Abstract
Background
Current estimates from objective accelerometer data suggest that American adults are sedentary for ~7.7h/day. Historically, sedentary behaviour was conceptualized as one end of the physical activity spectrum but is increasingly being viewed as a behaviour distinct from physical activity.
Methods
Prospective studies examining the associations between screen time (watching television, watching videos and using a computer) and sitting time and fatal and non-fatal cardiovascular disease (CVD) were identified. These prospective studies relied on self-reported sedentary behaviour.
Results
The majority of prospective studies of screen time and sitting time has shown that greater sedentary time is associated with an increased risk of fatal and non-fatal CVD. Compared with the lowest levels of sedentary time, risk estimates ranged up to 1.68 for the highest level of sitting time and 2.25 for the highest level of screen time after adjustment for a series of covariates, including measures of physical activity. For six studies of screen time and CVD, the summary hazard ratio per 2-h increase was 1.17 (95% CI: 1.13–1.20). For two studies of sitting time, the summary hazard ratio per 2-h increase was 1.05 (95% CI: 1.01–1.09).
Conclusions
Future prospective studies using more objective measures of sedentary behaviour might prove helpful in quantifying better the risk between sedentary behaviour and CVD morbidity and mortality. This budding science may better shape future guideline development as well as clinical and public health interventions to reduce the amount of sedentary behaviour in modern societies.
Keywords: Cardiovascular diseases, prospective studies, sedentary lifestyle, television
Introduction
The first Surgeon General’s Report on Physical Activity and Health in 1996 summarized almost four decades of epidemiological research on various health and disease outcomes.1 This report marked a critical developmental milestone in raising the consciousness about the importance of physical activity in enhancing the health of Americans for both the public health community and general public and drew attention to the enormous public health burden of being the least active group in a population.
Technological innovations displaced many labour-intensive physical activities at work, in the home and for transportation. A recent review of US studies estimated that mean occupational energy expenditure may have decreased by 142 calories/day from 1960–62 to 2003–06 among men.2 New inventions, such as television and computers, led to a new paradigm of recreation that increasingly became sedentary during leisure time. The increasing popularity of the automobile ushered in an era of declining non-motorized transportation.
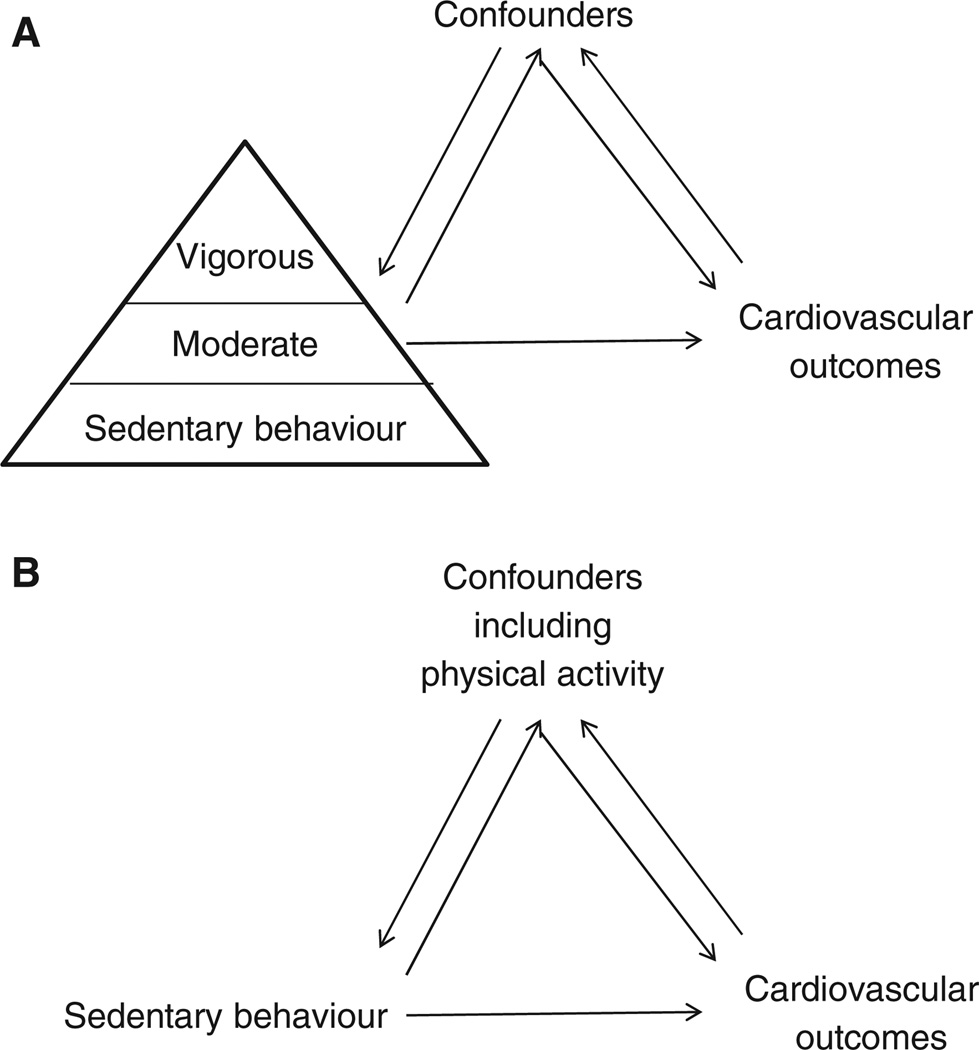
Historically, physical activity epidemiological research sought to unravel relationships between energy expenditure and health benefits.3 The resulting physical activity guidelines predicated on this research were largely oriented towards increasing physical activity levels in the population rather than reducing sedentary behaviour, per se.1 Most early researchers regarded time spent in sedentary behaviours during work, leisure and transportation as part of one end of a physical activity spectrum. An emerging conceptualization views sedentary behaviours as somewhat distinct from physical activity (Figure 1) and recognizes that, paradoxically, high levels of sedentary behaviour can coexist with high levels of total physical activity.4
Figure 1.
Traditional (A) and emerging (B) conceptualizations of the relationships between sedentary behaviour and physical activity and cardiovascular outcomes
In this review, our primary objective was to examine the relationship between sedentary behaviour and cardiovascular morbidity and mortality using prospective observational studies conducted largely during the past decade. Our secondary objectives were to summarize the evolution of epidemiological thought concerning possible adverse health effects of sedentary behaviour, present emerging evidence supporting links between sedentary behaviour and cardiovascular disease (CVD), illustrate the high prevalence of sedentary behaviour and review the limited evidence concerning mechanisms specific to sedentary behaviour underlying a possible association with CVD.
Defining sedentary behaviour
Activities having a metabolic expenditure ranging from 41.0 MET (one MET is resting energy expenditure set at 3.5 ml of oxygen/kg body mass/min) to ~1.5 METs are considered sedentary,5 although some researchers suggest the range should extend to 2.0 METs.6 Alternatively, because the MET value of quietly standing can be as little as 1.2, some have proposed that sedentary behaviour should be restricted to non-upright activities.7 Hence, definitional differences abound.
Generally, sleeping has a MET level of ~0.9 MET.8 Other sedentary activities include sitting, reading, meditating, relaxing, thinking, receiving a massage, watching television, using a computer, listening to music or the radio, talking on the telephone, writing letters, playing cards and riding in a car. Most of these activities involve basically sitting. However, tabled MET values for different types of sitting range from 1.0 to >2.0. Although not synonymous, sedentary behaviour and sitting clearly overlap.
Sedentary behaviours exist in many contexts: occupation, household, leisure-time and transportation.
Measuring sedentary behaviour
Researchers have used at least four methods to assess sedentary behaviour. Firstly, in occupational studies, those using job ratings developed by experts have crudely categorized workers into some framework.
Secondly, researchers have estimated sedentary behaviour from generally brief questionnaires. This method predominates in more recent prospective studies of the relationship between sedentary behaviour and adverse health events.
