Abstract
Objective
The study objective was to assess the prognostic value of the rapid shallow breathing index (RSBI) in predicting successful weaning of patients from prolonged mechanical ventilation (PMV) in long-term acute care (LTAC) facilities. The RSBI predicts successful ventilator weaning in acutely ill patients. However, its value in PMV is unclear.
Methods
A retrospective cohort study of patients receiving PMV in LTAC facilities was performed. RSBI was measured daily, with weaning per protocol. Initial, mean, and final RSBI; RSBI ≤ 105; rate of change; and variability were assessed.
Results
Twenty-five of 52 patients were weaned from PMV. Only the mean RSBI and the RSBI on the last day of weaning predicted success (78.7 ± 14.2 vs 99.3 ± 30.2, P = .007; 71.7 ± 31.2 vs 123.3 ± 92.5, P = .005, respectively). RSBI variability and rate of change were different between groups (coefficient of variation, .37 ± .12 vs .51 ± .30, P = .02, rate of change: −3.40 ± 9.40 vs 4.40 ± 11.1 RSBI points/day, P = .005, weaned vs failed).
Conclusion
Although isolated RSBI measurements do not predict successful weaning from PMV, RSBI trends may have prognostic value.
Keywords: Mechanical ventilation, Prolonged mechanical ventilation, Rapid shallow breathing index, Respiratory failure, Spontaneous breathing trial, Weaning
Patients receiving prolonged mechanical ventilation (PMV) have been recognized as a distinct population with “chronic critical illness,”1,2 in contrast to acutely ill patients in intensive care units (ICUs). These patients are usually survivors of catastrophic illness, are severely physically debilitated, and often have chronic metabolic, neuroendocrine, neuropsychiatric, and immunologic conditions.3 Improved intensive care has led to an increasing number of patients surviving catastrophic illness and receiving PMV. Thus, patients who recover from critical illness but require ongoing complex medical needs preventing their discharge (eg, intravenous antibiotics, wound management, PMV) receive care at long-term acute care (LTAC) hospitals. These facilities were initially created in the 1990s as a means to offload ICUs, providing a venue where weaning from mechanical ventilation and continued care could be provided.4
Studies focused on Medicare data have demonstrated increasing LTAC hospital expenditures, totaling approximately $1.325 billion in 2006.5 A recent multicenter, observational study of more than 1400 patients on PMV noted that on discharge from LTAC hospitals, 54% of patients were no longer on ventilators, 21% remained ventilator dependent, and 25% died.6 Thus, the growing patient population with “chronic critical illness” demonstrates the need for greater attention, both from a financial standpoint7 and a personnel and resource use perspective.8,9
The inability to wean from mechanical ventilation is one of the greatest obstacles for patients in LTAC hospitals to overcome before discharge. Because approximately half of these patients die or are lifelong ventilator dependent, many efforts have been directed toward determining accurate predictors of successful weaning in different populations on PMV,10–12 including scoring systems, physiologic measurements, and protocol-driven screening assessments. For patients with acute respiratory failure, the rapid shallow breathing index (RSBI) measured during spontaneous breathing trials (SBTs) was demonstrated to be a successful predictor of weaning from the ventilator within 24 hours.13 The RSBI is easy to measure and inexpensive, and an RSBI of ≤ 105 has high sensitivity (.97), specificity (.64), and positive and negative predictive values (.78 and .95, respectively).14 However, few studies have assessed the efficacy of the RSBI in predicting successful weaning from mechanical ventilation in the patient on PMV.12,15
The current study assessed the prognostic value of the RSBI with respect to predicting successful weaning from the ventilator in patients on PMV in LTAC hospitals. We tested the hypothesis that lower RSBI measurements were associated with successful weaning from mechanical ventilation in this population. We further postulated that comorbid conditions, as well as variability, and RSBI trends over the weaning period are associated with success in weaning from PMV.
