Abstract
Obesity has been characterized as a disease. Strategies to change the incidence and prevalence of this disease include a focus on changing physical and social environments, over and above individual-level strategies, using a multilevel or systems approach. We focus our attention on evidence published between 2008 and 2013 on the effectiveness of interventions in nutrition environments, i.e., environmental interventions designed to influence the intake of healthful foods and amount of energy consumed. An overarching socioecological framework that has guided much of this research was used to characterize different types of environmental strategies. Intervention examples in each area of the framework are provided with a discussion of key findings and related conceptual and methodological issues. The emphasis in this review is on adults, but clearly this literature is only one part of the picture. Much research has been focused on child-specific interventions, including environmental interventions. Some evidence suggests effectiveness of policy-based or other types of interventions that aim to regulate or restructure environments to promote healthy dietary choices, and these strategies would apply to both children and adults. Opportunities to evaluate these policy changes in adults’ social and physical environments are rare. Much of the existing research has been with children. As conceptual and methodological issues continue to be identified and resolved, we hope that future research in this domain will identify environmental strategies that can be included in intervention toolboxes to build healthy nutrition environments for both adults and children.
Keywords: environment, conceptual review, organizations, consumer, nutrition diet policy
INTRODUCTION
Obesity continues to be a major public health problem affecting ~33% of adults and 20% of children in the United States (22). Obesity is significantly more prevalent within racial and ethnic minority subgroups than among whites (22), and differences in dietary and physical activity behaviors likely underpin these disparities (23, 56). The adjective “obesogenic” has been used to describe environments that promote obesity either through increased energy intake or decreased energy expenditure (66). Obesogenic nutrition environments are spatially patterned such that they co-occur in areas with larger proportions of low-income and minority populations (4, 64, 88) and may thus contribute to socioeconomic and racial disparities in obesity (10, 64, 82). Relying solely on individual-level strategies to change dietary intake and physical activity is not sufficient. Creating supportive environments for behavior change is also needed, including the evaluation of interrelations between individual and environmental factors to drive a more dynamic and comprehensive approach to obesity prevention (4, 64, 69, 82). A multisectoral, systems-oriented approach is recommended in the 2012 Institute of Medicine (IOM) report on accelerating progress in obesity prevention (56).
This review focuses on environments that affect dietary quality and energy intake (i.e., nutrition environments). Efforts to change nutrition environments are key to preventing obesity in both adults and children. That this review focuses specifically on adults is important because of both their increased risk of obesity-related chronic diseases and the key role adults play in determining the types and preparation of foods brought into the home (56, 83). Several reviews based on observational studies have noted associations between nutrition environments and adults’ dietary intake (56, 83). Interventions that employ strategies designed to change nutrition environments offer an opportunity to assess causal relationships between the changes effected and the eating patterns of people who are exposed to these environments. The purpose of this review is to examine the process and outcomes of nutrition environment interventions that have been conducted since the previous review (88) and to identify future directions.
LITERATURE REVIEW
An initial list of references was generated from an electronic search of citations within PubMed and Web of Science articles published between 2008 [the year that nutrition environment approaches were proposed by Story and colleagues (88)] and June 2013. Key search terms used were policy, intervention, neighborhood, environment, nutrition, food, and diet. Titles and abstracts of identified articles were screened to ensure that the study evaluated (a) a policy or environmental intervention strategy and (b) a dietary outcome or related intermediate outcome (e.g., milk sales) for an adult population (aged 18+ years). References cited in identified papers were also screened using the same criteria to identify eligible published articles captured in the electronic search. Finally, Web pages hosted by organizations leading change in community nutrition environments [e.g., the Robert Wood Johnson Foundation Healthy Eating Research Program (http://www.healthyeatingresearch.org)] were searched for a list of ongoing environmental strategies.
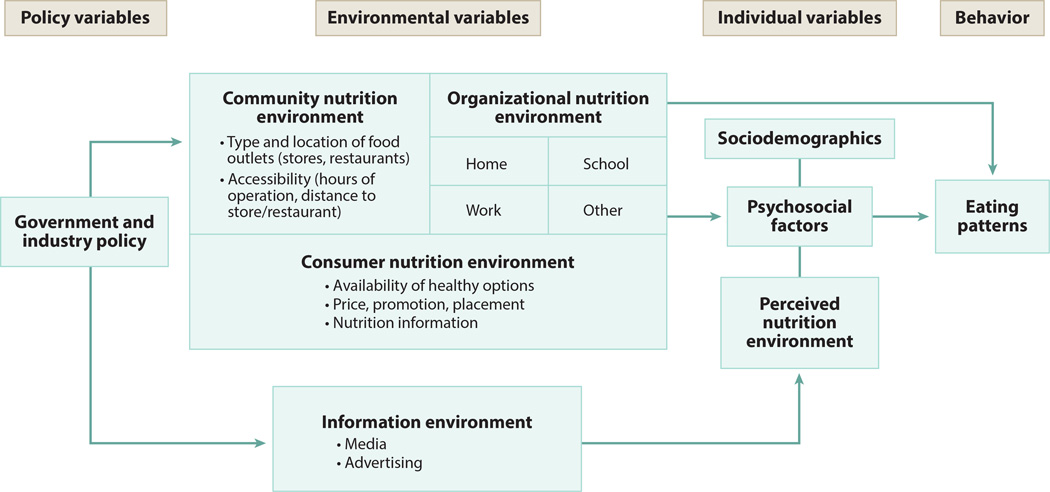
A socioecological framework tailored to characterize nutrition environments (44) has guided much of the research to date. The suggested conceptualization of the nutrition environment centers on individual perceptions of food in the neighborhood and connects to other higher-order domains, including those at the consumer level (food in neighborhood food outlets), community level (food outlets in the neighborhood), organizational level (food in systems, institutions, or workplaces), informational level (food in media and advertising), and policy level (food affected by governmental decisions) (36) (Figure 1). Story and colleagues (88) outline measures that map to the framework of nutrition environments developed by Glanz et al. (44). We used the Glanz et al. categories to organize the examination of evidence on environmental and policy changes related to eating patterns.
Figure 1.
Elements of the nutrition environment.
Results presented are based on a qualitative synthesis of intervention findings organized by nutrition environment domain, providing a description of the strategy and commenting on study outcomes in narrative form. We have conducted a representative, not comprehensive, review to provide a sense of the status of intervention research in each nutrition environment domain. We have recorded target population or setting, intervention target, and overall findings for each relevant study.
GOVERNMENT POLICIES
Governmental policy has been used to shape the accessibility and affordability of food within organizations, communities, and retailers. Likely the most far-reaching policy is the federal Farm Bill, which oversees agricultural production as well as 15 federal nutrition assistance programs (54, 58). The Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program, is the largest of the nutrition assistance programs and has significant influence on the accessibility of food for low-income adults in the United States (56, 93). An average of 48 million adults participated in SNAP in 2013 (about 1 in every 5 American adults) (93). Participating adults receive a monthly benefit (about $133 per person), accessible via an electronic benefit transfer (EBT) card, to purchase foods from program-approved retailers (93). Policies governing lunches and food offerings within schools, though discussed primarily in reference to children, also influence the overall food environment. Other policies implemented at regional and local levels that affect the food environment include food and beverage taxes, menu labeling, commercial zoning policies, and licensing and permitting requirements for food outlets. All vary substantially by locality.
