Abstract
Objective: To propose possible success-driven solutions for problem and complication rates encountered with the ATOMS® sling system, based on first-hand experience; and to provide possible actual alternative scenarios for the treatment of male stress urinary incontinence (SUI).
Patients and methods: During the defined period (between 4/2010 and 04/2014), 36 patients received ATOMS® system implants at our clinic. We collected pre- and post-operative evaluation data using the International Consultation on Incontinence Questionnaire Short Form (ICIQ SF). As an expansion of the questionnaire, we added questions about post-operative perineal pain, the general satisfaction with the results of the intervention and willingness to recommend the operation to a best friend.
Results: Our data shows a relatively high explantation rate, but a surprisingly high patient satisfaction rate. Explantation was required mainly due to late onset infections or other symptomatic factors. Compared to other studies early onset infections were rare.
Conclusion: A non-invasive, uncomplicated adjustable system to alleviate male stress urinary incontinence remains a challenge. Although there are various systems available for the treatment of male stress urinary incontinence, it seems that despite the advantages of the ATOMS® system, an artificial sphincter system may pose more advantages based on our experience, understanding and knowledge of its well-documented long-term solutions and problems.
Keywords: stress urinary incontinence (SUI), radical prostatectomy, artificial sphincter, port site infection, perineal infection, sling implants, Virtue® sling, Advance® sling, AMS 800®, ProAct®, Argus® sling, Male Reemex®, ATOMS® sling
Zusammenfassung
Fragestellung: Es erfolgt die Darstellung der Probleme und Komplikationsraten mit dem ATOMS®-Schlingensystem an Hand von eigenen Ergebnissen, um aktuelle Behandlungsmöglichkeiten von männlicher Stressinkontinenz zu analysieren.
Material und Methode: In dem definiertem Zeitraum (4/2010 bis 4/2014) wurde bei 36 Patienten ein ATOMS®-System in unserer Klinik implantiert. Die Evaluation erfolgte prä- und postoperativ mithilfe des internationalen Fragebogens zur Inkontinenz (ICIQ SF). Es erfolgte die Erweiterung des Fragebogen mit Fragen über die postoperative perineale Schmerzsymptomatik, die generelle Zufriedenheit mit Operationsergebnis und über die Bereitschaft zur Therapieweiterempfehlung an den besten Freund.
Ergebnisse: Unsere Daten zeigen eine relativ hohe Explantationsrate, jedoch eine hohe Patientenzufriedenheit. Die Explantation war in den meisten Fällen aufgrund einer Spätinfektion des Implantats oder aufgrund anderer symptomatische Faktoren notwendig. Im Vergleich zu anderen Studien zeigte sich unmittelbar postoperativ eine geringere Infektionsrate.
Schlussfolgerung: Ein nicht invasives, unkompliziertes adjustierbares System zur Linderung der männlichen Stressinkontinenz bleibt eine Herausforderung. Obwohl unterschiedliche Systeme zur Behandlung der männlichen Stressinkontinenz verfügbar sind, scheint es, dass ein artifizieller Sphincter mehr Vorteile gegenüber dem ATOMS®-Systems besitzt. Dies könnte jedoch auch aufgrund zahlreicher, gut dokumentierter und langfristiger Daten über den artifiziellen Sphincter begründet werden.
Introduction
Worldwide stress urinary incontinence affects 1.2% of men aged 45 to 54, 3.8% of men aged 55 to 64 and 4.9% of men aged ≥65 [1]. A radical prostatectomy (RPx) is considered one of the main reasons for iatrogenic (stress urinary incontinence) SUI [2]. The prevalence is estimated at 43% mainly due to various surgical techniques, definitions of incontinence and applicable treatment or recuperation periods [3].
Following a radical cystectomy with orthotic bladder replacement, up to 15% encounter stress incontinence during the day [4]. In case of external prostatic radiation and TUR-P, the respective stress urinary incontinence incidences lie between 1–16% and 1–3% [5], [6], [7].
The past few years were marked by a rapid and multi-facetted development of various systems designed for the treatment of male SUI. In the process, the artificial sphincter (AMS, USA) is considered the “Gold Standard” in the treatment of male SUI. The disadvantage of the system is the essential “service” surgery required after a few years. Such surgery is required immanently due to the particular system and practically unavoidable. In some cases it is essential to rely on the patient for the cognitive and manual adjustment of the system, but such reliance cannot be absolute. With growing age, patients may lose the adjustment skills and in such circumstances, the system must be serviced with medical proficiency and any intervention clearly imposes limits to quality of life. In addition, the high costs associated with the AMS 800® must be considered.
The ideal system for the treatment of bladder incontinence must be cost-efficient and impose minimal invasion. Other significant aspects include a limited post-operative complications rate, non-invasive long-term adjustability possibilities and long-term sustainability, as well as the possibility to instigate interventions such as radiation of the operation area. In any event, an ideal system should place no cognitive demands, such as manual adjustment, on the patient and allow miction without urethral resistance.
The disadvantages of artificial sphincters and the successful clinical treatment of male SUI led to various new systems requiring minimal invasion in the recent past. The reported success rates for most types of sling systems vary between 50 and 85% [8], depending on the definition of successful outcomes. Few of the available sling implants are adjustable and those that allow some adjustment (such as Male Reemex®), the adjustment requires surgical intervention [8].
The adjustability of actual sling systems promises long-term success. The benefits compared to those of the “Gold Standard” AMS sphincter include the simple implantation technique and short period of patient in-hospital immobilization.