Materials and Methods
This retrospective, observational cohort study assessed the respiratory records of patients requiring PMV who were admitted to the Pulmonary Rehabilitation and Ventilator Weaning Unit at the University Specialty Hospital (USH). This study was approved by the University of Maryland Institutional Review Board with a waiver of consent. The USH is a 180-bed LTAC hospital operated by the University of Maryland Medical System. The Ventilator Unit has 60 beds, a patient–nurse ratio of 6.5:1, a respiratory therapist–patient ratio of 9:1, 24-hour hospitalist coverage, hemodialysis unit, and a multidisciplinary support team consisting of physical, occupational, recreational, and speech therapists; clinical pharmacist services; social worker; psychiatric liaisons; and nutritionists. Criteria for transfer from acute care hospitals to the ventilator unit include hemodynamic stability, tracheostomy, inspired oxygen fraction ≤ 60% with oxygen saturation ≥ 90%, positive end-expiratory pressure (PEEP) ≤ 10 cm H2O, and no need for cardiac monitoring, intravenous vasoactive medications, or continuous intravenous drips. The potential ability to wean from mechanical ventilation is not a requirement for admission into the unit. Patients were classified according to primary cause of respiratory failure. All patients on mechanical ventilation were followed in consultation by board-certified pulmonologists from the Division of Pulmonary and Critical Care Medicine from the University of Maryland School of Medicine.
All study patients had undergone tracheostomy and were ventilator dependent for ≥ 21 days before admission to USH, consistent with the National Association for Medical Direction of Respiratory Care criteria for PMV.16 Patients admitted between June 2007 and January 2008 were included in the analysis. The age-adjusted Charlson Comorbidity Index (CCI) with Deyo modification was calculated for each patient as an assessment of comorbidity burden.17 Patients who were weaned from mechanical ventilation, were transferred to an acute care facility, or died within ≤ 3 days of admission to the LTAC hospital were excluded from the review because these patients had insufficient data for analysis.
All patients were supported with the same mechanical ventilators (Vela, VIASYS Healthcare, Yorba Linda, CA). At baseline, patients were supported using 1 of 2 modes: volume assist–control or pressure support. SBTs were conducted daily by respiratory therapists per protocol on all patients who were deemed to be fit for weaning by the attending pulmonologist. The SBT was initiated by placing the patient on continuous positive airway pressure of 5 to 8 cm H2O (to match the assumed physiologic baseline PEEP) with a 1-minute acclimatization period. After this acclimatization period, RSBI measurements were calculated by respiratory therapists on all patients who received an SBT using the equation RSBI = respiratory rate (breaths/min) ÷ average tidal volume (liters).
For this calculation, the respiratory rate and average tidal volume were measured after the first 1 minute of the SBT and reported in the daily respiratory records. Although these calculations were available to the pulmonary physician on request, the RSBI did not drive the decision to continue or terminate weaning trials. Weaning modes included decremental pressure support, continuous positive airway pressure trials, and tracheostomy collar trials. If at any point during the SBT or during the daily weaning trials the patient experienced respiratory distress or signs of weaning intolerance, he or she was placed back on baseline ventilator support.
Demographic data from our quality assessment database included age, gender, primary cause of respiratory failure, comorbid illnesses, and race. Weaning outcomes data were recorded (weaned off mechanical ventilation vs returned to mechanical ventilation) in addition to RSBI values and number of RSBI recordings. We defined successful weaning according to the National Association for Medical Direction of Respiratory Care Consensus Conference Guidelines (Table 1).16 Accordingly, patients were considered weaned if they were independent from mechanical ventilation for >48 hours or they required only nocturnal mechanical ventilation ≤ 6 hours for ≥ 7 days. Patients were considered “not weaned” if they required continuous mechanical ventilation, were transferred from USH to an acute care facility, or died during a weaning trial. A weaning trial was defined as the period of time (days) that a patient was considered as actively weaning by respiratory staff.
Table 1.
