Abstract
Background:
Effective communication enables healthcare professionals and students to practise their disciplines in a professional and competent manner. Simulated-based education (SBE) has been increasingly used to improve students’ communication and practice skills in Health Education.
Objective:
Simulated learning modules (SLMs) were developed using practice-based scenarios grounded in effective communication competencies. The effect of the SLMs on Pharmacy students’ (i) Practice skills and (ii) Professionalism were evaluated.
Methods:
SLMs integrating EXCELL competencies were applied in the classroom to study their effect on a number of learning outcomes. EXcellence in Cultural Experiential Learning and Leadership (EXCELL) Program is a schematic, evidence-based professional development resource centred around developing participants’ self-efficacy and generic communication competencies. Students (N=95) completed three hours of preliminary lectures and eight hours of SLM workshops including six scenarios focused on Pharmacy Practice and Experiential Placements. Each SLM included briefing, role-plays with actors, facilitation, and debriefing on EXCELL social interaction maps (SIMs). Evaluations comprised quantitative and qualitative survey responsed by students before and post-workshops, and post-placements, and teachers’ reflections. Surveys examine specific learning outcomes by using pharmacy professionalism and pharmacy practice effectiveness scales. Responses were measured prior to the commencement of SLMs, after completion of the two workshops and after students completed their block placement. Self-report measures enabled students to self-assess whether any improvements occurred.
Results:
Student responses were overwhelmingly positive and indicated significant improvements in their Pharmacy practice and professionalism skills, and commitment to professional ethics. Qualitative feedback strongly supported students’ improved communication skills and confidence. Teacher reflections observed ecological validity of SLMs as a method to enhance professionalism and communication skills, and suggested ways to improve this teaching modality.
Conclusion:
Inclusion of SLMs centred on practice and professionalism was evaluated as an effective, teaching strategy by students and staff. The integration of SIMs in SLMs has potential for wider application in clinical teaching.
Keywords: Patient Simulation, Health Communication, Clinical Competence, Education, Pharmacy, Program Evaluation, Australia
INTRODUCTION
Effective communication is the core skill for health professionals, enabling them to become competent practitioners and contribute toward optimisation of healthcare outcomes and effective interprofessional relationships.1,2,3 Within the Australian Qualifications Framework, learning encompass the three dimensions of Knowledge (what students know or understand), Skills (what students can do or how they apply their knowledge and understanding) and Competencies (the context in which knowledge and skills can be applied), the ‘KSC taxonomy of learning outcomes’.2 The National Competency Standard framework for Pharmacists in Australia defines ‘communication’ as the ability to effectively communicate in English information arguments and analyses, encompassing the capacity to participate in sustained and complex oral transactions demonstrating flexible and adaptive techniques as well as the ability to generate written texts that clearly express complex relationships between ideas and purposes.2 Health disciplines have successfully utilised simulation-based education (SBE) in communication training.4,5,6,7 Simulated learning modules utilising standardised patients have a significant impact on student communication skills across time and are well received by students and standardised patients5 who tend to find these modified tutorials more engaging.4 Health Workforce Australia’s comprehensive report on SBE in Australian medical education underscores the contribution in clinical preparation.8 SBE makes a valuable contribution to learning for students, especially for clinical skills, clinical decision making, patient-centred and interprofessional communication, and teamwork.8 Optimisation of Health students’ communication competencies enables their learning in the classroom and on placement.9,10 It can be somewhat challenging for academics and clinicians to determine the most successful approach to teaching communication in Health education because the majority of studies are context-specific in nature. The current lack of sufficient clinical placements, the need to maximise those placements that are available, and the importance of enhancing interprofessional practice fuelled the innovative approach of the present study. The study was informed by the principal researcher’s experiences as a Pharmacy Placements Convenor9, and consistent feedback from students and Placements preceptors regarding communication, practice and learning challenges, consistent with the literature.11,12 The intervention utilised components of the EXcellence in Cultural Experiential Learning and Leadership (EXCELL) Program, a schematic, evidence-based professional development resource centred around developing participants’ self-efficacy and generic communication competencies (i.e., seeking help, expressing disagreement, participating in a group, giving and receiving feedback and refusing a request). EXCELL has been integrated effectively in the curriculum of diverse disciplines including Nursing, Psychology, Pharmacy and Business to teach communication skills to support professionalization.13,14,15 The present study was part of a larger pharmacy education project that examined how SLMs could be used effectively within the teaching process. Various aspects of pharmacy practice and placement activities were addressed in each SLM competency (see Table 1). All of the scenarios addressed a variety of professional practice encounters in hospital and community pharmacy. The SLMs were grounded in the EXCELL communication competencies. The effect of the SLMs on Pharmacy students’ (i) Practice skills and (ii) Professionalism were evaluated.