The non-existence of mechanical components is also considered a valuable benefit.
The actually available systems may be classified into six main therapies:
Para-urethral injectable substances (Deflux®, Urovive®, Macroplastique®, Contigen®, Teflon®)
Non-adjustable systems (InVance®, Advance-XP®, Virtue® sling, I Stop TOMS®)
Adjustable systems (Male Reemex®; Argus® sling; Phorbas® system; Pro-Act®; ATOMS®)
Artificial sphincters (AMS 800®, Zephir ZSI 375®, Flow Secure®)
Stem cell therapy
Supravesical urinary tract (ileum, urethro-cutaneostomy).
Further differentiation based on these classifications lead to functional aspects of three therapeutic concepts [9]:
Urethral compression: semi-circular (InVance®, I Stop TOMS®, Argus, ProAct®) or circumferential (artificial sphincter)
Functional repositioning of the bulbar urethra (Advance®)
Combined compression and repositioning (ATOMS®).
A fixed synthetic sling is positioned after the retropubis, transobturatory under the bulbar urethra, or at the inferior ramus ossicle (InVance®).
The most common treatment modalities are the artificial sphincter and the sling system [2], also shown in the actualization of the EAU Guidelines [9].
The objective of an adjustable system is the possibility to adapt the system to the individual actual continence status of a patient. In other words, the system may be used to restore increased urethral resistance, or to reduce the urethral compression in case of urinary outlet obstruction. This requires a sub-urethral sling that allows tension adjustment post-operatively.
The ATOMS® system is considered a minimal invasive system that allows non-invasive adjustment. As such, it differs from other systems such as the Argus® sling.
Patients and methods
Our report relates to our clinical work and experience with the ATOMS® system (Figure 1 (Fig. 1), Figure 2 (Fig. 2), Figure 3 (Fig. 3)). We have been using the system for four years at our clinic and compared our findings with information obtained from other reported studies. Between 4/2010 and 04/2014, 36 patients received ATOMS® system implants at our clinic.
Figure 1. Components of the ATOMS® system (picture placed with kind permission of AMI GmbH, Feldkirch, Austria).

Figure 2. ATOMS® systems model (picture placed with kind permission of AMI GmbH, Feldkirch, Austria).
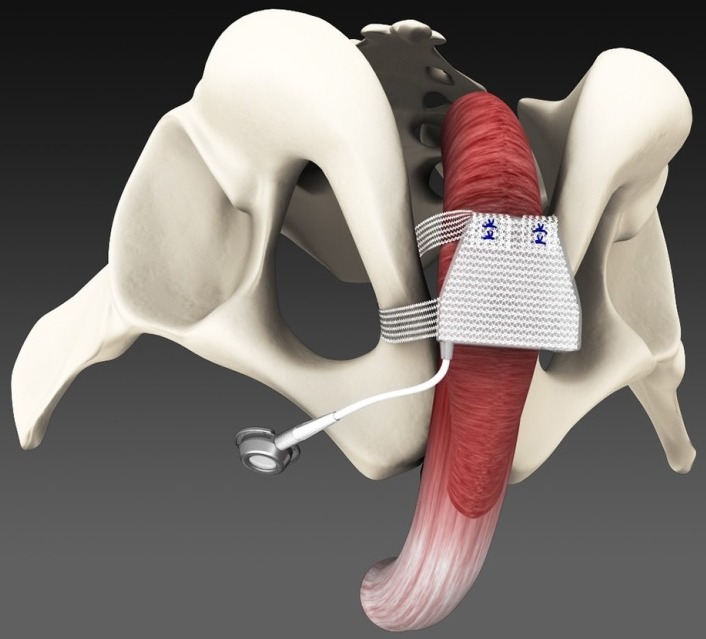
Figure 3. X-ray image of ATOMS® system implant.

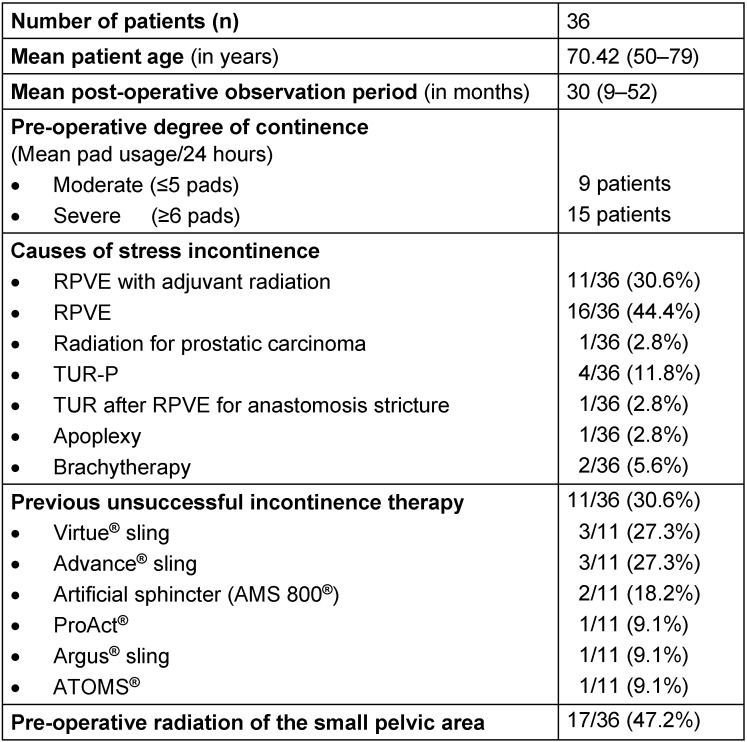
Table 1 (Tab. 1) shows the general pre-operative data for the collective patient group. The basis for data collection in terms of pre- and post-operative evaluation of patient satisfaction was the International Consultation on Incontinence Questionnaire Short Form (ICIQ SF). In addition and as adjuvant information, we included questions about post-operative perineal pain, the general satisfaction with the results of the intervention, as well as willingness to recommend the operation to a best friend. A markedly modified questionnaire was mailed to patients. Post-operative complications, the causes for the explantation and localized infections were recorded and analyzed to provide broader insight.