Proposed criteria for successful weaning from prolonged mechanical ventilation according to the National Association for Medical Direction of Respiratory Care Guidelines for the Management of Patients Requiring Prolonged Mechanical Ventilation
| A. Time without ventilator support: |
B. Freedom from ventilator support at: |
|---|---|
| 1. 48 h | 1. Time of discharge |
| 2. 7 d (or only requiring ≤6 h of nocturnal supporta) | 2. 6 mo postdischarge |
| 3. 14 d | 3. 1 y postdischarge |
Recommended by the NAMDRC as criteria for weaning success. Our definition of weaning success incorporated A.1 and A.2.
Statistical Analysis
Demographic and clinical characteristics were compiled and reported as mean ± standard deviation for numeric data or percentage for categoric data. For each patient, appropriate variables were collected and compiled every day during daily morning ventilator assessments by respiratory staff, with the end point being weaned or not weaned. Daily RSBI scores were recorded as continuous variables and categorized as a dichotomous variable with a cutoff point of 105. A comparison of the proportion of patients with RSBI ≤ 105 by weaning success or failure was examined by study day, using logistic regression to estimate both odds ratios and errors of prediction. RSBI measurements at admission and end point were summarized by mean and proportions. By using episode of care as the unit of analysis, a linear mixed model was fitted to examine differences in RSBI scores by weaning outcome, day, and outcome*day interaction (α = .05), with equally spaced repeated measures. As a standardized measure of variation, the coefficient of variation (CV) was calculated using the RSBI measurements for each trial (standard deviation/mean). The CV was chosen because it reflects variation of each individual’s RSBI in the context of its own mean. Trials with less than 3 measurements were eliminated in accordance with the earlier stated reasoning. Statistical analysis was performed using GB Stat v 9.0 (Silver Spring, MD).
Results
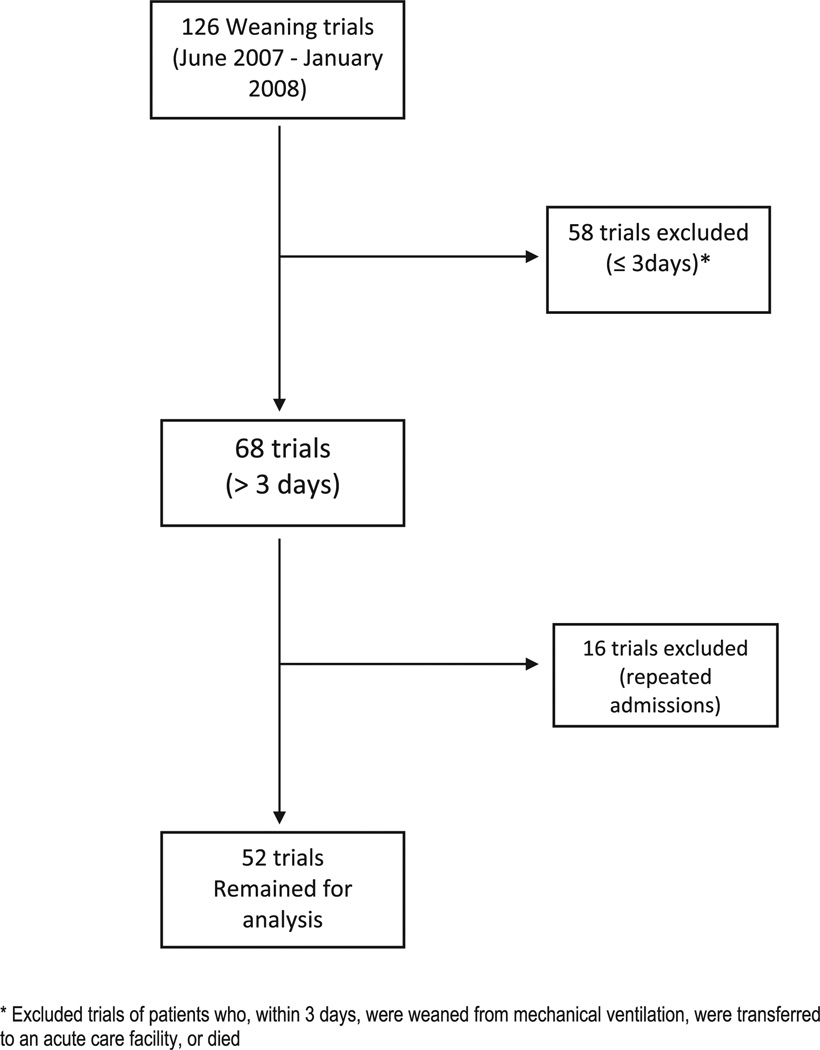
