Abstract
Background
The purpose of this study is to review the anatomic characteristics of internal thoracic artery (ITA) and its branches, in order to pursue the extension of its utilization and avoid intraoperative and postoperative complications.
Methods
The study was carried out on anterior chest walls obtained during routine autopsies of 50 specimens (30 male, 20 female). Macroscopic and microscopic dissection was performed and the following were studied: origin, length and termination of ITA, size and distance from the sternum, and types of branches.
Results
From the origin to the termination point, the length of the left internal thoracic artery (LITA) varied from 159 to 220 mm; with a mean of 182.60 mm. The length of the right internal thoracic artery (RITA) varied from 150 to 231 mm; with a mean of 185 mm. Four types of branches were distinguished. The RITA mean diameter was 2.31 mm, measured at the 2nd intercostal space, while the distance from the sternum was 12.77 mm, measured at the 3rd intercostal space. The LITA mean diameter was 1.98 mm with the distance from the sternum measured at 12.01 mm.
Conclusions
ITA has become the primary conduit for cardiac bypass surgery; many studies have generated fundamental anatomical knowledge for its clinical utilization, which is always useful in order to avoid intraoperative and postoperative complications.
Keywords: Bypass, cadaver, internal thoracic artery (ITA), left internal thoracic artery (LITA), right internal thoracic artery (RITA)
Introduction
Since 1968, when Green first anastomosed the internal thoracic artery (ITA) to a coronary artery, this vessel has gradually become the most frequently utilized conduit in coronary bypass surgery because of long-term better patency rate and improvement in both the duration and quality of survival of patients. The purpose of this study is to review the anatomic characteristics of ITA and its branches, in order to pursue the extension of its utilization and avoid intraoperative and postoperative complications.
Methods
The study was carried out on anterior chest walls obtained during routine autopsies of 50 specimens (30 male, 20 female). After performing two parallel incisions in the midclavicular lines, the sternum along with adjacent rib fragments were elevated. The tissue blocks contained the portions of the subclavian arteries that gave origin to the ITAs.
Macroscopic and microscopic dissection was performed and the following were studied: origin, length and termination of ITA, size and distance from the sternum, and types of branches.
Dissection of ITA and its branches was performed with the aid of a standard set of microsurgical instruments using an operating microscope (Figure 1). Measurements of the size and lengths were made using the calibrated scale of the microscope.
Figure 1.
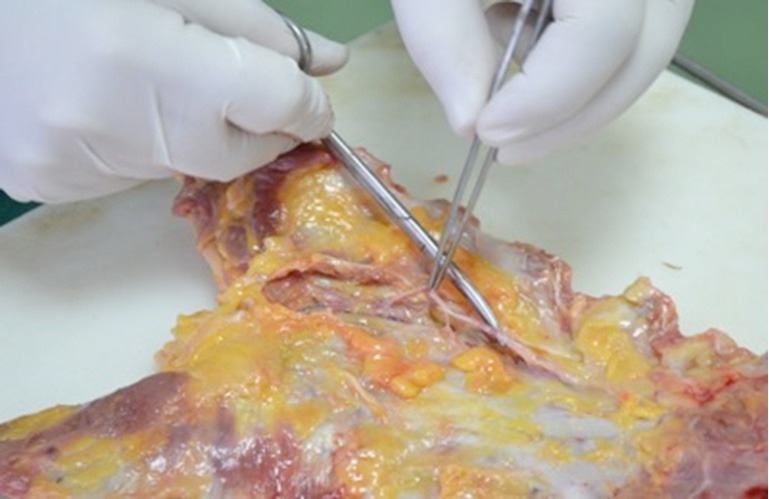
Preparation and dissection of the internal thoracic artery (ITA).
The student’s t test was used for comparison of mean values (SPSS version 17.0). Significance was accepted where P value was less than 0.05.
Results
The ITA was present in all individuals studied. The left internal thoracic artery (LITA) originated directly from the subclavian artery in 38/50 cadavers and from a common trunk with other arteries in 12/50. Right internal thoracic artery (RITA) originated from the subclavian artery in 49/50 cadavers, whereas in 1/50 arose from a common trunk with other arteries (Figure 2). From their origin, the ITAs passed medially and downward behind the 2nd to 6th costal cartilages, at a distance of about 1 cm from the sternal margin. The course of both ITAs was rectilinear in the majority of cases (Table 1). From the origin to the termination point, the length of LITA varied from 159 to 220 mm, with a mean of 182.60 mm. The RITA varied from 150 to 231 mm, with a mean of 185 mm.
Figure 2.

Right internal thoracic artery (RITA) arising from a common trunk with another artery.
Table 1. Incidence of courses of ITAs.
| Course of ITA | Right (n=50) | Left (n=50) |
|---|---|---|
| Rectilinear | 38 | 41 |
| Medial concavity | 11 | 9 |
| Lateral concavity | 1 | – |
| Tortous | – | – |
ITA, internal thoracic artery.
The most frequent type of termination was a bifurcation (superior epigastric and musculophrenic artery) in 96% of LITAs and in 90% of RITAs and a trifurcation (with an additional diaphragmatic branch) in 4% and 10% respectively. The most frequent termination point for both ITAs was the 6th intercostal space with the level of 6th rib to be the 2nd one.