Table 1. General pre-operative data about the patient group.
In view of the post-operative continence information, patients (n=10/36) that required explantation of the ATOMS® system were not included in the analysis, even though some of the patients developed functioning systems within certain periods. One patient suffered from deteriorating dementia and could contribute limited data only. Pre-operatively two patients were respectively fitted with urinary devices, in other words, long-term catheters. One patient died due to myocardial infarction. One patient required only port explantation following a port site infection that caused the saturated sub-urethral cushion at the full port catheter to maintain continence.
We implanted the titanium port system in the left lower abdomen. One patient received the newly established scrotal port developed by AMI (Agency for Medical Innovations, Austria).
Pre-operatively, we conducted an urodynamic and a cystoscopic investigation. Following a perineal incision, the sub-urethral four points of the sphincter replacement cushion were fixed using the two-transobturator polypropylene mesh arms by applying the “outside-in” technique. The titanium port was placed in the left symphesis region or left scrotal region. It was anchored to the sphincter replacement cushion via a catheter. The cushion was filled via the port using a mixture of distilled water and contrast (Ultravist®). Intra-operative filling volume (5–9 ml) occurred after the application of 10 ml followed by passive evacuation of the system through surrounding pressure on the silicon cushion. The 14 Charrière long-term catheter from the urinary tract was removed one day after surgery. Additional adjustment was done where necessary, but at the earliest after four weeks and then only once every 14 days.
The statistical analysis was completed using statistical software (IBM SPSS Statistics 22). The assumption for statistical significance was p<0.05. Data is shown at a mean of ± Standard Deviation (SD). Therapeutic results were recorded where the number of pads used within 24 hours were reduced to a maximum of two pads. Where the system had to be explanted, the patient was entered as a complete therapeutic failure. Infections that related to the ATOMS® system were recorded as early infections if the infection occurred within four weeks.
Outcomes
There were no intra-operative injuries to the urinary tract or bladder. Pre-operative data about the collective patient group and the data relating to post-operative outcomes are shown in Table 1 (Tab. 1). A total of 17 patients (47.2%) underwent pre-operative radiation of the small pelvic area. About a third of patients (11/34; 32.4%) showed pre-operative stress incontinence. The response to the questionnaire was 100%.
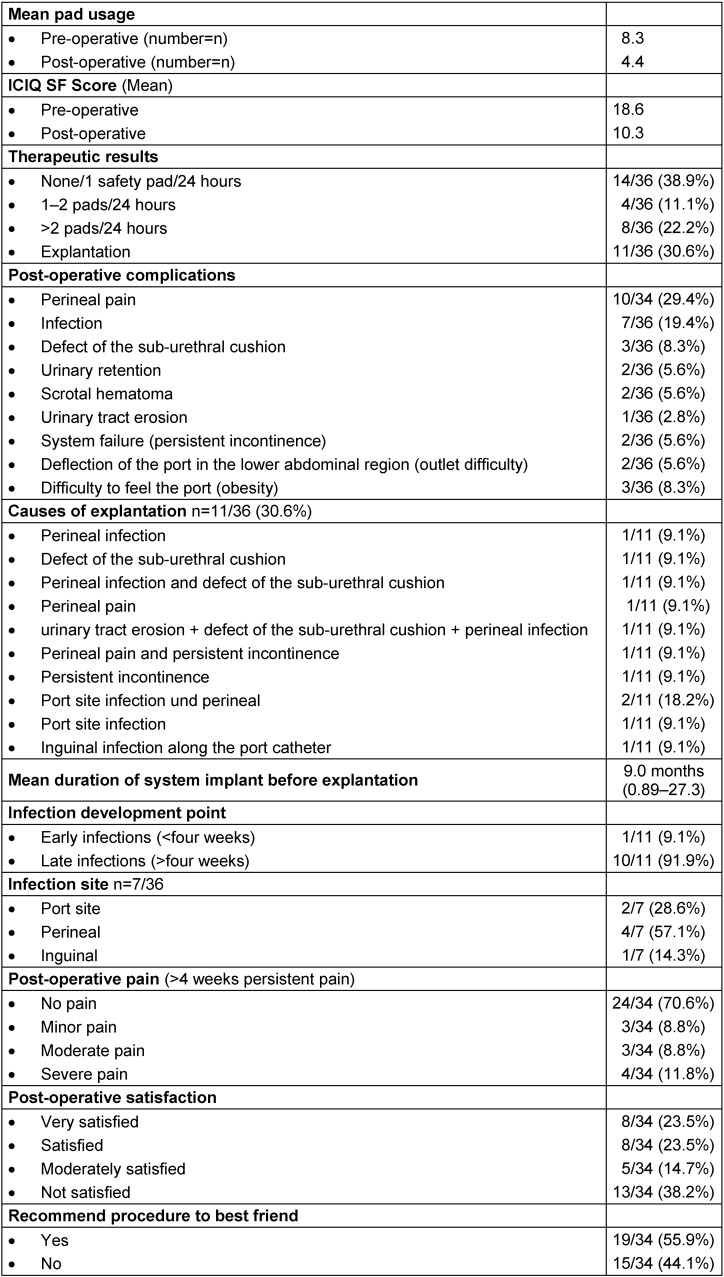
Patient satisfaction showed a significant reduction of the ICQ SF Scores from 18.65 to 10.31 (p>0.01), with a significant decline in the mean daily pad usage from 8.33 to 2.77 (p<0.01). Social continence (maximum of one pad/24 hours) was achieved by 14/36 patients (38.9%). At least 18/36 patients (50%) achieved one therapeutic result. Complete therapeutic failure was recorded for 11/36 patients (30.6%).