The records of 126 weaning trials of mechanically ventilated patients who were admitted to the ventilator weaning unit of USH between June 2007 and January 2008 were reviewed. Fifty-eight trials were excluded because they were for < 3 days. The patients ranged in age from 23 to 84 years with a mean of 57.9 ± 15.7 years (Table 2). Overall, 52 individuals were included in the analysis, including 23 men (44%) and 29 African-Americans (55.8%) (Figure 1). The primary causes for respiratory failure as determined by admitting diagnosis were neurologic/cerebrovascular events, trauma or surgery, and sepsis. Most patients had multiple comorbidities (34/52, 65.3% patients with > 1 comorbid illness). Of the remaining 68 weaning trials, 16 were excluded because they were repeated trials of patients who were weaning, transferred to acute care facilities, and then readmitted. Twenty five trials (48.1%) resulted in successful weaning from mechanical ventilation.
Table 2.
Demographic information on 52 patients requiring prolonged mechanical ventilation
| Characteristic | Total sample (%) N = 52 |
Not weaned (%) N = 27 |
Weaned (%) N = 25 |
P valuea |
|---|---|---|---|---|
| Age, y | 57.9 ± 15.7 | 61.7 ± 15.2 | 55.5 ± 15.7 | NS |
| Gender | NS | |||
| Male | 23 (44.2) | 14 (51.8) | 9 (36.0) | |
| Female | 29 (55.8) | 13 (48.1) | 16 (64.0) | |
| Race | NS | |||
| African-American | 29 (55.8) | 14 (51.8) | 15 (60.0) | |
| Caucasian | 22 (42.3) | 12 (44.4) | 10 (40.0) | |
| Asian | 1 (1.9) | 1 (3.7) | 0 | |
| Causes for respiratory failure | NS | |||
| Neurologic/cerebrovascular | 21 (40.4) | 13 (48.1) | 8 (32.0) | |
| Trauma/surgical | 15 (28.8) | 7 (25.9) | 8 (32.0) | |
| Sepsis | 9 (17.3) | 3 (11.1) | 6 (24.0) | |
| COPD | 6 (11.5) | 2 (7.4) | 4 (16.0) | |
| Cardiac | 3 (5.8) | 2 (7.4) | 1 (4.0) | |
| Neuromuscular/chest wall | 3 (5.8) | 1 (3.7) | 2 (8.0) | |
| ARDS | 1 (1.9) | 1 (3.7) | 0 | |
| Morbid obesity/hypoventilation/OSA | 1 (1.9) | 0 | 1 (4.0) |
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; NS, not significant; OSA, obstructive sleep apnea.
P values obtained using comparison of proportions or Student t test when appropriate.
Figure 1.
CONSORT diagram demonstrating patient flow.
There were no significant differences in demographic characteristics or number of patient comorbidities between weaning trials that ended in success or failure (Table 3). Reasons for weaning trial termination included transfer to acute care facility (81.4%), trial terminated by physician (7.4%), cardiopulmonary arrest (7.4%), or death (3.7%).
Table 3.
