ratio; Age: UK Age Trial, 39–41 years; Ca1: Canada, 40–49 years; Ca2: Canada, 50–59 years; Ed: Edinburgh, 45–64 years; G1: Göteborg, 40–49 years; G2: Göteborg, 50–59 years; Ma: Malmö, 45–70 years; NY: New York, 40–64 years; TC: Two-County, 40–74 years.
The effect of screening when it was introduced
Although the randomised trials now mainly have historical interest, they are still being heatedly debated.8 It is useful first to estimate what the effect on breast cancer mortality most likely was when screening was introduced about 25 years ago.
The average tumour size in the trials was 16 mm in the screened groups and 21 mm in the control groups.9 It takes only one more cell division for a 16-mm tumour to become one of 21 mm. For mammography screening to have more than a marginal effect, many cancers would need to metastasise in this little time window, which is less than one year.9 This is not plausible.
A large study found a linear correlation between tumour size and the risk of positive lymph nodes, and we calculated conservatively (as many metastases are overlooked) that tumours with a diameter of 16 mm have metastasised in 35% of the cases.9 If we assume that all patients with metastases will die from breast cancer, and those without would not, the expected effect of screening in the old trials is a 12% reduction in breast cancer mortality,9 in close agreement with the 10% reduction reported in the most reliable trials (the Canadian trial, the Malmö trial and the UK age trial) after 13 years.1 The true effect was likely smaller than 10%, however. The overdiagnosed tumours are smaller than other tumours, as they grow more slowly (length bias), and this inflates the difference in tumour size between the active and the control groups. Furthermore, as already noted, assessment of cause of death is biased.
The effect of screening today
A carefully conducted systematic review and other observational studies have found that screening does not decrease the incidence of advanced cancers, whether defined as those larger than 20 mm10 or belonging to higher stages.11 One study reported an 8% decline in late-stage cancer over 30 years,12 but that could easily have been caused by greater breast cancer awareness. In Denmark, for example, the average tumour size decreased by 9 mm in just 10 years, which was before screening was introduced.8
Many papers claiming that screening works have used relative rates, which is seriously misleading.8 Since screening adds many overdiagnosed, localised cancers to the screened group,1,13 the percentage of advanced cancers invariably goes down, but this cannot tell us anything about the possible benefit of screening.
As screening does not reduce the incidence of advanced cancers, we would not expect screening to have an effect on breast cancer mortality today. This is supported by observational studies. Denmark has a unique control group because, for 17 years, screening was only offered in 20% of the country. We found that the decline in breast cancer mortality in the relevant age group was 1% per year in the screening areas and 2% per year in the non-screening areas.14 There was also a control group in Norway, albeit less ideal, due to staggered introduction of screening, and a study found a 10% reduction in breast cancer mortality.15 However, this result was not statistically significant and most of the reduction was due to better treatment managed by interdisciplinary teams.15 Moreover, Norwegian researchers found no reduction in advanced cancers with screening.11
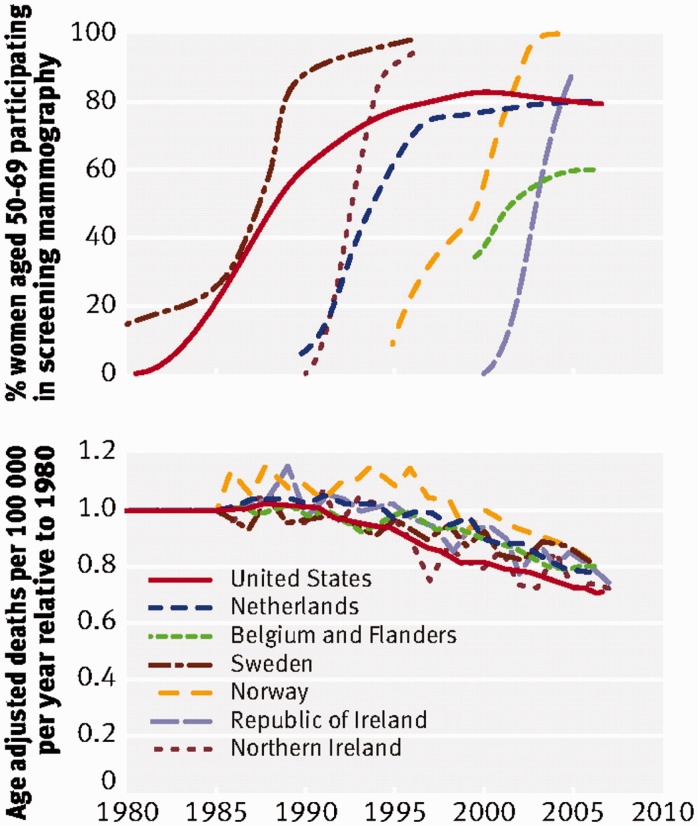
A study that compared three pairs of very similar neighbouring countries that had introduced screening 10–15 years apart16 found no relation at all between start of screening and the reduction in breast cancer mortality. The fall in breast cancer mortality started around 1990 in all countries, which was when effective treatments were introduced, and the rate of decline was about the same in all countries and also in the United States, where screening started as early as in Sweden, in the mid-1980s (Figure 2).17
Figure 2.