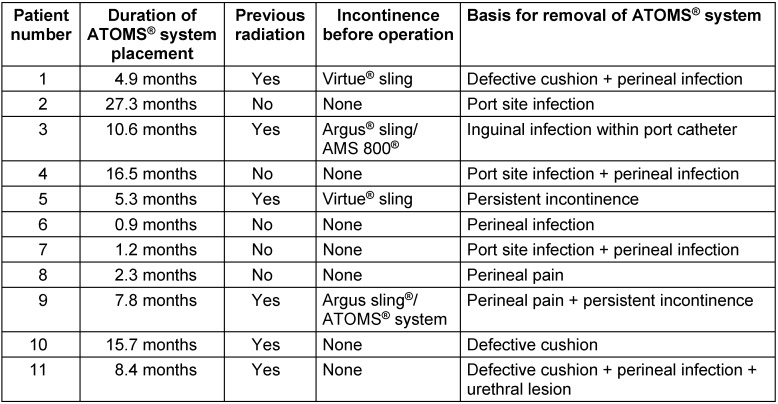
Explantation of the system was necessary for 11/36 patients (30.6%) and one patient required explantation of the port only. The system catheter was filled and provided with a cuff. Details of these patients are shown in Table 2 (Tab. 2). A total of four different reasons for explantation were identified as individual or concomitant causes.
Table 2. Pre-operative data und post-operative results.
The percentage of patients that underwent radiation of the small pelvic region, shown as part of the collective group, was 47.2% (17/36). Where explantation was required, more than half of the patients underwent radiation of the small pelvic area before receiving the implant (6/11; 54%). The statistical analysis showed no relative connection. Of these patients, 4/11 (36.4%) showed incontinence before the operation.
Nine possible types of complications were identified in the patient group. Infections that related specifically to the ATOMS® system affected 6/34. Other significant infections included those in the region of the port site, as well as the perineal and genito-femoral regions.
The implanted ATOMS® systems that required eventual explantation remained in place for a mean period of nine months (Table 3 (Tab. 3)).
Table 3. Overview of ATOMS® system explantation patients.
Post-operative perineal pain that lasted more than four weeks affected 10/34 patients. The questionnaire responses showed that 8/34 patients were very satisfied, while 13/34 patients indicated that they were not satisfied. According to the responses, 19 of the 34 patients would recommend the system to their best friends.
Discussion
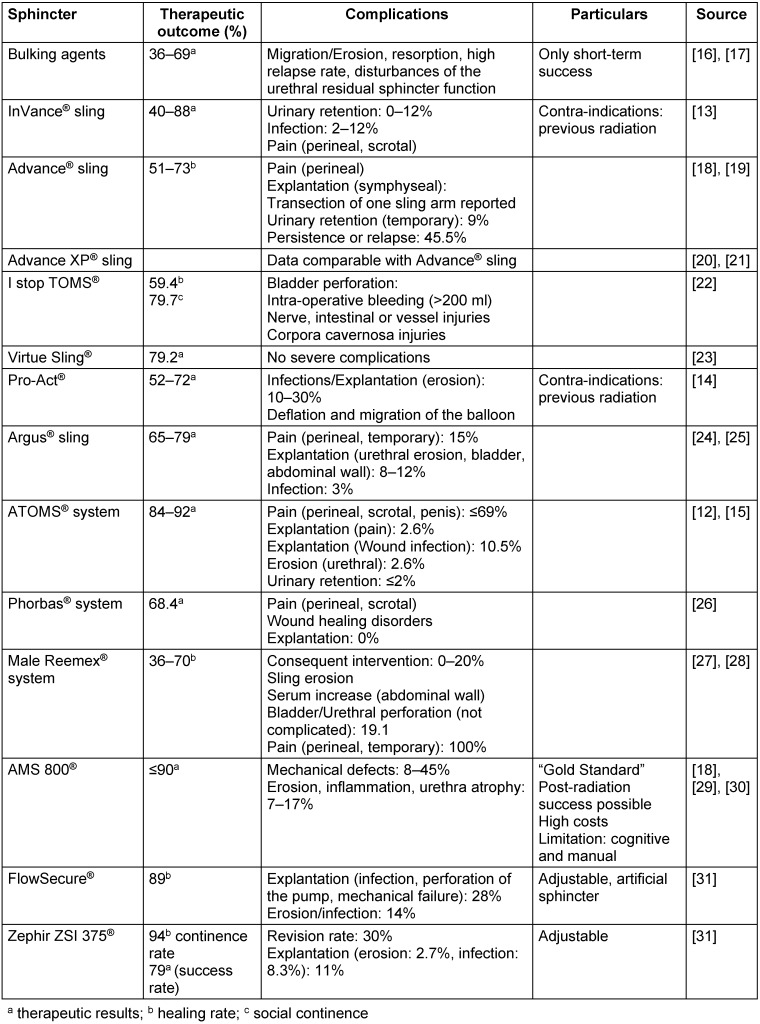
It is difficult to compare the respective available treatments (Table 4 (Tab. 4)), even within a single system, because of the different definitions and interpretations of measuring mechanisms for continence (such as number of pads, one-hour pad test, 24-hour pad test), the surgical expertise and various indications [10]. The evidence profile of a single, much quoted study about the functions of the system is insignificant [11].