Charlson Comorbidity Index and comorbid conditions of patients receiving prolonged mechanical ventilation
| Comorbidities | Total (%) | Not weaned (%) | Weaned (%) | P value |
|---|---|---|---|---|
| CCI | 5.4 ± 2.8 | 5.9 ± 3.0 | 4.8 ± 2.4 | .15 |
| Renal failure/hemodialysis | 12 (23.1) | 7 (10.4) | 5 (10.4) | |
| Cirrhosis | 4 (7.7) | 3 (4.5) | 1 (2.1) | |
| HIV/infectious | 6 (11.5) | 2 (3.0) | 4 (8.3) | |
| Cardiac | 26 (50.0) | 16 (23.9) | 10 (20.8) | |
| Severe malnutrition | 24 (46.2) | 14 (20.9) | 10 (20.8) | NS |
| Morbid obesity | 15 (28.9) | 10 (14.9) | 5 (10.4) | |
| Cancer | 7 (13.5) | 5 (7.5) | 2 (4.2) | |
| Organ transplant | 1 (1.9) | 0 | 1 (2.1) | |
| COPD/asthma/obstructive lung disease | 20 (38.5) | 10 (14.9) | 10 (20.8) | |
| No. of comorbidities per patient | No. patients (%) | Not weaned (%) | Weaned (%) | P value |
| 0 | 2 (3.8) | 0 | 2 (8.0) | |
| 1 | 16 (30.8) | 7 (25.9) | 9 (36.0) | |
| 2 | 16 (30.8) | 8 (29.6) | 8 (32.0) | NS |
| 3 | 10 (19.2) | 7 (25.9) | 3 (12.0) | |
| 4 | 3 (5.8) | 2 (7.4) | 1 (4.0) | |
| 5 | 5 (9.6) | 3 (11.1) | 2 (8.0) | |
CCI, Charlson Comorbidity Index; COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus; NS, not significant.
The mean CCI of all patients was 5.4 ± 2.8. There was no difference in severity of illness as noted by CCI in those who weaned compared with those who failed (4.8 ± 2.4 vs 5.9 ± 3.0, respectively (confidence interval, −.42 to 2.6; P = .15; Table 3).
There were no significant differences between initial RSBI scores measured on admission for patients who eventually weaned and those who failed (114.5 ± 64.9; range, 40–276 vs 101.3 ± 60.0; range, 20–333; confidence interval, −48.0 to 21.6; P = .45). Likewise, an initial RSBI of ≤ 105 was not associated with successful weaning, because 60% of those who weaned successfully had an initial RSBI ≤ 105 compared with 66.7% of those who failed weaning (P = .83). However, over the course of observation, the overall mean RSBI was significantly lower in the group that weaned than in the group that failed (78.7 ± 14.2 vs 99.3 ± 30.3; P = .007). The last RSBI measured was found to be significantly different between groups (weaned vs failed to wean, 71.7 ± 31.2 vs 123.3 ± 92.5, P = .005).
Patients who successfully weaned from PMV had less variability in their RSBI scores than patients who failed weaning trials (CV in patients who weaned vs those who failed, .37 ± .12 vs .51 ± .30, P = .02, Table 4). Linear regression of time (day) and RSBI measurement demonstrated that the group that weaned had a consistent decrease in RSBI compared with the group that failed to wean (−3.40 ± 9.40 vs 4.40 ± 11.1 RSBI points/day, P = .005).
Table 4.
Rapid shallow breathing index characteristics between groups (not weaned vs weaned)
| All patients | Not weaned | Weaned | P value | |
|---|---|---|---|---|
| Initial RSBI (range) | 107.7 ± 62.2 | 101.3 ± 60.0 (14–650) | 114.5 ± 64.9 (4–310) | .45 |
| Mean RSBI | 90.1 ± 55.7 | 99.3 ± 30.2 | 78.7 ± 14.2 | .007 |
| Final RSBI | 123.3 ± 92.5 | 71.7 ± 31.2 | .005 | |
| Initial RSBI ≤ 105 | 23/52 (63.5%) | 18/27 (66.7%) | 15/2 (60%) | .83 |
| RSBI variabilitya | .44 ± .24 | .51 ± .30 | .37 ± .12 | .02 |
| Δ RSBI change/day | 4.40 ± 11.1 | −3.40 ± 9.4 | .005 |
RSBI, rapid shallow breathing index.
RSBI variability reported as CV.