Thirdly, heart rate monitors can be used to assess sedentary behaviour.9,10
Finally, accelerometers that can objectively assess sedentary behaviour have advanced greatly with improved utility and falling unit costs. They have become increasingly attractive for large population-based studies, such as recent cycles of the National Health and Nutrition Examination Survey (NHANES) of the US population.11–13
Prevalence of sedentary behaviour
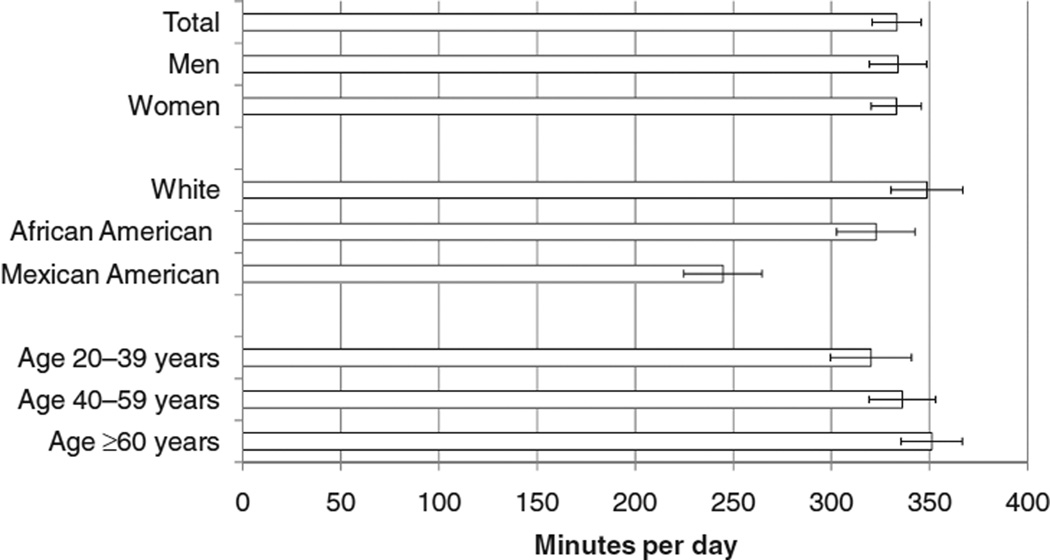
Adults in many Western countries spend large parts of their days being sedentary—up to half of a day for employed persons.14 Nielsen Inc. reported that the average American in 2010 spent ~35 h/week watching TV, 2 h watching time-shifted TV, 20 min watching online videos, 4 min watching mobile video and 4 h on the internet.15 Hence, time spent on screen viewing was the most common sedentary leisure-time behaviour.3,16 Data from the National Human Activity Pattern Survey showed that the most common sedentary activities, when ranked by the percentage of waking hours, were driving a car (10.9%), office work (9.2%), watching television or a movie (8.6%), performing various activities while sitting quietly (5.8%), eating (5.3%) and talking to someone in person or over the phone (3.8%).17 When asked, ‘How much time do you usually spend sitting or reclining on a typical day?’, US adults reported on average ~5.5 h/day during 2007–08, with nearly equal amounts for men and women, greater amounts for Whites than for African Americans and Mexican Americans and increasing amounts with increasing age (Ford ES, personal observations from NHANES) (Figure 2). In contrast, accelerometer measurements revealed average sedentary time to be 7.7 h/day, also with little difference between men and women.13 Australian adults showed that participants were sedentary for 57% of the time that an accelerometer was worn.18 If sleeping time is included as sedentary time, people may average ~75% of the day being sedentary.7 Regarding transportation, the average one-way commuting time in USA in 2009 was 25.1 min.19
Figure 2.
Age-adjusted and unadjusted mean time (95% CI) spent in sedentary behaviour per day among adults aged 20 years or older, NHANES 2007–08. The following question was asked about sitting or reclining work, at home or at school: ‘Include time spent sitting at a desk, sitting with friends, travelling in a car, bus or train, reading, playing cards, watching television or using a computer. Do not include time spent sleeping. How much time do you/usually spend sitting or reclining on a typical day?’
Methods
To identify prospective studies of sedentary behaviour and cardiovascular incidence and mortality, we executed a search strategy using the PubMed database (Supplementary data are available at IJE online). After reviewing 1304 citations produced by that search, we reviewed 37 articles in depth. In addition, we examined the bibliographies of articles that we reviewed. Studies had to be prospective, have incidence or mortality from CVD as an outcome, specifically assess sedentary behaviour (screen time and sitting) and be conducted on adults. We limited our search to publications written in English and did not contact authors for additional information. At the conclusion of this process, we were left with nine studies. Both authors abstracted the following data elements: author, year of publication, exposure categories, hazard ratios, 95% confidence intervals (CIs), adjustment variables, cardiovascular outcome, number of cardiovascular events and number of participants. Meta-analyses of the dose–response relationships for screen time or sitting time were performed. For screen time, we used the estimates of relative risk per 2 h of screen time that were previously calculated.20 For newer studies of screen time and studies of sitting time, we calculated estimated relative risks per 2 h/day of screen time from categories of sedentary behaviour.21 For each study, a standard error was derived from the CI and a weight was calculated as the inverse of the variance (1/SE2). Heterogeneity was assessed with the Q statistic and I.22,23 Depending on these statistics, fixed effect or random effect estimated relative risks were calculated. Stata 10 was used to conduct the analyses.
Prospective studies
Occupational studies
A seminal study by Morris et al.24 was conducted using about 31 000 employees aged 35–64 years of the London Transport Executive, who were followed during 1949–50. When compared with conductors, bus drivers had about double the age-adjusted rate of fatal coronary heart disease (CHD), but a similar rate of non-fatal CHD. This was the first indication that sedentary behaviour could markedly increase CHD risk. The authors also presented data on a larger second cohort of male civil servants and post office employees aged 35–59 years, followed during 1949–50 (179 726 person-years of follow-up). Based on job-related physical activity, participants were grouped into three categories: sedentary, intermediate and relatively much physical activity. The corresponding age-adjusted rates (per 1000 person-years) of fatal and non-fatal CHD were 2.4, 2.0 and 1.8, respectively.
Subsequent prospective studies used various methods to examine whether drivers in the transportation industry had an increased risk for CVD.25–33 A Swedish study found a 3-fold greater risk for fatal and non-fatal CHD among urban bus and tram drivers compared with members of other occupations after adjustment for a wide variety of confounders.33 Interestingly, lorry drivers were not at increased risk, a finding that the authors attributed to less job stress and air pollution exposure than that experienced by urban drivers. This study suggests caution in interpreting transportation studies.
Other prospective occupational studies examined the links between occupational sitting or sedentariness and CVD. A review of six such studies, each using questionnaires to assess sedentariness, failed to reach a definitive conclusion about the effect of occupational sedentary behaviour on CVD.14 Four studies showed increased estimated relative risks for the most sedentary compared with the most active group,34–37 whereas in two studies, the 95% CI included unity.38,39 Only three reviewed studies adjusted for non-occupational physical activity.35–37
Although not entirely consistent, occupational studies suggested that high levels of sedentary behaviour at work may increase the risk of developing CVD. Study limitations abounded, including a lack of CVD risk factor data for statistical adjustment, a lack of follow-up of employees who left their jobs and limited generalizability of findings. Also, in many occupational studies, the healthy worker effect must be considered—even when internal comparisons are analysed.40 These studies did not examine the separate contributions of sedentary behaviour and physical activity to CVD outcomes.
Population-based cohort studies
Sitting
Several prospective studies examined the links between time spent sitting and CVD (Table 1). In the Women’s Health Initiative, 73 743 postmeno-pausal women aged 50–79 years were followed for an average of 5.9 years during which time 1551 cardiovascular events occurred.41 A questionnaire assessed daily time spent sitting. Compared with women who sat <4 h/day, those who sat for ≥16 h/day had an increased risk of developing a fatal or non-fatal event (adjusted hazard ratio [aHR] = 1.68, 95% CI: 1.07–2.64).
Table 1.