Table 1.
SLM Scenarios (each practised at varying levels of difficulty in SLM workshops)
| Scenario | SLM Competency | Personnel | Scenario Description | Teaching process |
|---|---|---|---|---|
| 1 | Seeking help | Hospital and community Pharmacist. | Role-play between hospital and community pharmacist to arrange a discharge. | Whole group watch two actors model scenario, then practice in small groups. |
| 2 | Expressing disagreement | Pharmacy owner, Patient, Pharmacist. | Disagreement between Pharmacists regarding customer returning a medication. Ambiguity. | Clarification of legal requirements. Observation, modelling in small groups. |
| 3 | Participating in a group | Doctors (Consultant, Resident), Nurse, Pharmacist | Clinical review/ward round. Pharmacist needs to comment re cross-sensitivity of allergy. | Consultant doctor acts in either dominating or accommodating manner. Role cards required. |
| 4 | Receiving feedback | Pharmacist, Customer | Customer complaint: Vet’s (animal) prescription incorrectly dispensed | Negative scenario modelled first, followed by discussions. Students volunteer to model a more effective way. |
| 5 | Refusing a request | Pharmacist, Customer | Patient requests restricted medication. Pharmacist should deny sale. | Have different types of customer – old vs young, rude vs very nice, abusive. |
| 6 | Giving feedback –student acting in the role of the preceptor | Young Pharmacist, Pharmacy student | Young pharmacist giving an older pharmacy student verbal constructive or negative feedback. | Small groups, with actor playing role of student, being given feedback by preceptor, (played by student). |
METHODS
SLMs were implemented in the ‘Advanced Practical Experience’ course, a 4th year course which was part of a five-year Master of Pharmacy course. The course was designed to prepare students for pharmacy practice because it was undertaken prior to students completing a three-week block placement in a community or hospital pharmacy in Australia. There were 32 male and 59 female students (4 participants undeclared), and the mean age was 24.0 years (SD=4.10). There were 79.3% Australian citizens/permanent residents, with 63.0% born in Australia, and 20.7% overseas students. Students were born in 20 different countries; 28.3% had a non-English speaking background (NESB), spoke 16 different languages at home, and only 66.0% reported speaking English as the main home language. Pharmacy students (N=95) attended three hours of lectures and eight hours of workshops (i.e. two four-hour workshops, a week apart). Information sheets were provided to students outlining the voluntary nature of their participation in SLMs as well as the filming component, as per the ethics protocols. Students were informed that filming may be used for research purposes in the future. Introductory lectures outlined the concept of SLM and the assumed core knowledge component that underpinned each scenario. For example, Scenario 2 (‘expressing disagreement’) tested students’ knowledge of the legal requirements pertaining to a Pharmacist not being allowed to accept medicine that was returned by a customer. As the SLMs largely focused on the optimisation of professional communication skills, it was important to avoid any core knowledge gaps preventing students from participating effectively in the SLMs. Each SLM scenario was developed by combining competencies from the National Competency Standards Framework for Pharmacists in Australia, EXCELL, and the researchers’ personal practice/educational experiences.2,13,16,17,18,19,20 The six SLM competencies were: seeking help, expressing disagreement, participating in a group, giving and receiving feedback, and refusing a request. Each SLM focused on specific scenarios from practice and placements role-played with trained actors. Table 1 presents the SLM competencies and related scenario description, personnel/roles (pharmacists, patients, other health professionals, and pharmacy preceptors), as well as the teaching process utilised.
