Abstract
Background
The association of alcohol use with in-hospital trauma deaths remains unclear. This study identifies the association of blood alcohol content with in-hospital death accounting for injury severity and mechanism.
Methods
Historical cohort of 46,222 admissions to a statewide trauma center between January 1, 2002 and October 31, 2011. Blood alcohol was evaluated as an ordinal variable: 1–100 mg/dL as moderate blood alcohol, 101–230 mg/dL as high blood alcohol, and >230 mg/dL as very high blood alcohol.
Results
Blood alcohol was recorded in 44,502 (96.3%) of patients. Moderate blood alcohol was associated with an increased odds for both penetrating mechanism (Odds Ratio 2.22; 95% CI 2.04–2.42) and severe injury (Odds Ratio 1.25; 95% CI 1.16–1.35). Very high blood alcohol had a decreased odds for penetrating mechanism (Odds Ratio 0.75; 95% CI 0.67–0.85) compared to the undetectable blood alcohol group. An inverse U-shaped association was shown for severe injury and penetrating mechanism by alcohol group (p<0.001). Moderate blood alcohol had an increased odds for in-hospital death (Odds Ratio 1.50; 95% CI 1.25–1.79), and the odds decreased for very high blood alcohol (Odds Ratio 0.69; 95% CI 0.54–0.87). An inverse U-shaped association was also shown for in-hospital death by alcohol group (p<0.001). Model discrimination for in-hospital death had an area under the curve receiver operating characteristic of 0.64 (95% CI 0.63–0.65).
Conclusions
Injury severity and mechanism are strong intermediate outcomes between alcohol and death. Severe injury itself carried the greatest odds for death, and with the moderate BAC group at greatest odds for severe injury and the very high BAC group at the lowest odds for severe injury. The result was a similar inverse-U shaped curve for odds for in-hospital death. Clear associations between blood alcohol and in-hospital death cannot be analyzed without consideration for the different injuries by blood alcohol groups.
Level of Evidence
Level III
Study Type
Epidemiological
Keywords: In-Hospital Death, Trauma Severity Indices, Ethanol, Alcohol Drinking
INTRODUCTION
Excessive alcohol consumption accounts for 1 in 10 deaths including unintentional injuries in working-age adults in the United States1. Excessive alcohol, as defined by the Center for Disease Control and National Institute on Alcohol Abuse and Alcoholism, identifies harmful patterns of alcohol consumption2. Two-thirds of trauma patients with elevated blood alcohol content (BAC) can be classified as excessive alcohol consumers3 and nearly 33% (range 26–62%) of trauma patients have an elevated BAC at time of trauma admission4–6. Epidemiologic studies have examined the association of an elevated BAC with in-hospital mortality; however, results are mixed showing both positive and negative associations 4, 7–9 which may be due to inadequate methods to parse out the association of alcohol from injury on outcomes10.
Traditionally, studies addressing the relationship of alcohol, injury, and death have adjusted for injury4, 7, 11, 12, thus introducing bias. In a study using data from the Illinois state registry, adjusted results showed a decreased odds for death after alcohol exposure in a dose-dependent manner7. Another retrospective study identified a decreased odds for death in trauma patients compared to their sober counterparts after adjusting for injury severity and mechanism of injury9. However alcohol ingestion precedes injury, and thus injury is in the causal pathway of death. Because alcohol ingestion could both predispose individuals to injury and influence the type of injury, adjustment for it is likely to introduce an overadjustment bias13, 14. Additionally, many studies examining alcohol’s association with mortality have suffered high proportions of missing alcohol information including some as high as 70% from state-level trauma databanks, and they did not address the case mix of injuries that can occur at different blood alcohol levels7, 15, 16. Consequently, studies assessing the association of alcohol exposure with injury have found contradictory results7, 12, 17.
Using a unique cohort of patients from a statewide referral trauma center with routine, universal BAC testing, this study evaluated the relationship of BAC categories with in-hospital death. Medical examiner data was incorporated for missing alcohol information from the trauma center. Injury was assessed as an intermediate outcome and in relationship to in-hospital death. The hypothesis was ordinal BAC categories characterized patients’ injuries differently and had different odds for in-hospital death.