Summary of findings from prospective studies examining links between sedentary behaviour and cardiovascular outcomes
| Reference | Sample size, gender and age |
No. of events |
Exclusions | Follow-up (years) |
Sedentary categories |
Hazard ratio (95% CI) |
Adjustment factors | Measurement of physical activity |
|---|---|---|---|---|---|---|---|---|
| Sitting | ||||||||
| Manson et al. 200241 |
73 743 postmeno- pausal women, 50–79 years |
1551 total CV events, 345 inci- dent CHD |
Predicted survival <3 years; alcoholism; mental illness; dementia; history of CHD, stroke, cancer; non- ambulatory |
5.9 | ≥ 16 vs <4h/day | 1.68 (1.07–2.64) | Age, energy expenditure |
Weekly MET score derived from detailed question- naire of mild, moderate or vigorous recreational physical activities |
| Katzmarzyk et al. 200942 |
17 013 men and women, 18–90 years |
759 CVD deaths |
None stated | 12.0 | Almost none of the time |
1.00 | Age, smoking, alcohol use, leisure-time physical activity, Physical Activity Readiness Questionnaire |
Average weekly MET-hours during 12-month period |
| ~l/4 of the time | 1.01 (0.77–1.31) | |||||||
| ~l/2 of the time | 1.22 (0.94–1.60) | |||||||
| ~3/4 of the time | 1.47 (1.09–1.96) | |||||||
| Almost all the time |
1.54 (1.09–2.17) | |||||||
| Patel et al. 201043 |
69 776 women, 50–74 years |
2360 CVD deaths |
History of cancer, heart attack, emphysema/other lung disease; no daily life activities; no light housekeeping; deaths within first year |
14 | <3 h/day | 1.00 | Age, race, marital status, edu- cation, smoking status, body mass index, alcohol use, energy intake, comorbidities score, total physical activity |
Average MET-hours per week during past year for recreational and daily life activities |
| 3–5 h/day | 1.20 (1.10–1.32) | |||||||
| ≥6 h/day | 1.33 (1.17–1.52) | |||||||
| 53 440 men, 50–74 years |
4009 CVD deaths |
<3 h/day | 1.00 | |||||
| 3–5 h/day | 1.06 (0.99–1.14) | |||||||
| ≥6 h/day | 1.18 (1.08–1.30) | |||||||
| Matthews et al. 201244 |
240 819 men and women, 50–71 years |
4684 CV deaths |
History of cancer, CVD, respiratory disease |
8.5 | <3 h/day | 1.00 | Age, gender, race, education, smoking history, diet quality, moderate-vigorous physical activity |
Average time spent each week in activities of at least a moderate intensity in the past 10 years |
| 3–4 h/day | 0.98 (0.90–1.06) | |||||||
| 5–6 h/day | 1.02 (0.94–1.11) | |||||||
| 7–8 h/day | 0.95 (0.86–1.06) | |||||||
| ≥9 h/day | 1.16 (1.02–1.30) | |||||||
| Television viewing | ||||||||
| Warren et al. 201045 |
7744 men, 47.1 years |
377 CV deaths |
History of MI, stroke, cancer |
21 | Q1 | 1.00 | Age, smoking, alcohol use, leisure-time physical activity, Physical Activity Readiness Questionnaire |
Leisure and work physical activity rated relative to others. Was dichotomized into physically active vs inactive |
| Q2 | 1.02 (0.74–1.42) | |||||||
| Q3 | 1.27 (0.90–1.78) | |||||||
| Q4 | 0.96 (0.68–1.36) | |||||||
| Dunstan et al. 201046 |
8800 men and women, ≥25 years |
87 CVD deaths |
History of CVD, pregnancy, fasted ≥9 h, over- or under- reported energy intake |
6.6 | <2 h/day | 1.00 | Age, gender, smoking status, education, energy intake, alcohol use, Diet Quality Index, waist circumference, hypertension, total cholesterol, high-density lipoprotein cholesterol, triglycerides, lipid-lowering medications, oral glucose tolerance test, leisure exercise time |
Active Australia questionnaire |
| 2-<4 h/day | 1.19 (0.72–1.99) | |||||||
| ≥4 h/day | 1.80 (1.00–3.25) | |||||||
| Wijndaele et al. 201116 |
13 197 men and women with mean 61.5 years |
373 CVD deaths |
History of MI, stroke, cancer |
9.5 | Per hour/day | 1.08 (1.01–1.16) | Age, gender, education, smok- ing status, alcohol use, medications for hypertension and dyslipidemia, history of diabetes, family history of CVD and cancer, physical activity |
EPAQ2 |
| Per hour/day | 1.07 (0.99–1.15) | Age, gender, education, smok- ing status, alcohol use, medications for hypertension and dyslipidemia, history of diabetes, family history of CVD and cancer, physical activity, waist circumference |
||||||
| Stamatakis et al. 201147 |
4512 men and women, ≥35 years |
215 CV events |
Previous hospital stays for CVD |
4.3 | <2 h/day | 1.00 | Age, gender, ethnicity, body mass index, smoking, social class, long-standing illness, marital status, diabetes, hypertension and physical activity |
Average daily time of non-occupational moder- ate-vigorous physical ac- tivity during past 4 weeks. Occupational physical ac- tivity in 3 categories |
| 2-<4 h/day | 2.23 (1.31–3.80) | |||||||
| ≥ 4 h/day | 2.25 (1.30–3.89) | |||||||
| Matthews et al. 201244 |
240 819 men and women, 50–71 years |
4684 CV deaths |
History of cancer, CVD, respiratory disease |
8.5 | < 1 h/day | 1.00 | Age, gender, race, education, smoking history, diet quality, moderate-vigorous physical activity |
Average time spent each week in activities of at least a moderate intensity in the past 10 years |
| 1–2 h/day | 1.00 (0.86–1.16) | |||||||
| 3–4 h/day | 1.15 (1.00–1.33) | |||||||
| 5–6 h/day | 1.36 (1.17–1.59) | |||||||
| ≥7 h/day | 1.85 (1.56–2.20) | |||||||
| Ford 201248 | 7350 men and women, ≥20 years |
190 circula- tory disease |
None stated | 5.8 | < 1 h/day | 1.00 | Age, gender, race or ethni- city, education, leisure-time physical activity, Healthy Eating Index score, alcohol consumption, health status and health insurance coverage |
Average weekly minutes of moderate and vigorous leisure-time physical ac- tivity during past 30 days |
| 1 h/day | 1.42 (0.64–3.17) | |||||||
| 2 h/day | 0.82 (0.42–1.59) | |||||||
| 3 h/day | 1.42 (0.61–3.30) | |||||||
| 4 h/day | 0.84 (0.38–1.83) | |||||||
| ≥5 h/day | 1.20 (0.58–2.49) | |||||||
| per 2 h/day | 1.02 (0.78–1.33) | |||||||
| Riding in a car | ||||||||
| Warren et al. 201045 |
7744 men, 47.1 years |
377 CV deaths |
History of MI, stroke, cancer |
21 | Q1 | 1.00 | Age, smoking, alcohol use, leisure-time physical activity, Physical Activity Readiness Questionnaire |
Leisure and work physical activity rated relative to others. Was dichotomized into physically active vs inactive |
| Q2 | 1.09 (0.78–1.52) | |||||||
| Q3 | 1.23 (0.89–1.70) | |||||||
| Q4 | 1.50 (1.08–2.09) | |||||||
CHD — coronary heart disease; CV — cardiovascular; CVD — cardiovascular disease; MI — myocardial infarction.
In the 1981 Canada Fitness Survey, 759 CVD deaths occurred among 17 013 men and women aged 18–90 years followed for an average of 12.0 years.42 Overall, CVD mortality increased progressively across five categories of time spent sitting, determined by questionnaire, with an aHR of 1.54 (95% CI: 1.09–2.17) for those reporting sitting almost all the time during most days of the week compared with sitting almost none of the time. The risk for CVD mortality in function of time spent sitting increased among both men and women, with an apparently stronger dose–response relationship among women.
In the Cancer Prevention Study II (CPS II)— Nutrition Cohort, 69 776 women and 53 440 men were followed for 14 years, and there were 2360 and 4009 deaths from CVD, respectively.43 Participants were asked, ‘During the past year, on an average day (not counting spending time at your job), how many hours per day did you spend sitting (watching television, reading, etc.)?’ Comparing those reporting daily sitting of ≥6 h vs 0–<3 h, increased mortality from CVD was reported among men (aHR: 1.18; 95% CI: 1.08–1.30) and women (aHR: 1.33; 95% CI: 1.17–1.52). Again, the dose–response appeared stronger in women than men.
