Abstract
Older adults are more likely to have chronic wounds than younger people, and the effect of chronic wounds on quality of life is particularly profound in this population. Wound healing slows with age, but the basic biology underlying chronic wounds and the influence of age-associated changes on wound healing are poorly understood. Most studies have used in vitro approaches and various animal models, but observed changes translate poorly to human healing conditions. The effect of age and accompanying multimorbidity on the effectiveness of existing and emerging treatment approaches for chronic wounds is also unknown, and older adults tend to be excluded from randomized clinical trials. Poorly defined outcomes and variables; lack of standardization in data collection; and variations in the definition, measurement, and treatment of wounds also hamper clinical studies. The Association of Specialty Professors, in conjunction with the National Institute on Aging and the Wound Healing Society, held a workshop, summarized in this article, to explore the current state of knowledge and research challenges, engage investigators across disciplines, and identify research questions to guide future study of age-associated changes in chronic wound healing.
Keywords: chronic wound, pressure ulcer, diabetic foot ulcer, venous leg ulcer, wound repair, wound healing
Chronic wounds, which include venous leg ulcers (VLUs), diabetic foot ulcers (DFUs), arterial insufficiency, and pressure ulcers (PUs), disproportionately affect older adults and impose substantial morbidity and mortality on millions of older Americans. The great majority of chronic wounds are associated with conditions more common in older than younger individuals, including vascular disease, venous insufficiency, unrelieved pressure, and diabetes mellitus. In addition, an increasing number of older adults are undergoing surgery and are at risk of wound complications. Fundamental questions remain about the effect of aging on wound healing and the mechanisms of wound repair and tissue regeneration in older adults. Furthermore, few well-designed clinical trials have explored the treatment of wounds in older adults, leaving clinicians with scant evidence to guide optimal wound management, but with better scientific and clinical tools, along with an increasing number of highly motivated and talented investigators, a critical juncture to address these issues is being reached.
This workshop convened a transdisciplinary group of experts in the fields of wound repair and regeneration, skin aging, geriatric conditions, and gerontology from across the United States and Canada and program staff and scientists from the National Institute on Aging; the National Institute of Diabetes and Digestive and Kidney Diseases; the National Heart, Lung, and Blood Institute; and the National Institute of Nursing Research. The workshop aimed primarily to review current knowledge in epidemiological, basic science, and clinical topics; identify gaps in that knowledge; and develop a research agenda. Participants summarized research priorities and generated questions for future research (Table 1).
Table 1.
Research Questions for Wound Healing in Older Adults
| Category | Research Questions |
|---|---|
| Epidemiology and quality of life | What is the burden of illness due to chronic wounds in populations of older adults? |
| What is the frequency of multiple wounds and recurrent wounds in older adults? | |
| What is the reason for racial and ethnic disparities in prevention and management of chronic wounds in older adults? | |
| What is the effect of wound-associated pain on quality of life and function? | |
| What are the effects of other comorbidities in conjunction with chronic wounds, with respect to quality of life? | |
| What are the effects of socioeconomic status, living status, and other social factors on chronic wounds and quality of life? | |
| How does adhering to evidence-based clinical guidelines affect complications and quality of life? | |
| Does healing a chronic wound necessarily improve quality of health? | |
| What is the effect of treatment regimens or evidence-based guidelines for chronic wounds on quality of life? | |
| Basic biology of wound healing, chronic wounds, and aging | What causes acute injuries to become chronic wounds? |
| How can immune cells in the wound environment, or recruitment of immune cells to the wound, be modulated to harness benefit? | |
| What strategies can be used to reverse macrophage impairment? | |
| What factors regulate or activate macrophage phenotypes in wound repair? | |
| What are the mechanisms underlying endothelial and epidermal stem cell activation and homing to the wound site? | |
| What are the roles of proliferation and apoptosis in acute versus chronic wounds? | |
| What are reasons for delayed chemotaxis and lack of neutrophil function in chronic wounds? | |
| How does neutrophil depletion delay wound closure with advanced age? | |
| What are the mechanisms for matrix metalloproteinase overproduction with aging in chronic wounds? | |
| What drives the changing composition and properties of extracellular matrix during development and aging? | |
| What are the contributions of aging and comorbidities to the development of chronic wounds? | |
| Molecular and cellular processes | |
| Inflammation | What mechanisms contribute to low human inducibility factor 1a expression? |
| Does aging alter transforming growth factor beta signaling in chronic wounds? | |
| How important are changes in inflammatory responses to age-related changes in wound healing? | |
| How does inflammation affect the wound healing process in older adults? | |
| What is the optimal inflammatory response that will support rapid repair yet effectively reduce infection? | |
| Can manipulating inflammation alone force chronic wounds to heal? | |
| Oxidative stress | What is the role of specific mitochondrial deoxyribonucleic acid damage in impaired skin healing? |
| Microbial burden | Which microbiota are beneficial, and which are problematic for wound healing? |
| How does microbial bioburden in the wound influence systemic and local immune responses? | |
| How does age influence microbial burden in wounds and subsequent wound healing? | |
| Clinical care | |
| General | What is the clinical significance of delayed wound healing in older adults? |
| What is the significance of delayed wound healing from the individual’s point of view? | |
| Should wound care guidelines differ for older adults, accounting for heterogeneity and quality of life? | |
| Novel therapeutic approaches | What interventions effectively improve microcirculation and wound healing with aging? |
| What is the effect of wound therapies on universal outcomes, such as functional status, pain, physical impairment, mobility, and cognitive impairment, as opposed to wound-specific outcomes? | |
| What is the effect of multicomponent interventions on individual- and wound-specific outcomes? | |
| Are there special considerations related to older adults with chronic wounds and dementia? | |
| During surgery, what steps can anesthesiologists take to mitigate risk for chronic or nonhealing wounds? | |
| How do various wound treatments affect microbial burden? | |
| What new therapeutics can be developed based on the microbiome? | |
| How should cellular therapy be positioned in wound care? | |
| What potency assays are available to regulate cellular therapies? | |
| What is the effectiveness of physical modalities such as electrical stimulation and ultrasound in older adults? | |
| What is the effect of exercise on wound healing? | |
| What interventions effectively prevent chronic wounds in older adults? | |
| Nutrition | Can individuals be better categorized on the spectrum from cachexia to starvation, and can this categorization aid in determining the most-effective nutritional treatment strategies? |
| What is the optimal protein and energy intake for older adults with chronic wounds, especially at weight extremes? | |
| Is there a role for complete and various modular nutritional supplements, vitamin and mineral supplementation above the U.S. recommended daily intake, or appetite stimulants and anabolic steroids in the care of individuals with chronic wounds? | |
| Are complete or modular commercial nutritional supplements better than regular foods? |
EPIDEMIOLOGY OF CHRONIC WOUNDS IN OLDER ADULTS
The burden, particularly prevalence and incidence, of chronic wounds is unclear because of underreporting, poor definition of “chronic wound,” and inaccurate diagnostic coding for wound care. Many epidemiological studies do not distinguish between prevalence and incidence, and they often focus on endpoints, such as lower-extremity amputations (LEAs), which are easier to define and measure. Thus, estimates of prevalence and incidence vary between studies. Despite these limitations, studies indicate that the incidence of chronic wounds increases with age even into late life.1,2 Studies using the General Practice Research Database in the United Kingdom have found that VLU incidence is three to four times as high and PU incidence five to seven times as high in persons aged 80 and older than in those aged 65 to 70.1,2 Care for chronic wounds costs approximately $10 billion annually in the United States,3 and it is likely that wound care in adults aged 65 and older accounts for the majority of these costs.
Chronic wounds have a profound effect on quality of life (QOL), as assessed using generic and wound-specific instruments or according to health utility.4–6 The effect is similar to that of kidney or heart failure, and QOL decline is particularly precipitous in older adults, although overall QOL in older populations with chronic wounds is poorly understood. Existing measures do not differentiate age-related differences in the effect of chronic wounds between community-dwelling older adults and those in long-term care. Data from the U.S. Wound Registry indicate that individuals in outpatient wound centers have an average of eight comorbid conditions,7 but there is no clear distinction between the effect on QOL of chronic wounds and that of comorbidities.8,9 Furthermore, QOL as a function of wound severity, etiology, and complications is poorly understood.