METHODS
Environment
A historical cohort of patients admitted from the injury scene to the R. Adams Cowley Shock Trauma Center (STC) at the University of Maryland Medical Center between January 1, 2002 and October 31, 2011. All trauma admissions arrived via ambulance or medevac directly to STC, which is separate from the Emergency Department. Blood alcohol content was routinely measured with initial admission laboratory studies on all patients. Re-admissions and transfers to STC were excluded.
Definition of exposure and outcomes for analysis
Consistent with prior studies, BAC 1–100 mg/dL was defined as moderate BAC, 101–230 mg/dL as high BAC, and >230 mg/dL as very high BAC15, 18, 19. Serious injury was defined by an injury severity score (ISS) ≥1620. Mechanism of injury was dichotomized to penetrating versus non-penetrating in logistic regression21. Hypotension was defined as a mean arterial pressure ≤65 mmHg22. Shock index (systolic blood pressure/heart rate) was dichotomized to ≥1 or <1. In-hospital death is a dichotomous outcome.
Missing Data
Among patients who died after arrival to the trauma center, BAC was available in the trauma registry for 1422/2062 (68.8%). The large majority of missing BAC (460/640) occurred in patients who did not have any laboratory data collected because they were pronounced dead soon after arrival and became medical examiner cases. The proportion of missing alcohol laboratory data was reduced by retrieving postmortem alcohol testing on these patients from the State of Maryland Office of the Medical Examiner in 74% (474/640) of deaths in which BAC values were missing. After retrieving postmortem alcohol levels from the medical examiner, the proportion of alcohol testing in dead patients improved to 92.0% (1896/2062). Because of the low proportion of missing information, cases without admission BAC and demographics were excluded in the analysis of in-hospital death, and cases without injury severity scores were excluded in the analysis of injury.
The characteristics of the analysis cohort were very similar to the full STC cohort (Supplemental Table 1 and Supplemental Table 2). Of the 1720 (3.7%) patients with missing BAC values, 1330 (77.3%) were discharged home, 213 (12.4%) were discharged to acute and chronic care facilities, 11 (0.01%) left against medical advice or into custody, and 166 (9.6%) died. Of the 1255 (2.8%) patients with missing ISS, 1128 (89.9%) were discharged home, 121 (9.6%) were discharged to acute and chronic care facilities, and 6 (0.5%) died.
Analytic Approach
Patients 16–21 years old were included in the analysis as 2097/8933 (23.5%) had BAC >0 mg/dL. The primary outcome was in-hospital death. Alcohol exposure was evaluated in our primary analysis in four ordered BAC categories. Severe injury and mechanism of injury (penetrating versus blunt) were outcomes of alcohol that were assessed dichotomously20.
Baseline characteristics were presented as medians with interquartile ranges. Unadjusted comparisons of two or more proportions were performed using a chi-square test or Fisher’s exact test and continuous variables were performed using the Kruskal-Wallis one-way analysis of variance. Both unadjusted and adjusted analyses were performed with logistic regression model. Covariates included in the model for adjustment were age and sex. These were previously shown to be associated with in-hospital trauma death11, 23, 24. Likelihood ratio test was used for comparison of nested models and any covariates that did not cause a significant change in the overall model were removed (p>0.05). Model performance was measured with area under the curve receiver operating characteristics (AUROC). The simple random sampling method in SAS was used to produce a sample size of 5,000 to test model fit with the Hosmer-Lemeshow Goodness-of-Fit test. To test for significant trend between moderate, high and very high BAC groups, linear and quadratic contrasts in the coefficients corresponding to the variables representing the BAC groups were used. Analysis was performed using SAS Version 9.4 (SAS Institute, Cary, NC). A p-value ≤0.05 was set for statistical significance. The institutional review board of the University of Maryland Baltimore approved this study with waiver of consent and Health Insurance Portability and Accountability Act authorization.
RESULTS
BAC values were identified in 44,502/46,222 (96.3%) of the full STC cohort. Nearly all patients with BAC values arrived by medevac or ambulance 43,746 (98.3%) with an estimated time from injury to trauma center presentation of 54.6 (±41.4) minutes. Demographics, intermediate outcomes, and outcomes for ordered categories of BAC are shown in Table 1. The proportion of in-hospital deaths was 4.2% (1886).