The scenarios were fully scripted and also included various suggestions for intended modifications enabling all students to participate in the same SLMs and, at the same time, to explore varying degrees of difficulty in their communication approaches. Members of the teaching team provided group facilitation of small group role-plays with actors who also assisted facilitators with the debriefing. Actors were auditioned and briefed before the SLM workshops with regards to the scenarios and their variations. An EXCELL ‘Social Interaction Map (SIM) was developed for each SLM scenario. The aim of SIMs was to complement the competencies demonstrated in each role-play rather than offering prescriptive solutions to the social interactions, making their utilisation in this study rather novel. The maps provided step-by-step schemas for extending students’ verbal and non-verbal behavioural repertoire in professional contexts. Table 2 shows the SIM for the competency of ‘refusing a request professionally’. After each role-play, teachers used the SIM as a schema to debrief students and discuss the verbal, non-verbal behaviour and values that were evident at each stage of the interaction (ABCD).
Table 2.
Social interaction map example: ‘Refusing a request professionally’
| Stage | Verbal behaviour | Non-verbals | Values |
|---|---|---|---|
|
A Attending / Approach |
Pharmacist approaches patient at counter Makes eye contact with patient |
Importance of medication safety Legal/ethical requirements Respect for patient |
|
|
B Bridging |
I’ve been looking at your records of medication through the dispensing system | Pleasant face Calm but firm voice |
Professional self-respect & respect for patient Duty of care to patient |
|
C Comenting |
I’m afraid I can’t supply this medication to you because… | Maintain eye contact Even, unemotional, clear voice |
Professional self-respect & respect for patient Thics, legalities… Concern for customer wellbeing & dignity |
|
D Departure / Developing |
I’m sorry I can’t supply what you asked for, but this might help you instead… | Maintain eye contact Pleasant voice Open smile |
Professional self-respect & respect for patient Maintaining relationship & rapport with patient |
Questionnaires comprising qualitative and quantitative measures were administered to students on four occasions: prior to the start of the workshops (T1), at the end of the first SLM workshop (T2), after completion of both workshops (T3), and post-completion of semester and pharmacy placement (T4). Only questionnaires completed at T1 (response rate 98%) and T4 (response rate 66.3%) are reported in this paper. Table 3 presents the 18-item Measure of Pharmacy Professionalism scale that was developed to measures the six tenets of professionalism (i.e. altruism, accountability, excellence, duty, honour and integrity, and respect for others). The instrument exhibits satisfactory reliability measures.33 Items included “I am respectful to individuals who have different backgrounds than mine” (Item R) and “I treat all patients with the same respect, regardless of perceived social standing or ability to pay” (Item N). Responses ranged from SD=strongly disagree (rating 1) to SA=strongly agree (rating 5).
Table 3.
Measure of pharmacy professionalism33
| Items | Level of agreement | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| A. I do not expect anything in return when I help someone. | SD | D | N | A | SA |
| B. I attend class/placement/work daily as required. | SD | D | N | A | SA |
| C. If I realise that I will be late, I contact the appropriate individual at the earliest possible time to inform them. | SD | D | N | A | SA |
| D. If I do not follow through with my responsibilities, I readily accept the consequences. | SD | D | N | A | SA |
| E. I want to exceed the expectation of others. | SD | D | N | A | SA |
| F. It is important to produce quality work. | SD | D | N | A | SA |
| G. I complete my tasks independently and without supervision. | SD | D | N | A | SA |
| H. I follow through with my responsibilities. | SD | D | N | A | SA |
| I. I am committed to helping others. | SD | D | N | A | SA |
| J. I would take a job where I felt I was needed and could make a difference even if it paid less than other positions. | SD | D | N | A | SA |
| K. It is wrong to cheat to achieve higher rewards (i.e., grades, money). | SD | D | N | A | SA |
| L. I would report a medication error even if no one else was aware of the mistake. | SD | D | N | A | SA |
| M. I am able to accept constructive criticism. | SD | D | N | A | SA |
| N. I treat all patients with the same respect, regardless of perceived social standing or ability to pay. | SD | D | N | A | SA |
| O. I address others using appropriate names and titles. | SD | D | N | A | SA |
| P. I am diplomatic when expressing ideas and opinions. | SD | D | N | A | SA |
| Q. I accept decisions of those in authority. | SD | D | N | A | SA |
| R. I am respectful to individuals who have different backgrounds than mine | SD | D | N | A | SA |
Table 4 lists the 11-item Measure of Pharmacy Practice Skills utilised in the present study. It outlines the ‘Measure of pharmacy practice skills’ scale utilised in the present study. This scale was developed by adapting a New Zealand scale for assessment of graduates’ practice skills to correspond to the Australian Competency Standards, reflecting several relevant domains.2,34 The pharmacy students’ communication skills section was retained in its original format and included the student’s self-perceived ability to communicate effectively with pharmacy staff, health professionals, their preceptor, patients and customers, and other people (suppliers, representatives, receptionists).34
Table 4.