Although people of all races and ethnicities experience chronic wounds, there are racial and ethnic disparities in wound severity at presentation and in subsequent treatment of wounds, although these disparities are more likely to reflect socioeconomic differences and clinician bias than true differences in the wounds based on race or ethnicity. PU incidence in African-American nursing home residents is more than 1.5 times that of white residents.10–13 It is likely that that disparity arises from differences in diagnosis and care; PU incidence is greater in white residents who live in nursing homes where the majority of residents are African American than in those who live in nursing homes where the majority of residents are white.10–13 LEA risk is also higher in African Americans and Native Americans, than in non-Hispanic whites, and it varies according to culture in Hispanic individuals,14–16 although the incidence of diabetes mellitus is also higher in non-white individuals, and race and ethnicity is less of a predictor of LEA than other factors, such as differences in rates of peripheral vascular disease and smoking. Time to amputation is shorter for African Americans than for whites, but this disparity also might arise from differences in prevention and care; African Americans tend to receive less preventive care, and whites are more likely to receive revascularizations.17–19
BASIC SCIENCE OF WOUND REPAIR AND HEALING
Biology of Wound Healing, Chronic Wounds, and Aging
The complex process of wound healing occurs in overlapping phases: inflammation, proliferation, angiogenesis, epidermal restoration, and wound contraction and remodeling.20 Important cell types in this process are platelets, which recruit inflammatory cells and form a provisional matrix, and macrophages, which include several phenotypes and regulate the cytokine environment in the wound, which influences proliferative responses and wound closure.21 Matrix metalloproteinases (MMPs) are active throughout wound healing, aiding in phagocytosis, angiogenesis, cell migration during epidermal restoration, and tissue remodeling.
In chronic wounds, resident cells proliferate less and have a morphology similar to that seen in senescent cells. Fibroblasts from chronic VLUs, particularly ulcers of long duration, have poorer responses to platelet-derived growth factor (PDGF),22 alterations in transforming growth factor beta (TFG-β) and TGF-β type II receptor expression,23 and abnormal phosphorylation of critical signal transduction proteins.24 The low receptor expression in cells in these wounds is similar to that in cells exposed to low oxygen tension, suggesting that chronic wounds are hypoxic.24
Aging also is associated with alterations in wound healing. In a diabetic mouse model, the healing of burns is delayed in older mice as a result of diminished hypoxia-inducible factor 1 expression, fewer bone marrow–derived angiogenic cells (BMDACs), and dampened response and homing in BMDACs that are present (Figure 1).25,26 Aging also is associated with delays in macrophage and T-cell infiltration, angiogenesis, and epithelialization.
Figure 1.
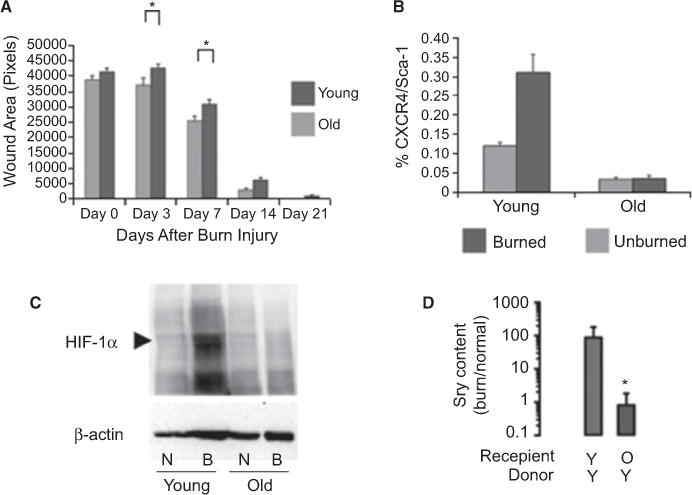
Burn wound repair is delayed in aged mice. (A) Wound area was evaluated 0, 3, 7, 14, and 21 days after burn injury in 2-month-old (young) versus 2-year-old C57BL/6J mice. *P < .05 versus young mice. (B) Bone marrow–derived angiogenic cells were identified using fluorescence-activated cell sorting as CXCR4+/Sca-1+. (C) Human inducibility factor (HIF)-1a concentrations in response to burn injury are lower in aged than younger mice. (D) Bone marrow–derived angiogenic cells from young male mice (Y) administered through tail vein injection to recipient female mice with burn wounds were less able to home in older recipients (O) than in younger ones (Y). Donor cells were identified using the Sry gene as a marker. *P < .01 versus young recipients. N = normal; B = burned. Adapted from Zhang X et al.25
The properties of the extracellular matrix (ECM) and its contribution to wound-healing changes throughout the life span (Table 2).27 Whereas younger skin can mount a robust response by producing ECM that can adapt to the mechanical demands of an injury, older skin has atrophied and has a prolonged, blunted healing response28 with inflammation and differences in signal transduction that result in inferior in ECM production. Healing in older animals also involves a protective and noninflammatory response characterized by lack of matrix molecule production and less scarring. Work in an in vitro model of aged rat skin suggests that age-associated disadvantages in healing may arise from overexpression of MMPs, particularly MMP2,29 consistent with findings that protease expression and activity are greater in older humans.30 Age-related changes in hormonal status affect repair. MMPs, particularly MMP2, are high principally in older postmenopausal women, and estrogen replacement therapy can stimulate the migration and proliferation of keratinocytes and elaboration of matrix.30
Table 2.
Properties in Cutaneous Extracellular Matrix (ECM) and Wound Healing over the Life Span27
| Age | Properties |
|---|---|
| Fetal | Highly regenerative skin |
| Large amount of cell mobility in a fragile ECM | |
| ECM rich in collagen III and hyaluronic acid | |
| Little inflammation in response to injury | |
| Scarless healing | |
| Juvenile | Massive production of type I collagen |
| Moderate and transient inflammation | |
| Cellular response in compliant ECM | |
| Early adult | Scarring properties at maximum |
| High production of type I collagen | |
| Fibrotic response in stiff ECM | |
| Aged adult | Prolonged inflammation |
| High matrix metalloproteinase and elastase expression | |
| Low expression of transforming growth factor beta | |
| Weakened cellular response in an atrophic ECM |
The microcirculation (arterioles, capillaries, venules) plays a critical role in wound healing. The vasoregulation of the microcirculation of aged skin is impaired, which reflects changes in inflammatory responses, fewer progenitor cells, and declines in circulatory mediators.31 Age-associated delays in microvascular responses to stressors lead to impaired temperature regulation and greater likelihood of tissue hypoperfusion,31 which inhibits wounds from reaching the angiogenic stage of repair. Optimal healing strategies after surgery and other stressors must therefore use multifactorial approaches to address changes in the microcirculation in older adults. Potential strategies include better use of existing vessels to optimize vasodilation (e.g., physical activity, pneumatic compression, pharmacological mediators);32–34 optimization of inflammatory and other cellular responses (e.g., stem cells);35,36 and strategies to address deficiencies in growth factors, sex steroids, and the extracellular matrix.37,38
MOLECULAR AND CELLULAR PROCESSES IN WOUND HEALING
Inflammation
Under normal wound healing conditions, early macrophages promote inflammation, and later macrophages clear neutrophils and switch to a reparative phenotype, but in the wounds of diabetic mice, macrophages fail to clear dying neutrophils and therefore remain in a proinflammatory phenotype.39 Similarly, in humans and mice, VLUs contain high levels of iron; thus, macrophages take up more iron and remain in a proinflammatory state.40 Although impairment in the switch from the proinflammatory to reparative phenotype is involved in chronic wounds, the intermediate steps between the two phenotypes are not clear. Whether an alteration in the macrophage switch affects wound healing in aging is unknown.
Excisional wounds heal more slowly in older mice than in young adult mice41 as a result of greater macrophage infiltration, especially at earlier phases of wound repair. Age-associated aberrations in macrophage functions decrease or delay vascularization, collagen deposition, and collagen remodeling.42 In contrast, scald wounds heal more slowly in older than younger mice, as a result of lower chemokine levels.43 Neutrophil depletion, which enhances wound healing in younger mammals,44 delays wound closure in aged mice.45 All these changes may arise from age-associated increases in basal or constitutive inflammation, which occur even in healthy individuals. Age-associated inflammation and delays in wound healing may have particular consequences for infection. In a mouse model of wounds inoculated with Staphylococcus aureus, older mice fail to clear the infection (Figure 2) and show less neutrophil chemotaxis, greater bacterial colonization, and slow macrophage infiltration.46
Figure 2.
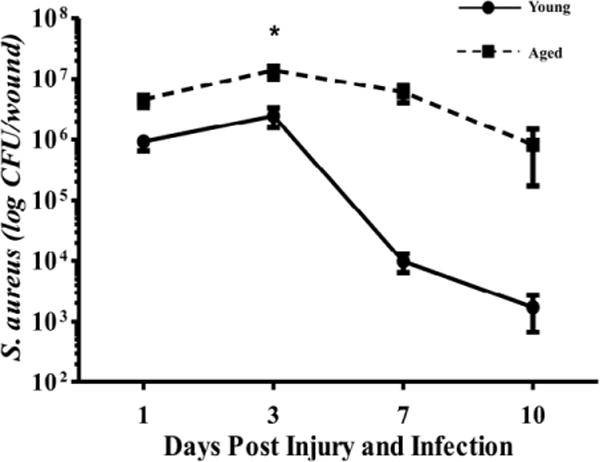
Implications of age-associated inflammation for infection. In a mouse model, older mice inoculated with Staphylococcus aureus fail to clear infection, unlike younger mice. *P < .001 versus young at same time point using two-way analysis of variance. Source: Brubaker et al.46
Age-associated inflammation is characterized by sustained high levels of proinflammatory cytokines, such as interleukin (IL)-6 and tumor necrosis factor alpha, and by declines in growth factors that are important for wound healing. TGF-β, which remains high during chronic inflammation, may promote the transformation of acute wounds into chronic ones by contributing to fibrotic replacement and scarring and by inhibiting reepithelialization.47 Angiotensin receptor signaling influences TGF-β expression. With diabetes mellitus or age, skin has greater expression of angiotensin II and the proinflammatory, vasoconstrictive AT1 receptor-signaling pathway.48–50 Treatment with the angiotensin receptor blocker (ARB) losartan improves muscle remodeling after injury,51 and individuals with diabetes mellitus taking ARBs are less likely to undergo amputation than those taking angiotensin-converting enzyme inhibitors,52 indicating that angiotensin receptor signaling increases fibrosis and satellite cell deactivation and may serve as a target for wound healing.