Table 1.
Demographics and Outcomes
| Total (44492) | Undetectable 0 (31957) | Moderate 1–100 mg/dL (3549) | High 101–230 mg/dL (5504) | Very High >230 mg/dL (3482) | P-value | |
|---|---|---|---|---|---|---|
| DEMOGRAPHICS | ||||||
| Age (Years) | 35 (23–49) | 36 (23–52) | 31 (22–45) | 31 (23–44) | 37 (26–48) | <0.001 |
| Sex (Male) | 31120 (70.0) | 21082 (66.0) | 2752 (77.5) | 4394 (79.8) | 2892 (83.1) | <0.001 |
|
| ||||||
| INTERMEDIATE OUTCOME | ||||||
| Injury Mechanism | ||||||
| Blunt | 37385 (84.0) | 27325 (85.5) | 2567 (72.3) | 4433 (80.5) | 3060 (87.9) | |
| Penetrating | 6099 (13.7) | 3803 (11.9) | 926 (26.1) | 998 (18.1) | 372 (10.7) | |
| Crush | 273 (0.6) | 241 (0.8) | 7 (0.2) | 18 (0.3) | 7 (0.2) | |
| Hanging | 67 (0.2) | 52 (0.2) | 6 (0.2) | 9 (0.2) | 0 (0.0) | |
| Ingestion | 16 (0.0) | 9 (0.0) | 2 (0.1) | 4 (0.1) | 1 (0.0) | <0.001 |
| Burn | 43 (0.1) | 33 (0.1) | 1 (0.0) | 4 (0.1) | 5 (0.1) | |
| Near Drowning | 20 (0.0) | 10 (0.0) | 3 (0.1) | 3 (0.1) | 4 (0.1) | |
| Inhalation | 500 (1.1) | 414 (1.3) | 31 (0.9) | 28 (0.5) | 27 (0.8) | |
| Other | 89 (0.2) | 70 (0.2) | 6 (0.2) | 7 (0.1) | 6 (0.2) | |
|
| ||||||
| MAP <65 | 1668 (3.7) | 1064 (3.3) | 225 (6.3) | 254 (4.6) | 1064 (3.3) | <0.001 |
| Pulseless (ACLS) (N=44486) | 654 (1.5) | 443 (1.4) | 108 (3.0) | 85 (1.5) | 18 (0.5) | <0.001 |
| Unsurvivable injury* | 297 (0.7) | 203 (0.6) | 45 (1.3) | 35 (0.6) | 14 (0.4) | <0.001 |
| Shock Index ≥ 1 | 2030 (4.6) | 1214 (3.8) | 379 (6.3) | 379 (6.9) | 226 (6.5) | <0.001 |
| Severe Injury (N=43237) | 10790 (24.3) | 7456 (24.1) | 975 (28.1) | 1517 (28.0) | 842 (24.5) | <0.001 |
| GCS≤8 (Comatose) | 3127 (7.0) | 1854 (5.8) | 341 (9.6) | 539 (9.8) | 393 (11.3) | <0.001 |
| Traumatic Brain Injury† | 3706 (8.6) | 2543 (8.2) | 308 (8.9) | 512 (9.4) | 343 (10.0) | <0.001 |
| Length of Stay (Days) | 0.6 (0.2–3.2) | 0.5 (0.2–3.2) | 0.6 (0.2–3.8) | 0.7 (0.3–3.6) | 0.6 (0.4–2.6) | <0.001 |
|
| ||||||
| OUTCOME | ||||||
| Home | 35313 (79.4) | 25077 (78.5) | 2786 (78.5) | 4509 (81.9) | 2941 (84.5) | |
| Acute Care | 7039 (15.8) | 5301 (16.6) | 538 (15.2) | 777 (14.1) | 423 (12.2) | |
| Chronic Care‡ | 110 (0.2) | 104 (0.3) | 4 (0.1) | 2 (0.0) | 0 (0.0) | <0.001 |
| Other | 144 (0.3) | 110 (0.3) | 9 (0.3) | 14 (0.3) | 11 (0.3) | |
| In-hospital death | 1886 (4.2) | 1365 (4.3) | 212 (6.0) | 202 (3.7) | 107 (3.1) | |
GCS = Glasgow Coma Score; ISS = Injury Severity Score; MAP = mean arterial blood pressure
Unsurvivable injury = abbreviated injury score of 6 (unsurvivable) for any anatomic region
Traumatic Brain Injury = abbreviated injury score ≥ 4 for brain
Continuous values are presented as medians with interquartile ranges, and categorical values are presented as numbers with percentages.