Top: Percentages of women participating in screening mammography in each country. Bottom: Change in national breast cancer mortality rate relative to country’s mean rate during 1980–1985.
Overdiagnosis
We took advantage of Denmark’s unique data and compared the trends in breast cancer incidence in screened and non-screened areas, taking into account changes in the background incidence before screening started and any compensatory drop in incidence of breast cancer among older, previously screened women (which provides an adjustment for lead time, i.e. the time screening advances detection of cancers). We found 33% overdiagnosis,18 somewhat less than in other countries, likely because of lower uptake, lower recall rates and deliberately lower detection rates of carcinoma in situ. In a systematic review of other countries with publicly organised screening programmes, we found 52% overdiagnosis.13
Many studies have used statistical modelling that incorporates an estimate of lead time. The problem with all of these studies is that they have used far too long estimates of lead time, several years. This overcompensation has had the effect that virtually all the overdiagnosis has been ‘modelled away’.8,9 The fundamental error with these models is that they do not distinguish between clinically relevant cancers, which would have appeared at a later time if there had not been screening, and the overdiagnosed cancers that would never have appeared. The models include all of them,19 but in actual fact, the lead time of clinically relevant cancers is less than a year.9,19
The effect of screening on total mortality
Breast cancer mortality is the wrong outcome. Not only because it is biased in favour of screening but also because the treatment of overdiagnosed, healthy women increases their risk of dying. Radiotherapy, for example, may cause deaths from heart disease, lung cancer and other cancers, and these iatrogenic deaths are not counted as breast cancer deaths.
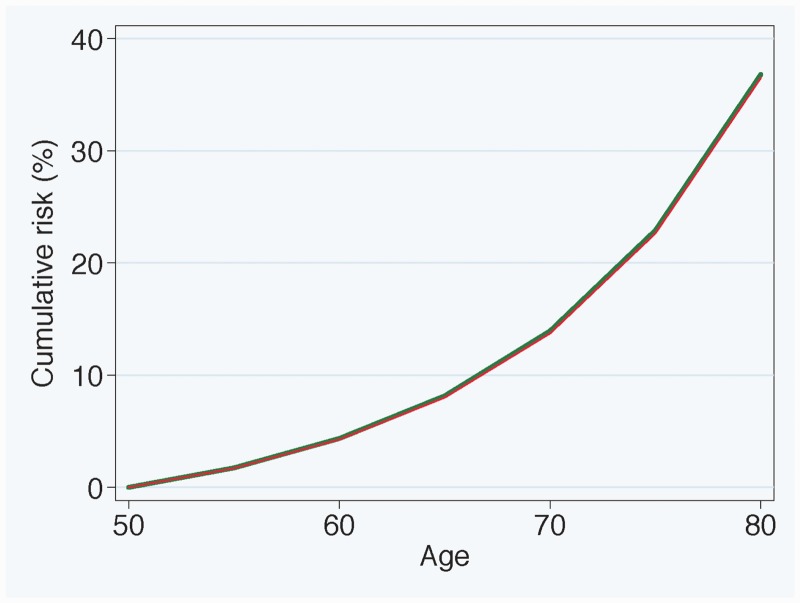
Figure 3 shows the effect of invitations to screening under three overly optimistic and partly erroneous assumptions: (1) screening reduces breast cancer mortality by 20%; (2) screening does not increase mortality from other causes; and (3) assessment of cause of death is not biased.20 The effect of screening on total mortality is barely visible.