MITOCHONDRIAL DYSFUNCTION AND OXIDATIVE STRESS
Mitochondria provide energy and produce reactive oxygen species to drive the increased mitotic and synthetic activity necessary for wound healing. Oxidative stress is also necessary for cellular signaling, the clearing of bacteria, the transition into the proliferative phase of wound healing, and enhancement of angiogenesis through the production of mediators such as nitric oxide and the hypoxia-inducible factor 1α pathway.53 Because of high energy needs during wound repair and to avoid the overuse of mitochondria as the sole energy source, the process of adenosine triphosphate generation shifts from oxidative phosphorylation to glycolysis. Although glycolysis is less efficient than oxidative phosphorylation, it probably protects the mitochondrial pool from increasing damage related to oxidative stress.54 Furthermore, efficient mitochondrial turnover mechanisms in the form of mitophagy and mitobiogenesis are required to maintain a healthy pool of mitochondria, yet the skin is exposed to higher levels of extrinsic insults than other organs, which probably lead to dysfunctional mitochondria, low adenosine triphosphate production, and oxidative damage that triggers mitochondrial turnover. Skin mitochondria, particularly in exposed skin, have a greater incidence of mitochondrial deoxyribonucleic acid mutations with older age,55 indicating not only an increase in the number of dysfunctional mitochondria but also defects in eliminating them. The chronic inflammation seen with age and chronic conditions increases the number of dysfunctional mitochondria, and older age has been associated with lower levels of antioxidants,56 although the link between age-associated mitochondrial dysfunction and impaired wound healing has been poorly studied.
MICROBIAL BURDEN
The effect of microbial burden on wound healing is unknown and probably underestimated. Traditionally, studies of microbial burden have relied on culture-based techniques and therefore have excluded the vast majority of microbes. Because culture-based studies also exclude bacteria that rely on microbial community interactions, they provide little information about the biofilm, a factor thought to be critical in wound healing. Recent studies using 16S ribosomal ribonucleic acid–based gene sequencing and quantitative polymerase chain reaction have revealed that the skin and wounds have rich microbiomes with marked variability according to body region, wound type, and sampling method.57–59 In particular, Staphylococcus, Anaerococcus, Corynebacterium, and anaerobic species appear to contribute to microbial burden and wound behavior; for example, a genomic study of DFUs suggested a negative correlation between Staphylococcus burden and the depth and duration of the ulcer.57 Bacterial community structure also has been correlated with clinical data. Of 30 individuals with open fractures related to traumatic injury, bacterial community structure differed between those who later developed complications and those who did not, as well as between upper and lower extremity wounds.60 Further study using genomic sequencing techniques and clinical correlations might identify microbial burden associated with the development of chronic wounds, but the best collection methods are still unknown, and more standardization is needed to facilitate comparisons of studies. Moreover, rodent studies suggest that aging affects bacterial clearance, but no microbiome research has focused on older adults.
BASIC SCIENCE RESEARCH CONSIDERATIONS
In vitro models have yielded much information on the basic biology of wound healing, and more-complex, -reproducible, and -relevant systems, such time-lapse photography to measure wound parameters, are available, but the mechanical environment in which these models are studied differs from the human environment. Attempting to study too many variables in these models can hinder new understanding, yet models that mimic the combination of comorbid conditions that occur in aged humans are needed. Stem cell research is promising, but concerns about immunogenicity, teratomas and other malignancies, the ability to maintain pluripotency, and limited supply hamper use of stem cells, as do ethical concerns.
Many studies in wound repair have relied on animal models, particularly mouse models, to increase understanding of the phases of wound healing and the changes that occur with age, but skin morphology and the mechanisms of wound repair differ markedly between mice and humans. Pig skin is closest to human skin,61 but a long life span and higher maintenance costs limit the utility of pig models. Moreover, studies in animal models have focused primarily on excisional wounds; incisional wounds, abrasions, and burns are poorly studied. Furthermore, there are no models that mimic chronic wounds or the comorbidities commonly seen with human aging.
It has been difficult to identify predictive, diagnostic, and indicative biomarkers of wound healing because of the multifactorial pathogenesis and the heterogeneity of sampling spanning between and within wound types. Little is known regarding the contribution of aging in the context of specific biomarkers in older adults. Gene expression profiles have been identified in biopsies from VLUs, DFUs, and other chronic wounds, yielding a large number of potential biomarkers of nonhealing wounds,62–65 but the correlations between these tissue-based markers and wound healing outcomes and how to harness this information into predictive and diagnostic tools are not clear. Rapid tests that detect high MMP levels in wounds can identify a subset of individuals with poor wound healing,66–70 but variability in obtaining and measuring specimens limit these tests. It is still not clear which individuals might heal with standard of care, whether observed differences represent cause or effect, or how age influences such tests. Furthermore, polymerase chain reaction–based identification of bacterial species is under development as an approach to point-of-care diagnostics related to polymicrobial and biofilm-infected wounds.71,72 Substantial research is needed to identify, evaluate, and validate biomarkers related to wound healing in general and specifically in older adults.
CLINICAL RESEARCH ON CHRONIC WOUNDS
Novel Therapeutic Approaches
Cellular and Tissue-Engineered Products
Cellular and tissue-engineered products are often combined with standard-of-care approaches such as moist wound healing, compression, and offloading. A new product that distinguishes itself from current cellular and tissue-engineered products is a topical wound spray (HP802–247), which delivers a specific, optimized ratio of primed allogeneic fibroblasts and keratinocytes directly to the ulcer in a fibrin spray.73,74 Phase 2b study data indicate that HP802–247 promotes significant healing of VLUs, with the odds of wound healing being 2.75 times as great with HP802–247 than with the vehicle control.73,75 Confirmatory Phase 3 clinical trials are under way in the United States and Europe. In general, a lack of well-controlled and comparative data, clear mechanism(s) of action, and clear definitions that distinguish between cellular therapies, advanced therapies, and dressings has limited development of evidence-based clinical protocols for the therapeutic use of cellular and tissue-engineered approaches. The need for better defined regulatory and reimbursement pathways has also hampered such development. The potential influences of age on cellular and tissue-engineered products are also poorly characterized.
Negative-Pressure Wound Therapy
Although data from randomized controlled trials and meta-analyses suggest that negative-pressure wound therapy is effective in older adults,76–82 few studies have focused specifically on older adults, and there are not enough data for a clear recommendation. Many variables that may influence wound healing are defined inadequately in these studies,83 and the mechanism of action for negative-pressure wound therapy is poorly understood. Primary effects may include macrodeformation (wound contraction) and microdeformation (the microscopic interaction between the wound and dressing). Potential secondary effects include high cell proliferation and granulation tissue, perhaps as a result of changes in bacterial levels or cell stress.84–90
Hyperbaric Oxygen Therapy
The benefit of hyperbaric oxygen therapy is even less clear. In a recent meta-analysis of six randomized controlled trials and six observational studies, the observational studies showed a benefit, but the randomized trials did not,91 and none of the studies focused on older adults. A retrospective study also failed to show efficacy or effectiveness.92 Some animal data suggest that hyperbaric oxygen therapy is effective at all ages.93,94 New mechanistic studies of hyperbaric oxygen therapy are focusing on stem cells. Vasculogenic and mesenchymal stem cells incur damage with chronological and replicative aging, resulting in poorer differentiation than in younger cells95–97 and lack of mobilization,98–100 but few clinical data have correlated circulating cells with wound healing.101
Electrical Stimulation
Physical therapy approaches also show promise for wound healing. Although electrotherapy has not been assessed in large clinical trials, a meta-analysis of several small trials with individuals of all ages has found that it effectively promotes wound closure.102 Electrotherapy improves blood flow and prevents PUs in individuals with spinal cord injury,103 and it may improve take of grafts and flaps, improve vascularization, reduce necrosis, and increase angiogenesis in patients with VLUs or critical limb ischemia.104–106
Ultrasound
Low-frequency (22.5–35 kHz) ultrasound applied in contact rapidly debrides the wound surface and is a fairly comfortable procedure;107 many individuals decline pretreatment with lidocaine after one or two treatments. Several studies have shown that low-frequency contact ultrasound works synergistically with antibiotics to provide a better kill rate of antibiotic-resistant strains of bacteria and biofilms than antibiotics alone.108–111 Low-frequency ultrasound also reduces antimicrobial resistance in vitro.111 Data from a small clinical study of 17 individuals aged 32 to 83 with ulcers of mixed etiologies suggest that low-frequency ultrasound promotes healing of all wounds without antibiotics.109 The effectiveness of low-frequency ultrasound in healing chronic wounds of older adults is unclear. Larger randomized clinical trials are under way in Canada (NCT01973361) and Australia,112 but additional large, multicenter trials are needed.