Chronic Care: Skilled Nursing Facility/Long Term Acute Care
Alcohol Exposure
Among the 12,535 (28.2%) patients with alcohol exposure, median BAC was 167 mg/dL (IQR: 89.0–238.8 mg/dL). The characteristics associated with the moderate BAC group included younger age and male gender. The very high BAC group was associated with older patients. In addition, the very high BAC group had the strongest association with a reported alcohol use disorder when compared to negative BAC group in unadjusted analysis (Odds Ratio (OR) 24.8; 95% Confidence Interval (CI) 22.4–27.6, p< 0.001) and adjusted analysis (OR 24.6; 95% CI 22.1–27.3, p< 0.001) (Supplemental Table 3).
Alcohol and Injury
The mechanism of injury varied considerably by BAC group. The moderate BAC group had the greatest proportion of penetrating injury (p<0.001), with assault by gunshot most frequently encountered cause within this BAC group (N= 456, 49.2% of cases). The proportions of severe injury, penetrating mechanism, hypotension (MAP ≤65), and pulselessness on arrival were greatest in this moderate BAC group compared to the other groups (p<0.001). The very high BAC group had the greatest proportion of blunt injuries (87.9%, 3060), and the lowest proportion of motor vehicle accidents (51.9%, 1588). The proportion of assault/fights (17.7%, 541) and falls (26.7%, 816) was largest among the very high BAC group.
In unadjusted analysis, moderate BAC was associated with an increased odds for penetrating mechanism (OR 2.59; 95% CI 2.39–2.81; p<0.001) and severe injury (OR 1.23; 95% CI 1.14–1.33, p<0.001). In contradistinction, the odds ratio was decreased for penetrating mechanism (OR 0.86; 95% CI 0.77–0.97, p=0.01) and had no association for severe injury (OR 1.02; 95% CI 0.94–1.11, p=0.65) in the very high BAC group. Test for quadratic trend (inverse U-shaped curve) was significant in unadjusted analysis for severe injury and penetrating injury (p<0.001). In adjusted analysis, the odds of the BAC groups for penetrating mechanism or severe injury continued to have an inverse U-shaped curve (Figures 1 and 2). AUROC for the outcome penetrating injury was 0.79 (95% CI 0.79–0.80), and the Hosmer-Lemeshow test showed the model fit the data well (p=0.34).
Figure 1.
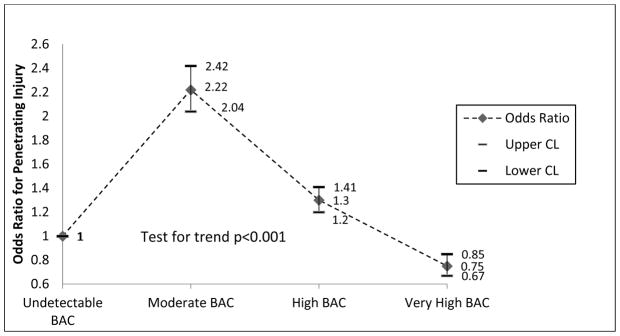
Odds Ratios for Penetrating Injury by BAC Group
Points represent adjusted odds for each alcohol group with 95% confidence interval error bars.
Adjusted for age and sex. Reference group is undetectable BAC (OR=1.0). P-value for quadratic test for trend.
Figure 2.