Measure of Pharmacy Practice skills34
| Items | Level of agreement | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| A. I am capable of contributing to the optimal use of medicines. | SD | D | N | A | SA |
| B. I am effective in terms of my communication in the workplace. | SD | D | N | A | SA |
| C. I am effective in terms of my collaboration in the workplace. | SD | D | N | A | SA |
| D. I am effective in terms of my self-management in the workplace. | SD | D | N | A | SA |
| E. I have sufficient awareness of possible ethical and legal dilemmas in Pharmacy practice. | SD | D | N | A | SA |
| F. I am effective in interacting with people with culturally and linguistically diverse backgrounds. | SD | D | N | A | SA |
| G. I have effective spoken English communication with: | |||||
| a. Other pharmacy staff | SD | D | N | A | SA |
| b. Health professionals | SD | D | N | A | SA |
| c. The preceptor | SD | D | N | A | SA |
| d. Patients and customers | SD | D | N | A | SA |
| e. Other people (suppliers, representatives, receptionists) | SD | D | N | A | SA |
Changes over time for the pharmacy practice skills and professionalism were collected and analysed using repeated-measures t-tests. In addition to analysis of students’ quantitative pre- (T1) and post-SLM (T4) responses. Qualitative data was collected about the students’ general evaluation of the SLMs at T4. This qualitative data analysis was facilitated by MAXqda computer software.21 Following the grounded theory technique, data was categorised through open, axial, and selective coding.22 The coding scheme was explained and the questions coded by an independent rater. Both sets of coding were examined independently by a third person with research training and content knowledge in order to ensure reliability. Coding accuracy had consistency well over 90%, indicating an appropriate level of inter-rater reliability.23 On the few occasions where disagreements occurred, the third person examined the transcript and adjusted the code/s as required.
RESULTS
There was a significant improvement for pharmacy practice skills between T1 and T4, t(54)= -2.74, p=0.008, d=0.36, and for pharmacy professionalism, t(54)= -4.80, p<0.001, d=0.64. (Table 5, Figure 1).
Table 5.
Means and Standard Deviation for pharmacy practice skills and pharmacy professionalism at T1 and T4.
| Measure | Time | Mean | SD |
|---|---|---|---|
| Pharmacy professionalism | 1 | 4.13 | 0.40 |
| 4 | 4.34 | 0.41 | |
| Pharmacy practice skills | 1 | 4.14 | 0.52 |
| 4 | 4.29 | 0.48 |
Figure 1.
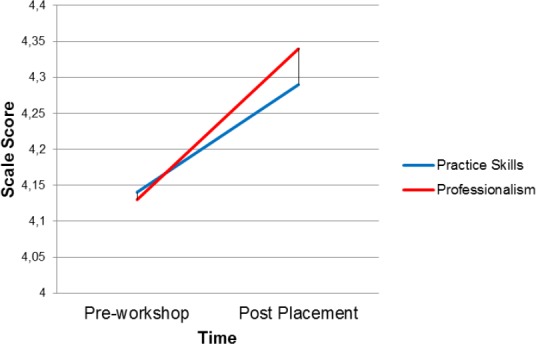
Means for Pharmacy Practice Skills and Pharmacy Professionalism at T1 and T4.