Table 4. Comparison of the respective therapeutic possibilities for the treatment of stress incontinence.
The overall analysis of patient satisfaction levels for our collective patient group, showed a sound and significant improvement in ICIQ SF Scores, from 18.65 to 10.31 (p<0.01), as well as a significant reduction in the mean daily use of pads, from 8.33 to 2.77 (p<0.01). A significant percentage, 14/36 patients (38.9%) achieved social continence (maximum of one pad/24 hours).
Half of our patient group, 18/36 (50%) showed at least one therapeutic result.
The detailed analysis of results shows a clearly different picture. About half of the patients (16/34 patients (47%) indicated that they were satisfied or very satisfied with the results of the operation. On the other hand, 13/34 patients (38%) indicated that they were not satisfied post-operatively, while 5/34 patients (15%) indicated only moderate satisfaction after the operation. More than half the patients 19/34 (56%) would recommend the ATOMS® system to their best friends. In a multi-center study by Hoda et al. [12], 92% of the patients were satisfied with the system and would recommend the therapy for male stress incontinence as first-line therapy.
About one third 11/36 (31%) of the patient group must be categorized as complete therapeutic failures as they required system explantation. It was also shown that infection is the main reason for explantation and therefore the biggest risk for explantation of the total system. In this regard, infections were identified as a single or concomitant complication.
Infections were detected in 7/36 (19.4%) of our collective patient group and this rate is clearly higher than the rate reported by Hoda [12]. In that study infections affected 4/99 (4%) of the patient group. Our patient group showed that infections were not identified only in the port site region (3/7) (as reported by [12]), but infections also affected the perineal (5/7) and inguinal (1/7) regions.
It is essential to differentiate between early and late infections. Our collective patient group showed only one patient suffering from an infection less than four weeks after implantation. This was the only early infection identified. Most early infections in the port site region are caused by a failure to change gloves during the operation when working between the perineal region and the abdominal area [12]. Late infections at the port site are caused mainly by unsterile port opening procedures to view or manage adjustments. In view of this, a high adjustment frequency of is not merely stressful for the patient, it also poses a high risk for port site infection. In our experience, it is possible to reduce adjustment frequencies by securing a very tight initial interface of the sub-urethral cushion. Late infections in the port region situated in the left lower abdomen are to be expected as the actual modification of the scrotal port implantation has an effect on the infection rate. Infections occur uni-localized or bi-localized. The perineal infection encountered was not localized, it was accompanied by other problems (including a defect of the sub-urethral cushion, port site infection and urinary tract erosion). Any port site infection increases the risk of perineal infection. The eventual result of the infection was explantation. An analysis of causes for explantation shows many variables (Table 2 (Tab. 2)). The port site infection was not the only cause of the explantation (of only the port), the infection was aggravated by the defect of the sub-urethral cushion, perineal pain and urinary tract erosion. It is essential to note combinations and concomitant problems. It is of critical importance to note that the simultaneous infections indicate different locations, not a primary infection site that caused progressive infection. The mean implantation period of the system before required explantation was nine months (274.5 days).
Only one patient showed a port site infection within four weeks of implantation. Despite the port site infection that required removal of the port, we resolved the continence problems for the particular patient. The problem required mere removal of the port, followed by shortening and filling the catheter. Such cases always pose the risk of descending infection. The situation applies to both recurring port site infections and patients that refuse further surgery. At the very least, the system can no longer be adjusted once continence is maintained. Hoda et al. [12] explanted an entire system affected by infection and re-implanted a new ATOMS® system three months later.
Problems relating to the consequences of previous radiation of the small pelvic area following surgical intervention relating to incontinence are well known. As such, the specific sphincter replacement systems (InVance® and Pro-Act®) are contra-indicated for the treatment of such patients [9], [13], [14]. To date available analyses of the therapeutic results of the ATOMS® system show no significant effects of radiation on the system [12]. In terms of the explantations rate we can confirm this advantage of the ATOMS® system. There is no statistical connection within the sub-group analysis.
Of the group that required explantation, 4/11 (36.4%) of the patients suffered from incontinence.
In severely obese patients it may be difficult to feel and adjust the port anchored to the fascia. In other patients we noticed a dip in the port that obscured pricking. In such cases the newly obtainable scrotal port could provide a functional solution.
Total explantation was required for 2/11 patients, because the transurethral cushion provided no clearly improved continence, despite the achieved filling volume.
Problems relating to long-lasting post-operative pain (Table 2 (Tab. 2)) in the perineal area, after the implantation of the ATOMS® system, are particularly varied.