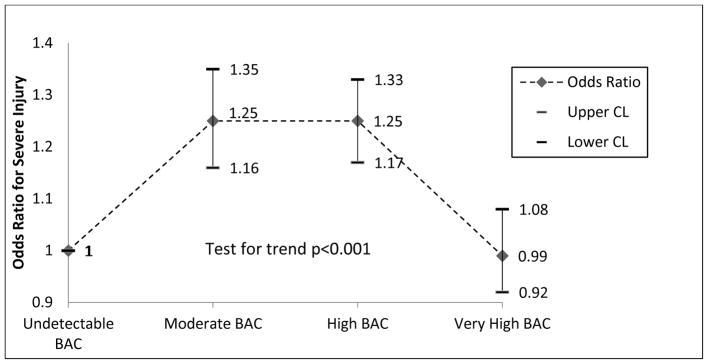
Odds Ratios for Severe Injury by BAC Group
Points represent adjusted odds for each alcohol group with 95% confidence interval error bars.
Adjusted for age and sex. Reference group is undetectable BAC (OR=1.0). P-value for quadratic test for trend.
Alcohol and In-hospital Death
The proportion of deaths was greatest in the moderate BAC group and lowest in the very high BAC group (4.03% versus 1.15%, p<0.001). In unadjusted analysis, the moderate BAC group had an increased odds for in-hospital death compared to negative BAC group (OR 1.42; 95% CI 1.23–1.65, p<0.001), and the odds was decreased for the very high BAC group (OR 0.71; 95% CI 0.58–0.87, p<0.001). The increased odds for in-hospital death remained in the moderate BAC group and the odds remained decreased for the very high BAC group in adjusted analysis (Figure 3). Test for quadratic trend (inverse U-shaped curve) was significant in unadjusted and adjusted analysis for in-hospital death (p<0.001). Similar to the odds for penetrating mechanism and severe injury, an inverse U-shaped odds for in-hospital death occurred across all BAC groups in both unadjusted and adjusted analysis (Figure 3). Severe injury had the highest odds for in-hospital death (OR 49.3; 95% CI 40.5–60.0, p<0.001) in adjusted analysis with baseline characteristics and injury mechanism included in the model. Test for interaction showed neither injury mechanism nor injury severity interacted with the alcohol groups in the analysis for inhospital death. AUROC for the outcome in-hospital death was 0.64 (95% CI 0.63–0.65), and the Hosmer-Lemeshow test showed the model fit the data well (p=0.86).
Figure 3.
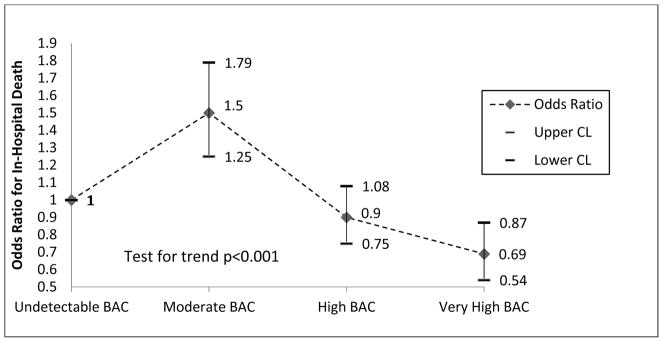
Odds Ratios for In-Hospital Death by BAC Group
Points represent adjusted risk for each alcohol group with 95% confidence interval error bars.
Adjusted for age and sex. Reference group is undetectable BAC (OR=1.0). P-value for quadratic test for trend.
DISCUSSION
Injury mechanism and severity differed considerably by BAC groups. Alcohol exposure by BAC groups was associated with both injury and in-hospital death in an inverse U-shaped distribution. Previous studies have inappropriately reported protective effects from alcohol and adjusted for injury whereas the results from this study examined injury mechanism and severity separately as intermediate outcomes from alcohol exposure7–9, 25. In a previous study, gunshot wounds had a three-fold higher proportion of deaths than stab wounds in a large trauma cohort26. Similarly, the moderate BAC group in this study had the highest odds for in-hospital death with a greater proportion of penetrating injuries, mainly gunshot wounds, than any other group. Severe injury itself carried the greatest odds for death, and with the moderate BAC group at greatest odds for severe injury and the very high BAC group at the lowest odds for severe injury, ISS likely was a contributing factor in the similar results for in-hospital death by BAC group. Although it may appear that the very high alcohol BAC patients are at lower odds for in-hospital death when compared to their undetectable BAC counterparts, it is important to consider their odds for life threatening injury is lower and a major determinant of death.