Students appreciated the opportunity to practise different scenarios that pharmacists come across in their daily practice, which also made them aware of the importance of non-verbal communication skills and confidence. Having the opportunity to give as well as receive feedback was also highly valued by the students. They acknowledged that the newly acquired communication strategies helped them to improve their professionalism and practice skills, and enhance cooperation with other professionals. Congruent with the quantitative findings, students’ qualitative comments were positive overall in relation to the effect of SLMs on their practice skills and professionalism. Students particularly valued the following aspects of SLMs: gaining new communication skills, especially appropriate assertion; receiving clear feedback, and explanations about how to improve their interaction skills in SLM role-plays with trained actors. They also emphasised that SLMs made them aware of the importance of structured communication at different levels of complexity, which was nicely illustrated in the ABCD approach in the Social Interaction Maps (Figure 1). In addition, students appreciated that the newly acquired communication skills enhanced their practice skills, and their interactions with other professionals. Analysis of the students’ qualitative comments revealed three major themes related to the aim of the study. The themes were: ‘SLMs as teaching tools’; ‘appropriate assertiveness’, and ‘approaches to practice’.
Theme 1: Simulated scenarios as teaching tools
Students focused on how particular aspects of the SLMs helped them, such as their ‘real life’ interface: (I liked how no time limit was given to counsel a patient in SLMs, which was more similar to real life situations); the importance of behavioural feedback: (The feedback given to each scenario will be useful to utilise in future practice); and the way the novel scenarios challenged their thinking:
Many students emphasised how SLMs were time-efficient method and recommended their integration earlier in the curriculum: (It is so efficient to learn these skills through SLMs. I highly recommend School of Pharmacy to organise similar workshop in semester 1 of Master programme).
Theme 2: The appropriate assertiveness
A commonly reported theme evident in student responses related to managing anger appropriately. One student explained: (SLMs gave me guidance on how I can improve my assertiveness by having a stronger voice and not becoming passive in an aggressive situation). Another stated: (SLMs allowed me to see how interactions and conflicts can and how easily they can become aggressive & affect future relationships). For another student: (Seeing the “what not to do” responses were particularly helpful as in practice I now know what to look for and catch myself if the conversation is becoming too aggressive or passive). Several students reflected on how the SLMs impacted positively on their placement, as expressed in the following exemplar:
During placement I dealt with angry customers better because I have attended SLMs.
Theme 3: Approaches to Practice
A recurrent theme incorporated students’ reflections on how SLMs impacted positively on their practice. In addition to the previous quote about handling angry customers, students expressed the following:
I learnt to approach pharmacy practice with an open mind and see why and how the other person is responding before I respond to them.
It was useful to learn how to explain ‘why’, rather than just giving a plain statement. It was also great to learn to prepare how to deal with a certain situation rather than handle the situation ‘right off the bat ’.
Really showcased how different styles of communication get different results in professional practice situations.
How easily situations can escalate without correct techniques.
Finally, the following student’s comment encapsulates the impact on professionalism and practice:
Teaching me how to deal in certain situations and how to approach a problem was good. Improving my ability to act in a professional manner as well.
Students also mentioned that they would prefer more direct alignment between any future SLM activities and course assessment, and felt this could increase student engagement in the workshop (e.g. not all students gave permission to be filmed or participated in the role-plays performed in front of the whole workshop group). Through the SLM engagement, students became acutely aware of how their individual behaviour can change the dynamic of interpersonal interactions, and how this can directly affect important outcomes in pharmacy practice. Students also stated that SLMs helped them acquire communication skills that facilitated management of complex and personally and professionally challenging situations often encountered in pharmacy practice.
Some negative evaluation was expressed by students regarding the length of the workshops, repetition of scenarios, and suggestions that SLMs would be better held earlier in the program. Comments specifically related to the processes used in the SLM workshops included the hope that SLMs could be performed more frequently in the curriculum, with more scenarios and role-plays enacted in smaller, more intimate groups. Students also observed that they would prefer SLMs to be more aligned with the course assessment. Several students found the topics of dealing with conflict and communicating with other health professionals irrelevant as they did not encounter these situations during placement.
DISCUSSION
This study evaluated the effect of simulation on Pharmacy students’ practice skills and professionalism. Participation in SLMs enabled MPharm Pharmacy students to apply their knowledge and skills to a variety of pharmacy placement and practice role-plays in a safe, informal environment in the classroom. The study achieved its intended aim.
