Abstract
Background
Demand for England’s accident and emergency (A&E) services is increasing and is particularly concentrated in areas of high deprivation. The extent to which primary care services, relative to population characteristics, can impact on A&E is not fully understood.
Aim
To conduct a detailed analysis to identify population and primary care characteristics associated with A&E attendance rates, particularly those that may be amenable to change by primary care services.
Design and setting
This study used a cross-sectional population-based design. The setting was general practices in England, in the year 2011–2012.
Method
Multivariate linear regression analysis was used to create a model to explain the variability in practice A&E attendance rates. Predictor variables included population demographics, practice characteristics, and measures of patient experiences of primary care.
Results
The strongest predictor of general practice A&E attendance rates was social deprivation: the Index of Multiple Deprivation (IMD-2010) (β = 0.3. B = 1.4 [95% CI =1.3 to 1.6]), followed by population morbidity (GPPS responders reporting a long-standing health condition) (β = 0.2, B = 231.5 [95% CI = 202.1 to 260.8]), and knowledge of how to contact an out-of-hours GP (GPPS question 36) (β = −0.2, B = −128.7 [95% CI =149.3 to −108.2]). Other significant predictors included the practice list size (β = −0.1, B = −0.002 [95% CI = −0.003 to −0.002]) and the proportion of patients aged 0–4 years (β = 0.1, B = 547.3 [95% CI = 418.6 to 676.0]). The final model explained 34.4% of the variation in A&E attendance rates, mostly due to factors that could not be modified by primary care services.
Conclusion
Demographic characteristics were the strongest predictors of A&E attendance rates. Primary care variables that may be amenable to change only made a small contribution to higher A&E attendance rates.
Keywords: accident and emergency department, general practice, primary health care, socioeconomic factors
INTRODUCTION
High demand for accident and emergency (A&E) services is an issue of current importance in England because of the rapidly increasing use of A&E and the high cost of these services.1 National and local studies have found high demand for A&E to be concentrated in areas with greater socioeconomic deprivation,2–7 which may reflect a greater healthcare need, a lack of understanding of appropriate services, or a relative lack of primary care services in these areas (the inverse care law).8 National studies have found other important sociodemographic influences on A&E attendance rates including the level of population morbidity,6 younger populations,9 and older populations.6 Studies conducted at a local level have found older populations2 and ethnicity10–13 to be important influences on A&E attendance rates.
Although general practice factors are less powerful determinants of A&E use, national patient surveys have demonstrated an association with access to a GP.6,14 Local-level studies have found that the ability to see a preferred GP15 and satisfaction at being able to speak to a GP by telephone12 are predictors of A&E attendance rates, although Harris et al found that access to primary care did not explain variation in A&E rates.7 General practice standards of care, as evidenced by the national Quality and Outcomes Framework (QOF)16 score, do not appear to influence A&E attendance rates.12
This study aimed to determine the strength of relationship between all types of A&E attendance and characteristics of both populations and primary care. Its purpose was to identify possible factors within the control of primary care, and hence potentially open to change, which were associated with high A&E attendance rates. Development of a general practice-based dataset allowed simultaneous consideration of patient and primary care characteristics with measures of patient experiences of primary care.
METHOD
This study used a cross-sectional population-based design. The setting was general practices in England, in the year 2011–2012. All data were available at practice level.
Variables
The outcome variable was the crude rate of all A&E attendances, at all types of A&E department per 1000 population.17 Predictor variables were either measures of population demographics including deprivation,18 population morbidity,19 ethnic group, and age (Health and Social Care Information Centre, unpublished data, 2013), or measures of primary care including QOF score,16 practice characteristics,19,20 and measures of patient experiences of primary care derived from the General Practice Patient Survey (GPPS).19 The dataset was constructed using data from the Health and Social Care Information Centre and population data derived from the 2011 Census recorded at lower super output area to link with practice, rather than patient, postcodes. The Index of Multiple Deprivation (IMD-2010) score associated with the general practice postcode was used as a proxy for the level of deprivation experienced by the practice population.18
How this fits in
Population characteristics such as social deprivation are known to predict high use of accident and emergency (A&E) departments. As such, A&E attendance rates are in large part determined by the characteristics of the registered population of each general practice. In this detailed analysis of population, general practice, and patient survey data, the extent to which general practice factors can moderate that relationship is determined. The study aimed to identify variables within the control of primary care, and hence potentially open to change, which are associated with A&E attendance rates.