Nutrition
Older adults categorized as undernourished are at risk of developing PUs and other complex wounds,113,114 although factors other than inadequate nutrient intake may confound this association.115 Commonly used putative markers of nutritional deficiency have low sensitivity and specificity as nutritional indicators in these older high-risk populations.115 Most of these individuals have multiple additional comorbidities, such as ongoing inflammation, disuse atrophy, or other metabolic disturbances, and these comorbidities can have a greater effect than nutritional intake in altering the putative nutritional markers.116 In addition, despite a wealth of nutritional studies, no consensus has been reached on optimal nutritional care for older adults with chronic wounds. The recommended daily protein allowance assumes that adults are healthy, consume high-quality protein, and have adequate energy intake.117 Recognizing that inflammation, the adequacy of energy intake, and other stressors common in older adults with complex wounds influence protein requirements, the Agency for Healthcare Research and Quality developed recommendations for protein intake for individuals with uncomplicated PUs, but these estimates are based on anecdotal evidence.117,118 There is conflicting evidence that dietary interventions or commercial supplementation are effective in preventing PUs or accelerating healing.118–121 Of the few studies that report evidence of benefit, most are methodologically weak, and their findings have yet to be verified.119,121–124 Further research is needed in this area, but disentangling nutritional needs from other factors affecting metabolic response to injury, especially when multiple comorbid conditions are present, remains a challenge.114,120,125
Clinical Research Considerations
The majority of wound care is performed in the outpatient setting, and clinical trials therefore focus on outpatient care, but the presence of a wound significantly affects inpatient costs, length of hospital stay, and discharge planning. Thus, future clinical studies will require a clear definition of hospital-based wound healing in older adults. Variations in data collection and in the definition, measurement, and treatment of wounds in older adults have hindered the development of such a definition. Measurable outcomes also must be defined, and several have been suggested. A well-structured electronic medical record that follows the individuals through the continuum of care facilitates the measurement of these variables for clinical outcomes and research (Table 3).
Table 3.
Potential Outcomes for Clinical Studies of Wound Healing in Older Adults
| Synergy between age and comorbidities132 |
| Pathology of tissue left behind in the wound133 |
| Costs of nonhealing wounds134 |
| Goals for healing at the time of wound presentation135,136 |
| Effects of standardized clinical decision support based on electronic medical records137 |
| Quality of life |
| Functional status |
| Morbidity |
| Pain |
| Level of independence |
| Sepsis |
| Prevention of amputation and mortality |
| Palliative care versus healing |
Approval of products or devices by the U.S. Food and Drug Administration (FDA) is a major driver in the design and conduct of clinical trials,126 but the approval process in general is long and expensive, and only one in 25 products is eventually approved. Approval is even more constrained for wound care. The FDA has approved only three products for wound care in the past 20 years127 and has defined only one endpoint—complete healing—for wounds. Thus, traditional, FDA-driven, randomized trials, albeit effective for assessing efficacy, may not inform clinical decision-making for wound care.126 Other study designs, such as pragmatic or comparative effectiveness approaches, might be more appropriate.128
A critical concern regarding clinical trial design for older adults is that of inclusion criteria. Clinical trial populations tend to be homogenous, and many comorbidities associated with older age are excluded. Age itself can be an exclusion criterion, but it is not clear that it should be. A meta-analysis of 10 trials has found that it is wound chronicity, rather than age, that plays a strong role in healing in individuals receiving standard care for DFUs.129 Another study found that the area and duration of the wound, but not age, influence healing of VLUs after spray therapy.130 Thus, age does not appear to be a significant factor in the response to wound treatment, although it can be an important predictor, as the formula derived from a clinical database for an ulcerated leg severity assessment illustrates.131
UNANSWERED QUESTIONS, FUTURE DIRECTIONS, AND RESEARCH CHALLENGES
Future research will require common definitions and standardized procedures for data collection and will need to address the analytical challenges associated with studying older adults, such as population heterogeneity, missing data from death or dropout, limited sample sizes, and variable follow-up times. Valid clinical and individual measures, particularly those of most value to the individuals, also are needed. With better measures and more data, the FDA might accept additional endpoints for clinical trials in wound care, particularly in older adults. Common comorbidities are a major concern in geriatrics and therefore should be explored in clinical trials and in basic and preclinical studies. Issues related to polypharmacy also should be explored. Specific research questions regarding wound healing in older adults are listed in Table 1.
Because the concept of chronic wounds crosses many disciplines, more collaboration is needed to answer common questions. Transdisciplinary collaboration between clinicians and basic scientists can facilitate development of animal models that more closely mimic human wound closure. Interaction between wound care clinicians and basic scientists can identify optimal strategies to obtain and use clinical samples, and multicenter collaborations among wound care clinicians, geriatricians, and gerontologists will improve clinical trial design for older adults and incorporate measures of QoL. Investigators studying wound healing can also learn from other fields, such as oncology, and engagement with government, industry, data-mining companies, and consulting groups might provide access to public and proprietary databases and information focused on public health. Potential resources are listed in Table 4.
Table 4.
Available or Forthcoming Resources
| Resource | Purpose |
|---|---|
| Infrastructure, databases, and registries | |
| U.S. Wound Registry (www.uswoundregistry.com) | Registry of de-identified data encompassing 100 hospital-based outpatient wound centers in 32 states and Puerto Rico |
| Designated by the Centers for Medicare and Medicaid Services as a Qualified Clinical Data Registry for the Physician Quality Reporting System | |
| Stony Brook University Clinical Decision Support system | Institutional review board–approved, electronic medical record–based system to facilitate enrollment in clinical studies |
| Measures | |
| EQ-5D | General quality-of-life instruments |
| Medical Outcomes Study 36-item Short-Form Health Survey | |
| Sickness Impact Profile | |
| Cardiff Wound Impact Schedule | Wound-specific quality-of-life instruments |
| Freiburg Life Quality Assessment | |
| Funding sources | |
| R21/R33 mechanism, National Institute on Aging | Link institutions to create infrastructure with multiple areas of expertise |
| Infrastructure to support clinical trials evaluating questions for which the sum is greater than all the parts |
Future research on wound healing in older adults will also benefit from efforts to address structural challenges in the research enterprise. Well-conducted education and implementation science studies can improve the ability of front-line providers to provide critical wound care, aid in convincing hospital and nursing home administrators of the value of educational programs, and increase implementation of preventive approaches. Perverse incentives related to the fee-for-service model, which has traditionally ignored prevention, also must be addressed. Moreover, development of a formal wound care specialty would promote consensus on standard wound care, provide a more-unified approach to wound research, and perhaps improve and expand cross-disciplinary educational approaches.
Acknowledgments
This workshop was supported by generous grants to ASP from the National Institute on Aging (1 U13 AG04093801) and the John A. Hartford Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of National Institute on Aging or the National Institutes of Health (NIH). In addition, the views expressed in written conference materials or publications and by speakers or moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, or organizations imply endorsement by the U.S. government. We are grateful to Nancy Woolard for her assistance with organizing the workshop. To see the agenda, a list of workshop moderators and attendees, and workshop presentations, please visit http://www.im.org/p/cm/ld/fid=599.
Footnotes
Conflict of Interest: Dr. Gould reports nonfinancial support from MiMedx, Cytomedix, Celleration, and Cardinal Health. Dr. Abadir has a patent pending on a novel, protective, anti-inflammatory receptor and its use in preservation of mitochondrial function, wound healing and repair. Dr. Davidson reports grants from NIH and the Department of Veterans Affairs. Dr. Fife is the Executive Director of The Chronic Disease Registry (d/b/a the U.S. Wound Registry), a 501c(3) organization that provided some of the data for this presentation, specifically the data on the use of biological dressings in older adults and their associated healing rates. Dr. Grice reports grants from Janssen Research and Development and consulting fees from GOJO, Amway International, GlaxoSmithKline, and L’Oreal. Dr. High reports grants from Chimerix, Sanofi-Pasteur, Optimer, Astellas; is a consultant for University of Virginia and the University of Minnesota; and has received other financial or material support from McGraw-Hill Publishers and Uptodate, Inc. Dr. Jacobson is an employee of Smith & Nephew, which produces the cell therapy product described in the presentation. Dr. McFarland Horne reports grants from John A. Hartford Foundation during the conduct of the study. Dr. Tomic-Canic reports grants from NIH, Organogenesis Inc., Novan, and Smith & Nephew; is a scientific board member for Molnlycke; and has the following patents: Methods and compositions for promoting wound healing issued to Hospital for Special Surgery; GM-CSF cosmeceutical compositions and methods of use thereof issued to NYU School of Medicine; Biological markers of chronic wound tissue and methods of using for criteria in surgical debridement pending to NYU School of Medicine; De novo synthesis of glucocortocoid in the epidermis and it uses and applications patent pending to NYU School of Medicine; and growth factor-mediated cosmeceuticals and use of thereof to enhances skin quality patent pending to NYU School of Medicine.