Discussion
In 52 patients requiring PMV, we demonstrated that individual measurements of the RSBI were not able to predict immediate, successful weaning from mechanical ventilation. Likewise, initial RSBI measurements of ≤ 105 at the onset of the weaning period were not associated with weaning success. Although these findings were not consistent with our initial hypothesis, when analyzing the RSBI over the course of a weaning trial, we found that the CV, as well as the trend in RSBI measurements over time, had value in predicting weaning success when using ≤ 105 as a discriminator of weaning success versus failure.
The final RSBI measured was found to be significantly lower in those who weaned versus those who failed. This can be explained by the reason for weaning trial termination, because those who failed to wean likely had their trials terminated because of medical instability.
Scheinhorn and colleagues12 determined that an RSBI measurement of ≤ 80 best predicted patients’ tolerance of an expedited PMV weaning protocol, including a 1-hour SBT, with high sensitivity (89%). Chao and Scheinhorn15 later determined that a more lenient RSBI cutoff point of ≤ 97 had similarly high accuracy (87.1%) in predicting 1-hour SBT tolerance. Our study focused on the outcome of weaning success, rather than SBT tolerance. Although we did not determine an optimal cutoff point for SBT tolerance, we found that RSBI trends over time indicated gradual progress toward weaning success in a fashion similar to the way a single, daily RSBI measurement may predict all-or-none SBT tolerance on a given day in a more acute patient population. Thus, because weaning from PMV may be considered a gradual physical training process that entails repeated lengthening trials of spontaneous breathing, a decrease in RSBI over time can be considered an improvement in pulmonary function and progress toward ventilator independence.
In our population, we found that no specific comorbid condition was associated with prolonged time to successful weaning. This includes conditions that have been identified in prior studies to be associated with prolonged ventilator dependence, including preexisting obstructive pulmonary disease (chronic obstructive pulmonary disease or asthma), hemodialysis-dependent renal failure, cardiac disease (congestive heart failure and ischemic disease), and malnutrition.18–22 Our study’s modest sample size may have limited our ability to detect associations between primary diagnoses or comorbid factors with successful weaning and, possibly, the predictive performance of individual RSBI measurements.
The high percentage of patients with renal failure (23.1%) in our study may partially explain our lower overall weaning success rate (38.2%) when compared with other groups reporting weaning success rates up to 60% in similar patient populations.3,21–25 In general, renal failure is a robust negative predictor of weaning failure, with some sources reporting only a 7% to 10% weaning success rate.20,22,23 The fact that our LTAC facility is one of the few in the area that supports its own in-house dialysis unit may have increased the proportion of patients who failed to wean in our sample. The explanation of why hemodialysis is a negative predictor of weaning success is not known, but may be attributed to total body fluid accumulation and the adverse effects of this state on lung mechanics and gas exchange.
With respect to overall severity of illness, both groups had a similar comorbidity burden when comparing CCI. Thus, although it would make clinical sense that patients with more comorbid illnesses have worse outcomes, it remains unclear whether comorbidities have a role in predicting weaning success in patients on PMV. However, we urge caution in interpreting the CCI in the population on PMV, because the original purpose and design of the CCI was to determine the risk of 1-year mortality attributable to comorbidity in a general hospital population. Therefore, although the CCI has been widely used and validated in the acutely critically ill population, we know of no study that validates the CCI in the population on PMV.
Our study demonstrated that individual measurements of the RSBI are of little value in predicting successful weaning candidates in the population on PMV. However, despite the clinical bedside limitations of “snapshot” indices, we noted the predictive value when analyzing serial RSBI measurements. RSBI variability was found to be low in general, because the CV was < 1 across all weaning trials of all patients. We found that RSBI variability, as reflected by CV, was significantly lower in the group that successfully weaned. In addition, we noted an inverse relationship between the rate of change of serial RSBI measurements and weaning success, as reflected by a gradual decrease in daily RSBI measurements in those who weaned compared with an increase in those who failed. These findings imply that when trending these measurements over time, a decrease in variation and a negative trend in overall RSBI measurement may indicate increased likelihood of successful weaning in this population.