In the NIH-AARP study, 240 819 US participants aged 50–71 years were followed for 8.5 years, and 4684 participants died of cardiovascular causes.44 Time spent sitting was assessed with the question, ‘During a typical 24-h period over the past 12 months, how much time did you spend sitting? (<3, 3–4, 5–6, 7–8 or 9+h/d)’. When compared with participants who reported sitting <3 h/day, the aHRs for participants sitting longer amounts of time, in h/day, were 0.98 (95% CI: 0.90–1.06) for 3–4, 1.02 (95% CI: 0.94–1.11) for 5–6, 0.95 (95% CI: 0.86–1.06) for 7–8 and 1.16 (95% CI: 1.02–1.30) for ≥9 (P for trend = 0.139).
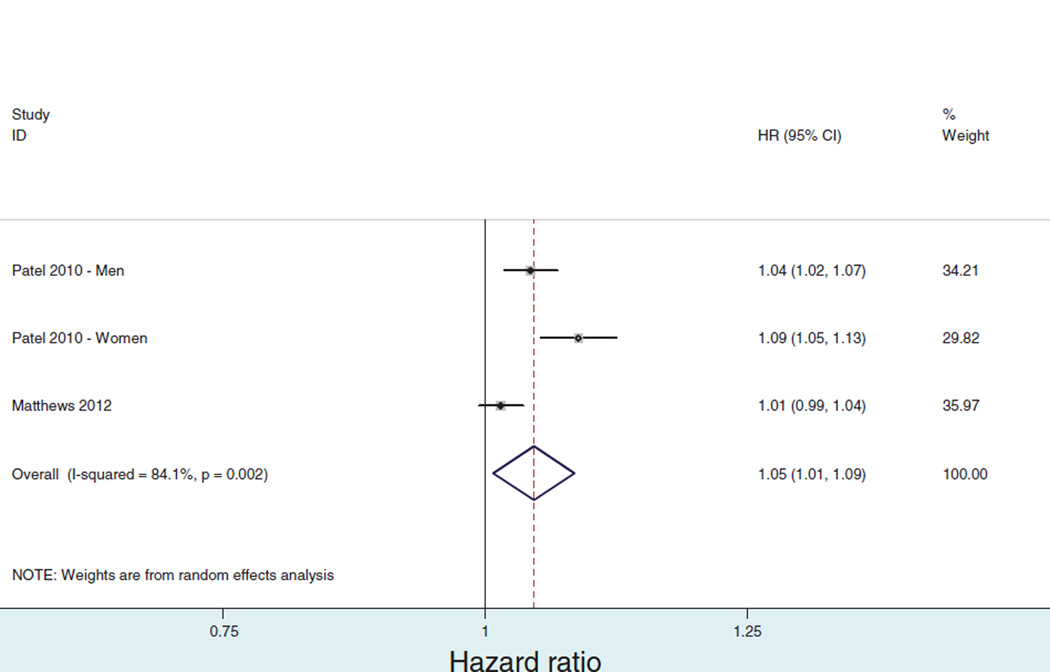
Each of these prospective studies reported an increased risk for developing or dying from CVD with risk estimates for the highest compared with lowest levels of sitting time ranging from 1.16 to 1.68. Three of the four studies were mortality studies. A couple of studies showed somewhat stronger measures of association among women than among men, but CIs for the estimates overlapped considerably. Although a gender bias may exist in the reporting of sedentary behaviours, it is unclear whether data exist to examine this bias. Given the enormous differences in the response options for the questions about time spent sitting, performing a meta-analysis incorporating all these studies proved unfeasible. Using the two studies that allowed an estimate of the relationship between 2-h/day sitting and mortality from CVD to be calculated,43,44 the random effects summary HR per 2 h/day of sitting is 1.05 (95% CI: 1.01–1.09; test for heterogeneity: Q = 12.56, P = 0.002; I2 = 84.1%) (Figure 3).
Figure 3.
Associations between time spent sitting (per 2 h/day) and cardiovascular events
Watching television
Six prospective studies specifically incorporated questions about the amount of time spent watching television. A 21-year follow-up of 7744 men in the Aerobics Center Longitudinal Study (ACLS) identified 377 CVD deaths.45 When comparing the top with lowest quartiles, the authors noted an aHR of 0.96 (95% CI: 0.68–1.36) for watching television and an aHR of 1.50 (95% CI: 1.08–2.09) for riding in a car.
In the Australian Diabetes, Obesity and Lifestyle Study, 8800 men and women aged 25 years or older had a median follow-up of 6.6 years during which 284 participants died (87 CVD deaths).46 Participants reported time spent watching television or videos during the previous 7 days excluding time spent in activities while the television was on. Although the reliability of reported screen time was good (ρ = 0.82), the criterion validity was poor (ρ = 0.3). Comparing those who reported watching television for ≥4 h/day vs <2 h/day, the aHR was 1.80 (95% CI: 1.00–3.25) for CVD mortality.
The European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk Study followed 13 197 men and women (mean age of 61.5 years) for a median of 9.5 years and recorded 373 CVD deaths.16 Participants were asked four questions about time spent watching television or videos during week- and weekend days. These questions had high reliability with acceptable validity. The aHR/h/day of television viewing was 1.07 (95% CI: 0.99–1.15) for CVD deaths.
In the Scottish Health Survey, 4512 adults aged 35 years or older were followed from 2003 to 2007, during which time 215 participants had an incident CVD event.47 Participants who reported a screen time of ≥4 h/day vs <2 h/day had an aHR of 2.25 (95% CI: 1.30–3.89) for diseases of the circulatory system.
An analysis of data from 240 819 US participants aged 50–71 years from the NIH-AARP study who were followed for 8.5 years (4684 cardiovascular deaths) showed that the aHRs rose progressively across quintiles of time spent watching television or videos.44 The amount of time that participants spent watching television or videos was assessed with the question, ‘During a typical 24-h period over the past 12 months, how much time did you spend watching television or videos? (None, 1–2, 3–4, 5–6, 7–8 or 9+ h/day)’. Compared with participants who watched <1 h of television or videos per day, those who watched television or videos for ≥7 h/day had almost double the risk of dying from CVD (aHR: 1.85, 95% CI: 1.56–2.20).
In a study of a national sample of US 7350 adults with a median follow-up of 5.8 years, 190 deaths from diseases of the circulatory system were recorded.48 The aHR for screen time (time spent watching television or videos or using a computer outside of work) of ≥5 h/day compared with <1 h/day was 1.20 (95% CI: 0.58–2.49). The aHR per 2-h/day of screen time was 1.02 (95% CI: 0.78–1.33).