In the group, 10/34 patients (29.4%) complained of continued pain in the perineal region lasting more than four weeks after implantation. In the multi-centric study by Hoda et al. [12] patients complained only of temporary pain or sensitivity issues (68.7% of patients), but the associated pain did not lead to explantation. In our group, 2/11 patients suffered such symptomatic pain that became essential to remove the implants. Due to the pain, one patient refused additional occlusion of the system. It is understandable, because the compression pressure within the urinary tract increases.
Eventually the cushion changes shape (it takes on a balloon shape) because of the dorsal and ventral pressure on the tissue. It seems as if a high filling volume leads to a clearly reduced increase in continence in cases of a very high proportional increase in pain. At the upper filling volume limits there is no material increase in continence and one should therefore assume that the system has failed. In such cases it is reasonable to recommend explantation and to opt for a circular system. Adjustment should not increase residual urinary volume to >100 ml as that will not increase the patient’s pain to intolerable levels.
The effects of the filling volumes on pain symptomatics, continence rates and the effects of filling volumes compared to the pre-operative degree of incontinence require further investigation.
The defining advantage of the sling system compared to an artificial sphincter is that miction is possible without system manipulation. As such the system is particularly beneficial in patients with limited manual or mental abilities. Although available literature often refers to the advantage that the ATOMS® system does not necessarily require revision surgery due to mechanical failure as compared to those required for artificial sphincters [15] it is important to note that three patients in our collective patient group experienced problems relating to defective ATOMS® system sub-urethral cushions.
An actual overview of the success rates and problems experienced with therapy options offered by competitors in the market is shown in Table 4 (Tab. 4).
Relevance in practice
There are various systems available for the treatment of male stress urinary incontinence. Compared to the artificial sphincter, the ATOMS® system allows simple adjustment and a simple surgical technique. The system does not depend on manual or mental ability for day-to-day management. The main advantage compared to other systems is the non-invasive, uncomplicated adjustability. However, according to our data it is imperative to note the relative high onset rate of late infections and the high explantation requirement rate. For now, the artificial sphincter remains the “Gold Standard” within the application limits (patient suitability) and the well-known related long-term problems.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele JJ Members of Committees; Fourth International Consultation on Incontinence. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–240. doi: 10.1002/nau.20870. Available from: http://dx.doi.org/10.1002/nau.20870. [DOI] [PubMed] [Google Scholar]
- 2.Trost L, Elliott DS. Male stress urinary incontinence: a review of surgical treatment options and outcomes. Adv Urol. 2012;2012:287489. doi: 10.1155/2012/287489. Available from: http://dx.doi.org/10.1155/2012/287489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Treiyer A, Anheuser P, Bütow Z, Steffens J. A single center prospective study: prediction of postoperative general quality of life, potency and continence after radical retropubic prostatectomy. J Urol. 2011 May;185(5):1681–1685. doi: 10.1016/j.juro.2010.12.052. Available from: http://dx.doi.org/10.1016/j.juro.2010.12.052. [DOI] [PubMed] [Google Scholar]
- 4.Soave A, Dahlem R, Rink M, Ahyai S, Fisch M. Inkontinenzmanagement beim orthotopen Blasenersatz. [Management of urinary incontinence after orthotopic urinary diversion]. Urologe A. 2012 Apr;51(4):494–499. doi: 10.1007/s00120-012-2814-9. (Ger). Available from: http://dx.doi.org/10.1007/s00120-012-2814-9. [DOI] [PubMed] [Google Scholar]
- 5.Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995 Jan;332(2):75–79. doi: 10.1056/NEJM199501123320202. Available from: http://dx.doi.org/10.1056/NEJM199501123320202. [DOI] [PubMed] [Google Scholar]
- 6.Scalliet PG, Remouchamps V, Curran D, Ledent G, Wambersie A, Richard F, van Cangh P. Retrospective analysis of results of p(65)+Be neutron therapy for treatment of prostate adenocarcinoma at the cyclotron of Louvain-la-Leuve. Part II: Side effects and their influence on quality of life measured with QLQ-C30 of EORTC. Int J Radiat Oncol Biol Phys. 2004 Apr;58(5):1549–1561. doi: 10.1016/j.ijrobp.2003.09.001. Available from: http://dx.doi.org/10.1016/j.ijrobp.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Shipley WU, Zietman AL, Hanks GE, Coen JJ, Caplan RJ, Won M, Zagars GK, Asbell SO. Treatment related sequelae following external beam radiation for prostate cancer: a review with an update in patients with stages T1 and T2 tumor. J Urol. 1994 Nov;152(5 Pt 2):1799–1805. doi: 10.1016/s0022-5347(17)32388-1. [DOI] [PubMed] [Google Scholar]