The properties of the RSBI that make it a practical index to gauge weaning progress are its ease in calculating and accuracy in predicting weaning success. Despite this, some variability has been noted with its validity in the acutely ill population demonstrating variation of the RSBI predictive ability depending on patient characteristics, such as gender or endotracheal tube size.26 Some have chosen to test the RSBI as an adjunct to other measurements, such as compliance, in predicting successful weaning from PMV in an effort to improve its predictive value.27 This variation in measuring and interpreting the RSBI has emerged when using the RSBI as a predictive index in patients in ICUs, a population with fluctuating and frail health status. The population on PMV, although considered “chronically critically ill”2,6 by some, represents a more homogenous group more stable with respect to health status. Thus, measurements of pulmonary parameters in such a group may be more reflective of gradual progress toward successful weaning. In viewing weaning from PMV as a process rather than an all-or-none decision, isolated, single RSBI measurements may not be the best parameter on which to base progress.
When placing our findings into the clinical context of caring for the patient in the LTAC hospital receiving PMV, one may need to review several RSBI measurements over the course of a few days to ascertain a patient’s weaning progress. Our results suggest that single measures of RSBI are not predictive of weaning for chronically ventilated patients, and rather, those who demonstrate a consistent decline in RSBI are more likely to wean. This information may be helpful to nursing and respiratory staff because it helps identify patients who are more likely to progress in clinical status, compared with those who may remain static or even deteriorate. Thus, if such a favorable RSBI trend is noted early in the course of the day, appropriate plans can be made by physicians, nurses, and respiratory therapists alike with respect to appropriating resources, staffing, and disposition.
Conclusions
When analyzed individually, single RSBI measurements have little value in predicting successful weaning in patients requiring PMV. However, we found its value may be in following serial RSBI measurements, because downward trends and decreasing variability were associated with weaning success. Thus, the incorporation of serial RSBI values into the management of patients with PMV may allow clinicians to more accurately predict weaning success in this population.
References
- 1.Nelson JE, Meier DE, Litke A, Natale DA, Siegel RE, Morrison RS. The symptom burden of chronic critical illness. Crit Care Med. 2004;32:1527–1534. doi: 10.1097/01.ccm.0000129485.08835.5a. [DOI] [PubMed] [Google Scholar]
- 2.Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 2010;182:446–454. doi: 10.1164/rccm.201002-0210CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson JE, Kinjo K, Meier DE, Ahmad K, Morrison RS. When critical illness becomes chronic: informational needs of patients and families. J Crit Care. 2005;20:79–89. doi: 10.1016/j.jcrc.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Munoz-Price LS. Long-term acute care hospitals. Clin Infect Dis. 2009;49:438–443. doi: 10.1086/600391. [DOI] [PubMed] [Google Scholar]
- 5.Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. JAMA. 2010;303:2253–2259. doi: 10.1001/jama.2010.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, et al. Post-ICU mechanical ventilation at 23 long-term care hospitals: a multicenter outcomes study. Chest. 2007;131:85–93. doi: 10.1378/chest.06-1081. [DOI] [PubMed] [Google Scholar]
- 7.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Criner GJ. Long-term ventilation introduction and perspectives. Respir Care Clin N Am. 2002;8:345–353. doi: 10.1016/s1078-5337(02)00021-7. v. [DOI] [PubMed] [Google Scholar]