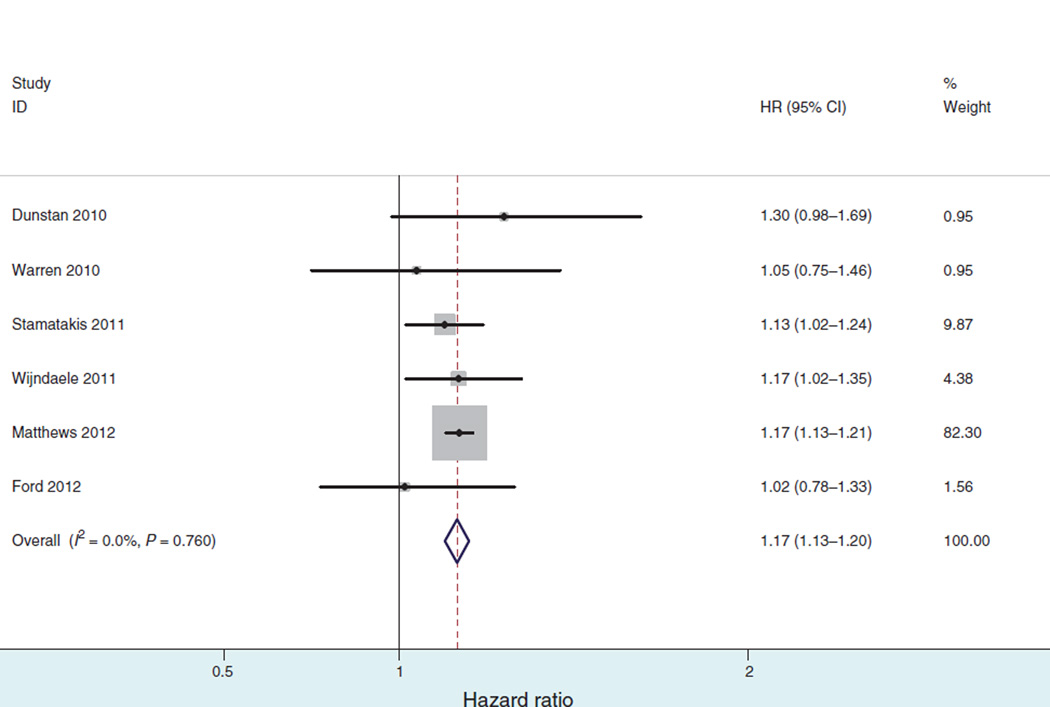
In three of these six prospective studies, the CIs for the hazard ratios excluded 1.0. All studies attempted to control for a series of confounders, but had only age, smoking status and, importantly, physical activity in common. Interestingly, the Australian study that adjusted for several cardiometabolic factors, which could be considered to be mediating variables, yielded the highest risk estimates. A very recent meta-analysis of the first four studies yielded a summary relative risk for fatal or non-fatal CVD of 1.15 (95% CI: 1.06–1.23) per 2 h/day prolonged television viewing.20 Updating the result from that analysis with results from the two most recent studies yields a fixed effects summary HR per 2 h/day of screen time of 1.17 (95% CI: 1.13–1.20; test for heterogeneity: Q = 2.61, P = 0.760; I2 = 0%) (Figure 4). Because of its large size, the NIH-AARP study dominates the analysis. Once excluded, the summary HR was 1.14 (95% CI: 1.05–1.22; test for heterogeneity: Q = 1.95, P = 0.745; I2 = 0%).
Figure 4.
Associations between screen time (per 2 h/day) and cardiovascular events
Does adequate physical activity mitigate the possible harmful effects of excessive sedentary behaviour?
Several prospective studies tried to address this issue by stratifying analyses by physical activity sta-tus.16,43,45 Researchers stratified participants of the CPS II into five physical activity levels (<24.5, 24.5–<31.5, 31.5–42.0, 42.0–<52.5 and ≥52.5 MET-h/week) and found positive gradients between sitting time and all-cause mortality for each level of physical activity, particularly among women and in the most sedentary group.43 In the ACLS cohort, increased time spent riding in a car did not predict CVD mortality for participants who were physically active but was strongly associated for participants who were physically inactive.45 Finally, the aHR for all-cause mortality did not differ statistically between participants with high and low physical activity in the EPIC Norfolk Study.16
These three prospective studies suggest that physical activity may not necessarily undo the possible harms from excessive sedentary behaviour. The results from the CPS II are of particular interest because, even at the highest levels of physical activity (~2 h of moderate activity per day), sedentary behaviour appeared to be related to all-cause mortality in a dose-response manner.
Do breaks in sedentary time potentially negate the harmful effects of sedentary behaviour?
Thus far, no prospective studies have examined whether breaks in sedentary time relate favourably to incident or fatal CVD. However, data from at least two cross-sectional studies have reported associations between the number of breaks and various cardiometabolic parameters after accounting for moderate to vigorous physical activity.49,50 Among 168 Australians aged 30–87 years, the number of breaks measured by accelerometers was inversely related to concentrations of triglycerides and less so to BMI, waist circumference, and 2-h plasma glucose.49 More recently, analyses of 4757 American adults aged 20 years or older revealed that the number of breaks in sedentary time measured by accelerometer was inversely proportional to the waist circumference and C-reactive protein levels.50
Mechanisms
Relatively little evidence identifying unique potential mechanisms for the effect of sedentary behaviour on cardiovascular outcomes exists, especially when high levels of physical activity also exist. In animal studies, the unloading of hindlimbs in rats produced reversible reductions of lipoprotein lipase (LPL) activity, which was confined to the affected limbs, and subsequent reductions in the local uptake of triglycerides and circulating concentrations of high-density lipoprotein cholesterol (HDLC).51
Evidence from related areas of investigation may shed light on the mechanisms that link excessive sedentary behaviour to CVD. Air travel is a mode of transport characterized by prolonged sitting, often in cramped spaces. When reports about deep vein thrombosis (DVT) in airline passengers emerged, immediate attention was drawn to the long periods during which passengers are required to sit. In a randomized trial, ~10% of passengers aged 50 years or older on long flights developed asymptomatic DVT.52 Besides prolonged sitting, host factors and airplane cabin environmental factors are thought to contribute to DVT on long flights.
Bed rest is a step down the MET scale from sitting, and the physiological changes effected by the former may have relevance to the latter. Prolonged bed rest produces adverse effects on numerous organ systems including the cardiovascular system involving negative repercussions on postural hypotension, cardiac function, cardiac filling, stroke volume, cardiac output, heart rate and thromboembolic events.53–59 These complications may be germane to the studies of excessive sitting or sedentary behaviour and CVD. Furthermore, bed rest may lead to glucose intolerance, an important CVD risk factor.55
Discussion
Since the 1950s, epidemiological studies have suggested that sedentary behaviour adversely affects health. The landmark systematic review of prospective studies by Powell et al. in 1987 conclusively linked physical activity to CHD.60 The review focused largely on quantifying the dose, intensity and type of physical activity needed to produce benefits. After many adjustments for possible confounding variables across studies, the highest levels of physical activity conferred an almost 50% reduction in risk for CVD. At that time, sedentary behaviour was considered to be at the lower end of a physical activity continuum, even though the amount of sedentary behaviour assigned to the least active category in studies was uncertain.
Largely in the past decade, interest has burgeoned in studying the possible health impact of sedentary behaviour apart from physical activity, perhaps in recognition of the growing amount of sedentary pursuits in modern society. This different conceptual approach seeks to address questions of whether sedentary behaviour affects health outcomes at each level of physical activity. Thus, the questions that were asked in the more recent studies differ from those considered previously.
The growing number of studies reporting positive associations between sedentary behaviour and CVD suggest that the results are unlikely to be spurious findings. Two alternative explanations are that either the findings are true or the findings reflect various types of bias. If true, it may be that sedentary behaviour displaces time spent in light physical activity, with time spent in sedentary behaviours being a lost opportunity to perform substantive amounts of physical activity.61 However, when several trials sought to reduce television viewing among children, they did not consistently improve measured physical activity levels.62–64 In fact, the links between watching television and poor dietary and snacking habits were more often repeatedly demonstrated.65 Thus, disentangling the possible effects of sedentary behaviour from those of unhealthy dietary and snacking behaviour remains a critical challenge before reaching firm conclusions or stipulating guidelines for costly interventions.
Limitations
Several limitations deserve consideration. Firstly, the validity and reliability of questions to assess sedentary behaviour are often unknown. A review of questions about television watching concluded that there was variable validity.66 Less is known about questions for assessing sitting particularly outside the workplace. A review of occupational physical activity assessments found sitting questions to be more reliably reported than other work activity questions.67 Some misclassification of exposure likely exists in many studies. The degree of misclassification is unlikely to be non-differential because respondents are more likely to systematically underreport their sedentary behaviour. In most studies, the reference group represents the least sedentary group. If that group becomes populated with participants who actually are more sedentary, the baseline risk of the reference group increases resulting in underestimating hazard ratios.
Secondly, different approaches in selecting reference and exposure categories in studies complicate comparisons of their results. For example, in studies of sitting, reference categories were either <3 or <4 h/ day and the top category ranged from ≥6 h/day to ≥ 16 h/day.
Thirdly, most of the reviewed prospective studies had mortality rather than incidence as their outcome.