Author Contributions: Drs Gould and Schmader were co-chairs for the conference. Dr. McFarland-Horne drafted the manuscript. All authors served on the conference planning committee or presented material at the conference. All authors reviewed and approved the final manuscript submitted for publication.
Sponsor’s Role: None.
References
- 1.Margolis DJ, Bilker W, Santanna J, et al. Venous leg ulcer: Incidence and prevalence in the elderly. J Am Acad Dermatol. 2002;46:381–386. doi: 10.1067/mjd.2002.121739. [DOI] [PubMed] [Google Scholar]
- 2.Margolis DJ, Bilker W, Knauss J, et al. The incidence and prevalence of pressure ulcers among elderly patients in general medical practice. Ann Epidemiol. 2002;12:321–325. doi: 10.1016/s1047-2797(01)00255-1. [DOI] [PubMed] [Google Scholar]
- 3.Bickers DR, Lim HW, Margolis D, et al. The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55:490–500. doi: 10.1016/j.jaad.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 4.Badia JG, Santos AB, Segura JC, et al. Predictors of mortality among elderly dependent home care patients. BMC Health Serv Res. 2013;13:316. doi: 10.1186/1472-6963-13-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hopman WM, Harrison MB, Coo H, et al. Associations between chronic disease, age and physical and mental health status. Chronic Dis Can. 2009;29:108–116. [PubMed] [Google Scholar]
- 6.Redekop WK, Stolk EA, Kok E, et al. Diabetic foot ulcers and amputations: Estimates of health utility for use in cost-effectiveness analyses of new treatments. Diabetes Metab. 2004;30:549–556. doi: 10.1016/s1262-3636(07)70154-4. [DOI] [PubMed] [Google Scholar]
- 7.Horn SD, Fife CE, Smout RJ, et al. Development of a wound healing index for patients with chronic wounds. Wound Repair Regen. 2013;21:823–832. doi: 10.1111/wrr.12107. [DOI] [PubMed] [Google Scholar]
- 8.Edwards H, Finlayson K, Courtney M, et al. Health service pathways for patients with chronic leg ulcers: Identifying effective pathways for facilitation of evidence based wound care. BMC Health Serv Res. 2013;13:86. doi: 10.1186/1472-6963-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carter MJ. Cost-effectiveness research in wound care: Definitions, approaches, and limitations. Ostomy Wound Manage. 2010;56:48–59. [PubMed] [Google Scholar]
- 10.Harms S, Bliss DZ, Garrard J, et al. Prevalence of pressure ulcers by race and ethnicity for older adults admitted to nursing homes. J Gerontol Nurs. 2014;40:20–26. doi: 10.3928/00989134-20131028-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coleman S, Gorecki C, Nelson EA, et al. Patient risk factors for pressure ulcer development: Systematic review. Int J Nurs Stud. 2013;50:974–1003. doi: 10.1016/j.ijnurstu.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Yin J, Cai X, et al. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011;306:179–186. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baumgarten M, Margolis D, van Doorn C, et al. Black/white differences in pressure ulcer incidence in nursing home residents. J Am Geriatr Soc. 2004;52:1293–1298. doi: 10.1111/j.1532-5415.2004.52358.x. [DOI] [PubMed] [Google Scholar]
- 14.Lanting LC, Joung IM, Mackenbach JP, et al. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: A review. Diabetes Care. 2005;28:2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- 15.Dillingham TR, Pezzin LE, Mackenzie EJ. Racial differences in the incidence of limb loss secondary to peripheral vascular disease: A population-based study. Arch Phys Med Rehabil. 2002;83:1252–1257. doi: 10.1053/apmr.2002.34805. [DOI] [PubMed] [Google Scholar]
- 16.Lavery LA, van Houtum WH, Ashry HR, et al. Diabetes-related lower-extremity amputations disproportionately affect Blacks and Mexican Americans. South Med J. 1999;92:593–599. doi: 10.1097/00007611-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Holman KH, Henke PK, Dimick JB, et al. Racial disparities in the use of revascularization before leg amputation in Medicare patients. J Vasc Surg. 2011;54:420–426. doi: 10.1016/j.jvs.2011.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowe VL, Weaver FA, Lane JS, et al. Racial and ethnic differences in patterns of treatment for acute peripheral arterial disease in the United States, 1998–2006. J Vasc Surg. 2010;51(4 Suppl):21S–26S. doi: 10.1016/j.jvs.2009.09.066. [DOI] [PubMed] [Google Scholar]
- 19.Regenbogen SE, Gawande AA, Lipsitz SR, et al. Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Ann Surg. 2009;250:424–431. doi: 10.1097/SLA.0b013e3181b41d53. [DOI] [PubMed] [Google Scholar]
- 20.Shaw TJ, Martin P. Wound repair at a glance. J Cell Sci. 2009;122(Pt 18):3209–3213. doi: 10.1242/jcs.031187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mirza R, DiPietro LA, Koh TJ. Selective and specific macrophage ablation is detrimental to wound healing in mice. Am J Pathol. 2009;175:2454–2462. doi: 10.2353/ajpath.2009.090248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agren MS, Steenfos HH, Dabelsteen S, et al. Proliferation and mitogenic response to PDGF-BB of fibroblasts isolated from chronic venous leg ulcers is ulcer-age dependent. J Invest Dermatol. 1999;112:463–469. doi: 10.1046/j.1523-1747.1999.00549.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim BC, Kim HT, Park SH, et al. Fibroblasts from chronic wounds show altered TGF-beta-signaling and decreased TGF-beta Type II receptor expression. J Cell Physiol. 2003;195:331–336. doi: 10.1002/jcp.10301. [DOI] [PubMed] [Google Scholar]
- 24.Falanga V, Zhou L, Yufit T. Low oxygen tension stimulates collagen synthesis and COL1A1 transcription through the action of TGF-beta1. J Cell Physiol. 2002;191:42–50. doi: 10.1002/jcp.10065. [DOI] [PubMed] [Google Scholar]
- 25.Zhang X, Sarkar K, Rey S, et al. Aging impairs the mobilization and homing of bone marrow-derived angiogenic cells to burn wounds. J Mol Med. 2011;89:985–995. doi: 10.1007/s00109-011-0754-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Du J, Liu L, Lay F, et al. Combination of HIF-1alpha gene transfection and HIF-1-activated bone marrow-derived angiogenic cell infusion improves burn wound healing in aged mice. Gene Ther. 2013;20:1070–1076. doi: 10.1038/gt.2013.32. [DOI] [PubMed] [Google Scholar]
- 27.Gurtner GC, Werner S, Barrandon Y, et al. Wound repair and regeneration. Nature. 2008;453:314–321. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 28.Ashcroft GS, Mills SJ, Ashworth JJ. Ageing and wound healing. Biogerontology. 2002;3:337–345. doi: 10.1023/a:1021399228395. [DOI] [PubMed] [Google Scholar]
- 29.Ballas CB, Davidson JM. Delayed wound healing in aged rats is associated with increased collagen gel remodeling and contraction by skin fibroblasts, not with differences in apoptotic or myofibroblast cell populations. Wound Repair Regen. 2001;9:223–237. doi: 10.1046/j.1524-475x.2001.00223.x. [DOI] [PubMed] [Google Scholar]
- 30.Ashcroft GS, Horan MA, Herrick SE, et al. Age-related differences in the temporal and spatial regulation of matrix metalloproteinases (MMPs) in normal skin and acute cutaneous wounds of healthy humans. Cell Tissue Res. 1997;290:581–591. doi: 10.1007/s004410050963. [DOI] [PubMed] [Google Scholar]
- 31.Bentov I, Reed MJ. Anesthesia, microcirculation, and wound repair in aging. Anesthesiology. 2014;120:760–772. doi: 10.1097/ALN.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoshida H, Itoh S, Hara T, et al. A phosphodiesterase 3 inhibitor, K-134, improves hindlimb skeletal muscle circulation in rat models of peripheral arterial disease. Atherosclerosis. 2012;221:84–90. doi: 10.1016/j.atherosclerosis.2011.12.044. [DOI] [PubMed] [Google Scholar]
- 33.Krcma M, Cechurova D, Jankovec Z, et al. Effect of mild increase of physical activity on microvasculary reactivity in obese subjects with diabetes mellitus type 2. Exp Clin Endocrinol Diabetes. 2009;117:150–152. doi: 10.1055/s-0028-1100417. [DOI] [PubMed] [Google Scholar]