The GPPS was distributed to 2.7 million adults registered with a GP between January and September 2012, of whom 982 999 (36%) responded. Of the 58 questions in the survey, five were selected for inclusion (Box 1). Four were selected on the basis of being likely to relate to A&E rates and potentially amenable to change by primary care (primary care variables). The fifth, relating to the presence of long-term conditions, was included as a population characteristic. The dataset contained records from the 8123 general practices that submitted QOF data in 2011–2012. Practices with a total list size of <750 or a list size per full-time equivalent (FTE) GP of <500 were removed following a previously used methodology.21 Practices with missing A&E attendance data were also removed.
Box 1. General Practice Patient Survey (GPPS) variables included in analysis.
| GPPS question number | Question | Definition of positive response a |
|---|---|---|
| 3 | Generally, how easy is it to get through to someone at your GP surgery on the phone? | Proportion of responders answering ‘very easy’ or ‘fairly easy’ |
| 12 | Last time you wanted to see or speak to a GP or nurse from your GP surgery were you able to get an appointment to see or speak to someone? | Proportion of responders answering ‘yes’ or ‘yes, but I had to call back closer to, or on the day I wanted the appointment’ |
| 30 | Do you have a long-standing health condition? | Proportion of responders answering ‘yes’ |
| 33 | How confident are you that you can manage your own health? (very, fairly, not very, not at all confident) | Proportion of responders answering ‘very confident’ or ‘fairly confident’ |
| 36 | Do you know how to contact an out-of-hours GP service when the surgery is closed? | Proportion of responders answering ‘yes’ |
All responses were weighted to adjust for non-response bias.
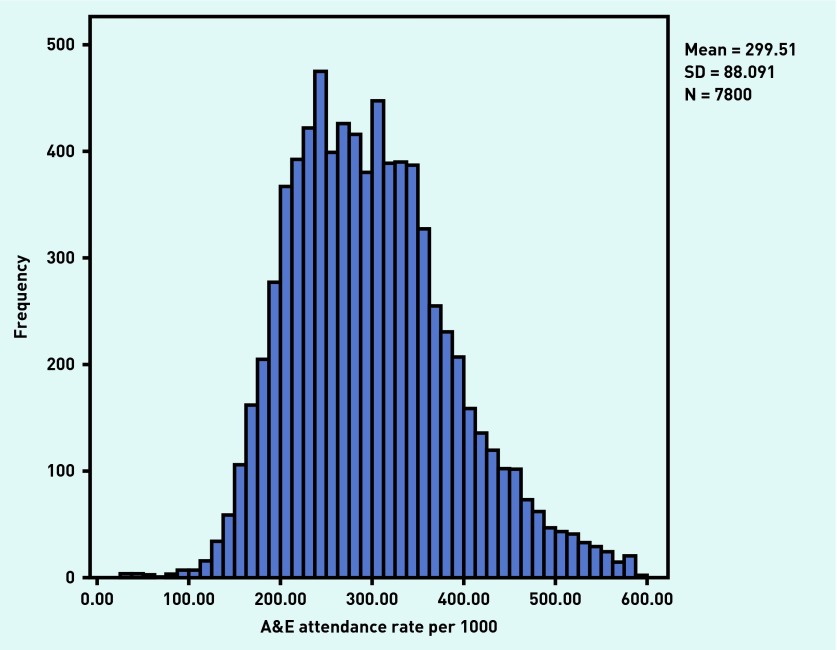
A test for normality revealed slight positive skewness in the distribution of A&E attendance rates. Practices with extremely high A&E rates may be atypical because of their setting or population. For example, practices co-located with an A&E department6,12,22 or with a high proportion of registered homeless individuals23,24 may be expected to have unusually high A&E rates. Including these practices in analysis carries a risk of them exerting an undue effect on study results. By removing the 2% of practices with the highest A&E attendance rates, the dependent variable became more normally distributed (Figure 1). As almost all practices in England were included, and based on the premise that large samples of independent variables will be approximately normally distributed, parametric methods were used to analyse the data.25 Afterwards, t-tests were performed to measure any differences between the included and excluded practices. Missing values for IMD score occurred in 4.2% of practices. All other variables used in multivariate analysis had less than 0.05% missing values.