ISS is a commonly used metric of trauma severity and incorporated into analyses investigating mortality20. However, it may not fully account for the amount of tissue damage. Studies have shown including mechanism of injury (blunt and penetrating) improved the analyses for mortality27. ISS and injury mechanism were analyzed separate from BAC in association with inhospital death because ISS and injury mechanism occurred after alcohol exposure as intermediate outcomes. The similar inverse U-shaped curves from alcohol exposure on injury severity, injury mechanism, and in-hospital death made it difficult to parse the effect of alcohol from injury on in-hospital death. Previous studies that adjusted for ISS have shown a protective or negligible effect from BAC4, 7, 9, 17. These epidemiologic studies adjusted for injury severity in their analyses of outcomes from acute alcohol exposure and may have obscured the association of death with BAC7, 12, 17 by overadjustment13. Experimental studies with investigator control of injury severity are needed to better define the roles of alcohol, injury, and death.
BAC is an important biomarker for acute alcohol exposure but it does not characterize drinkers who arrive with undetectable levels but have an alcohol use disorder or recently binge drank. BAC characterizes alcohol use disorder better than other biomarkers like carbohydrate-deficient transferrin (CDT)28, and our results showed categorizing BAC into four groups revealed more information about possible drinking patterns than dichotomous BAC7. Levels >230 mg/dL have been used to represent alcohol use disorder in other studies29. Over a quarter of our alcohol-positive patients arrived in the very high BAC group (>230 mg/dL), and they had a strong association with a documented alcohol use disorder. This cohort should be studied separately from other alcohol exposures because they had different demographics, injury characteristics, and were more likely to arrive with a survivable injury. This may explain other studies that showed this cohort at greater odds for readmissions than undetectable BAC patients and intoxicated patients without an alcohol use disorder 30. The differences between BAC groups in our cohort demonstrate the importance of better characterizing drinking behaviors and their associated traumas for future studies.
The volume and characteristics of the center’s patients are comparable to patients treated in multiple trauma centers throughout the United States21. As with all hospital-based studies, these results could be biased for all trauma deaths as these data did not include pre-hospital deaths which may comprise a substantial proportion of all trauma deaths4. Although there was less than 5% missing BAC, those without BAC information had a higher case-rate for death which biased our results towards no effect from alcohol exposure as most these patients died early and never had their blood drawn. In addition, while the admission BAC is not representative of the BAC at time of injury, most of our patients arrived less than an hour after their injury, and thus our BAC measurement on admission closely approximates the BAC at time of injury. Furthermore, nearly a quarter of dead patients had BAC assessment from the medical examiner’s office which may have introduced variability in the final BAC. Another limitation is the incompleteness of urine toxicology data and the results did not account for co-substance use. Furthermore, model discrimination for the outcome in-hospital death was poor. Future studies applying other methods such as mediation or pathway analysis may better discriminate the relationship between alcohol exposure, injury, and death. Our cohort’s large sample, near-complete BAC capture, and detailed injury descriptions help to better understand the relationship between acute alcohol exposure, injury, and death.
Different BAC groups are associated with very different types of injury, revealing an inverse U-shaped association with injury and in-hospital death. Moderate BAC is associated with an increased odds for penetrating mechanism, severe injury, and in-hospital death, while very high BAC is associated with non-penetrating mechanism and non-severe injury. Clear associations between BAC groups and death cannot be analyzed without consideration for the different injuries by BAC group.
Supplementary Material
Acknowledgments
This research was supported in part by National Institute of Health grants 1RO1AA018313-01A1 (Gordon Smith) and K12RR023250 (Giora Netzer) and F32AA022553-01 (Majid Afshar). Majid Afshar and Gordon Smith had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Administrative, technical, or material support: Betsy Kramer, Project Manager for Clinical Information Systems contributed to the manuscript by providing the dataset from the Shock Trauma Registry.
Footnotes
Conflicts of Interest: No conflicts of interest to disclose amongst the authors.