- 34.Husmann M, Willenberg T, Keo HH, et al. Integrity of venoarteriolar reflex determines level of microvascular skin flow enhancement with intermittent pneumatic compression. J Vasc Surg. 2008;48:1509–1513. doi: 10.1016/j.jvs.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 35.Scalia R. The microcirculation in adipose tissue inflammation. Rev Endocr Metab Disord. 2013;14:69–76. doi: 10.1007/s11154-013-9236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jadlowiec C, Brenes RA, Li X, et al. Stem cell therapy for critical limb ischemia: What can we learn from cell therapy for chronic wounds? Vascular. 2012;20:284–289. doi: 10.1258/vasc.2011.201206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roubelakis MG, Trohatou O, Roubelakis A, et al. Platelet-rich plasma (PRP) promotes fetal mesenchymal stem/stromal cell migration and wound healing process. Stem Cell Rev. 2014;10:417–428. doi: 10.1007/s12015-013-9494-8. [DOI] [PubMed] [Google Scholar]
- 38.Makrantonaki E, Zouboulis CC. Androgens and ageing of the skin. Curr Opin Endocrinol Diabetes Obes. 2009;16:240–245. doi: 10.1097/MED.0b013e32832b71dc. [DOI] [PubMed] [Google Scholar]
- 39.Khanna S, Biswas S, Shang Y, et al. Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLoS One. 2010;5:e9539. doi: 10.1371/journal.pone.0009539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sindrilaru A, Peters T, Wieschalka S, et al. An unrestrained proinflammatory M1 macrophage population induced by iron impairs wound healing in humans and mice. J Clin Invest. 2011;121:985–997. doi: 10.1172/JCI44490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swift ME, Kleinman HK, DiPietro LA. Impaired wound repair and delayed angiogenesis in aged mice. Lab Invest. 1999;79:1479–1487. [PubMed] [Google Scholar]
- 42.Swift ME, Burns AL, Gray KL, et al. Age-related alterations in the inflammatory response to dermal injury. J Invest Dermatol. 2001;117:1027–1035. doi: 10.1046/j.0022-202x.2001.01539.x. [DOI] [PubMed] [Google Scholar]
- 43.Shallo H, Plackett TP, Heinrich SA, et al. Monocyte chemoattractant protein-1 (MCP-1) and macrophage infiltration into the skin after burn injury in aged mice. Burns. 2003;29:641–647. doi: 10.1016/s0305-4179(03)00070-6. [DOI] [PubMed] [Google Scholar]
- 44.Dovi JV, Szpaderska AM, DiPietro LA. Neutrophil function in the healing wound: Adding insult to injury? Thromb Haemost. 2004;92:275–280. doi: 10.1160/TH03-11-0720. [DOI] [PubMed] [Google Scholar]
- 45.Nishio N, Okawa Y, Sakurai H, et al. Neutrophil depletion delays wound repair in aged mice. Age (Dordr) 2008;30:11–19. doi: 10.1007/s11357-007-9043-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brubaker AL, Rendon JL, Ramirez L, et al. Reduced neutrophil chemotaxis and infiltration contributes to delayed resolution of cutaneous wound infection with advanced age. J Immunol. 2013;190:1746–1757. doi: 10.4049/jimmunol.1201213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurosaka M, Suzuki T, Hosono K, et al. Reduced angiogenesis and delay in wound healing in angiotensin II type 1a receptor-deficient mice. Biomed Pharmacother. 2009;63:627–634. doi: 10.1016/j.biopha.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 48.Hao SY, Ren M, Yang C, et al. Activation of skin reninangiotensin system in diabetic rats. Endocrine. 2011;39:242–250. doi: 10.1007/s12020-010-9428-z. [DOI] [PubMed] [Google Scholar]
- 49.Yevdokimova N, Podpryatov S. The up-regulation of angiotensin II receptor type 1 and connective tissue growth factor are involved in high-glucose-induced fibronectin production by cultured human dermal fibroblasts. J Dermatol Sci. 2007;47:127–139. doi: 10.1016/j.jdermsci.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 50.Abiko M, Rodgers KE, Campeau JD, et al. Alterations of angiotensin II receptor levels in sutured wounds in rat skin. J Invest Surg. 1996;9:447–453. doi: 10.3109/08941939609025862. [DOI] [PubMed] [Google Scholar]
- 51.Burks TN, Andres-Mateos E, Marx R, et al. Losartan restores skeletal muscle remodeling and protects against disuse atrophy in sarcopenia. Sci Transl Med. 2011;3:82ra37. doi: 10.1126/scitranslmed.3002227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Margolis DJ, Hoffstad O, Thom S, et al. The differential effect of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers with respect to foot ulcer and limb amputation in those with diabetes. Wound Repair Regen. 2010;18:445–451. doi: 10.1111/j.1524-475X.2010.00624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schafer M, Werner S. Oxidative stress in normal and impaired wound repair. Pharmacol Res. 2008;58:165–171. doi: 10.1016/j.phrs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 54.Im MJ, Hoopes JE. Energy metabolism in healing skin wounds. J Surg Res. 1970;10:459–464. doi: 10.1016/0022-4804(70)90070-3. [DOI] [PubMed] [Google Scholar]
- 55.Yang JH, Lee HC, Lin KJ, et al. A specific 4977-bp deletion of mitochondrial DNA in human ageing skin. Arch Dermatol Res. 1994;286:386–390. doi: 10.1007/BF00371798. [DOI] [PubMed] [Google Scholar]
- 56.Taylor R, James T. The role of oxidative stress in the development and persistence of pressure ulcers. In: Bader D, Bouten C, Colin D, et al., editors. Pressure Ulcer Research. Berlin, Heidelberg: Springer; 2005. pp. 205–232. [Google Scholar]
- 57.Gardner SE, Hillis SL, Heilmann K, et al. The neuropathic diabetic foot ulcer microbiome is associated with clinical factors. Diabetes. 2013;62:923–930. doi: 10.2337/db12-0771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Price LB, Liu CM, Frankel YM, et al. Macroscale spatial variation in chronic wound microbiota: A cross-sectional study. Wound Repair Regen. 2011;19:80–88. doi: 10.1111/j.1524-475X.2010.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Han A, Zenilman JM, Melendez JH, et al. The importance of a multifaceted approach to characterizing the microbial flora of chronic wounds. Wound Repair Regen. 2011;19:532–541. doi: 10.1111/j.1524-475X.2011.00720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hannigan GD, Hodkinson BP, McGinnis K, et al. Culture-independent pilot study of microbiota colonizing open fractures and association with severity, mechanism, location, and complication from presentation to early outpatient follow-up. J Orthop Res. 2014;32:597–605. doi: 10.1002/jor.22578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sullivan TP, Eaglstein WH, Davis SC, et al. The pig as a model for human wound healing. Wound Repair Regen. 2001;9:66–76. doi: 10.1046/j.1524-475x.2001.00066.x. [DOI] [PubMed] [Google Scholar]
- 62.Stojadinovic O, Pastar I, Vukelic S, et al. Deregulation of keratinocyte differentiation and activation: A hallmark of venous ulcers. J Cell Mol Med. 2008;12:2675–2690. doi: 10.1111/j.1582-4934.2008.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Charles CA, Tomic-Canic M, Vincek V, et al. A gene signature of nonhealing venous ulcers: Potential diagnostic markers. J Am Acad Dermatol. 2008;59:758–771. doi: 10.1016/j.jaad.2008.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117:1219–1222. doi: 10.1172/JCI32169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gallagher KA, Liu ZJ, Xiao M, et al. Diabetic impairments in NO-mediated endothelial progenitor cell mobilization and homing are reversed by hyperoxia and SDF-1 alpha. J Clin Invest. 2007;117:1249–1259. doi: 10.1172/JCI29710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schultz GS, Gibson D. Measurement of biomarkers for impaired healing in fluids and tissues. In: Mani R, Romanelli M, Shukla V, editors. Measurements in Wound Healing. London: Springer; 2013. pp. 243–258. [Google Scholar]
- 67.Liu Y, Min D, Bolton T, et al. Increased matrix metalloproteinase-9 predicts poor wound healing in diabetic foot ulcers. Diabetes Care. 2009;32:11711–11719. doi: 10.2337/dc08-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gibson D, Cullen B, Legerstee R, et al. MMPs made easy. Wounds Int. 2009;1:1–6. [Google Scholar]
- 69.Rayment EA, Upton Z, Shooter GK. Increased matrix metalloproteinase-9 (MMP-9) activity observed in chronic wound fluid is related to the clinical severity of the ulcer. Br J Dermatol. 2008;158:951–961. doi: 10.1111/j.1365-2133.2008.08462.x. [DOI] [PubMed] [Google Scholar]
- 70.Ladwig GP, Robson MC, Liu R, et al. Ratios of activated matrix metallo-proteinase-9 to tissue inhibitor of matrix metalloproteinase-1 in wound fluids are inversely correlated with healing of pressure ulcers. Wound Repair Regen. 2002;10:26–37. doi: 10.1046/j.1524-475x.2002.10903.x. [DOI] [PubMed] [Google Scholar]