Figure 1.
Distribution of final dataset general practice A&E attendance rates per 1000 registered population.
Statistical methods
All analyses were performed using SPSS (versions 20 & 22). The assumptions of a linear regression model were tested by visual inspection of scatter plots of the relations between each predictor and outcome, demonstrating linear relationships. Univariate analysis followed by multivariate linear regressions were used to create a model to explain the variability in practice A&E attendance rates. Potential variables were included in the regression model if P≤0.2 on univariate analysis to avoid omitting potentially significant predictor variables. To demonstrate the extent to which variables within the control of primary care (based on GPPS responses, n = 4) contributed to this explanatory model, these variables were temporarily omitted from the model, and the effect on the overall predictive ability of the model was observed.
Predictor variables were considered significant if P<0.01 to account for multiple testing.26 Variables were excluded if the tolerance statistic for multicollinearity (1-R2) was <0.2.
Sensitivity analysis
Given that previous studies of A&E use by age have been inconclusive,2,9,24,27,28 a wider range of age cohorts was used, repeating the analysis using three cut-off points: 65, 75, and 85 years.
RESULTS
The initial dataset consisted of records from 8123 practices. Practices were excluded because of small list size (n = 163), missing A&E attendance data (n = 1), and atypically high A&E attendance rates (n = 159). The final sample consisted of 7800 practices (96.0% of all practices in England). All further analysis was conducted on this sample. Excluded practices had significantly smaller mean list sizes, lower mean QOF scores, and higher mean IMD scores.
Table 1 describes the main characteristics of general practices included in this study, their registered populations, and responses to selected GPPS questions.
Table 1.
Characteristics of general practices and their populations in England, 2011–2012 (n = 7800)
| Mean | SD | 10th centile | 90th centile | |
|---|---|---|---|---|
| Practice A&E attendance rate, per 1000 population | 299.5 | 88.1 | 25.8 | 587.5 |
| Total QOF points | 971.7 | 39.9 | 929.7 | 998.0 |
| Practice list size | 6980 | 4244 | 2392 | 12 520 |
| List size per FTE GP | 1839 | 1256 | 1074 | 2635 |
| IMD score | 25.8 | 17.0 | 7.2 | 51.3 |
| Black/black British, % | 4.2 | 7.4 | 0.1 | 12.3 |
| Asian/Asian British, % | 10.2 | 16.3 | 0.5 | 28.4 |
| White ethnicity, % | 81.8 | 22.3 | 46.3 | 98.4 |
| Age 0–4 years, % | 6.1 | 1.8 | 4.2 | 8.4 |
| Age ≥65 years, % | 16.1 | 6.1 | 7.9 | 23.6 |
| GPPS Q3: Patients finding it easy to contact surgery by phone, % | 80.8 | 14.1 | 60.7 | 95.7 |
| GPPS Q12: Patients able to get an appointment at last attempt, % | 88.9 | 6.2 | 80.7 | 95.8 |
| GPPS Q30: Patients with a long-standing health condition, % | 61.9 | 7.1 | 52.9 | 70.7 |
| GPPS Q33: Patients confident in managing own health, % | 92.3 | 3.8 | 87.2 | 96.5 |
| GPPS Q36: Patients knowing how to contact an out-of-hours service, % | 61.7 | 10.1 | 48.0 | 73.6 |
A&E = accident and emergency. FTE = full-time equivalent. GPPS = General Practice Patient Survey. IMD = Index of Multiple Deprivation. QOF = Quality and Outcomes Framework. SD = standard deviation.
Multiple linear regression
The final model (Table 2) explained 34.4% of the variation in A&E attendance rates between general practices in England in 2011–2012.
Table 2.