- 9.Happ MB, Hoffman LA. Research needs related to the care of patients on prolonged mechanical ventilation. Heart Lung. 2011;40:93–94. doi: 10.1016/j.hrtlng.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Morganroth ML, Morganroth JL, Nett LM, Petty TL. Criteria for weaning from prolonged mechanical ventilation. Arch Intern Med. 1984;144:1012–1016. [PubMed] [Google Scholar]
- 11.Scheinhorn DJ, Hassenpflug M, Artinian BM, LaBree L, Catlin JL. Predictors of weaning after 6 weeks of mechanical ventilation. Chest. 1995;107:500–505. doi: 10.1378/chest.107.2.500. [DOI] [PubMed] [Google Scholar]
- 12.Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, Wallace WA. Outcomes in post-ICU mechanical ventilation: a therapist-implemented weaning protocol. Chest. 2001;119:236–242. doi: 10.1378/chest.119.1.236. [DOI] [PubMed] [Google Scholar]
- 13.Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med. 1996;335:1864–1869. doi: 10.1056/NEJM199612193352502. [DOI] [PubMed] [Google Scholar]
- 14.Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. 1991;324:1445–1450. doi: 10.1056/NEJM199105233242101. [DOI] [PubMed] [Google Scholar]
- 15.Chao DC, Scheinhorn DJ. Determining the best threshold of rapid shallow breathing index in a therapist-implemented patient-specific weaning protocol. Respir Care. 2007;52:159–165. [PubMed] [Google Scholar]
- 16.MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest. 2005;128:3937–3954. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Jubran A, Mathru M, Dries D, Tobin MJ. Continuous recordings of mixed venous oxygen saturation during weaning from mechanical ventilation and the ramifications thereof. Am J Respir Crit Care Med. 1998;158:1763–1769. doi: 10.1164/ajrccm.158.6.9804056. [DOI] [PubMed] [Google Scholar]
- 19.Grasso S, Leone A, De MM, Anaclerio R, Cafarelli A, Ancona G, et al. Use of N-terminal pro-brain natriuretic peptide to detect acute cardiac dysfunction during weaning failure in difficult-to-wean patients with chronic obstructive pulmonary disease. Crit Care Med. 2007;35:96–105. doi: 10.1097/01.CCM.0000250391.89780.64. [DOI] [PubMed] [Google Scholar]
- 20.Vieira JM, Jr, Castro I, Curvello-Neto A, Demarzo S, Caruso P, Pastore L, Jr, et al. Effect of acute kidney injury on weaning from mechanical ventilation in critically ill patients. Crit Care Med. 2007;35:184–191. doi: 10.1097/01.CCM.0000249828.81705.65. [DOI] [PubMed] [Google Scholar]
- 21.Reid C. Frequency of under- and overfeeding in mechanically ventilated ICU patients: causes and possible consequences. J Hum Nutr Diet. 2006;19:13–22. doi: 10.1111/j.1365-277X.2006.00661.x. [DOI] [PubMed] [Google Scholar]
- 22.Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M. Impact of renal dysfunction on weaning from prolonged mechanical ventilation. Crit Care. 1997;1:101–104. doi: 10.1186/cc112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dasgupta A, Rice R, Mascha E, Litaker D, Stoller JK. Four-year experience with a unit for long-term ventilation (respiratory special care unit) at the Cleveland Clinic Foundation. Chest. 1999;116:447–455. doi: 10.1378/chest.116.2.447. [DOI] [PubMed] [Google Scholar]
- 24.Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, LaBree LD, Heltsley DJ. Post-ICU mechanical ventilation: treatment of 1,123 patients at a regional weaning center. Chest. 1997;111:1654–1659. doi: 10.1378/chest.111.6.1654. [DOI] [PubMed] [Google Scholar]
- 25.Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, et al. Ventilator-dependent survivors of catastrophic illness transferred to 23 long-term care hospitals for weaning from prolonged mechanical ventilation. Chest. 2007;131:76–84. doi: 10.1378/chest.06-1079. [DOI] [PubMed] [Google Scholar]
- 26.Epstein SK, Ciubotaru RL. Influence of gender and endotracheal tube size on preextubation breathing pattern. Am J Respir Crit Care Med. 1996;154:1647–1652. doi: 10.1164/ajrccm.154.6.8970349. [DOI] [PubMed] [Google Scholar]
- 27.Aboussouan LS, Lattin CD, Anne VV. Determinants of time-to-weaning in a specialized respiratory care unit. Chest. 2005;128:3117–3126. doi: 10.1378/chest.128.5.3117. [DOI] [PubMed] [Google Scholar]