SLMs can be effectively integrated into Health curricula and were well received by students. They offered an opportunity for students to apply their knowledge and skills to a range of simulated role-plays, in order to enhance their practice and professionalism skills in a safe workshop environment. This study achieved its two aims, demonstrated through clear alignment between quantitative and qualitative findings, both tremendously positive. The findings support previously documented reports of students appreciating communication simulation activities in the classroom.24,25 Students acknowledged what SLMs helped them achieve in terms of their professionalisation and improvement of communication skills24,26,27, also (as illustrated in their quantitative and qualitative responses), successfully complementing the traditional curriculum and some of its challenges.28
It is encouraging to note the nuance in the qualitative student responses in terms of the effect that SLMs had on the way they understand professionalism and the multi-faceted mature of pharmacy practice. Seemingly, SLMs helped students to move beyond their ‘common’ understanding of what constitutes professional pharmacy practice, and start addressing the ‘grey’ areas of the sometimes ambiguous, uncertain, challenging sociobehavioural aspects encountered in the pharmacy. Similar pedagogic challenges have been recognised in Pharmacy education in the past.29,30,31
Significantly, almost all students found SLMs relevant in terms of acquisition of important professional pharmacy practice skills. It is also important to interpret these results in light of the fact that students’ responses were collected after the completion of the three-week placement block, enabling them to apply and trial the skills acquired through SLMs in practice before they reflected on them in the survey (T4). One of the main aims of Health professionals’ education is to develop students’ skill base in order to enable them to be professional, efficient practitioners.26,32,33,34 This study quite encouragingly demonstrates that the generic skills outlined in the EXCELL Program, and it’s adapted ‘Social Interaction Maps’ can be successfully implemented in yet another novel way to enhance learning of practitioners-in-training in the somewhat demanding area of communication teaching.
The four SLM facilitators performed an individual and structured group reflection and debriefing on the SLM design and execution after the completion of SLMs. One of the most important advantages of utilising SLMs was the opportunity for relaxed, flexibly paced, formal and informal role-plays, individual and group reflections, and feedback amongst small groups of students, facilitators, actors, and, finally, the whole workshop group. A range of professional practice environments were represented, including interprofessional interactions, adding to the fullness of students’ learning experience. In addition, SLMs, in students’ own words, exposed them to practising in an environment that they described as a ‘more professional level’ since it included trained actors and a variety of simulated interprofessional healthcare setting situations they know exist but they do not regularly experience in the classroom or on placement, similar to the reports in the literature.7,28,34
SLMs had inherent limitations in their design and execution because of their novel approach. An obvious limitation is the potential wish by the students to appear more competent than they actually are. Further, students’ subjective perceptions of the SLMs were sought and this is a limitation in itself due to students’ self-reports being subjective and unvalidated. Similar undertakings would improve their validity by including objective evaluations (blind raters). A control group, and a larger sample size, utilisation of validated questionnaires, and a longitudinal design would also strengthen future studies of SLMs in Pharmacy education and improve generalisability of results over a longer period of time. The actors’ capacity to engage and enact the desired behaviour in the interactions in a consistent, appropriate manner could be improved by choosing actors with a specific set of skills and experience. Participation in SLM workshops was mandatory but did not contribute to students’ grades, which, although explained to students, may have influenced their perceptions of the role of SLMs in the curriculum (although nevertheless most perceptions were extremely positive). Clearly, this curricular innovation represented a major staff commitment in terms of time and resources. While SLMs were highly satisfying for students and staff, their execution and long-term sustainability requires careful planning and consideration in order to ensure sufficient quality and feasibility.
CONCLUSIONS
Incorporating simulated learning and schematic EXCELL SIMs is highly promising in terms of the tremendously positive student and staff feedback. The SLMs proved to be a successful pedagogic strategy. Inclusion of practice and professionalism focused SLM scenarios were reported by students and staff to be a much needed teaching strategy. The strength of such SLMs is in providing an opportunity to the students to be exposed to professional practice situations in a supportive, constructive environment where they could experiment and receive immediate feedback on their level of performance. Promisingly, students indicated many areas in which their practice and professionalism skills improved and identified the areas of newly acquired professional practice confidence. While the intervention was limited to a single cohort and relied almost exclusively on self-reports, the study highlighted the potential to include the EXCELL-influenced SLMs more widely in the Health disciplines.