Multivariate predictors of practice A&E attendance rates in England, 2011–2012
| Variable | Regression coefficient, B (95% CI) | Standardised regression coefficient, β | P-value |
|---|---|---|---|
| IMD score | 1.4 (1.3, 1.6) | 0.28 | <0.001 |
| GPPS responders with a long-standing health condition (proportion) | 231.5 (202.1 to 260.8) | 0.18 | <0.001 |
| GPPS responders who know how to contact an out-of-hours GP (proportion) | −128.7 (−149.3 to −108.2) | −0.15 | <0.001 |
| Practice list size | −0.002 (−0.0003 to −0.002) | −0.12 | <0.001 |
| Patients aged 0–4 years (proportion) | 547.3 (418.6 to 676.0) | 0.10 | <0.001 |
| GPPS responders confident in managing own health (proportion) | −212.3 (−268.6 to −156.0) | −0.09 | <0.001 |
| Population black or black British (proportion) | 88.7 (61.6 to 115.8) | 0.07 | <0.001 |
| GPPS responders able to get an appointment to see or speak to someone (proportion) | −101.2 (−140.8 to −61.49) | −0.07 | <0.001 |
| Population Asian or Asian British (proportion) | −37.4 (−49.9 to −25.9) | −0.07 | <0.001 |
| GPPS responders easy to get through to the surgery on the phone (proportion) | −19.4 (−35.4 to −3.3) | −0.03 | 0.018 |
| Total patients aged ≥65 years (proportion) | −43.0 (−88.5 to 2.4) | −0.03 | 0.063 |
| List size per FTE GP | −0.002 (−0.003 to 0.000) | −0.02 | 0.024 |
| Total QOF score | −0.2 (−0.06 to 0.02) | −0.01 | 0.386 |
FTE = full-time equivalent. GPPS = General Practice Patient Survey. IMD = Index of Multiple Deprivation. QOF = Quality and Outcomes Framework.
Population factors were the most important predictors of A&E attendance rates (highest values for the regression coefficient, β). Deprivation was the most important predictor, followed by the proportion of the population with a long-term health condition. Four primary care variables (knowledge of how to contact an out-of-hours GP, practice list size, patient confidence in managing own health, and ability to get an appointment) were also predictors of A&E attendance rates. More positive responses to these four questions were associated with lower A&E attendance rates.
Temporarily removing the four GPPS primary care variables reduced the explanatory power of the model by 3.3%.
Collinearity tolerance values revealed no evidence that collinearity was acting to distort the findings. Sensitivity analysis found that the model was not sensitive to change in the three older adults’ age groups.
DISCUSSION
Summary
Several factors that predict A&E attendance were identified, the most powerful of which was deprivation, followed by the proportion of the population with a long-standing health condition.
Primary care characteristics associated with A&E use were: patient knowledge of how to contact an out-of-hours GP; practice list size; patient confidence in managing their own health; and ability to get an appointment, although the total contribution of these variables to the overall predictive power of the model was small.
Strengths and limitations
This study was based on data from almost all general practices across England in 2011–2012, making its findings directly generalisable across England, and providing sufficient power to detect true associations. The study considered in a single analysis several characteristics of the population (including deprivation, ethnic group, and age); of general practice; and of patient experience of primary care, enabling identification of important primary care variables relative to population characteristics. Highly atypical practices that may have skewed the study results were excluded before analysis.
A&E attendances by individuals with no registered GP could not be included within this study, creating a potential bias. Furthermore, this study included all types of A&E attendance, some of which would have been unrelated to primary care services, for example, traffic or sports injuries, potentially weakening any observed association.
List inflation29 may have acted as a source of bias given that practices in deprived areas may be more likely to have inflated list sizes.30 This may have reduced the strength of the observed association between deprivation and A&E attendances. A&E attendance data are derived from Hospital Episode Statistics, and are incomplete, recording fewer attendances than the Department of Health Weekly A&E situation reports (17.6 million attendances and 21.5 million, respectively).1
This study used the IMD score associated with the practice postcode as a proxy for population deprivation. Although this has been shown to be a valid proxy, it may underestimate the effect of deprivation.31 Ethnicity analysis was based on broad ethnic categories, possibly masking differences in A&E use between ethnic sub-groups. A limitation of the GPPS is its low response rate (36% in 2012), although studies have shown it to be a valid measure of access32 and reliable in measuring specific performance measures,33 with a weighting scheme that adjusts for bias resulting from low response rates.19 It was not possible to include the effect of distance to A&E in this study, which has been found to be important in some previous research,4,6,12,15 but not others.28,34 A possible residual confounding factor is the familiarity of the practice population with the organisation of the NHS, likely to be a factor of how long the patients have lived in the UK and which may explain some of the association between A&E attendance and ethnicity. Finally, as with all cross-sectional observational studies, the associations observed can be used to generate hypotheses but cannot demonstrate causality nor explain any observed associations.