Figure 3.
Cumulative risk of dying according to age for women invited to screening from age 50 years (red graph) and for women who are not invited (green graph) assuming screening reduces breast cancer mortality by 20% and does not increase deaths from other causes. Based on data for England and Wales for 2009 from Office for National Statistics. Reproduced with permission from Paul Pharoah.
If we take into account the cardiac and lung cancer deaths caused by radiotherapy and rather generously assume that screening reduces breast cancer mortality by 20% and results in 20% overdiagnosis, in accordance with the Independent UK Panel,4 there appears to be no mortality benefit.21 This result can be discussed, e.g. modern radiotherapy may be less harmful, but considering that screening does not reduce the rate of advanced cancers and therefore cannot work, it seems likely to me that screening increases total mortality. It is also noteworthy that the randomised trials did not find a trace of an effect on total cancer mortality, including breast cancer mortality (relative risk 1.00), although this was expected given the claimed effect on breast cancer mortality.1
Psychological harms of false-positive findings and overdiagnosed cancers
Generic questionnaires cannot capture fully the psychological consequences of breast screening.22 A Danish study was therefore based on a specially designed questionnaire that was developed using focus groups.22 Even after three years, women who had experienced a false-positive diagnosis had an anxiety level and other psychological problems that fell between that for women with breast cancer and women who were told they did not have cancer.22 Thus, the psychological harms of screening are substantial and long-lasting, and they affect a huge number of women, as the cumulative risk of a false-positive result after 10 mammograms is in the range of about 20% to 60%.1 Added to this comes the psychological harms inflicted on all the overdiagnosed women who do not know they are overdiagnosed but think they suffer from a fatal disease.
Utility analyses
An analysis of quality-adjusted life years that assumed a 15% reduction in breast cancer mortality showed that screening might have caused net harm for up to 10 years after the start of screening.23 This analysis was deliberately optimistic, however. It did not include the psychological harms caused by radiotherapy and chemotherapy; it assumed there were no reoperations (although 17% were reoperated); the duration of the quality-adjusted life year loss after a false-positive finding was set at only 0.2 years, although it is more than three years;22 and the analysis did not include the extra deaths caused by treatment of the overdiagnosed, healthy women.21
It is therefore clear that any utility analysis that takes account of these additional factors will come out negative. This was also the result of a recent utility assessment, although these investigators also used deliberately optimistic estimates and did not factor in all the harms.5,24
Conclusions
Mammography screening has been promoted to the public with three simple promises that all appear to be wrong: It saves lives and breasts by catching the cancers early. Screening does not seem to make the women live longer; it increases mastectomies;1,25 and cancers are not caught early, they are caught very late.9 They are also caught in too great numbers. There is so much overdiagnosis that the best thing a women can do to lower her risk of becoming a breast cancer patient is to avoid going to screening, which will lower her risk by one-third.13 We have written an information leaflet that exists in 16 languages on www.cochrane.dk, which we hope will make it easier for a woman to make an informed decision about whether or not to go to screening.