- 71.Wolcott RD, Dowd SE. A rapid molecular method for characterising bacterial bioburden in chronic wounds. J Wound Care. 2008;17:513–516. doi: 10.12968/jowc.2008.17.12.31769. [DOI] [PubMed] [Google Scholar]
- 72.Dowd SE, Wolcott RD, Kennedy J, et al. Molecular diagnostics and personalised medicine in wound care: Assessment of outcomes. J Wound Care. 2011;20:232, 234–239. doi: 10.12968/jowc.2011.20.5.232. [DOI] [PubMed] [Google Scholar]
- 73.Kirsner RS, Marston WA, Snyder RJ, et al. Spray-applied cell therapy with human allogeneic fibroblasts and keratinocytes for the treatment of chronic venous leg ulcers: A phase 2, multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2012;380:977–985. doi: 10.1016/S0140-6736(12)60644-8. [DOI] [PubMed] [Google Scholar]
- 74.Goedkoop R, Juliet R, You PH, et al. Wound stimulation by growth-arrested human keratinocytes and fibroblasts: HP802–247, a new-generation allogeneic tissue engineering product. Dermatology. 2010;220:114–120. doi: 10.1159/000277380. [DOI] [PubMed] [Google Scholar]
- 75.Kirsner RS, Marston WA, Snyder RJ, et al. Durability of healing from spray-applied cell therapy with human allogeneic fibroblasts and keratinocytes for the treatment of chronic venous leg ulcers: A 6-month follow-up. Wound Repair Regen. 2013;21:682–687. doi: 10.1111/wrr.12076. [DOI] [PubMed] [Google Scholar]
- 76.Ruttermann M, Maier-Hasselmann A, Nink-Grebe B, et al. Local treatment of chronic wounds: In patients with peripheral vascular disease, chronic venous insufficiency, and diabetes. Dtsch Arztebl Int. 2013;110:25–31. doi: 10.3238/arztebl.2013.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Othman D. Negative pressure wound therapy literature review of efficacy, cost effectiveness, and impact on patients’ quality of life in chronic wound management and its implementation in the United Kingdom. Plast Surg Int. 2012;2012:374–398. doi: 10.1155/2012/374398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ubbink DT, Westerbos SJ, Nelson EA, et al. A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg. 2008;95:685–692. doi: 10.1002/bjs.6238. [DOI] [PubMed] [Google Scholar]
- 79.Vikatmaa P, Juutilainen V, Kuukasjarvi P, et al. Negative pressure wound therapy: A systematic review on effectiveness and safety. Eur J Vasc Endovasc Surg. 2008;36:438–448. doi: 10.1016/j.ejvs.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 80.Blume PA, Walters J, Payne W, et al. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: A multicenter randomized controlled trial. Diabetes Care. 2008;31:631–636. doi: 10.2337/dc07-2196. [DOI] [PubMed] [Google Scholar]
- 81.Vuerstaek JD, Vainas T, Wuite J, et al. State-of-the-art treatment of chronic leg ulcers: A randomized controlled trial comparing vacuum-assisted closure (V.A.C.) with modern wound dressings. J Vasc Surg. 2006;44:1029–1037. doi: 10.1016/j.jvs.2006.07.030. discussion 1038. [DOI] [PubMed] [Google Scholar]
- 82.Llanos S, Danilla S, Barraza C, et al. Effectiveness of negative pressure closure in the integration of split thickness skin grafts: A randomized, double-masked, controlled trial. Ann Surg. 2006;244:700–705. doi: 10.1097/01.sla.0000217745.56657.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Birke-Sorensen H, Malmsjo M, Rome P, et al. Evidence-based recommendations for negative pressure wound therapy: Treatment variables (pressure levels, wound filler and contact layer)—steps towards an international consensus. J Plast Reconstr Aesthet Surg. 2011;64(Suppl):S1–S16. doi: 10.1016/j.bjps.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 84.Cameron AR, Frith JE, Gomez GA, et al. The effect of time-dependent deformation of viscoelastic hydrogels on myogenic induction and Rac1 activity in mesenchymal stem cells. Biomaterials. 2014;35:1857–1868. doi: 10.1016/j.biomaterials.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 85.Sahin I, Ozturk S, Deveci M, et al. Experimental assessment of the neovascularisation of acellular dermal matrix in the wound bed pretreated with mesenchymal stem cell under subatmospheric pressure. J Plast Reconstr Aesthet Surg. 2014;67:107–114. doi: 10.1016/j.bjps.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 86.Muller P, Langenbach A, Kaminski A, et al. Modulating the actin cytoskeleton affects mechanically induced signal transduction and differentiation in mesenchymal stem cells. PLoS One. 2013;8:e71283. doi: 10.1371/journal.pone.0071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wiegand C, White R. Microdeformation in wound healing. Wound Repair Regen. 2013;21:793–799. doi: 10.1111/wrr.12111. [DOI] [PubMed] [Google Scholar]
- 88.Li Z, Yao SJ, Alini M, et al. Chondrogenesis of human bone marrow mesenchymal stem cells in fibrin-polyurethane composites is modulated by frequency and amplitude of dynamic compression and shear stress. Tissue Eng Part A. 2010;16:575–584. doi: 10.1089/ten.TEA.2009.0262. [DOI] [PubMed] [Google Scholar]
- 89.Wozniak MA, Kwong L, Chodniewicz D, et al. R-Ras controls membrane protrusion and cell migration through the spatial regulation of Rac and Rho. Mol Biol Cell. 2005;16:84–96. doi: 10.1091/mbc.E04-04-0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Katsumi A, Milanini J, Kiosses WB, et al. Effects of cell tension on the small GTPase Rac. J Cell Biol. 2002;158:153–164. doi: 10.1083/jcb.200201105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.O’Reilly D, Pasricha A, Campbell K, et al. Hyperbaric oxygen therapy for diabetic ulcers: Systematic review and meta-analysis. Int J Technol Assess Health Care. 2013;29:269–281. doi: 10.1017/S0266462313000263. [DOI] [PubMed] [Google Scholar]
- 92.Margolis DJ, Gupta J, Hoffstad O, et al. Lack of effectiveness of hyper-baric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation: A cohort study. Diabetes Care. 2013;36:1961–1966. doi: 10.2337/dc12-2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gomez CR, Knutson GJ, Clifton KB, et al. Age-dependent response of murine female bone marrow cells to hyperbaric oxygen. Biogerontology. 2012;13:287–297. doi: 10.1007/s10522-012-9373-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bonomo SR, Davidson JD, Tyrone JW, et al. Enhancement of wound healing by hyperbaric oxygen and transforming growth factor beta3 in a new chronic wound model in aged rabbits. Arch Surg. 2000;135:1148–1153. doi: 10.1001/archsurg.135.10.1148. [DOI] [PubMed] [Google Scholar]
- 95.Liu L, Rando TA. Manifestations and mechanisms of stem cell aging. J Cell Biol. 2011;193:257–266. doi: 10.1083/jcb.201010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nishimura EK, Granter SR, Fisher DE. Mechanisms of hair graying: Incomplete melanocyte stem cell maintenance in the niche. Science. 2005;307:720–724. doi: 10.1126/science.1099593. [DOI] [PubMed] [Google Scholar]
- 97.Maslov AY, Barone TA, Plunkett RJ, et al. Neural stem cell detection, characterization, and age-related changes in the subventricular zone of mice. J Neurosci. 2004;24:1726–1733. doi: 10.1523/JNEUROSCI.4608-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Richa E, Papari M, Allen J, et al. Older age but not donor health impairs allogeneic granulocyte colony-stimulating factor (G-CSF) peripheral blood stem cell mobilization. Biol Blood Marrow Transplant. 2009;15:1394–1399. doi: 10.1016/j.bbmt.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 99.Wang TF, Wen SH, Chen RL, et al. Factors associated with peripheral blood stem cell yield in volunteer donors mobilized with granulocyte colony-stimulating factors: The impact of donor characteristics and procedural settings. Biol Blood Marrow Transplant. 2008;14:1305–1311. doi: 10.1016/j.bbmt.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 100.Suzuya H, Watanabe T, Nakagawa R, et al. Factors associated with granulocyte colony-stimulating factor-induced peripheral blood stem cell yield in healthy donors. Vox Sang. 2005;89:229–235. doi: 10.1111/j.1423-0410.2005.00701.x. [DOI] [PubMed] [Google Scholar]
- 101.Tecilazich F, Dinh T, Pradhan-Nabzdyk L, et al. Role of endothelial progenitor cells and inflammatory cytokines in healing of diabetic foot ulcers. PLoS One. 2013;8:e83314. doi: 10.1371/journal.pone.0083314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koel G, Houghton PE. Electrostimulation: Current status, strength of evidence Guidelines, and meta-analysis. Adv Wound Care (New Rochelle) 2014;3:118–126. doi: 10.1089/wound.2013.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gyawali S, Solis L, Chong SL, et al. Intermittent electrical stimulation redistributes pressure and promotes tissue oxygenation in loaded muscles of individuals with spinal cord injury. J Appl Physiol. 2011;110:246–255. doi: 10.1152/japplphysiol.00661.2010. [DOI] [PubMed] [Google Scholar]