SNAP Interventions
Although SNAP does not exclude or subsidize certain foods, increasing access to farmer’s markets in low-income neighborhoods has been a popular strategy to promote healthy food purchasing among SNAP participants (66). The use of food stamps at farmer’s markets was much higher preceding the rollout of EBT in 1996 (29). Many vendors at farmer’s markets do not accept electronic transactions because of a lack of electricity or associated costs, which prevent SNAP participants from making purchases (29). Interventions targeting farmer’s markets have focused on increasing EBT purchases by establishing onsite EBT card terminals (10, 18, 29) and providing discounts or rebates for EBT transactions (7, 29) with success. More studies among SNAP participants across the United States are needed to further evaluate the success of providing discounts or rebates at farmer’s markets in varying geographic and demographic contexts (52, 53). With respect to implementation issues, increasing access to farmer’s markets for SNAP-eligible adults is limited by the fact that many vendors did not continue to offer EBT purchasing after the pilot program ended, suggesting that farmer’s market vendor subsidies for EBT terminals are needed. Low EBT redemption rates relative to overall sales at farmer’s markets may suggest that outreach to low-income adults is also needed to ensure program sustainability in some areas (29).
Research to elucidate and evaluate strategies to address barriers experienced by both farmer’s market vendors and SNAP-eligible adults is needed to improve access to this healthy food venue. Controversy also exists about whether SNAP participants can afford to purchase healthy food with current allotments (57). A recent IOM/National Research Council committee was asked to ascertain whether the adequacy of the SNAP benefit allotment could be evaluated, and the Committee concluded that additional factors, including those related to the nutrition environment, would need to be considered in the evaluative process (58).
Menu Labeling
Food consumed away from home now accounts for about one-third of total calories consumed in the United States (59). The content of the food provided within restaurant venues is of concern; a review of Web-based nutrition information found that only 4% of main entrées at major chain restaurants fell within one-third of the recommended daily intake using the USDA (US Department of Agriculture) guidelines for dietary intake of energy, sodium, fat, and saturated fat (99). Making decisions for healthful eating is difficult in restaurant environments that do not provide point-of-purchase nutritional information and promote energy-dense foods and large portion sizes (56, 88). Two reviews of menu-labeling intervention findings have noted a lack of consistent associations between menu labeling and foods purchased (43, 91). Additional studies have been published (16, 17, 28, 48, 50, 62, 71, 94, 99) since the review was published in 2011 (91). Again, findings are mixed, although differences could be explained by study design employed (i.e., experimental versus quasi-experimental). Given the recent federal mandate for menu labeling as part of the Affordable Care Act of 2010, continued review of this literature is needed as more evidence is published.
Overall, findings from these studies do not provide evidence that support menu labeling as an effective strategy to change purchasing patterns. Analysis by subgroups does provide additional information. One study found that calories purchased decreased among patrons of coffee shops compared with patrons of restaurants (62), whereas another study found that calories purchased decreased among those who used the menu label in their food-purchasing decision compared with those who saw and did not use or did not see the menu label (94). Restaurants may be responsive to modifying menus in response to consumer demand for more information. Some studies have found that healthy menu options increased after menu-labeling enactment (12, 64), although none noted a difference in the overall menu caloric content (11, 16, 72). Beyond labeling, implementation of nutritional standards for restaurants has also been proposed (28).
Differences in the association between menu labeling and purchasing by subgroup may provide additional process information for this area of research. Specifically, this strategy as implemented appears to be more effective for individuals who are more educated or familiar with nutrition labeling in general (85). Process information in minority and low-income samples indicates, however, that menu-labeling implementation can have high fidelity in these communities (64) and that caloric information is salient to purchasing decisions (74). This nutritional information, however, does not necessarily translate to decreases in consumption (29), which may be related to how and what nutrition information is provided. For example, difficulties in calculating calories per serving arise when ranges of calories are presented for a menu item that comes in multiple flavors or when calories are presented for a menu item that contains multiple servings (28).
Identifying additional strategies to enhance menu-labeling practices is needed because nutrition information alone has not been found to change dietary behavior overall. This limited success may be attributed in part to a lack of understanding of portion sizes, especially in venues outside the home (32). Larger portion sizes have been associated with eating meals away from home as well as with obesity (31). In concert with providing more healthy options and nutrition information, limiting portion sizes within restaurants may also be a useful strategy to promote healthy food environments.
Food Taxation
Intervention evidence supporting food taxes is also limited (27). Simulation studies on the price elasticity of soda have demonstrated minimal impact on weight-related outcomes (80). A study using a quasi-experimental design to model changes in taxes on soda within states in relation to population levels of body mass index (BMI) and obesity over time found evidence of a small positive effect (34). No studies were found that evaluated the effect of a “fat tax” on outcomes within the United States, although evaluation of this strategy has begun in Europe (73) and Great Britain (65). More studies are needed that evaluate the impact of taxes implemented on actual dietary intake.
Soda taxes may not have been effective in altering weight-related outcomes because the amount of the tax has been too small (26, 80). On the basis of price elasticity data, a tax that raises the price of soda by an estimated 10–20% is needed to significantly impact consumption (5, 26, 80). Simulation studies and the quasi-experimental study using the 4% average state soda tax found small effects on obesity (34, 80), which may provide evidence to support soda tax increases. Barriers to a more widespread implementation of soda taxes include opposition from the beverage industry as well as established state sales tax exemptions for food and beverages (26, 80). An excise tax (i.e., a tax on the manufacturer) may be more attractive to manufacturers than a sales tax and is administratively easier for governing bodies to implement and enforce (79). An excise tax may also be more effective in altering consumer purchasing because it would raise the shelf price of the product, which may be more impactful on purchasing decisions than taxes, which are added during checkout (26, 79). Consumers do not appear to support implementation of soda restrictions overall (51), although greater support has been demonstrated among groups of younger age and higher socioeconomic status (10). Discussion about using this tax revenue to fund obesity-prevention initiatives is not new (15), and the need to implement an even higher soda tax is suggested by the fact that currently enacted tax levels among 28 selected states were not found to be sufficient to impact population-level dietary behaviors or weight-related outcomes.
Other Public Policies
The Healthy Food Financing Initiative (HFFI), formerly the Pennsylvania Fresh Food Financing Initiative (35), is a flagship federal financing program to increase supermarket development in low-income communities and communities of color; its effectiveness has yet to be evaluated with respect to dietary outcomes. Similar policy development in other regions and cities is emerging (48, 92), and evaluation of these programs will be informative (35). Evaluation is needed of interventions that employ local public policy, including zoning, permitting, and licensure, to bring about obesity-related or dietary outcomes. South Los Angeles implemented a ban on incoming fast-food outlets, which did not appear to change obesity rates at the census tract level (90); however, associations with dietary outcomes have yet to be assessed.
ADVERTISING AND MEDIA (INFORMATION ENVIRONMENT)
We live in a world that supports a plethora of information, including advertising, from multiple sites and sources that is designed to influence our preferences and behaviors. US food industries emphasize low cost, taste, and convenience of foods, with health playing a minor role to a specialized market (15, 24). Advertising of food products and outlets to consumers still occurs primarily via television, radio, and print media. Yet, the advent of the Internet has introduced social media and many websites, games, and applications that now may also host advertising and contribute to the food-related information environment (23). The Internet is also used as a channel for the delivery of behavior change programs. In this article, however, the information environment refers to advertising or noncommercial nutrition information or social marketing.