Fourthly, because the magnitude of the hazard ratios is generally small, unmeasured or incorrectly specified confounders are of concern. Because sedentary behaviour is precisely that—a behaviour— there is a great susceptibility to this bias when physical activity and dietary behaviours are known to co-occur as part of broader behavioural pattern. Sedentary individuals and those who are not considered sedentary are likely to differ in a myriad of measurable and immeasurable ways. Physical activity and diet are notoriously difficult to measure accurately, adding to the difficulty of appropriately specifying models that might also include factors as mediating variables. Although several studies adjusted for total energy intake, only a limited number of studies adjusted for some kind of dietary pattern.44,46,48 The observational studies regarding the purported health benefits of some vitamins have taught the epidemiological community some painful lessons about extrapolating from observational studies and, thus, appropriate confirmatory studies are needed.
Fifthly, at the inception of prospective studies, participants who were in poor health may have been more sedentary than healthier participants. Attempting to rule out reverse causation, some studies excluded from analyses those participants who expired within the first few years of follow-up, often finding no change in results.16,47
Sixthly, the factors that govern sedentary status may also affect CVD risk. For example, a body of research has suggested that persons subject to the combination of low decision latitude to select their work circumstances and poor support are likely to occupy jobs characterized by high levels of stress and sedentariness and experience higher morbidity and mortality than those in opposing circumstances.68
Uniqueness
The question of whether sedentary behaviour is truly distinct from physical activity rather than simply representing one end of the physical activity spectrum3,5 can be examined from the following perspectives:
Energy expenditure: Sedentary behaviour occupies the lower end of an energy expenditure scale with a range of MET values for associated activities ranging from 1.0 to 1.5 or 2.0 METs. Changing posture from motionless sitting to motionless standing raises energy expenditure by ~9%.69
Physiology: A key study showed that local muscle concentrations of LPL of unloaded hind legs of rats decreased in function of unloaded time but increased again when rats were allowed to use their hind legs.51 Because LPL serves to regulate lipid concentrations and maintain cardiometabolic homeostasis, these findings provided a rationale for relating sedentary behaviour to cardiometabolic aberrations. Unfortunately, few other studies provide unique physiological mechanisms of sedentary behaviour, with none replicated in humans.
Epidemiology and statistics: Several studies have found that physical activity and sedentary behaviour are poorly associated having correlation coefficients ranging from −0.002 to −0.09.43,70,71 Moreover, risk estimates for sedentary behaviour and CVD events were often independent of physical activity.
Determinants research: It seems plausible that sedentary behaviour might arise from a unique set of motivational cues differing substantially or entirely from those that motivate someone to engage in physical activity. Research into the determinants of sedentary behaviour is still young. Intuitively, the seductive nature of technology and its spread, especially as part of entertainment, is likely a major contributor to sedentary behaviour. Extrapolating beyond available empirical evidence is problematical as illustrated by a study that showed that the degree of neighbourhood walkability correlated favorably with physical activity levels72 but not with sedentary behaviour.73 In another study, neighbourhood walkability was inversely associated with television viewing time in women but not in men.74 Hence, determinants of pursuing specific sedentary behaviours may be as unique as those governing why people choose to walk, play tennis, golf or engage in some other activity.5
Guideline development and risk communication: If sedentary behaviour negatively affects health and has a unique set of determinants, then separate recommendations to specifically limit sedentary behaviour will need to be developed that complement those that address physical activity. Currently, specific recommendations and risk communication strategies may be premature and await further evidence concerning the frequency, timing and duration of breaks necessary to combat the cardiovascular health consequences of excessive sedentary behaviour.
Public health interventions: Public health approaches to reduce sedentary behaviour and increase physical activity in populations are likely to differ substantially. For example, a great deal of research has linked attributes of the physical environment to physical activity levels.75 However, whether modifications to the environment that might encourage more physical activity would also serve to reduce sedentary behaviour is not guaranteed, as some research intimates.
Clinical practice: Because clinical advice to patients to raise their levels of physical activity may not reduce their sedentary behaviour, clinicians may need to assess for, and counsel in response to, the amounts of both physical activity and sedentary behaviour of their patients.
Public health interventions
Many employed people engage largely in desk work. One option is to find ways to reduce the job-related sitting time or find ways to introduce a sufficient number of breaks during the day to mitigate excessive risks from sitting. A recent review offered several options for modifying the work space including providing employees with standing desks, a therapy ball to sit on, stepping devices and walking work stations.76 In addition, the authors proposed adding breaks. However, the frequency and duration of breaks needed to offset any risk of excessive sitting remains unknown and requires investigation. Widespread adoption of measures to break up periods of prolonged sedentary behaviour at work awaits rigorous studies concerning the cost-effectiveness of potential interventions.
Because a sizeable portion of waking hours is spent being sedentary in one’s home, targeting the domestic environment is an obvious strategy given that much of the population may not recognize the possible adverse impact of that excessive sedentary behaviour on health. Also, as the evidence base concerning how to specifically reduce the domestic sedentary behaviour is scant, some form of education may be necessary even though education alone cannot guarantee behavioural change. With high and increasing levels of watching television or using computers or other forms of screen time in contemporary societies,77 efforts aimed at decreasing time performing these activities in a position other than sitting hold considerable appeal. Although studies have successfully reduced television viewing time by children and adolescents,62,64 relatively little research has included adults. Consequently, there is a dearth of evidence-based interventions to guide domestic interventions among adults. The introduction of labour-saving devices in the home was meant, in part, to free up people’s time to engage in more desirable leisure-time pursuits. If the unintended effect of these devices was to promote sedentary behaviours, perhaps a return to more traditional ways of performing household chores might prove beneficial to one’s health (but perhaps not to one’s psyche). Shifting people from one sedentary behaviour such as using a computer to another one such as reading a book is unlikely to improve health.
Much of the current energy directed towards public health interventions at the community level revolves around changing policies, systems and environments. The models that are being developed and tested specifically seek to raise physical activity levels in the US population rather than reduce sedentary behaviour and sitting, per se. Therefore, some recalibration of these approaches may be required to produce decreases in sedentary behaviour for Americans.
Because so many people spend so much time commuting in a car to work as well as using a car for other activities, efforts to promote public transportation and get people to perform errands on foot or by bicycle could reduce the time that people sit motionlessly. However, the MET level of sitting in a bus or train vs that of sitting in a car is very similar, so shifting people from transportation by car to that of mass transit would not necessarily reduce sedentary behaviour. Because of limited seating, many people have little choice but to stand in public transport systems, which in itself would reduce sedentary behaviour. In addition, some additional energy expenditure may derive from walking or bicycling to and from public transportation stops.
Clinical interventions
Most American adults have an encounter with the medical system each year with 70% of respondents of the 2009 Behavioral Risk Factor Surveillance System reporting a routine check-up in the previous year (Ford E, personal observation). These encounters present precious opportunities for clinicians to counsel their patients about the possible benefits of reducing sedentary behaviour and sitting. Participants in a clinical trial who received individual counselling and physical activity prescriptions reduced their sitting time an average of 2 h/day, whereas participants who received usual care reduced sitting time 1 h/day.78 It is yet unclear how well-informed physicians are about the emerging evidence of the possible harmful effects of sedentary behaviour. Once the relationship between sedentary behaviour and CVD is better understood and evidence-based clinical approaches emerge to mitigate risk, clinicians may benefit from professional education about routinely enquiring about their patients’ sedentary habits and physical activity levels and providing appropriate counselling.
Future directions
Prospective observational studies are generally accorded a high level of confidence in epidemiology. However, fewer than a dozen prospective studies have examined the links between various forms of sedentary behaviour (television watching, riding in a car, sitting, etc.) and risks of fatal or non-fatal CVD. Because the outcome of interest has been almost entirely limited to mortality, additional studies of incident CVD are desirable. Also, self-reported questions were used to assess exposure time. Consequently, additional prospective studies are needed, especially ones using a consistent way to measure sedentary behaviour while using less heterogeneous ways of analysing data. Some degree of standardization, for example of the reference category, would aid in the interpretation of future data and would help to establish the magnitude of the risk reduction and dose–response relationships. Prospective studies that use accelerometers or other objective methods to measure amounts of sedentary behaviour may prove valuable in confirming findings from the existing prospective studies. Ideally, studies that include more than one assessment of sedentary behaviour over time would permit an understanding of increasing, decreasing and stationary levels of sedentary behaviour on health outcomes.