- 8.Hoda MR, Primus G, Schumann A, Fischereder K, von Heyden B, Schmid N, Moll V, Hamza A, Karsch JJ, Steinbach F, Brössner C, Bauer W, Fornara P. Behandlung der Belastungsinkontinenz nach radikaler Prostatektomie : Adjustierbares transobturatorisches System - prospektive multizentrische Anwendungsbeobachtung. [Treatment of stress urinary incontinence after radical prostatectomy: adjustable transobturator male system - results of a multicenter prospective observational study]. Urologe A. 2012 Nov;51(11):1576–1583. doi: 10.1007/s00120-012-2950-2. (Ger). Available from: http://dx.doi.org/10.1007/s00120-012-2950-2. [DOI] [PubMed] [Google Scholar]
- 9.Lucas MG, Bosch RJ, Burkhard FC, Cruz F, Madden TB, Nambiar AK, Neisius A, de Ridder DJ, Tubaro A, Turner WH, Pickard RS European Association of Urology. EAU guidelines on surgical treatment of urinary incontinence. Actas Urol Esp. 2013 Sep;37(8):459–472. doi: 10.1016/j.acuro.2013.02.002. Available from: http://dx.doi.org/10.1016/j.acuro.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Bauer RM, Hampel C, Haferkamp A, Höfner K, Hübner W Für den Arbeitskreis „Urologische Funktionsdiagnostik und Urologie der Frau“ der Akademie der Deutschen Gesellschaft für Urologie. Diagnostik und operative Therapie der Postprostatektomie-Belastungsinkontinenz : Empfehlungen des Arbeitskreises Urologische Funktionsdiagnostik und Urologie der Frau. [Diagnosis and surgical treatment of postprostatectomy stress incontinence: recommendation of the working group Urologische Funktionsdiagnostik und Urologie der Frau]. Urologe A. 2014 Jun;53(6):847–853. doi: 10.1007/s00120-014-3531-3. (Ger). Available from: http://dx.doi.org/10.1007/s00120-014-3531-3. [DOI] [PubMed] [Google Scholar]
- 11.Mathis S, Guba B, Adlbrecht C, Pramesberger C. Belastungsinkontinenz. Evidenz zu 4 minimal-invasiven Behandlungsmethoden mit fragwürdigem Nutzen - systematische Ubersichtsarbeit. [Stress urinary incontinence. Evidence for 4 minimally invasive methods of treating - systematic overview]. Urologe A. 2009 Nov;48(11):1330, 1332–1330, 1338. doi: 10.1007/s00120-009-2058-5. (Ger). Available from: http://dx.doi.org/10.1007/s00120-009-2058-5. [DOI] [PubMed] [Google Scholar]
- 12.Hoda MR, Primus G, Fischereder K, Von Heyden B, Mohammed N, Schmid N, Moll V, Hamza A, Karsch JJ, Brössner C, Fornara P, Bauer W. Early results of a European multicentre experience with a new self-anchoring adjustable transobturator system for treatment of stress urinary incontinence in men. BJU Int. 2013 Feb;111(2):296–303. doi: 10.1111/j.1464-410X.2012.11482.x. Available from: http://dx.doi.org/10.1111/j.1464-410X.2012.11482.x. [DOI] [PubMed] [Google Scholar]
- 13.Welk BK, Herschorn S. The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int. 2012 Feb;109(3):328–344. doi: 10.1111/j.1464-410X.2010.10502.x. Available from: http://dx.doi.org/10.1111/j.1464-410X.2010.10502.x. [DOI] [PubMed] [Google Scholar]
- 14.Herschorn S. Update on management of post-prostatectomy incontinence in 2013. Can Urol Assoc J. 2013 Sep;7(9-10 Suppl 4):S189–S191. doi: 10.5489/cuaj.1621. Available from: http://dx.doi.org/10.5489/cuaj.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seweryn J, Bauer W, Ponholzer A, Schramek P. Initial experience and results with a new adjustable transobturator male system for the treatment of stress urinary incontinence. J Urol. 2012 Mar;187(3):956–961. doi: 10.1016/j.juro.2011.10.138. Available from: http://dx.doi.org/10.1016/j.juro.2011.10.138. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto T, Gotoh M, Kato M, Majima T, Toriyama K, Kamei Y, Iwaguro H, Matsukawa Y, Funahashi Y. Periurethral injection of autologous adipose-derived regenerative cells for the treatment of male stress urinary incontinence: Report of three initial cases. Int J Urol. 2012 Jul;19(7):652–659. doi: 10.1111/j.1442-2042.2012.02999.x. Available from: http://dx.doi.org/10.1111/j.1442-2042.2012.02999.x. [DOI] [PubMed] [Google Scholar]
- 17.Strasser H, Marksteiner R, Margreiter E, Mitterberger M, Pinggera GM, Frauscher F, Fussenegger M, Kofler K, Bartsch G. Transurethral ultrasonography-guided injection of adult autologous stem cells versus transurethral endoscopic injection of collagen in treatment of urinary incontinence. World J Urol. 2007 Aug;25(4):385–392. doi: 10.1007/s00345-007-0190-7. Available from: http://dx.doi.org/10.1007/s00345-007-0190-7. [DOI] [PubMed] [Google Scholar]