Evaluations of the effects of advertising on adult food preferences within intervention settings are emerging (59, 69, 101). Overall, exposure to food advertisement treatments has influenced adult food preferences across diverse populations. In a study among Australian parents and their children, viewing of food advertisements on the Internet was associated with increased endorsement, desire to consume, and frequency of desired consumption of the advertised food among adults (78). Among US adults, exposure to advertising for fruits and vegetables resulted in increased willingness to pay for such foods, and resulting simulation models suggested that broad-based advertising for fruits and vegetables would lower average individual caloric intake by ~1,800 kcal per year (59). Surveys of the general public in the United States have shown that individuals are generally favorable toward policies that control or regulate advertising and promotion of food products (61). First Amendment protections in the United States make it nearly impossible to regulate advertising; however, some voluntary industry efforts are taking place, particularly in advertising directed at children (77). Broader implementation and evaluation of these voluntary efforts are needed.
Media advertising can be considered an intervention designed to change population behavioral performance; therefore, the potential for media to influence behaviors related to eating and dietary habits is huge, for the good and the bad. Advertising and promotional activities are implemented daily to increase the frequency of food product purchases by both youth and adults, and innovative methods are constantly being identified to promote food products, both internationally and regionally. Engaging the Internet brings an additional complexity into the information environment because increasing numbers of individuals use the Internet and social media in various ways. With regard to smaller-scale efforts, recent work on the use of electronic communication devices among public housing residents (8, 9) suggests a potential future direction for interventions that use group interactions.
In sum, broadening the discussion to include evaluation of social media and websites for marketing and advertising of food products and purchasing may be a promising direction for research (8, 9). Following the developments of media as they make inroads into the environments of advertising and marketing will help keep evaluation of this outlet on track.
WORKSITES AND OTHER INSTITUTIONAL SETTINGS (ORGANIZATIONAL NUTRITION ENVIRONMENTS)
The field of organizational nutrition environment change is mature enough that multiple efficacy studies have now targeted organizations for change. There is a growing literature on the dissemination of these types of interventions to change population health. Institutional environments are fertile settings for intervention because strategies can use existing structures, and the policies and programs that can be offered within them, to influence healthy eating. Structures discussed here are workplaces, health care systems, and religious organizations.
Workplaces
Workplaces are perhaps one of the most studied of the organizational areas of intervention. There have been Cochrane and other reviews of workplace health promotion (3, 19, 36, 51), and at least one other systematic review of workplace interventions to improve eating behaviors in adult populations has been published (75).
The Community Guide to Preventive Services Task Force recommends multicomponent interventions that include nutrition and physical activity (including strategies such as providing nutrition education or dietary prescription, physical activity prescription or group activity, and behavioral skills development and training) to control overweight and obesity among adults in worksite settings. In addition, a Cochrane review (36) noted consistent changes as a result of workplace interventions focused on physical activity. Many workplace interventions have included multiple strategies (materials, classes, changes in access to food supplies, and changes in social norms) and have also focused on physical activity to reduce obesity, making it difficult to specify which strategy or target behavior can be credited with behavioral change success and precluding an evidence-based modification of the collection of strategies (3). Incentive programs at workplaces, providing rewards for healthy eating, physical activity, and/or weight loss, have generally shown to be beneficial, although these were not typically used in conjunction with more programmatic or policy interventions.
A recent task force on worksite health promotion intervention discussed issues of dissemination and implementation research and recommended several strategies (79). Issues discussed in this review include the mechanisms by which workplace interventions function, the diversity of workplaces and the individual and unique responses to the intervention, and the contributions of individual and environmental multicomponent interventions to changes in workplace behaviors (86, 87). We are learning about the extent of the reach and sustainability of these long-term studies, which are attempting to establish policies and programs in organizations that we hope will lead to health promotion changes, such as reductions in obesity, in very large numbers of working adults. Resolving the gulf between health promotion and worker health and safety might be another promising area to consider. A few projects, notably those of Sorenson & Barbeau (86), have integrated these two areas of workplace health promotion activity.
Religious Organizations
Religious organizations, both Black churches (34) and Hispanic churches as well as a broader range of religious settings (13), have been used as settings for policy and programmatic change. In general, these studies have found that a multicomponent intervention that includes policy change, promotional materials, religious organizational involvement, and community health workers has improved eating behaviors. The sustainability and reach of these interventions were tested in follow-up studies, with positive outcomes in organizational changes, indicating a high potential for dissemination to occur (49).
Organizations have a remarkable ability to control their food offerings, such as vending machines or food-offering stations. This control is best exemplified by the use of tobacco sales policies in workplaces and other organizations. A similar set of strategies is being enacted for food availability in some workplaces and public places to increase individuals’ access to healthy options and decrease the availability of less healthful options. These approaches may be key elements of future interventions.
NEIGHBORHOOD-LEVEL FOOD AVAILABILITY (COMMUNITY NUTRITION ENVIRONMENT)
The community nutrition environment domain has been defined as the distribution of neighborhood food outlets, including supercenters, supermarkets, grocery stores, convenience stores, and restaurants (both full service and quick service), as well as farmer’s markets and community gardens (43, 67, 68, 88). Two main methods have been used to quantify the community nutrition environment. The most common approach for determining neighborhood food availability involves enumerating the number of food outlets within a specified area such as a census tract or a predefined circular buffer using geographic information systems (GIS), whereas a second approach involves on-the-ground audits of stores in a neighborhood (20, 21, 84). Most studies enumerate food sources around the home, but more studies are now assessing food sources in reference to other places such as workplaces and schools. Studies have typically used GIS technology to quantify density and proximity measures of food outlets within defined geographical units (20, 84). Linking extant geospatial data to individual-level observational data is attractive to many investigators because this approach is less time- and resource-intensive than is field enumeration of neighborhood food outlets. This measurement approach is subject to misclassification, however, because extant data may not be collected frequently enough to capture changes in the distribution of neighborhood food outlets. On-the-ground audits have also been used to establish truth in GIS data to address this limitation.
With respect to the interventions below, those in this section refer to interventions, beyond governmental financing initiatives as described above (see Government Policies), that seek to change which food outlets are offered within neighborhoods. Interventions that seek to change the availability and pricing of foods within food outlets already established in neighborhoods are grouped with the consumer nutrition environment and discussed in the next section.
Several intervention studies have undertaken environmental strategies to increase the number of food outlets that offer fresh produce in neighborhoods (25, 38). Successful interventions include increasing the number of farmer’s market days and establishing community gardens (26, 40, 81). The Veggie Project was a multicomponent intervention that brought farmer’s markets to four Boys’ and Girls’ Club sites situated within low-income, minority, urban communities in Nashville, Tennessee (37). The intervention included a discount voucher program to offset the cost of healthy foods for participating families and was associated with a significant increase in fruit and vegetable purchases, as evaluated by a before–after quasi-experimental study (37).
Three separate ongoing community-level, obesity-prevention initiatives to change the community nutrition environment in California used community-based participatory approaches to identify ways of providing additional healthy food outlets in the neighborhood (42). Selected strategies varied by community and examples included establishing an organic farmer’s market, delivering boxes of fruits and vegetables to low-income neighborhood residents, setting up a low-cost fruit and vegetable stand at an elementary school, and transforming a convenience store into a produce outlet (30, 100). These efforts also proposed to incorporate national low-income voucher programs to address the economic barriers of people in those communities (25). Evaluation of these efforts has yet to be completed.