Comparison with existing literature
Population characteristics were found to be the strongest predictors of A&E attendance, particularly deprivation, as has been found in many previous studies.9,12,34,35 The proportion of the population with a long-standing health condition was also an important predictor of A&E attendances, in agreement with the findings of Shah and Cook.9 Practices at which patients felt more confident in managing their own health had lower A&E attendances, supporting the finding that psychological components such as anxiety or worry contribute to patient decisions to attend A&E.10,29,36
The present results confirm the finding of Cowling et al, that people able to get an appointment to see or speak to a doctor or nurse were less likely to attend A&E.6 In addition, other primary care factors, not considered within that study, were found to be associated with A&E rates, namely knowledge of how to contact out-of-hours GPs, ease of getting through to the surgery by phone, and patient confidence in managing health.
In this study, the population proportion of young children (<5 years), was associated with A&E rates, as found in some other studies,9,28 but the population proportion of older adults (>65, >75, or >85 years) had no significant association. This contrasts with the findings of some studies,24 but supports others.9,28
The present study found that the two included ethnic groups were associated with opposite effects on A&E attendance: higher proportions of Asian or Asian British patients were associated with lower A&E attendance rates whereas higher proportions of black or black British patients were associated with higher rates. Earlier studies had shown that white groups used A&E more than those from non-white backgrounds,11–13 although the studies were based on relatively small geographical areas with high proportions of particular non-white ethnic groups and therefore with limited generalisability to other areas of the UK. A recent national study found that the proportion of the population of white ethnicity was not a significant predictor of A&E use;6 however, this study did not include measures of any non-white ethnic groups.
Characteristics of primary care that may be amenable to change were of particular interest as they can be used to generate hypotheses about interventions to reduce A&E attendances. It was found that the proportion of the population who knew how to contact an out-of-hours GP was a significant predictor of practice A&E attendance rates. Similarly, in a qualitative study, Rajpar et al found that 11/54 A&E attendees (20.4%) were unaware of the arrangement for out-of-hours services locally.13
Practice list size was negatively associated with A&E attendances in this study, in agreement with the findings of Baker et al,12 although the list size per FTE GP was not a significant predictor, as found by Cowling et al.6 This suggests that the relationship between practice size and A&E rates may be related to the organisation and management of larger practices, rather than the ratio of GPs to patients.
Cowling et al 6 investigated predictors of ‘self-referred discharged A&E attendances’. Studies confined to ‘self-referrals’ may include many patients attending A&E on the advice of healthcare professionals, including those attending for primary care reasons.28,37 Although discharged attendances are more likely to refer to patients who could have been managed in primary care, this study sought to determine the extent to which primary care could influence total A&E demand, relative to population variables.
Implications for research
Although much of the variation in A&E attendance rate is determined by factors outside the control of primary care such as deprivation, age, and ethnic group, several factors have been identified that are independently related to A&E attendance rates and that might be amenable to change. In addition to the findings of Cowling et al,6 showing that accessibility to GPs reduced the likelihood of A&E attendance, other factors were found that might contribute to reductions in A&E attendance through patient support and education. In particular, 38% of patients did not know how to contact an out-of-hours GP service, indicating scope for increasing awareness in practice populations. Although patient confidence in managing their health was also a significant predictor, mean values above 90% for this attribute make it unlikely that substantial further improvements could be achieved.
Interventions to improve access to primary care may be most effectively targeted towards families of young children, given the age profile of practices with higher A&E rates, although the impact on total A&E attendances may be relatively small. In 2012–2013, 10% of all A&E attendances (1.8 million attendances) were for children aged <5.38
Further research into the organisational attributes that contribute to reduced A&E attendance rates are needed. The association between lower attendance rates and larger practice size may, for example, be related to higher levels of managerial capacity in larger practices. Finally, further research is required to explore the differential use of A&E by ethnic group, including more detailed analysis of ethnic group and possibly language and cultural background.
This cross-sectional analysis of general practices in England aimed at identifying population and primary care characteristics associated with A&E attendance rates, particularly those that may be amenable to change by primary care services. Multivariable linear regression produced a model that explained 34.4% of the variation in A&E attendances. Deprivation and population morbidity were the two most important predictors of A&E rates. Patient knowledge of how to contact an out-of-hours GP was also important, although modifiable primary care variables contributed relatively little to the total predictive power of the model.
Acknowledgments
None.