Our understanding of ways to break up sedentary time is in its infancy. To guide the development of rational public health and clinical interventions, the frequency and duration of such breaks needed to mitigate the harms from excessive sedentary behaviour must be thoroughly understood. More cross-sectional studies can help guide the design of randomized controlled trials that seek to examine the frequency and duration of breaks needed to reduce cardiovascular risk. In the occupational setting, workers could be randomized to intervention groups in which workstations are modified or to a control group in which the work setting remains unchanged. Thereafter, group changes in CVD risk factors, illness, medical costs, work absence and productivity could be compared.
The estimated cost of physical inactivity is high—~$251 billion in 2003 dollars in USA.79 Consequently, reducing sedentary behaviour might produce substantial reductions in costs, but this supposition remains to be established empirically. Given the increasingly precarious financial plight of federal and state governments, a key consideration in implementing future interventions will be their cost-effectiveness. Such research tailored to the USA is urgently needed.
Current physical activity guidelines generally focus on raising the level of physical activity in the population and do not specifically define precise reductions of sedentary behaviour. Evidence-based revisions or updates of future guidelines will allow rational and cost-effective recommendations specific to reducing sedentary behaviour.
Conclusions
Conventional wisdom dictates that people have grown more sedentary during the twentieth and twenty-first centuries, but few objective data exist to characterize the magnitude of the change. Regardless of this past uncertainty, recent data clearly indicate that the level of sedentary behaviour in the US population and in other nations with developed economies is quite substantial. Although studies during the 1950s first identified an increase in CVD risk experienced by people in highly sedentary jobs, only in recent years have the potential CVD risks from sedentary behaviour, as distinct from physical activity, come to be appreciated. Our review of prospective studies found a significant association between screen time and cardiovascular mortality independent of levels of physical activity. Furthermore, two large cohort studies that lent themselves to a meta-analytic summary also suggested a significant increased risk between the time spent sitting and cardiovascular mortality, also independent of physical activity. Despite the need to solidify the evidence base concerning the health risks caused by excessive sedentary behaviour, available data are clear that being in the least active group is not desirable, especially when excessive sedentary behaviour is likely to comprise membership in that group.
Supplementary Material
KEY MESSAGES.
On average, adults in many societies spend a large portion of their day being sedentary.
A limited number of prospective studies have found that the amount of time being sedentary—for example time spent sitting or watching television—is associated with increased risk for fatal and non-fatal CVD.
Cross-sectional studies showing that the number of breaks in sedentary time is favourably associated with cardiometabolic factors require additional replication and confirmation in experimental studies.
Additional research is needed to clarify the relationships between the amount of time that adults are sedentary and fatal and non-fatal outcomes such as CVD and to develop strategies to mitigate any such increased risk.
Footnotes
Supplementary Data are available at IJE online.
Conflict of interest: None declared.
References
- 1.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 2.Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6:e19657. doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietz WH. The role of lifestyle in health: the epidemiology and consequences of inactivity. Proc Nutr Soc. 1996;55:829–840. doi: 10.1079/pns19960082. [DOI] [PubMed] [Google Scholar]
- 4.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev. 2000;28:153–158. [PubMed] [Google Scholar]
- 6.Salmon J, Owen N, Crawford D, Bauman A, Sallis JF. Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol. 2003;22:178–188. doi: 10.1037//0278-6133.22.2.178. [DOI] [PubMed] [Google Scholar]
- 7.Chastin SF, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture. 2010;31:82–86. doi: 10.1016/j.gaitpost.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wareham NJ, Jakes RW, Rennie KL, et al. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2003;6:407–413. doi: 10.1079/PHN2002439. [DOI] [PubMed] [Google Scholar]
- 10.Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88:612–617. doi: 10.1093/ajcn/88.3.612. [DOI] [PubMed] [Google Scholar]
- 11.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 12.Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM. Patterns of objectively measured physical activity in the United States. Med Sci Sports Exerc. 2008;40:630–638. doi: 10.1249/MSS.0b013e3181620ebc. [DOI] [PubMed] [Google Scholar]
- 13.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Uffelen JG, Wong J, Chau JY, et al. Occupational sitting and health risks: a systematic review. Am J Prev Med. 2010;39:379–388. doi: 10.1016/j.amepre.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 15.The Nielsen Company. [23 June 2011, date last accessed];Three Screen Report. http://blog.nielsen.com/nielsenwire/online_mobile/what-consumers-watch-nielsens-q1-2010-three-screen-report/
- 16.Wijndaele K, Brage S, Besson H, et al. Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk Study. Int J Epidemiol. 2011;40:150–159. doi: 10.1093/ije/dyq105. [DOI] [PubMed] [Google Scholar]
- 17.Dong L, Block G, Mandel S. Activities contributing to total energy expenditure in the United States: results from the NHAPS Study. Int J Behav Nutr Phys Act. 2004;1:4. doi: 10.1186/1479-5868-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30:1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 19.McKenzie B, Rapino M. American Community Survey Reports No. ACS-15. Washington, DC: U.S. Census Bureau; 2011. Commuting in the United States: 2009. [Google Scholar]
- 20.Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose- response data. Stata J. 2006;6:40–57. [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris JN, Heady JA, Raffle PA, Roberts CG, Parks JW. Coronary heart-disease and physical activity of work. Lancet. 1953;265:1111–1120. doi: 10.1016/s0140-6736(53)91495-0. [DOI] [PubMed] [Google Scholar]
- 25.Taylor HL, Klepetar E, Keys A, Parlin W, Blackburn H, Puchner T. Death rates among physically active and sedentary employees of the railroad industry. Am J Public Health Nations Health. 1962;52:1697–1707. doi: 10.2105/ajph.52.10.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Netterstrom B, Laursen P. Incidence and prevalence of ischaemic heart disease among urban bus drivers in Copenhagen. Scand J Soc Med. 1981;9:75–79. doi: 10.1177/140349488100900205. [DOI] [PubMed] [Google Scholar]
- 27.Balarajan R, McDowall ME. Professional drivers in London: a mortality study. Br J Ind Med. 1988;45:483–486. doi: 10.1136/oem.45.7.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paradis G, Theriault G, Tremblay C. Mortality in a historical cohort of bus drivers. Int J Epidemiol. 1989;18:397–402. doi: 10.1093/ije/18.2.397. [DOI] [PubMed] [Google Scholar]
- 29.Michaels D, Zoloth SR. Mortality among urban bus drivers. Int J Epidemiol. 1991;20:399–404. doi: 10.1093/ije/20.2.399. [DOI] [PubMed] [Google Scholar]
- 30.Alfredsson L, Hammar N, Hogstedt C. Incidence of myocardial infarction and mortality from specific causes among bus drivers in Sweden. Int J Epidemiol. 1993;22:57–61. doi: 10.1093/ije/22.1.57. [DOI] [PubMed] [Google Scholar]
- 31.Merlo DF, Stagi E, Fontana V, et al. A historical mortality study among bus drivers and bus maintenance workers exposed to urban air pollutants in the city of Genoa, Italy. Occup Environ Med. 2010;67:611–619. doi: 10.1136/oem.2009.050377. [DOI] [PubMed] [Google Scholar]
- 32.Holme I, Helgeland A, Hjermann I, Leren P, Lund-Larsen PG. The Oslo study: 4-year mortality, coronary risk factors and socioeconomic indicators. Tidsskr Nor Laegeforen. 1980;100:1262–1266. [PubMed] [Google Scholar]