- 18.Bauer RM, Gozzi C, Hübner W, Nitti VW, Novara G, Peterson A, Sandhu JS, Stief CG. Contemporary management of postprostatectomy incontinence. Eur Urol. 2011 Jun;59(6):985–996. doi: 10.1016/j.eururo.2011.03.020. Available from: http://dx.doi.org/10.1016/j.eururo.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 19.Soljanik I, Becker AJ, Stief CG, Gozzi C, Bauer RM. Repeat retrourethral transobturator sling in the management of recurrent postprostatectomy stress urinary incontinence after failed first male sling. Eur Urol. 2010 Nov;58(5):767–772. doi: 10.1016/j.eururo.2010.08.034. Available from: http://dx.doi.org/10.1016/j.eururo.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 20.Bauer RM, Hampel C, Haferkamp A, Höfner K, Hübner W Für den Arbeitskreis „Urologische Funktionsdiagnostik und Urologie der Frau“ der Akademie der Deutschen Gesellschaft für Urologie. Diagnostik und operative Therapie der Postprostatektomie-Belastungsinkontinenz: Empfehlungen des Arbeitskreises Urologische Funktionsdiagnostik und Urologie der Frau. [Diagnosis and surgical treatment of postprostatectomy stress incontinence: recommendation of the working group Urologische Funktionsdiagnostik und Urologie der Frau]. Urologe A. 2014 Jun;53(6):847–853. doi: 10.1007/s00120-014-3531-3. (Ger). Available from: http://dx.doi.org/10.1007/s00120-014-3531-3. [DOI] [PubMed] [Google Scholar]
- 21.Collado Serra A, Resel Folkersma L, Domínguez-Escrig JL, Gómez-Ferrer A, Rubio-Briones J, Solsona Narbón E. AdVance/AdVance XP transobturator male slings: preoperative degree of incontinence as predictor of surgical outcome. Urology. 2013 May;81(5):1034–1039. doi: 10.1016/j.urology.2013.01.007. Available from: http://dx.doi.org/10.1016/j.urology.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Grise P, Vautherin R, Njinou-Ngninkeu B, Bochereau G, Lienhart J, Saussine C HOMme INContinence Study Group. I-STOP TOMS transobturator male sling, a minimally invasive treatment for post-prostatectomy incontinence: continence improvement and tolerability. Urology. 2012 Feb;79(2):458–463. doi: 10.1016/j.urology.2011.08.078. Available from: http://dx.doi.org/10.1016/j.urology.2011.08.078. [DOI] [PubMed] [Google Scholar]
- 23.Comiter CV, Rhee EY, Tu LM, Herschorn S, Nitti VW. The virtue sling – a new quadratic sling for postprostatectomy incontinence – results of a multinational clinical trial. Urology. 2014 Aug;84(2):433–438. doi: 10.1016/j.urology.2014.02.062. Available from: http://dx.doi.org/10.1016/j.urology.2014.02.062. [DOI] [PubMed] [Google Scholar]
- 24.Romano SV, Metrebian SE, Vaz F, Muller V, D'Ancona CA, de Souza EA, Nakamura F. Resultados a largo plazo del estudio multicéntrico fase III del tratamiento de la incontinencia de orina post prostatectomía con un sling masculino ajustable: seguimiento mínimo 3 años. [Long-term results of a phase III multicentre trial of the adjustable male sling for treating urinary incontinence after prostatectomy: minimum 3 years]. Actas Urol Esp. 2009 Mar;33(3):309–314. doi: 10.1016/s0210-4806(09)74146-4. [DOI] [PubMed] [Google Scholar]
- 25.Hübner WA, Gallistl H, Rutkowski M, Huber ER. Adjustable bulbourethral male sling: experience after 101 cases of moderate-to-severe male stress urinary incontinence. BJU Int. 2011 Mar;107(5):777–782. doi: 10.1111/j.1464-410X.2010.09619.x. Available from: http://dx.doi.org/10.1111/j.1464-410X.2010.09619.x. [DOI] [PubMed] [Google Scholar]
- 26.Bauer RM, Kretschmer A, Hübner W. Moderne operative Therapiemoglichkeiten der mannlichen Belastungsinkontinenz. [Modern operative treatment possibilities in male stress urinary incontinence]. Urologe A. 2014 Mar;53(3):339–40, 342, 344. doi: 10.1007/s00120-013-3351-x. (Ger). Available from: http://dx.doi.org/10.1007/s00120-013-3351-x. [DOI] [PubMed] [Google Scholar]
- 27.Kim JH, Kim JC, Seo JT. Long term follow-up of readjustable urethral sling procedure (remeex system1) for male stress urinary incontinence. Abstract. Society for Urodynamics and Female Urology, 2011 Winter Meeting; 2011 Mar 1–5; Phoenix, Arizona. Neurourol Urodyn. 2011 Feb;30(2):29. doi: 10.1002/nau.21058. Available from: http://dx.doi.org/10.1002/nau.21058. [DOI] [Google Scholar]
- 28.Sousa EA. Male Remeex System™ (MRS) for the surgical treatment of male incontinence: 12 years from the first case. Eur Urol Suppl. 2014 Apr;13(1):e72. doi: 10.1016/S1569-9056(14)60074-9. Available from: http://dx.doi.org/10.1016/S1569-9056(14)60074-9. [DOI] [Google Scholar]
- 29.Lai HH, Hsu EI, Teh BS, Butler EB, Boone TB. 13 years of experience with artificial urinary sphincter implantation at Baylor College of Medicine. J Urol. 2007 Mar;177(3):1021–1025. doi: 10.1016/j.juro.2006.10.062. Available from: http://dx.doi.org/10.1016/j.juro.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 30.Silva LA, Andriolo RB, Atallah AN, da Silva EM. Surgery for stress urinary incontinence due to presumed sphincter deficiency after prostate surgery. Cochrane Database Syst Rev. 2011;(4):CD008306. doi: 10.1002/14651858.CD008306.pub2. Available from: http://dx.doi.org/10.1002/14651858.CD008306.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Chung E. A state-of-the-art review on the evolution of urinary sphincter devices for the treatment of post-prostatectomy urinary incontinence: past, present and future innovations. J Med Eng Technol. 2014 Aug;38(6):328–332. doi: 10.3109/03091902.2014.899400. Available from: http://dx.doi.org/10.3109/03091902.2014.899400. [DOI] [PubMed] [Google Scholar]