This type of intervention research is still novel, and the main barrier to effective implementation is a lack of evidence-based model strategies and demonstrated protocols about how to create change in communities (39). The structural changes to the neighborhood required to implement these environmental approaches can be difficult to achieve in the short term, let alone to ensure sustainability, within the timing of grant funding cycles (36). Other barriers to success include failure to identify intervention partners with all the expertise needed; interventions may engage community stakeholders who have limited experience with advocating for or implementing structural- or policy-level changes (70). For example, Morland (70) and others found an overall lack of business expertise among key personnel when creating a community-based cooperative (co-op) market. Nonetheless, reviewing this type of formative research may be invaluable for the planning and execution of similar strategies. ChangeLab Solutions (formerly Public Health Law and Policy; http://changelabsolutions.org/) provides an online collection of reports that address these issues, although evaluation of these recommendations is needed. Lessons learned from smoking cessation policy and business change implementation over the past decade may also prove informative, given the possible consideration of unhealthy eating choices as an addictive behavior (60).
Interventions within more rigorous study designs that include a nonintervention control group and that target the community nutrition environment still need to be implemented and evaluated. Taking a systems approach, interventions in the community nutrition environment in conjunction with interventions at the individual level would likely have synergistic effects, and assessment of these could be built into the evaluation. To more directly attribute behavior change to the structural changes effected, designs should be set up to allow researchers to separate these effects from other individual-level intervention elements. Using a randomized controlled design, comparison of multiple arms (e.g., environmental change alone, environmental change plus other intervention elements, and control) would be ideal to ascertain whether modifications to the nutrition environment are effective in increasing healthy dietary behaviors. However, as has been pointed out (55, 57), this study design is rarely feasible for such reasons as cost, so the use of quasi-experimental and nonrandomized designs that still retain the intervention component may be optimal for evaluation purposes. Another approach could be to estimate the role of the environment as an effect modifier of traditional individual-level intervention approaches on the corresponding outcomes (47). Evaluation of the impact of environmental strategies on intermediate outcomes such as psychosocial correlates of healthy eating (e.g., social support and self-efficacy) may also provide valuable insights.
Finally, long-term evaluation of any of these strategies is entirely lacking to date because the existing studies of interventions focused on environmental or policy-level changes to the community nutrition environment are still in progress or have only short-term outcomes. Threats to evaluating long-term outcomes include the high mobility of low-income populations. These groups have the least access to healthy foods and are therefore more likely to be the focus of these interventions, but they may be difficult to follow long term (66).
AVAILABILITY AND AFFORDABILITY OF HEALTHY FOODS IN RETAIL OUTLETS (CONSUMER NUTRITION ENVIRONMENT)
The consumer nutrition environment includes measures of food availability within neighborhood food outlets. Strategies to influence product stocking, pricing, and display are used to affect what is available and promoted to the consumer within stores—whether small grocer or large supermarket—and in restaurants. Some intervention studies have been designed to test whether modifying components of the consumer nutrition environment (e.g., availability, price, and acceptability of healthy food) within the retail environment of existing food outlets is associated with increasing healthy dietary choices. Consumer-level strategies share a common goal of increasing the accessibility of healthy food in neighborhood stores and may work through influencing the behaviors of store retailers as well as those of consumers.
Targeting store retailers is important because they decide which products to stock, how to display them, and how much variety to offer (41). Strategies to change retailer food stocking and display practices include offering incentives to provide more healthy foods and produce (16, 40), improving mechanisms and offering incentives for purchasing food from local farms (66), monitoring or purchasing refrigeration units for the storage of perishable produce items (66), placement of healthy foods within the store (1, 16, 36, 40), and point-of-purchase promotion of healthy foods and produce (1, 36). Implementation of these strategies may also require operation within higher policy-level domains.
Similar approaches to increase the availability of healthy foods have also been used within restaurant settings including nutrition training for chefs on how to prepare dishes that are lower in fat, changing catering policies to require healthy food choices, and encouraging point-of-purchase promotion and information such as table tents and menu-labeling policies (43, 62). Some success has been demonstrated for interventions among small grocery retailers using a combination of product placement and promotion strategies, with reported small increases in sales of fruits and vegetables among specific customers (1).
Other environmental-level strategies focus on making healthy foods attractive to consumers in store environments. The most popular strategy evidenced in the literature was the implementation of price discounts for healthy food (38, 43, 92), whereas a few studies also attempted in-store sampling and cooking demonstrations of healthy food items (1, 36). Although there is currently no evaluation data available for in-store taste demonstration strategies, the use of price discounts has been consistently associated with changing food purchasing in several studies (38, 76, 89). Larger increases in sales of fruits and vegetables were demonstrated among participants given price discounts within the previously described Veggie Project (37). A similar increase in healthy food sales was noted at 6 months and 12 months postintervention among those assigned to receive price discounts in randomized controlled trials (11, 76, 97). A combination of discount plus nutrition education strategies resulted in an even greater increase in fruit and vegetable purchases, and the number of participants who consumed recommended amounts of fruits and vegetables increased from 42% at baseline to more than 61% for both discount groups (96). In an observational study in South Africa, participation in healthy food discount programs was associated with reported increased consumption of fruits and vegetables and whole grain foods as well as decreased consumption of fast and fried foods and foods high in sugar or salt (4). These findings were replicated using grocery receipt scanner data to measure food purchasing (89).
However, the ability to implement environmental strategies within stores depends on the store’s willingness to change, business practices, and available resources. Fidelity of intervention strategies targeting small-store owners could limit the potential impact on customer food choice via these approaches (1). Reviews of small-store interventions have noted differences in intervention fidelity (1), although these differences could be due to the location of small stores studied (i.e., U.S. versus U.K. implementation). Although most small-store owners in the United Kingdom supported intervention goals to improve health among members of the neighborhood, their inability to compete with larger supermarket pricing of fruits and vegetables was a common barrier to maintaining produce availability (1). Similar to community-level strategies used in the United States, a lack of business expertise and clear definition of roles and responsibilities was also cited by small-store owners as a significant barrier to implementing healthy food stocking strategies (1). Such barriers identified by US small-store retailers included a lack of consumer demand, refrigerator or freezer space, and profitability (6) in addition to neighborhood crime (5).
With respect to pricing interventions, the effects of these programs have been demonstrated in mostly white populations, but effects may vary by ethnic group (11). In a randomized controlled trial in New Zealand, for example, increases in healthy food purchasing tied to the price discount intervention were seen in European and Asian groups but not in Maori groups (11). Selection or cultural adaptation of strategies to address group food preferences may be warranted.
Continued study is needed to determine whether increased availability of healthy foods in retail stores impacts shopping and dietary behaviors of neighborhood customers (36). Facilitating low prices or promoting alternative strategies for small-store owners as well as training intervention store personnel in elements of health promotion may be helpful. Evaluation of programs using retailer financial incentives to promote healthy food availability may offer a solution to address pricing barriers faced by small stores. Exploration of the impact of placement and promotion of healthy foods is also needed, as is further development of tools to assess these components (43). These may be more attractive alternative strategies for small-store owners who are not able to provide discounted pricing on healthy foods. In addition, interventions that evaluate price discounting among at-risk groups may be warranted given the noted differences in response among groups of varying socioeconomic status (11) and to ensure that efforts do not contribute to greater disparities in healthy dietary behaviors. Ensuring that price discounts include culturally appropriate foods is a must.
PERCEIVED NUTRITION ENVIRONMENT
An alternate method of measuring proximity and access to neighborhood food and food stores is via self-report. Perceptions of the food environment have produced different associations with dietary intake compared with their corresponding objective measures, perhaps owing to the inclusion of other dimensions of access (14). A combination of objective and perceived measures may provide a more comprehensive measure of the nutrition environment and perhaps increase the likelihood of detecting associations with dietary outcomes (14).