This work was presented as an abstract at the Research Society on Alcoholism Conference 2014
AUTHOR CONRIBUTION
Study concept and design: Giora Netzer, Sarah Murthi, Gordon Smith, and Majid Afshar
Acquisition of Data: Giora Netzer, Gordon Smith, Majid Afshar
Analysis and Interpretation of Data: Majid Afshar, Gordon Smith, Sarah Murthi, and Giora Netzer
Drafting of the manuscript: Majid Afshar, Gordon Smith, Sarah Murthi, and Giora Netzer
Administrative, technical, or material support: Betsy Kramer, Project Manager for Clinical Information Systems contributed to the manuscript by providing the dataset from the Shock Trauma Registry.
Contributor Information
Giora Netzer, Email: gnetzer@medicine.umaryland.edu.
Sarah Murthi, Email: smurthi@umm.edu.
Gordon S. Smith, Email: gssmith@som.umaryland.edu.
References
- 1.Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the united states. Prev Chronic Dis. 2014;11:E109. doi: 10.5888/pcd11.130293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the u.S., 2006. Am J Prev Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Savola O, Niemela O, Hillbom M. Blood alcohol is the best indicator of hazardous alcohol drinking in young adults and working-age patients with trauma. Alcohol and Alcoholism. 2004;39(4):340–345. doi: 10.1093/alcalc/agh064. [DOI] [PubMed] [Google Scholar]
- 4.Jurkovich GJ, Rivara FP, Gurney JG, Fligner C, Ries R, Mueller BA, Copass M. The effect of acute alcohol intoxication and chronic alcohol abuse on outcome from trauma. JAMA. 1993;270(1):51–56. [PubMed] [Google Scholar]
- 5.Waller PF, Stewart JR, Hansen AR, Stutts JC, Popkin CL, Rodgman EA. The potentiating effects of alcohol on driver injury. JAMA. 1986;256:1461–1466. [PubMed] [Google Scholar]
- 6.MacLeod JB, Hungerford DW. Alcohol-related injury visits: Do we know the true prevalence in u.S. Trauma centres? Injury. 2011;42:922–926. doi: 10.1016/j.injury.2010.01.098. [DOI] [PubMed] [Google Scholar]
- 7.Friedman LS. Dose–response relationship between in-hospital mortality and alcohol following acute injury. Alcohol. 2012;46:769–775. doi: 10.1016/j.alcohol.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Blondell RD, Looney SW, Krieg CL, Spain DA. A comparison of alcohol-positive and alcohol-negative trauma patients. Journal of Study of Alcohol. 2002;63(3):380–383. doi: 10.15288/jsa.2002.63.380. [DOI] [PubMed] [Google Scholar]
- 9.Yaghoubian A, Kaji A, Putnam B, De Virgilio N, De Virgilio C. Elevated blood alcohol level may be protective of trauma patient mortality. Am Surg. 2009;75:950–953. [PubMed] [Google Scholar]
- 10.Afshar M, Smith GS, Terrin ML, et al. Blood alcohol content, injury severity, and adult respiratory distress syndrome. The Journal of Trauma and Acute Care Surgery. 2014;76(6):1447–1455. doi: 10.1097/TA.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kowalenko T, Burgess B, Szpunar SM, Irvin-Babcock CB. Alcohol and trauma—in every age group. The American Journal of Emergency Medicine. 2013;31(4):705–709. doi: 10.1016/j.ajem.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 12.Fabbri A, Marchesini G, Morselli-Labate AM, et al. Blood alcohol concentration and management of road trauma patients in the emergency department. The Journal of Trauma Injury, Infection, and Critical Care. 2001;50(3):521–528. doi: 10.1097/00005373-200103000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miettinen OS. Matching and design efficiency in retrospective studies. American Journal of Epidemiology. 1970;91(2):111–118. doi: 10.1093/oxfordjournals.aje.a121118. [DOI] [PubMed] [Google Scholar]
- 15.Shandro JR, Rivara FP, Wang J, Jurkovich GJ, Nathens AB, MacKenzie EJ. Alcohol and risk of mortality in patients with traumatic brain injury. The Journal of Trauma: Injury, Infection, and Critical Care. 2009;66(6):1584–1590. doi: 10.1097/TA.0b013e318182af96. [DOI] [PubMed] [Google Scholar]