Funding
This research was completed in partial fulfilment of the requirements for the degree of Master of Public Health at King’s College London, funded by NHS Health Education South London. The research was funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
Ethical approval
Ethical approval was not required for this study, as it was an audit of publicly available anonymised healthcare data.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Health & Social Care Information Centre Hospital episode statistics: accident and emergency attendances in England (experimental statistics) 2011–12. Summary Report. http://www.hscic.gov.uk/catalogue/PUB09624/acci-emer-atte-eng-2011-12-rep.pdf (accessed 24 Aug 2015)
- 2.Bankart MJG, Baker R, Rashid A, et al. Characteristics of general practices associated with emergency admission rates to hospital: a cross-sectional study. Emerg Med J. 2011;28(7):558–563. doi: 10.1136/emj.2010.108548. [DOI] [PubMed] [Google Scholar]
- 3.Blatchford O, Capewell S, Murray S, Blatchford M. Emergency medical admissions in Glasgow: general practices vary despite adjustment for age, sex, and deprivation. Br J Gen Pract. 1999;49(444):551–554. [PMC free article] [PubMed] [Google Scholar]
- 4.McKee CM, Gleadhill DN, Watson JD. Accident and emergency attendance rates: variation among patients from different general practices. Br J Gen Pract. 1990;40(333):150–153. [PMC free article] [PubMed] [Google Scholar]
- 5.Majeed A, Bardsley M, Morgan D, et al. Cross sectional study of primary care groups in London: association of measures of socioeconomic and health status with hospital admission rates. BMJ. 2000;321(7268):1057–1060. doi: 10.1136/bmj.321.7268.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowling TE, Cecil EV, Soljak MA, et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PloS One. 2013 doi: 10.1371/journal.pone.0066699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris MJ, Patel B, Bowen S. Primary care access and its relationship with emergency department utilisation: an observational, cross-sectional, ecological study. Br J Gen Pract. 2011 doi: 10.3399/bjgp11X613124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hart JT. The inverse care law. Lancet. 1971;1(7696):405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 9.Shah SM, Cook DG. Socio-economic determinants of casualty and NHS Direct use. J Public Health (Oxf) 2008;30(1):75–81. doi: 10.1093/pubmed/fdn001. [DOI] [PubMed] [Google Scholar]
- 10.Forbes L, Harvey S, Newson R, et al. Risk factors for accident and emergency (A&E) attendance for asthma in inner city children. Thorax. 2007;62(10):855–860. doi: 10.1136/thx.2006.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hull S, Jones IR, Moser K, Fisher J. The use and overlap of AED and general practice services by patients registered at two inner London general practices. Br J Gen Pract. 1998;48(434):1575–1579. [PMC free article] [PubMed] [Google Scholar]
- 12.Baker R, Bankart MJ, Rashid A, et al. Characteristics of general practices associated with emergency-department attendance rates: a cross-sectional study. BMJ Qual Saf. 2011;20(11):953–958. doi: 10.1136/bmjqs.2010.050864. [DOI] [PubMed] [Google Scholar]
- 13.Rajpar SF, Smith MA, Cooke MW. Study of choice between accident and emergency departments and general practice centres for out of hours primary care problems. J Accid Emerg Med. 2000;17(1):18–21. doi: 10.1136/emj.17.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowling TE, Harris MJ, Watt HC, et al. Access to general practice and visits to accident and emergency departments in England: cross-sectional analysis of a national patient survey. Br J Gen Pract. 2014 doi: 10.3399/bjgp14X680533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunther S, Taub N, Rogers S, Baker R. What aspects of primary care predict emergency admission rates? A cross sectional study. BMC Health Serv Res. 2013;13:11. doi: 10.1186/1472-6963-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Information Centre for Health and Social Care Quality and Outcomes Framework, achievement, prevalence and exceptions data, 2011/2012. http://www.hscic.gov.uk/catalogue/PUB08135/qof-11-12-rep.pdf (accessed 24 Aug 2015)
- 17.Health & Social Care Information Centre NHS comparators. 2012. https://www.nhscomparators.nhs.uk/NHSComparators/Login.aspx (accessed 14 Aug 2015)
- 18.GOV.UK English Indices of Deprivation 2010. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 24 Aug 2015)