ACKNOWLEDGEMENTS
This research was financially supported in part by Health Workforce Australia (HWA). The authors would also like to gratefully acknowledge the support and assistance provided by Ms. Ruth Hills and Ms. Alannah Priddle of Griffith University during this project.
Footnotes
CONFLICT OF INTEREST
The authors are unaware of any conflicts of interest.
Funding: Supported in part by Health Workforce Australia (HWA).
Contributor Information
Jasmina Fejzic, School of Pharmacy, University of Queensland. Brisbane (Australia). j.fejzic@uq.edu.au [at the time of the study: School of Pharmacy, Griffith University].
Michelle Barker, Department of International Business and Asian Studies, Griffith Business School. Brisbane (Australia). m.barker@griffith.edu.au.
References
- 1.Wallman A, Vaudan C, Sporrong S. Communications training in pharmacy education, 1995-2010. Am J Pharm Educ. 2013;77(2):583. doi: 10.5688/ajpe77236. doi:10.5688/ajpe77236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canberra: Pharmaceutical Society of Australia (PSA); 2010. Pharmaceutical Society of Australia. National Competency Standards Framework for Pharmacists in Australia. [Google Scholar]
- 3.Coelho RB, Costa FA. Impact of pharmaceutical counseling in minor health problems in rural Portugal. Pharm Pract (Granada) 2014;12(4):583. doi: 10.4321/s1886-36552014000400002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussainy SY, Styles K, Duncan G. A virtual practice environment to develop communication skills in pharmacy students. Am J Pharm Educ. 2012;76(10):583. doi: 10.5688/ajpe7610202. doi:10.5688/ajpe7610202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rickles NM, Tieu P, Myers L, Galal S, Chung V. The impact of a standardized patient program on student learning of communication skills. Am J Pharm Educ. 2009 Feb 19;73(1):583. doi: 10.5688/aj730104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weller JM, Nestel D, Marshall SD, Brooks PM, Conn JJ. Simulation in clinical teaching and learning. Med J Aust. 2012;196(9):594. doi: 10.5694/mja10.11474. [DOI] [PubMed] [Google Scholar]
- 7.Smithburger PL, Kane-Gill SL, Kloet MA, Lohr B, Seybert AL. Advancing interprofessional education through the use of high fidelity human patient simulators. Pharm Pract (Granada) 2013;11(2):61–65. doi: 10.4321/s1886-36552013000200001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutton B, Bearman M, Jolly B, Nestel D, Brookes P, Flanagan B, Watson M, McMenamin C. Simulated Learning Environments Medical Curriculum Report. Health Workforce Australia. 2010 [Google Scholar]
- 9.Fejzic J, Henderson AJ, Smith NA, Mey A. Community pharmacy experiential placement: Comparison of preceptor and student perspectives in an Australian postgraduate pharmacy programme. Pharm Educ. 2013;13(1):15–21. [Google Scholar]
- 10.Kubota Y, Yano Y, Seki S, Takada K, Sakuma M, Morimoto T, Akaike A, Hiraide A. Assessment of pharmacy students’ communication competence using the Roter Interaction Analysis System during objective structured clinical examinations. Am J Pharm Educ. 2011;75(3):583. doi: 10.5688/ajpe75343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Legal M, Billingsley M, Carriere F, Zed P, Loewen P. Advancing experiential learning in institutional pharmacy practice: The University of British Columbia’s AGILE Project. UBC Pharmaceutical Sciences Student Journal. 2013;1(2) [Google Scholar]
- 12.Stupans I, March G, Owen SM. Enhancing learning in clinical placements: reflective practice, self-assessment, rubrics and scaffolding. Assess Eval High Educ. 2013;38(5):507–519. [Google Scholar]
- 13.Mak A, Kennedy M. Internationalising the student experience: preparing instructors to embed intercultural skills in the curriculum. Innov High Educ. 2012;37(4):323–334. [Google Scholar]
- 14.Barker M, Mak A. From classroom to boardroom and ward developing generic intercultural skills in diverse disciplines. J Stud Int Educ. 2013;17(5):573–589. [Google Scholar]
- 15.Caruana V, Ploner J. A critical review of contemporary practice and educational research in internationalization within the business education subject communities. The Higher Education Academy. 2012 [Google Scholar]