- 33.Rosengren A, Anderson K, Wilhelmsen L. Risk of coronary heart disease in middle-aged male bus and tram drivers compared to men in other occupations: a prospective study. Int J Epidemiol. 1991;20:82–87. doi: 10.1093/ije/20.1.82. [DOI] [PubMed] [Google Scholar]
- 34.Sjol A, Thomsen KK, Schroll M, Andersen LB. Secular trends in acute myocardial infarction in relation to physical activity in the general Danish population. Scand J Med Sci Sports. 2003;13:224–230. doi: 10.1034/j.1600-0838.2003.00310.x. [DOI] [PubMed] [Google Scholar]
- 35.Hu G, Sarti C, Jousilahti P, Silventoinen K, Barengo NC, Tuomilehto J. Leisure time, occupational, and commuting physical activity and the risk of stroke. Stroke. 2005;36:1994–1999. doi: 10.1161/01.STR.0000177868.89946.0c. [DOI] [PubMed] [Google Scholar]
- 36.Hu G, Jousilahti P, Borodulin K, et al. Occupational, commuting and leisure-time physical activity in relation to coronary heart disease among middle-aged Finnish men and women. Atherosclerosis. 2007;194:490–497. doi: 10.1016/j.atherosclerosis.2006.08.051. [DOI] [PubMed] [Google Scholar]
- 37.Hu G, Tuomilehto J, Borodulin K, Jousilahti P. The joint associations of occupational, commuting, and leisure-time physical activity, and the Framingham risk score on the 10-year risk of coronary heart disease. Eur Heart J. 2007;28:492–498. doi: 10.1093/eurheartj/ehl475. [DOI] [PubMed] [Google Scholar]
- 38.Rosenman RH, Bawol RD, Oscherwitz M. A 4-year prospective study of the relationship of different habitual vocational physical activity to risk and incidence of ische-mic heart disease in volunteer male federal employees. Ann N Y Acad Sci. 1977;301:627–641. doi: 10.1111/j.1749-6632.1977.tb38234.x. [DOI] [PubMed] [Google Scholar]
- 39.Johansson S, Rosengren A, Tsipogianni A, Ulvenstam G, Wiklund I, Wilhelmsen L. Physical inactivity as a risk factor for primary and secondary coronary events in Göteborg, Sweden. Eur Heart J. 1988;9:8–19. doi: 10.1093/eurheartj/9.suppl_l.8. [DOI] [PubMed] [Google Scholar]
- 40.Li CY, Sung FC. A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 1999;49:225–229. doi: 10.1093/occmed/49.4.225. [DOI] [PubMed] [Google Scholar]
- 41.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 42.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 43.Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–445. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blair SN. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121:384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 47.Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. J Am Coll Cardiol. 2011;57:292–299. doi: 10.1016/j.jacc.2010.05.065. [DOI] [PubMed] [Google Scholar]
- 48.Ford ES. Combined television viewing and computer use and mortality from all-causes and diseases of the circulatory system among adults in the United States. BMC Public Health. 2012;12:70. doi: 10.1186/1471-2458-12-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 50.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic bio-markers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551:673–682. doi: 10.1113/jphysiol.2003.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scurr JH, Machin SJ, Bailey-King S, Mackie IJ, McDonald S, Smith PD. Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights: a randomised trial. Lancet. 2001;357:1485–1489. doi: 10.1016/S0140-6736(00)04645-6. [DOI] [PubMed] [Google Scholar]
- 53.Persson AV, Davis RJ, Villavicencio JL. Deep venous thrombosis and pulmonary embolism. Surg Clin North Am. 1991;71:1195–1209. doi: 10.1016/s0039-6109(16)45585-4. [DOI] [PubMed] [Google Scholar]
- 54.Dittmer DK, Teasell R. Complications of immobilization and bed rest. Part 1: musculoskeletal and cardiovascular complications. Can Fam Physician. 1993;39:1428–1437. [PMC free article] [PubMed] [Google Scholar]
- 55.Teasell R, Dittmer DK. Complications of immobilization and bed rest. Part 2: other complications. Can Fam Physician. 1993;39:1440–1446. [PMC free article] [PubMed] [Google Scholar]
- 56.Rousseau P. Immobility in the aged. Arch Fam Med. 1993;2:169–177. doi: 10.1001/archfami.2.2.169. [DOI] [PubMed] [Google Scholar]
- 57.Krasnoff J, Painter P. The physiological consequences of bed rest and inactivity. Adv Ren Replace Ther. 1999;6:124–132. doi: 10.1016/s1073-4449(99)70030-0. [DOI] [PubMed] [Google Scholar]
- 58.Kyrle PA, Eichinger S. Deep vein thrombosis. Lancet. 2005;365:1163–1174. doi: 10.1016/S0140-6736(05)71880-8. [DOI] [PubMed] [Google Scholar]
- 59.English KL, Paddon-Jones D. Protecting muscle mass and function in older adults during bed rest. Curr Opin Clin Nutr Metab Care. 2010;13:34–39. doi: 10.1097/MCO.0b013e328333aa66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Powell KE, Thompson PD, Caspersen CJ, Kendrick JS. Physical activity and the incidence of coronary heart disease. Annu Rev Public Health. 1987;8:253–287. doi: 10.1146/annurev.pu.08.050187.001345. [DOI] [PubMed] [Google Scholar]
- 61.Williams DM, Raynor HA, Ciccolo CT. A review of TV viewing and its association with health outcomes in adults. Am J Lifestyle Med. 2008;2:250–259. [Google Scholar]
- 62.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 63.Ford BS, McDonald TE, Owens AS, Robinson TN. Primary care interventions to reduce television viewing in African-American children. Am J Prev Med. 2002;22:106–109. doi: 10.1016/s0749-3797(01)00410-x. [DOI] [PubMed] [Google Scholar]
- 64.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Simoes EJ, Byers T, Coates RJ, Serdula MK, Mokdad AH, Heath GW. The association between leisure-time physical activity and dietary fat in American adults. Am J Public Health. 1995;85:240–244. doi: 10.2105/ajph.85.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Clark BK, Sugiyama T, Healy GN, Salmon J, Dunstan DW, Owen N. Validity and reliability of measures of television viewing time and other non-occupational sedentary behaviour of adults: a review. Obes Rev. 2009;10:7–16. doi: 10.1111/j.1467-789X.2008.00508.x. [DOI] [PubMed] [Google Scholar]
- 67.Ainsworth BE, Jacobs DR, Jr, Leon AS, Richardson MT, Montoye HJ. Assessment of the accuracy of physical activity questionnaire occupational data. J Occup Med. 1993;35:1017–1027. [PubMed] [Google Scholar]
- 68.Karasek R, Baker D, Marxer F, Ahlbom A, Theorell T. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health. 1981;71:694–705. doi: 10.2105/ajph.71.7.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Levine JA, Schleusner SJ, Jensen MD. Energy expenditure of nonexercise activity. Am J Clin Nutr. 2000;72:1451–1454. doi: 10.1093/ajcn/72.6.1451. [DOI] [PubMed] [Google Scholar]
- 70.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289:1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 71.Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40:639–645. doi: 10.1249/MSS.0b013e3181607421. [DOI] [PubMed] [Google Scholar]
- 72.Van Dyck D, Cardon G, Deforche B, Sallis JF, Owen N, De Bourdeaudhuij I. Neighborhood SES and walkability are related to physical activity behavior in Belgian adults. Prev Med. 2010;50:S74–S79. doi: 10.1016/j.ypmed.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 73.Van Dyck D, Cardon G, Deforche B, Owen N, Sallis JF, De Bourdeaudhuij I. Neighborhood walkability and sedentary time in Belgian adults. Am J Prev Med. 2010;39:25–32. doi: 10.1016/j.amepre.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 74.Sugiyama T, Salmon J, Dunstan DW, Bauman AE, Owen N. Neighborhood walkability and TV viewing time among Australian adults. Am J Prev Med. 2007;33:444–449. doi: 10.1016/j.amepre.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 75.Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 76.Chau JY, van der Ploeg HP, van Uffelen JG, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med. 2010;51:352–356. doi: 10.1016/j.ypmed.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 77.Braun J. [1 March 2012, date last accessed];One Television Year in the World. http://www.international-television.org/tv_market_data/world-tv-programme-viewing-trends-2009 html.
- 78.Kallings LV, Sierra Johnson J, Fisher RM, et al. Beneficial effects of individualized physical activity on prescription on body composition and cardiometabolic risk factors: results from a randomized controlled trial. Eur J Cardiovasc Prev Rehabil. 2009;16:80–84. doi: 10.1097/HJR.0b013e32831e953a. [DOI] [PubMed] [Google Scholar]
- 79.Chenoweth D, Leutzinger J. The economic cost of physical inactivity and excess weight in American adults. J Phys Act Health. 2006;3:148–163. doi: 10.1123/jpah.3.2.148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.