I believe that if screening had been a drug, it would have been withdrawn from the market long ago. Many drugs are withdrawn although they benefit many patients, when serious harms are reported in rather few patients. The situation with mammography screening is the opposite: Very few, if any, will benefit, whereas many will be harmed. I therefore believe it is appropriate that a nationally appointed body in Switzerland has now recommended that mammography screening should be stopped because it is harmful.5
Declarations
Competing interests
None declared
Funding
None declared
Ethical approval
Not applicable
Guarantor
PCG
Contributorship
Sole author
Provenance
Not commissioned; peer-reviewed by Michael Baum
References
- 1.Gøtzsche PC, Jørgensen KJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev 2013; 6: CD001877–CD001877. (first published in 2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002; 137: 347–360. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Task Force on Preventive Health Care, Tonelli M, Connor Gorber S, Joffres M, Dickinson J, Singh H, Lewin G, et al. Recommendations on screening for breast cancer in average-risk women aged 40–74 years. CMAJ 2011; 183: 1991–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012; 380: 1778–1786. [DOI] [PubMed] [Google Scholar]
- 5.Biller-Andorno N, Jüni P. Abolishing mammography screening programs? A view from the Swiss Medical Board. N Engl J Med 2014; 370: 1965–1967. [DOI] [PubMed] [Google Scholar]
- 6.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; 365: 1687–1717. [DOI] [PubMed] [Google Scholar]
- 7.Gøtzsche PC. Relation between breast cancer mortality and screening effectiveness: systematic review of the mammography trials. Dan Med Bull 2011; 58: A4246–A4246. [PubMed] [Google Scholar]
- 8.Gøtzsche PC. Mammography screening: truth, lies and controversy, London: Radcliffe, 2012. [DOI] [PubMed] [Google Scholar]
- 9.Gøtzsche PC, Jørgensen KJ, Zahl PH, Mæhlen J. Why mammography screening has not lived up to expectations from the randomised trials. Cancer Causes Control 2012; 23: 15–21. [DOI] [PubMed] [Google Scholar]
- 10.Autier P, Boniol M, Middleton R, Doré JF, Héry C, Zheng T, et al. Advanced breast cancer incidence following population-based mammographic screening. Ann Oncol 2011; 22: 1726–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalager M, Adami HO, Bretthauer M, Tamimi RM. Overdiagnosis of invasive breast cancer due to mammography screening: results from the Norwegian screening program. Ann Intern Med 2012; 156: 491–499. [DOI] [PubMed] [Google Scholar]
- 12.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 2012; 367: 1998–2005. [DOI] [PubMed] [Google Scholar]
- 13.Jørgensen KJ, Gøtzsche PC. Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ 2009; 339: b2587–b2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jørgensen KJ, Zahl PH, Gøtzsche PC. Breast cancer mortality in organised mammography screening in Denmark: comparative study. BMJ 2010; 340: c1241–c1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast-cancer mortality in Norway. N Engl J Med 2010; 363: 1203–1210. [DOI] [PubMed] [Google Scholar]
- 16.Autier P, Boniol M, Gavin A, Vatten LJ. Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ 2011; 343: d4411–d4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bleyer A. US breast cancer mortality is consistent with European data. BMJ 2011; 343: d5630–d5630. [DOI] [PubMed] [Google Scholar]
- 18.Jørgensen KJ, Zahl PH, Gøtzsche PC. Overdiagnosis in organised mammography screening in Denmark: a comparative study. BMC Womens Health 2009; 9: 36–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zahl PH, Jørgensen KJ, Gøtzsche PC. Overestimated lead times in cancer screening has led to substantial underestimation of overdiagnosis. Br J Cancer 2013; 109: 2014–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pharoah PD, Sewell B, Fitzsimmons D, Bennett HS, Pashayan N. Cost effectiveness of the NHS breast screening programme: life table model. BMJ 2013; 346: f2618–f2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baum M. Harms from breast cancer screening outweigh benefits if death caused by treatment is included. BMJ 2013; 346: f385–f385. [DOI] [PubMed] [Google Scholar]
- 22.Brodersen J, Siersma VD. Long-term psychosocial consequences of false-positive screening mammography. Ann Fam Med 2013; 11: 106–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raftery J, Chorozoglou M. Possible net harms of breast cancer screening: updated modelling of Forrest report. BMJ 2011; 343: d7627–d7627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swiss Medical Board. Systematisches Mammographie-Screening. See www.medicalboard.ch/fileadmin/docs/public/mb/Fachberichte/2013-12-15_Bericht_Mammographie_Final_Kurzfassung_e.pdf (last checked 15 December 2013).
- 25.Jørgensen KJ, Keen JD, Gøtzsche PC. Is mammographic screening justifiable considering its substantial overdiagnosis rate and minor effect on mortality? Radiology 2011; 260: 621–627. [DOI] [PubMed] [Google Scholar]