- 104.Zhao M, Bai H, Wang E, et al. Electrical stimulation directly induces preangiogenic responses in vascular endothelial cells by signaling through VEGF receptors. J Cell Sci. 2004;117(Pt 3):397–405. doi: 10.1242/jcs.00868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Goldman R, Brewley B, Zhou L, et al. Electrotherapy reverses inframalleolar ischemia: A retrospective, observational study. Adv Skin Wound Care. 2003;16:79–89. doi: 10.1097/00129334-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 106.Junger M, Zuder D, Steins A, et al. Treatment of venous ulcers with low frequency pulsed current (Dermapulse): Effects on cutaneous microcirculation. Hautarzt. 1997;48:897–903. doi: 10.1007/s001050050682. [DOI] [PubMed] [Google Scholar]
- 107.Herberger K, Franzke N, Blome C, et al. Efficacy, tolerability and patient benefit of ultrasound-assisted wound treatment versus surgical debridement: A randomized clinical study. Dermatology. 2011;222:244–249. doi: 10.1159/000326116. [DOI] [PubMed] [Google Scholar]
- 108.Qian Z, Sagers RD, Pitt WG. The effect of ultrasonic frequency upon enhanced killing of P. aeruginosa biofilms. Ann Biomed Eng. 1997;25:69–76. doi: 10.1007/BF02738539. [DOI] [PubMed] [Google Scholar]
- 109.Breuing KH, Bayer L, Neuwalder J, et al. Early experience using low-frequency ultrasound in chronic wounds. Ann Plast Surg. 2005;55:183–187. doi: 10.1097/01.sap.0000168695.20350.07. [DOI] [PubMed] [Google Scholar]
- 110.Carmen JC, Roeder BL, Nelson JL, et al. Ultrasonically enhanced vancomycin activity against Staphylococcus epidermidis biofilms in vivo. J Biomater Appl. 2004;18:237–245. doi: 10.1177/0885328204040540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Conner-Kerr T, Alston G, Stovall A, et al. The effects of low-frequency ultrasound (35 kHz) on methicillin-resistant Staphylococcus aureus (MRSA) in vitro. Ostomy Wound Manage. 2010;56:32–43. [PubMed] [Google Scholar]
- 112.Michailidis L, Williams CM, Bergin SM, et al. Comparison of healing rate in diabetes-related foot ulcers with low frequency ultrasonic debridement versus non-surgical sharps debridement: A randomised trial protocol. J Foot Ankle Res. 2014;7:1–18. doi: 10.1186/1757-1146-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sherman AR, Barkley M. Nutrition and wound healing. J Wound Care. 2011;20:357–367. doi: 10.12968/jowc.2011.20.8.357. [DOI] [PubMed] [Google Scholar]
- 114.Williams JZ, Barbul A. Nutrition and wound healing. Crit Care Nurs Clin North Am. 2012;24:179–200. doi: 10.1016/j.ccell.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 115.Jensen GL, Compher C, Sullivan DH, et al. Recognizing malnutrition in adults: Definitions and characteristics, screening, assessment, and team approach. JPEN J Parenter Enteral Nutr. 2013;37:802–807. doi: 10.1177/0148607113492338. [DOI] [PubMed] [Google Scholar]
- 116.Legendre C, Debure C, Meaume S, et al. Impact of protein deficiency on venous ulcer healing. J Vasc Surg. 2008;48:688–693. doi: 10.1016/j.jvs.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 117.Castellanos VH, Litchford MD, Campbell WW. Modular protein supplements and their application to long-term care. Nutr Clin Pract. 2006;21:485–504. doi: 10.1177/0115426506021005485. [DOI] [PubMed] [Google Scholar]
- 118.Dorner B, Posthauer ME, Thomas D, et al. The role of nutrition in pressure ulcer prevention and treatment: National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care. 2009;22:212–221. doi: 10.1097/01.ASW.0000350838.11854.0a. [DOI] [PubMed] [Google Scholar]
- 119.Langer G, Knerr A, Kuss O, et al. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2009;(3):CD003216. doi: 10.1002/14651858.CD003216. [DOI] [PubMed] [Google Scholar]
- 120.Lin JJ, Chung XJ, Yang CY, et al. A meta-analysis of trials using the intention to treat principle for glutamine supplementation in critically ill patients with burn. Burns. 2013;39:565–570. doi: 10.1016/j.burns.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 121.Little MO. Nutrition and skin ulcers. Curr Opin Clin Nutr Metab Care. 2013;16:39–49. doi: 10.1097/MCO.0b013e32835bc0a1. [DOI] [PubMed] [Google Scholar]
- 122.Desneves KJ, Todorovic BE, Cassar A, et al. Treatment with supplementary arginine, vitamin C and zinc in patients with pressure ulcers: A randomised controlled trial. Clin Nutr. 2005;24:979–987. doi: 10.1016/j.clnu.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 123.Ohura T, Nakajo T, Okada S, et al. Evaluation of effects of nutrition intervention on healing of pressure ulcers and nutritional states (randomized controlled trial) Wound Repair Regen. 2011;19:330–336. doi: 10.1111/j.1524-475X.2011.00691.x. [DOI] [PubMed] [Google Scholar]
- 124.Blass SC, Goost H, Tolba RH, et al. Time to wound closure in trauma patients with disorders in wound healing is shortened by supplements containing antioxidant micronutrients and glutamine: A PRCT. Clin Nutr. 2012;31:469–475. doi: 10.1016/j.clnu.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 125.Mathus-Vliegen EM. Old age, malnutrition, and pressure sores: An illfated alliance. J Gerontol A Biol Sci Med Sci. 2004;59A:355–360. doi: 10.1093/gerona/59.4.m355. [DOI] [PubMed] [Google Scholar]
- 126.Eaglstein WH, Kirsner RS, Robson MC. Food and Drug Administration (FDA) drug approval end points for chronic cutaneous ulcer studies. Wound Repair Regen. 2012;20:793–796. doi: 10.1111/j.1524-475X.2012.00849.x. [DOI] [PubMed] [Google Scholar]
- 127.Armstrong DG, Wrobel J, Robbins JM. Guest editorial: Are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007;4:286–287. doi: 10.1111/j.1742-481X.2007.00392.x. [DOI] [PubMed] [Google Scholar]
- 128.Eaglstein WH, Kirsner RS. Expectations for comparative effectiveness and efficacy research: With welcomed questions may come unwelcome answers. JAMA Dermatol. 2013;149:18–19. doi: 10.1001/jamadermatol.2013.1324. [DOI] [PubMed] [Google Scholar]
- 129.Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis Diabetes Care. 1999;22:692–695. doi: 10.2337/diacare.22.5.692. [DOI] [PubMed] [Google Scholar]
- 130.Lantis JC, II, Marston WA, Farber A, et al. The influence of patient and wound variables on healing of venous leg ulcers in a randomized controlled trial of growth-arrested allogeneic keratinocytes and fibroblasts. J Vasc Surg. 2013;58:433–439. doi: 10.1016/j.jvs.2012.12.055. [DOI] [PubMed] [Google Scholar]
- 131.Kulkarni SR, Gohel MS, Wakely C, et al. The Ulcerated Leg Severity Assessment score for prediction of venous leg ulcer healing. Br J Surg. 2007;94:189–193. doi: 10.1002/bjs.5597. [DOI] [PubMed] [Google Scholar]
- 132.Brem H, Tomic-Canic M, Entero H, et al. The synergism of age and db/db genotype impairs wound healing. Exp Gerontol. 2007;42:523–531. doi: 10.1016/j.exger.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 133.Golinko MS, Joffe R, de Vinck D, et al. Surgical pathology to describe the clinical margin of debridement of chronic wounds using a wound electronic medical record. J Am Coll Surg. 2009;209:254–260. doi: 10.1016/j.jamcollsurg.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 134.Brem H, Maggi J, Nierman D, et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200:473–477. doi: 10.1016/j.amjsurg.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Schiffman J, Golinko MS, Yan A, et al. Operative debridement of pressure ulcers. World J Surg. 2009;33:1396–1402. doi: 10.1007/s00268-009-0024-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Brem H, Tomic-Canic M, Tarnovskaya A, et al. Healing of elderly patients with diabetic foot ulcers, venous stasis ulcers, and pressure ulcers. Surg Technol Int. 2003;11:161–167. [PubMed] [Google Scholar]
- 137.Rennert R, Golinko M, Kaplan D, et al. Standardization of wound photography using the Wound Electronic Medical Record. Adv Skin Wound Care. 2009;22:32–38. doi: 10.1097/01.ASW.0000343718.30567.cb. [DOI] [PubMed] [Google Scholar]