No published studies designed specifically to change perceptions of the neighborhood food environment were identified. However, some studies showed that perceptions of the proximity of food outlets or sources of healthy foods may not be concordant with an objective classification. This difference could manifest as nonreporting of a food outlet despite the objective presence of that same food outlet. In a study of the greater Boston area, Caspi and colleagues found an approximate 32% mismatch of this type (21). Nonconcordance could also manifest as a difference in food outlet classification. Gustafson and colleagues found that individuals who lived in areas with a supercenter (e.g., Walmart) and convenience store perceived their neighborhood as high in the availability of healthy foods (46, 47), whereas researchers categorized these stores as unhealthy food outlets (95). Both studies found that individuals who discrepantly reported nutrition environment perceptions relative to objective measures consumed fewer fruits and vegetables and weighed more (46, 47). The lack of concordance between objective and perceived measures may provide additional points of intervention or process information to boost effectiveness of environmental strategies. It may also speak to the need to incorporate additional dimensions of access (e.g., cost, travel mode, and travel duration) when considering perceptions of the nutrition environment (2).
Perceptions of the food environment may be more salient to dietary behavior change than are objective measures of the nutrition environment (35). Qualitative research may illuminate additional attitudinal change agents, especially with respect to understudied domains of access. For example, food and retail qualities of importance for low-income shoppers have included relationships with store personnel in addition to the internal store environment, product quality, and product price (98). These attitudes were highly related to how shoppers considered dimensions of access within the food environment (98). Evaluation is needed of interventions using strategies to influence individual perceptions of the neighborhood nutrition environment.
CONCLUSIONS AND FUTURE DIRECTIONS
We have identified recent evidence concerning effective strategies for changing the nutrition environment. Overlapping those discussed in the IOM report (56), these include instituting a tax on sodas, using worksite environments to support healthful changes in the obesogenic environment, bringing supermarkets to underserved neighborhoods, increasing the numbers of farmer’s market days, and encouraging discount pricing of healthy foods within retail outlets. These strategies apply mostly to both children and adults. Research into the efficacy and effectiveness of intervention modalities that incorporate environmental strategies is falling behind associational research and is also falling behind practice. To drive these efforts forward, successful models and demonstrated protocols for community-level change are needed. Incorporation of a nonintervention control group in study designs is ideal for assessing effects directly attributable to changes in the environment. Yet, not everything can be evaluated in the context of a randomized controlled trial. Taking advantage of natural experiments may be one key way to evaluate environmental strategies and may be an efficient use of resources for research. Evaluations of the community environment as an effect modifier of other interventions on obesity risk may hold promise. For example, considering the home or workplace environment when delivering an individual-level intervention may help explain findings that vary by a higher group level or may identify future research opportunities.
More studies that incorporate both objective and perceived measures of the nutrition environment are also needed to further understand relationships with dietary behaviors. Because perceived and objective measures may be tapping different dimensions of access to the food environment, utilizing both assessments in analyses may form a more comprehensive picture of how environment influences dietary behaviors. Because of the more proximal position to behavior patterns, a greater focus on interventions that change perceptions themselves is warranted. Including perceived and objective measures of the nutrition environment in intervention evaluations may be insightful in multiple contexts. First, evaluating perceived and objective measures as effect modifiers in traditional intervention studies may identify groups for whom the intervention is more or less effective. Second, inclusion of perceived and objective measures within environmental interventions may provide process information to gauge the implementation success of environmental strategies.
Policy changes are clearly needed, as is evaluation of such policies. Given the lack of success demonstrated by informational strategies alone (e.g., menu labeling), perhaps we should take greater advantage of lessons learned from smoking cessation policy to invoke desired behavioral change. There is now a rigorously conducted set of studies that supports the use of many types of tobacco control policies implemented concurrently to help smokers quit and to prevent youths from beginning to smoke. Using this evidence and applying it to changes in eating behavior may yield novel and more effective approaches to using the information and policy environment to effect dietary behavior change. For example, behavioral change as a result of currently enacted soda taxes has not been demonstrated. Increasing the tax further for sugar-sweetened beverages, as was done for tobacco products, may be necessary. To be commensurate with taxes placed on cigarettes, for example, soda tax would need to be an added 58%, which would translate to a population-level shift in BMI of 0.6 kg/m2 (for methods, see 33).
Policy and evaluation of policy to control marketing and promotion of key food sales are key elements to the promotion of healthy eating. Given the outlay of money for food advertising, these efficacious messaging systems can be presumed to change people’s behaviors and need to be considered and curtailed to reduce future increases in the consumption of empty calories. These types of policies are underevaluated and often misunderstood (45), as in the case of the recent law to limit sales of large soda containers in New York City. At the time of this writing, this law was under review by a higher court, but this attempt to limit soda manufacturers from selling oversized soda containers in New York City brought on a campaign by the beverage distributors to label the law as antifreedom and misguided in its attempts to control soda sales (92). Evaluating the effects of these types of policies, if and when they are put into place, on both individual behavior and on the behaviors of food companies will be enlightening.
Counteradvertising, as is being done with tobacco, might be an additional solution. Counteradvertising to provide truthful messages to the public about tobacco products has been efficacious in changing individual smoking behavior. How this strategy will affect healthy eating is currently unknown. In addition, how to engage counteradvertising without increasing stigma for overweight people is also unknown and should be the focus of research.
A larger focus on the use of multiple organizational units (worksites, hospitals, schools, communities) within natural policy units such as cities, counties, or states is a promising direction. The use of theory to guide these interventions is often quite poor, and the role of theory in this area of research is not well established. Some interventions might be more powerful or more far reaching and sustainable if theory is used. This area needs research attention.
The framework that presents schematically the effects of the relationships among community, organization, consumer, and information environments and the perceptions of those environments on individual-level eating behaviors appears to be valuable. Additional research should explicitly test the framework to further guide intervention opportunities. Evaluations of environmental-level interventions that aim to restructure environments to promote healthy dietary choices are fairly new and relatively few in number (22). As a result, a large evidence base to identify successful strategies has yet to be formed for adults, although it has been for children (http://www.transtria.com/evidence_review.php).
As previously mentioned, multimodal strategies that include multiple channels and organizational levels might be the answer, but few have been evaluated. Much work needs to be done also to sufficiently consider population differences based on socioeconomic and geographic characteristics in order to tailor specific approaches to sectors of the population. Such research efforts are needed to identify environmental strategies that can be used in the intervention toolboxes that public health and community members can use to build healthy nutrition environments.
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
Contributor Information
Deborah J. Bowen, Email: dbowen@uw.edu.
Wendy E. Barrington, Email: wendybar@uw.edu.
Shirley A.A. Beresford, Email: beresfrd@u.washington.edu.