- 16.Bilello J, McCray V, Davis J, Jackson L, Danos LA. Acute ethanol intoxication and the trauma patient: Hemodynamic pitfalls. World Journal of Surgery. 2011;35(9):2149–2153. doi: 10.1007/s00268-011-1191-7. [DOI] [PubMed] [Google Scholar]
- 17.Madan AK, Yu K, Beech DJ. Alcohol and drug use in victims of life-threatening trauma. The Journal of Trauma Injury, Infection, and Critical Care. 1999;47(3):568–571. doi: 10.1097/00005373-199909000-00026. [DOI] [PubMed] [Google Scholar]
- 18.Rootman DB, Mustard R, Kalia V, Ahmed N. Increased incidence of complications in trauma patients cointoxicated with alcohol and other drugs. The Journal of Trauma: Injury, Infection, and Critical Care. 2007;62(3):755–758. doi: 10.1097/TA.0b013e318031aa7f. [DOI] [PubMed] [Google Scholar]
- 19.Tien HC, Tremblay LN, Rizoli SB, et al. Association between alcohol and mortality in patients with severe traumatic head injury. Archives of Surgery. 2006;141(12):1185–1191. doi: 10.1001/archsurg.141.12.1185. [DOI] [PubMed] [Google Scholar]
- 20.Baker SP, O’Neill B, Haddon W, Long WB. The inury severity score: A method for describing patients with multiple injuries and evaluating emergency care. The Journal of Trauma Injury, Infection, and Critical Care. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 21.Champion HR, Copes WS, Sacco WJ, et al. The major trauma outcome study: Establishing national norms for trauma care. The Journal of Trauma Injury, Infection, and Critical Care. 1990;30(11):1356–1365. [PubMed] [Google Scholar]
- 22.Yeguiayan JM, Garrigue D, Binquet C, et al. Medical pre-hospital management reduces mortality in severe blunt trauma: A prospective epidemiological study. Critical Care. 2011;15(1):R34. doi: 10.1186/cc9982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryb GE, Cooper C. Race/ethnicity and acute respiratory distress syndrome: A national trauma data bank study. Journal of the National Medical Association. 2010;102:865–869. doi: 10.1016/s0027-9684(15)30700-8. [DOI] [PubMed] [Google Scholar]
- 24.Shih HC, Hu SC, Yang CC, Ko TJ, Wu JK, Lee CH. Alcohol intoxication increases morbidity in drivers involved in motor vehicle accidents. Am J Emerg Med. 2003;21(2):91–94. doi: 10.1053/ajem.2003.50025. [DOI] [PubMed] [Google Scholar]
- 25.Salim A, Ley EJ, Cryer HG, Margulies DR, Ramicone E, Tillou A. Positive serum ethanol level and mortality in moderate to severe traumatic brain injury. Archives of Surgery. 2009;144:865–871. doi: 10.1001/archsurg.2009.158. [DOI] [PubMed] [Google Scholar]
- 26.Band RA, Salhi RA, Holena DN, Powell E, Branas CC, Carr BG. Severity-adjusted mortality in trauma patients transported by police. Annals of Emergency Medicine. 2014;63(5):608–614. doi: 10.1016/j.annemergmed.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haider AH, Chang DC, Haut ER, Cornwell EE, 3rd, Efron DT. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153:138–142. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Fleming M, Bhamb B, Schurr M, Mundt M, Williams A. Alcohol biomarkers in patients admitted for trauma. Alcohol Clin Exp Res. 2009;33(10):1777–1781. doi: 10.1111/j.1530-0277.2009.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adachi J, Mizoi Y, Fukunaga T, Ogawa Y, Ueno Y, Imamichi H. Degrees of alcohol intoxication in 117 hospitalized cases. J Stud Alcohol. 1991;52(5):448–453. doi: 10.15288/jsa.1991.52.448. [DOI] [PubMed] [Google Scholar]
- 30.Rivara FP, Koepsell TD, Jurkovich GJ, Gurney JG, Soderberg R. The effects of alcohol abuse on readmission for trauma. JAMA. 1993;270(16):1962–1964. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