- 16.Mak A, Westwood M, Barker M, Ishiyama FI. Developing sociocultural competencies for success among international students: The ExcelL programme. J Int Educ. 1998;9(1):33–38. [Google Scholar]
- 17.Maganlal S, Hills R, McMillan S, Barker M, Blauberg N, Shallcross L. Volume 35. Enhancing intercultural competence among pharmacy students through the EXCELL program. In: Brown N, Jones SM, Adam A, editors. Research and Development in Higher Education: Connections in Higher Education. Milperra: HERDSA; 2012. ISBNp 0-908557-89-2. [Google Scholar]
- 18.Mak AS, Westwood MJ, Ishiyama FI, Barker MC. Optimising conditions for learning sociocultural competencies for success. Int J Intercult Relat. 1999;23(1):77–90. [Google Scholar]
- 19.Woods P, Barker M, Daly A. Teaching intercultural skills in the multicultural classroom. 4th Annual Hawaii International Conference on Business. Honolulu. 2004 [Google Scholar]
- 20.Coombes I, Avent M, Cardiff L, Bettenay K, Coombes J, Whitfield K, Stokes J, Davies G, Bates I. Improvement in pharmacist’s performance facilitated by an adapted competency-based general level framework. J Pharm Pract Res. 2010;40(2):111–118. [Google Scholar]
- 21.Given LM. The Sage encyclopedia of qualitative research methods: Sage Publications. 2008 [Google Scholar]
- 22.Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory: Sage. 2008 [Google Scholar]
- 23.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook: SAGE Publications. 1994 [Google Scholar]
- 24.Blom L, Wolters M, Ten Hoor-Suykerbuyk M, van Paassen J, van Oyen A. Pharmaceutical education in patient counseling:20h spread over 6 years? Patient Educ Couns. 2011;83(3):465–471. doi: 10.1016/j.pec.2011.05.018. doi:10.1016/j.pec.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 25.Branch C. Pharmacy students’ learning and satisfaction with high-fidelity simulation to teach drug-induced dyspepsia. Am J Pharm Educ. 2013;77(2):583. doi: 10.5688/ajpe77230. doi:10.5688/ajpe77230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crea KA. Practice skill development through the use of human patient simulation. Am J Pharm Educ. 2011;75(9):583. doi: 10.5688/ajpe759188. doi:10.5688/ajpe759188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seybert AL, Kobulinsky LR, McKaveney TP. Human Patient Simulation in a Pharmacotherapy Course. Am J Pharm Educ. 2008;72(2):583. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noble C, Coombes I, Shaw PN, Nissen LM, Clavarino A. Becoming a pharmacist: the role of curriculum in professional identity formation. Pharm Pract (Granada) 2014;12(1):583. doi: 10.4321/s1886-36552014000100007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Droege M, Assa-Eley MT. Pharmacists as care providers: Personal attributes of recent pharmacy graduates. Am J Pharm Educ. 2005;65(3):290–295. [Google Scholar]
- 30.Hassali MA, Shafie AA, Al-Haddad MS, Abduelkarem AR, Ibrahim MI, Palaian S, Abrika OS. Social pharmacy as a field of study: the needs and challenges in global pharmacy education. Res Social Adm Pharm. 2011;7(4):415–420. doi: 10.1016/j.sapharm.2010.10.003. doi:10.1016/j.sapharm.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Marriott JL, Nation RL, Roller L, Costelloe M, Galbraith K, Stewart P, Charman WN. Pharmacy education in the context of Australian practice. Am J Pharm Educ. 2008;72(6):583. doi: 10.5688/aj7206131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tofade T. Coaching younger practitioners and students using components of the co-active coaching model. Am J Pharm Educ. 2010;74(3):583. doi: 10.5688/aj740351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chisholm MA, Cobb H, Duke L, McDuffie C, Kennedy WK. Development of an instrument to measure professionalism. Am J Pharm Educ. 2006;70(4):583. doi: 10.5688/aj700485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kairuz T, Noble C, Shaw J. Preceptors, interns, and newly registered pharmacists’ perceptions of new zealand pharmacy graduates’ preparedness to practice. Am J Pharm Educ. 2010;74(6):583. doi: 10.5688/aj7406108. [DOI] [PMC free article] [PubMed] [Google Scholar]