LITERATURE CITED
- 1.Adams J, Halligan J, Watson DB, Ryan V, Penn L, et al. The Change4Life convenience store programme to increase retail access to fresh fruit and vegetables: a mixed methods process evaluation. PLOS ONE. 2012;7(6):e39431. doi: 10.1371/journal.pone.0039431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggarwal A, Cook AJ, Jiao J, Sequin RA, Vernez Moudon A, et al. Access to supermarkets and fruit and vegetable consumption. Am. J. Public Health. 2014;104(5):917–923. doi: 10.2105/AJPH.2013.301763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am. J. Prev. Med. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 4.An R, Patel D, Segal D, Sturm R. Eating better for less: a national discount program for healthy food purchases in South Africa. Am. J. Health Behav. 2013;37(1):56–61. doi: 10.5993/AJHB.37.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andreyeva T, Chaloupka FJ, Brownell KD. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev. Med. 2011;52(6):413–416. doi: 10.1016/j.ypmed.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Ayala GX, Laska MN, Zenk SN, Tester J, Rose D, et al. Stocking characteristics and perceived increases in sales among small food store managers/owners associated with the introduction of new food products approved by the Special Supplemental Nutrition Program for Women, Infants, and Children. Public Health Nutr. 2012;15(9):1771–1779. doi: 10.1017/S1368980012001255. [DOI] [PubMed] [Google Scholar]
- 7.Baronberg S, Dunn L, Nonas C, Dannefer R, Sacks R. The impact of New York City’s Health Bucks Program on electronic benefit transfer spending at farmers markets, 2006–2009. Prev. Chronic Dis. 2013;10:E163. doi: 10.5888/pcd10.130113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett GG, McNeill LH, Wolin KY, Duncan DT, Puleo E, Emmons KM. Safe to walk? Neighborhood safety and physical activity among public housing residents. PLOS Med. 2007;4(10):e306. doi: 10.1371/journal.pmed.0040306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bennett GG, Wolin KY, Puleo E, Emmons KM. Pedometer-determined physical activity among multiethnic low-income housing residents. Med. Sci. Sports Exerc. 2006;38(4):768–773. doi: 10.1249/01.mss.0000210200.87328.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Black C, Moon G, Baird J. Dietary inequalities: What is the evidence for the effect of the neighbourhood food environment? Health Place. 2014;27C:229–242. doi: 10.1016/j.healthplace.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blakely T, Ni Mhurchu C, Jiang Y, Matoe L, Funaki-Tahifote M, et al. Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomised, controlled trial. J. Epidemiol. Community Health. 2011;65(10):902–908. doi: 10.1136/jech.2010.118588. [DOI] [PubMed] [Google Scholar]
- 12.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J. Urban Health. 2010;87(5):771–781. doi: 10.1007/s11524-010-9460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowen DJ, Beresford SAA, Christensen CL, Kuniyuki AA, McLerran D, et al. Effects of a multilevel dietary intervention in religious organizations. Am. J. Health Promot. 2009;24(1):15–22. doi: 10.4278/ajhp.07030823. [DOI] [PubMed] [Google Scholar]
- 14.Briggs S, Fisher A, Lott M, Miller S, Tessman N. Real Food, Real Choice: Connecting SNAP Recipients with Farmer’s Markets. Portland, OR: Community Food Secur. Coalit.; 2010. [Google Scholar]
- 15.Brownell KD, Frieden TR. Ounces of prevention—the public policy case for taxes on sugared beverages. N. Engl. J. Med. 2009;360(18):1805–1808. doi: 10.1056/NEJMp0902392. [DOI] [PubMed] [Google Scholar]
- 16.Brownson RC, Haire-Joshu D, Luke DA. Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu. Rev. Public Health. 2006;27:341–370. doi: 10.1146/annurev.publhealth.27.021405.102137. [DOI] [PubMed] [Google Scholar]
- 17.Bruemmer B, Krieger J, Saelens BE, Chan N. Energy, saturated fat, sodium were lower in entrées at chain restaurants at 18 months compared with 6 months following the implementation of mandatory menu labeling regulation in King County, Washington. J. Acad. Nutr. Diet. 2012;112(8):1169–1176. doi: 10.1016/j.jand.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Buttenheim AM, Havassy J, Fang M, Glyn J, Karpyn AE. Increasing supplemental nutrition assistance program/electronic benefits transfer sales at farmers’ markets with vendor-operated wireless point-of-sale terminals. J. Acad. Nutr. Diet. 2012;112(5):636–641. doi: 10.1016/j.jand.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 19.Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst. Rev. 2008;8(4):CD003440. doi: 10.1002/14651858.CD003440.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Carlson A, Frazão E. Food costs, diet quality and energy balance in the United States. Physiol. Behav. 2014;134:20–31. doi: 10.1016/j.physbeh.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Caspi CE, Kawachi I, Subramanian SV, Adamkiewicz G, Sorensen G. The relationship between diet and perceived and objective access to supermarkets among low-income housing residents. Soc. Sci. Med. 2012;75(7):1254–1262. doi: 10.1016/j.socscimed.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC (Cent. Dis. Control Prev.) Overweight and obesity. Atlanta: CDC; Updated Sept. 10. http://www.cdc.gov/obesity. [Google Scholar]
- 24.Chandon P, Wansink B. Does food marketing need to make us fat? A review and solutions. Nutr. Rev. 2012;70(10):571–593. doi: 10.1111/j.1753-4887.2012.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charreire H, Casey R, Salze P, Simon C, Chaix B, et al. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutr. 2010;13(11):1773–1785. doi: 10.1017/S1368980010000753. [DOI] [PubMed] [Google Scholar]
- 26.Cheadle A, Samuels SE, Rauzon S, Yoshida SC, Schwartz PM, et al. Approaches to measuring the extent and impact of environmental change in three California community-level obesity prevention initiatives. Am. J. Public Health. 2010;100(11):2129–2136. doi: 10.2105/AJPH.2010.300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chriqui JF, Chaloupka FJ, Powell LM, Eidson SS. A typology of beverage taxation: multiple approaches for obesity prevention and obesity prevention-related revenue generation. J. Public Health Policy. 2013;34:403–423. doi: 10.1057/jphp.2013.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohn EG, Larson EL, Araujo C, Sawyer V, Williams O. Calorie postings in chain restaurants in a low-income urban neighborhood: measuring practical utility and policy compliance. J. Urban Health. 2012;89(4):587–597. doi: 10.1007/s11524-012-9671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole K, McNees M, Kinney K, Fisher K, Krieger JW. Increasing access to farmers markets for beneficiaries of nutrition assistance: evaluation of the Farmers Market Access Project. Prev. Chronic Dis. 2013;10:E168. doi: 10.5888/pcd10.130121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff. (Millwood) 2009;28(6):w1110–w1121. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 31.Ello-Martin JA, Ledikwe JH, Rolls BJ. The influence of food portion size and energy density on energy intake: implications for weight management. Am. J. Clin. Nutr. 2005;82(1 Suppl.):236S–241S. doi: 10.1093/ajcn/82.1.236S. [DOI] [PubMed] [Google Scholar]
- 32.Evans AE, Jennings R, Smiley AW, Medina JL, Sharma SV, et al. Introduction of farm stands in low-income communities increases fruit and vegetable among community residents. Health Place. 2012;18(5):1137–1143. doi: 10.1016/j.healthplace.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 33.Finkelstein EA, Zhen C, Nonnemaker J, Todd JE. Impact of targeted beverage taxes on higher- and lower-income households. Arch. Intern. Med. 2010;170(22):2028–2034. doi: 10.1001/archinternmed.2010.449. [DOI] [PubMed] [Google Scholar]