The Pearson correlation of the diameter of ITAs at the 2nd intercostal space according to gender was negative, with values greater in males (Diameter-RITA Pearson correlation: −0.015/Diameter-LITA Pearson correlation: −0.105).
The diameter of ITAs and distance from sternal margin are shown in Table 2.
Table 2. Diameter of ITAs (2nd intercostal space) and distance from the sternum (3rd intercostal space).
| Measurements | Size (mm) | Distance (mm) |
|---|---|---|
| RITA | 2.31 ±0.70 | 12.77±0.37 |
| LITA | 1.98±0.04 | 12.01±0.30 |
RITA, right internal thoracic artery; LITA, left internal thoracic artery.
Four types of branches were distinguished:
Sternal: running to the sternum;
Perforating: piercing the intercostal muscles in their route to the pectoral muscles;
Intercostal: running in the intercostal spaces;
Common trunks: combining the above mentioned types.
Numbers of all four types of ITA branches are shown in Table 3.
Table 3. Mean number of ITA branches.
| Type of branch | LITA | RITA |
|---|---|---|
| Sternal | 5.1 | 5.9 |
| Perforating | 4.8 | 1.9 |
| Intercostal | 6.8 | 5.7 |
| Common trunks | 3.1 | 3.2 |
RITA, right internal thoracic artery; LITA, left internal thoracic artery.
Discussion
Due to the fact that ITA has become the primary conduit for cardiac bypass surgery, many studies have generated fundamental anatomical knowledge for its clinical utilization.
The IMA usually has a separate origin from the subclavian artery. It occasionally has a common origin with the thyrocervical trunk, the scapular artery, the dorsal scapular artery, thyroid artery or costocervical trunk. On its way caudally, the artery first runs ventral to the pleural cupola, crossing the brachiocephalic vein underneath. It continues dorsal to the sternoclavicular joint and the costal cartilages and ventral to the parietal pleura. From the 3rd intercostal space the artery runs between the transversus thoracis muscle and the intercostal muscles where it gives off branches at each intercostal space. Between the 6th intercostal space and the seventh costal cartilage the ITA divides into the superior epigastric artery and the musculophrenic artery (1).
In our study the ITA always originates from the subclavian artery, in isolation or in association with another artery. It was observed that the right side was significantly longer than the left. In men the ITA was found to be longer than in women, probably due to the fact that the length of the thorax in women is generally shorter. The ITA was not found to be absent in any specimen in the present study as also observed in the series studied by Arnold et al., Henriquez et al., and Gupta et al. (2-4). The course of ITAs apart from being rectilinear showed a medial concavity in 22% (11/50) on the right and 18% (9/50) on the left side. Only one case of lateral concavity on the right side and no case of tortuosity was observed. Henriquez et al. reported rectilinear course in 34%, medial concavity in 30%, lateral concavity in 29%, and tortuosity in 7%.
In the present study the commonest level of termination of RITA and LITA was on the 6th intercostal space or the 6th rib as described in various textbooks of Anatomy. Our results concerning the type of termination were similar to that reported by Henriquez et al. (3).
The ITA is usually described to give sternal, intercostal, perforating, and common trunks (5). Sternal branches were arising directly from ITA as usually described by earlier workers and in textbooks of anatomy. In addition, our study agrees with Gupta et al., that there are sternal branches arising by a common stem with anterior intercostal and perforating arteries. The branching pattern of ITAs deserves more attention because in ITA dissections, eventually, there can be a diminishment of the sternal blood supply, which can lead to necrosis. Carrier et al. reported that after sternotomy and bilateral grafting of ITA, the decrease in blood supply to the sternum is only transient and is completely reverted one month after the operation (6). Green has also stated that important collateral blood vessels can provide a continued blood supply to the sternum even after bilateral mobilization of ITA (7).
The current results of our study are in complete concordance with other similar reports and indicate that knowledge of the anatomic characteristics of ITA is an invaluable signpost in coronary surgery.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hefel L, Schwabegger A, Ninković M, et al. Internal mammary vessels: anatomical and clinical considerations. Br J Plast Surg 1995;48:527-32. [DOI] [PubMed] [Google Scholar]
- 2.Arnold M. The surgical anatomy of sternal blood supply. J Thorac Cardiovasc Surg 1972;64:596-610. [PubMed] [Google Scholar]
- 3.Henriquez-Pino JA, Gomes WJ, Prates JC, et al. Surgical anatomy of the internal thoracic artery. Ann Thorac Surg 1997;64:1041-5. [DOI] [PubMed] [Google Scholar]
- 4.Gupta M, Sodhi L, Sahni D. The Branching Pattern of Internal Thoracic Artery On The Anterior Chest Wall. J Anat Soc India 2002;51:194-8. [Google Scholar]
- 5.Romanes GJ. Cunningham's Manual of Practical Anatomy: Volume II: Thorax and Abdomen. In: Romanes GJ, editor, The wall of the thorax. 15th ed. University Press Oxford 1996;15. [Google Scholar]
- 6.Carrier M, Grégoire J, Tronc F, et al. Effect of internal mammary artery dissection on sternal vascularization. Ann Thorac Surg 1992;53:115-9. [DOI] [PubMed] [Google Scholar]
- 7.Green GE. Sternotomy incision, mobilization, and routing of ITA grafts. In: Surgical revascularization of the heart. Green GE, Singh RN, Sosa JA, editors. New York: Igaku-Shoin, 1991:119-27. [Google Scholar]