- 19.NHS England GP Patient Survey. December 2012. Survey fieldwork dates and materials. https://gp-patient.co.uk/surveys-and-reports#december-2012 (accessed 7 Sep 2015)
- 20.Health & Social Care Information Centre General and Personal Medical Services, England 2002–2012 as at 30 September. 2013. http://www.hscic.gov.uk/catalogue/PUB09536/nhs-staf-2002-2012-gene-prac-rep.pdf (accessed 24 Aug 2015)
- 21.Murray J, Young J, Forster A, et al. Feasibility study of a primary care-based model for stroke aftercare. Br J Gen Pract. 2006;56(531):775–780. [PMC free article] [PubMed] [Google Scholar]
- 22.Cooke M, Fisher J, Dale J, et al. Reducing attendances and waits in emergency departments: a systematic review of present innovations. London: National Co-ordinating Centre for NHS Service Delivery; 2004. http://wrap.warwick.ac.uk/134/ (accessed 24 Aug 2015) [Google Scholar]
- 23.Little GF, Watson DP. The homeless in the emergency department: a patient profile. J Accid Emerg Med. 1996;13(6):415–417. doi: 10.1136/emj.13.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sempere-Selva T, Peiró S, Sendra-Pina P, et al. Inappropriate use of an accident and emergency department: magnitude, associated factors, and reasons — an approach with explicit criteria. Ann Emerg Med. 2001;37(6):568–579. doi: 10.1067/mem.2001.113464. [DOI] [PubMed] [Google Scholar]
- 25.Ashworth M, Seed P, Armstrong D, et al. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract. 2007;57(539):441–448. [PMC free article] [PubMed] [Google Scholar]
- 26.Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310(6973):170. doi: 10.1136/bmj.310.6973.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev. 2011;68(2):131–155. doi: 10.1177/1077558710379422. [DOI] [PubMed] [Google Scholar]
- 28.Hendry SJ, Beattie TF, Heaney D. Minor illness and injury: factors influencing attendance at a paediatric accident and emergency department. Arch Dis Child. 2005;90(6):629–633. doi: 10.1136/adc.2004.049502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health & Social Care Information Centre Attribution data set GP-registered populations scaled to ONS population estimates — 2011. http://www.hscic.gov.uk/searchcatalogue?productid=4710&q=title%3a%22Attribution+data+set+GP-registered+populations%22&sort=Relevance&size=10&page=1#top (accessed 24 Aug 2015)
- 30.Ashworth M, Jenkins M, Burgess K, et al. Which general practices have higher list inflation? An exploratory study. Fam Pract. 2005;22(5):529–531. doi: 10.1093/fampra/cmi057. [DOI] [PubMed] [Google Scholar]
- 31.Strong M, Maheswaran R, Pearson T. A comparison of methods for calculating general practice level socioeconomic deprivation. Int J Health Geogr. 2006;5:29. doi: 10.1186/1476-072X-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Campbell JL, Carter M, Davey A, et al. Accessing primary care: a simulated patient study. Br J Gen Pract. 2013 doi: 10.3399/bjgp13X664216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roland M, Elliott M, Lyratzopoulos G, et al. Reliability of patient responses in pay for performance schemes: analysis of national General Practitioner Patient Survey data in England. BMJ. 2009 doi: 10.1136/bmj.b3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carlisle R, Groom LM, Avery AJ, et al. Relation of out of hours activity by general practice and accident and emergency services with deprivation in Nottingham: longitudinal survey. BMJ. 1998;316(7130):520–523. doi: 10.1136/bmj.316.7130.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hull SA, Jones IR, Moser K. Factors influencing the attendance rate at accident and emergency departments in East London: the contributions of practice organization, population characteristics and distance. J Health Serv Res Policy. 1997;2(1):6–13. doi: 10.1177/135581969700200104. [DOI] [PubMed] [Google Scholar]
- 36.Hansagi H, Olsson M, Sjöberg S, et al. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001;37(6):561–567. doi: 10.1067/mem.2001.111762. [DOI] [PubMed] [Google Scholar]
- 37.Davison AG, Hildrey AC, Floyer MA. Use and misuse of an accident and emergency department in the East End of London. J R Soc Med. 1983;76(1):37–40. [PMC free article] [PubMed] [Google Scholar]
- 38.Health & Social Care Information Centre Accident and emergency attendances in England — 2012–13. http://www.hscic.gov.uk/catalogue/PUB13464 (accessed 24 Aug 2015)