- 34.Fletcher JM, Frisvold D, Tefft N. Can soft drink taxes reduce population weight? Contemp. Econ. Policy. 2010;28(1):23–35. doi: 10.1111/j.1465-7287.2009.00182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fleischhacker SE, Flournoy R, Moore LV. Meaningful, measurable, and manageable approaches to evaluating healthy food financing initiatives: an overview of resources and approaches. J. Public Health Manag. Pract. 2013;19(6):541–549. doi: 10.1097/PHH.0b013e318271c6eb. [DOI] [PubMed] [Google Scholar]
- 36.Freak-Poli RLA, Cumpston M, Peeters A, Clemes SA. Workplace pedometer interventions for increasing physical activity. Cochrane Database Syst. Rev. 2013;4:CD009209. doi: 10.1002/14651858.CD009209.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Freedman DA, Bell BA, Collins LV. The Veggie Project: a case study of a multi-component farmers’ market intervention. J. Prim. Prev. 2011;32(3–4):213–224. doi: 10.1007/s10935-011-0245-9. [DOI] [PubMed] [Google Scholar]
- 38.Freedman DA, Mattison-Faye A, Alia K, Guest MA, Hébert JR. Comparing farmers’ market revenue trends before and after the implementation of a monetary incentive for recipients of food assistance. Prev. Chronic Dis. 2014;11:E87. doi: 10.5888/pcd11.130347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gantner LA, Olson CM. Evaluation of public health professionals’ capacity to implement environmental changes supportive of healthy weight. Eval. Progr. Plan. 2012;35(3):407–416. doi: 10.1016/j.evalprogplan.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giang T, Karpyn A, Laurison HB, Hillier A, Perry RD. Closing the grocery gap in underserved communities: the creation of the Pennsylvania Fresh Food Financing Initiative. J. Public Health Manag. Pract. 2008;14(3):272–279. doi: 10.1097/01.PHH.0000316486.57512.bf. [DOI] [PubMed] [Google Scholar]
- 41.Gittelsohn J, Rowan M, Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Prev. Chronic Dis. 2012;9:110015. [PMC free article] [PubMed] [Google Scholar]
- 42.Glanz K, Bader MD, Iyer S. Retail grocery store marketing strategies and obesity: an integrative review. Am. J. Prev. Med. 2012;42(5):503–512. doi: 10.1016/j.amepre.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 43.Glanz K, Hoelscher D. Increasing fruit and vegetable intake by changing environments, policy and pricing: restaurant-based research, strategies, and recommendations. Prev. Med. 2004;39(Suppl. 2):S88–S93. doi: 10.1016/j.ypmed.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 44.Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am. J. Health Promot. 2005;19(5):330–333. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- 45.Gollust SE, Barry CL, Niederdeppe J. Americans’ opinions about policies to reduce consumption of sugar-sweetened beverages. Prev. Med. 2014;63:52–57. doi: 10.1016/j.ypmed.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 46.Gustafson AA, Sharkey J, Samuel-Hodge CD, Jones-Smith J, Folds MC, et al. Perceived and objective measures of the food store environment and the association with weight and diet among low-income women in North Carolina. Public Health Nutr. 2011;14(6):1032–1038. doi: 10.1017/S1368980011000115. [DOI] [PubMed] [Google Scholar]
- 47.Gustafson AA, Sharkey J, Samuel-Hodge CD, Jones-Smith JC, Cai J, Ammerman AS. Food store environment modifies intervention effect on fruit and vegetable intake among low-income women in North Carolina. J. Nutr. Metab. 2012;2012:932653. doi: 10.1155/2012/932653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hammond D, Goodman S, Hanning R, Daniel S. A randomized trial of calorie labeling on menus. Prev. Med. 2013;57:860–866. doi: 10.1016/j.ypmed.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 49.Hannon PA, Bowen DJ, Christensen CL, Kuniyuki A. Disseminating a successful dietary intervention to faith communities: feasibility of using staff contact and encouragement to increase uptake. J. Nutr. Educ. Behav. 2008;40(3):175–180. doi: 10.1016/j.jneb.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int. J. Behav. Nutr. Phys. Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harris JR, Hannon PA, Beresford SAA, Linnan LA, McLellan DL. Health promotion in smaller workplaces in the United States. Annu. Rev. Public Health. 2014;35:327–342. doi: 10.1146/annurev-publhealth-032013-182416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am. J. Public Health. 2012;102(9):1644–1654. doi: 10.2105/AJPH.2012.300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hilmers A, Chen TA, Dave JM, Thompson D, Cullen KW. Supplemental Nutrition Assistance Program participation did not help low income Hispanic women in Texas meet the dietary guidelines. Prev. Med. 2014;62:44–48. doi: 10.1016/j.ypmed.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 54.Hood C, Martinez-Donate A, Meinen A. Promoting healthy food consumption: a review of state-level policies to improve access to fruits and vegetables. WMJ. 2012;111(6):283–288. [PubMed] [Google Scholar]
- 55.IOM (Inst. Med.) Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making. Washington, DC: Natl. Acad. Press; 2010. [PubMed] [Google Scholar]
- 56.IOM (Inst. Med.) Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: Natl. Acad. Press; 2012. [PubMed] [Google Scholar]
- 57.IOM (Inst. Med.) Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. Washington, DC: Natl. Acad. Press; 2013. [PubMed] [Google Scholar]
- 58.IOM (Inst. Med.), NRC (Natl. Res. Counc.) Supplemental Nutrition Assistance Program: Examining the Evidence to Define Benefit Adequacy. Washington, DC: Natl. Acad. Press; 2013. [PubMed] [Google Scholar]
- 59.Johnson DB, Payne EC, McNeese MA, Allen D. Menu-labeling policy in King County, Washington. Am. J. Prev. Med. 2012;43(3) Suppl. 2:S130–S135. doi: 10.1016/j.amepre.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 60.Kenny PJ. Reward mechanisms in obesity: new insights and future directions. Neuron. 2011;69(4):664–679. doi: 10.1016/j.neuron.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kraak VI, Story M, Wartella EA, Ginter J. Industry progress to market a healthful diet to American children and adolescents. Am. J. Prev. Med. 2011;41(3):322–333. doi: 10.1016/j.amepre.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 62.Krieger JW, Chan NL, Saelens BE, Ta ML, Solet D, Fleming DW. Menu labeling regulations and calories purchased at chain restaurants. Am. J. Prev. Med. 2013;44(6):595–604. doi: 10.1016/j.amepre.2013.01.031. [DOI] [PubMed] [Google Scholar]
- 63.Larson N, Story M. A review of environmental influences on food choices. Ann. Behav. Med. 2009;38:S56–S73. doi: 10.1007/s12160-009-9120-9. [DOI] [PubMed] [Google Scholar]
- 64.Lee-Kwan SH, Goedkoop S, Yong R, Batorsky B, Hoffman V, et al. Development and implementation of the Baltimore healthy carry-outs feasibility trial: process evaluation results. BMC Public Health. 2013;13:638. doi: 10.1186/1471-2458-13-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Madden D. The poverty effects of a ‘fat-tax’ in Ireland. Health Econ. 2015;24:104–121. doi: 10.1002/hec.3006. [DOI] [PubMed] [Google Scholar]
- 66.McCormack LA, Laska MN, Larson NI, Storey M. Review of the nutritional implications of farmers’ markets and community gardens: a call for evaluation and research efforts. J. Am. Diet. Assoc. 2010;110(3):399–408. doi: 10.1016/j.jada.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 67.McKinnon RA, Reedy J, Morrissette MA, Lytle LA, Yaroch AL. Measures of the food environment: a compilation of the literature, 1990–2007. Am. J. Prev. Med. 2009;36(4):S124–S133. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 68.Mitchell NS, Catenacci VA, Wyatt RH, Hill JO. Obesity: overview of an epidemic. Psychiatr. Clin. N. Am. 2011;34(4):717–732. doi: 10.1016/j.psc.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moore LV, Diez Roux AV, Brines S. Comparing perception-based and geographic information system (GIS)-based characterizations of the local food environment. J. Urban Health. 2008;85(2):206–216. doi: 10.1007/s11524-008-9259-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morland KB. An evaluation of a neighborhood-level intervention to a local food environment. Am. J. Prev. Med. 2010;39(6):e31–e38. doi: 10.1016/j.amepre.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 71.Morley B, Scully M, Martin J, Niven P, Dixon H, Wakefield M. What types of nutrition menu labelling lead consumers to select less energy-dense fast food? An experimental study. Appetite. 2013;67:8–15. doi: 10.1016/j.appet.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 72.Namba A, Auchincloss A, Leonberg BL, Wootan MG. Exploratory analysis of fast-food chain restaurant menus before and after implementation of local calorie-labeling policies, 2005–2011. Prev. Chronic Dis. 2013;10:E101. doi: 10.5888/pcd10.120224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nederkoorn C, Havermans RC, Giesen JC, Jansen A. High tax on high energy dense foods and its effects on the purchase of calories in a supermarket. An experiment. Appetite. 2011;56(3):760–765. doi: 10.1016/j.appet.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 74.Nevarez CR, Lafleur MS, Schwarte LU, de Silva P, Samuels SE. Salud Tiene Sabor: a model for healthier restaurants in a Latino community. Am. J. Prev. Med. 2013;44(3) Suppl. 3:S186–S192. doi: 10.1016/j.amepre.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 75.Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health. 2010;10:62. doi: 10.1186/1471-2458-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ni Mhurchu C, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am. J. Clin. Nutr. 2010;91(3):736–747. doi: 10.3945/ajcn.2009.28742. [DOI] [PubMed] [Google Scholar]
- 77.Ohri-Vachaspati P, Leviton L, Bors P, Brennan L, Brownson RC, Strunk S. Strategies proposed by Healthy Kids, Healthy Communities partnerships to prevent childhood obesity. Prev. Chronic Dis. 2012;9:100292. [PMC free article] [PubMed] [Google Scholar]
- 78.Pettigrew S, Tarabashkina L, Roberts M, Quester P, Chapman K, Miller C. The effects of television and Internet food advertising on parents and children. Public Health Nutr. 2013;16(12):2205–2212. doi: 10.1017/S1368980013001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pomeranz JL. Advanced policy options to regulate sugar-sweetened beverages to support public health. J. Public Health Policy. 2012;33(1):75–88. doi: 10.1057/jphp.2011.46. [DOI] [PubMed] [Google Scholar]
- 80.Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obes. Rev. 2013;14(2):110–128. doi: 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Quandt SA, Dupuis J, Fish C, D’Agostino RB., Jr Feasibility of using a community-supported agriculture program to improve fruit and vegetable inventories and consumption in an underresourced urban community. Prev. Chronic Dis. 2013;10:E136. doi: 10.5888/pcd10.130053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rivard C, Smith D, McCann SE, Hyland A. Taxing sugar-sweetened beverages: a survey of knowledge, attitudes and behaviours. Public Health Nutr. 2012;15(8):1355–1361. doi: 10.1017/S1368980011002898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Robert Wood Johnson (RWJ) Found. Healthy eating research. Healthy Eat. Res. Minneapolis, MN: 2014. http://www.healthyeatingresearch.org. [Google Scholar]
- 84.Rose D, Bodor JN, Hutchinson PL, Swalm CM. The importance of a multi-dimensional approach for studying the links between food access and consumption. J. Nutr. 2010;140(6):1170–1174. doi: 10.3945/jn.109.113159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Roseman MG, Mathe-Soulek K, Higgins JA. Relationships among grocery nutrition label users and consumers’ attitudes and behavior toward restaurant menu labeling. Appetite. 2013;71C:274–278. doi: 10.1016/j.appet.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 86.Sorensen G, Barbeau E. Steps to a Healthier US Workforce: Integrating Occupational Health and Safety and Worksite Health Promotion: State of the Science. Washington, DC: Dep. Health Hum. Serv., Public Health Serv., Cent. Dis. Control Prev., Natl. Inst. Occup. Saf. Health; 2012. [Google Scholar]
- 87.Sorensen G, Landsbergis P, Hammer L, Amick BC, 3rd, Linnan L, et al. Preventing chronic disease in the workplace: a workshop report and recommendations. Am. J. Public Health. 2011;101(Suppl. 1):S196–S207. doi: 10.2105/AJPH.2010.300075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu. Rev. Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 89.Sturm R, An R, Segal D, Patel D. A cash-back rebate program for healthy food purchases in South Africa: results from scanner data. Am. J. Prev. Med. 2013;44(6):567–572. doi: 10.1016/j.amepre.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sturm R, Cohen DA. Zoning for health? The year-old ban on new fast-food restaurants in South LA. Health Aff. (Millwood) 2009;28(6):w1088–w1097. doi: 10.1377/hlthaff.28.6.w1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Swartz JJ, Braxton D, Viera AJ. Calorie menu labeling on quick-service restaurant menus: an updated systematic review of the literature. Int. J. Behav. Nutr. Phys. Act. 2011;8:135. doi: 10.1186/1479-5868-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ulmer VM, Rathert AR, Rose D. Understanding policy enactment: the New Orleans Fresh Food Retailer Initiative. Am. J. Prev. Med. 2012;43(3) Suppl. 2:S116–S122. doi: 10.1016/j.amepre.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 93.USDA (U.S. Dep. Agric.) Food Nutr. Serv. Supplemental Nutrition Assistance Program (SNAP) Alexandria, Va: USDA Food Nutr. Serv.; 2014. Updated Dec. 4. http://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap. [Google Scholar]
- 94.Vadiveloo MK, Dixon LB, Elbel B. Consumer purchasing patterns in response to calorie labeling legislation in New York City. Int. J. Behav. Nutr. Phys. Act. 2011;8:51. doi: 10.1186/1479-5868-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vernez Moudon A, Drewnowski A, Duncan GE, Hurvitz PM, Saelens BE, Scharnhorst E. Characterizing the food environment: pitfalls and future directions. Public Health Nutr. 2013;16(7):1238–1243. doi: 10.1017/S1368980013000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Waterlander WE, de Boer MR, Schuit AJ, Seidell JC, Steenhuis IH. Price discounts significantly enhance fruit and vegetable purchases when combined with nutrition education: a randomized controlled supermarket trial. Am. J. Clin. Nutr. 2013;97(4):886–895. doi: 10.3945/ajcn.112.041632. [DOI] [PubMed] [Google Scholar]
- 97.Waterlander WE, Steenhuis IH, de Boer MR, Schuit AJ, Seidell JC. The effects of a 25% discount on fruits and vegetables: results of a randomized trial in a three-dimensional Web-based supermarket. Int. J. Behav. Nutr. Phys. Act. 2012;9:11. doi: 10.1186/1479-5868-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Webber CB, Sobal J, Dollahite JS. Shopping for fruits and vegetables. Food and retail qualities of importance to low-income households at the grocery store. Appetite. 2010;54(2):297–303. doi: 10.1016/j.appet.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 99.Wu HW, Sturm R. What’s on the menu? A review of the energy and nutritional content of US chain restaurant menus. Public Health Nutr. 2013;16(1):87–96. doi: 10.1017/S136898001200122X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Young CR, Aquilante JL, Solomon S, et al. Improving fruit and vegetable consumption among low-income customers at farmers markets: Philly Food Bucks, Philadelphia, Pennsylvania, 2011. Prev. Chronic Dis. 2013;10:E166. doi: 10.5888/pcd10.120356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zimmerman FJ, Shimoga SV. The effects of food advertising and cognitive load on food choices. BMC Public Health. 2014;14(1):342. doi: 10.1186/1471-2458-14-342. [DOI] [PMC free article] [PubMed] [Google Scholar]