Introduction
Recurrent laryngeal nerve (RLN) injury is one of the most severe complications of thyroid surgery. Hoarseness due to unilateral RLN injury and breathing disorders and even asphyxia due to bilateral RLN injury can impose serious impacts on the patient’s life. It is estimated that the incidence of RLN injury during thyroid surgeries ranges 0.3-18.9% (1-5), making RLN protection a great concern among thyroid surgeons. Intraoperative neuromonitoring (IONM) combines both the functional and anatomic techniques and has the following features: intra-operative navigation and rapid identification of the RLN distribution; predicting nerve variation and protecting of the functional integrity of RLN; clarifying the mechanism and lowering the incidence of RLN injury; and easy to perform. It is a helpful adjunct for complicated surgeries (6,7).
With an attempt to help the surgeons thoroughly understand IONM and carry out this technique in a standardized and reasonable manner, the Chinese Thyroid Association established the Clinical Guidelines on IONM during Thyroid and Parathyroid Surgeries (China Edition).
Basic principles of IONM
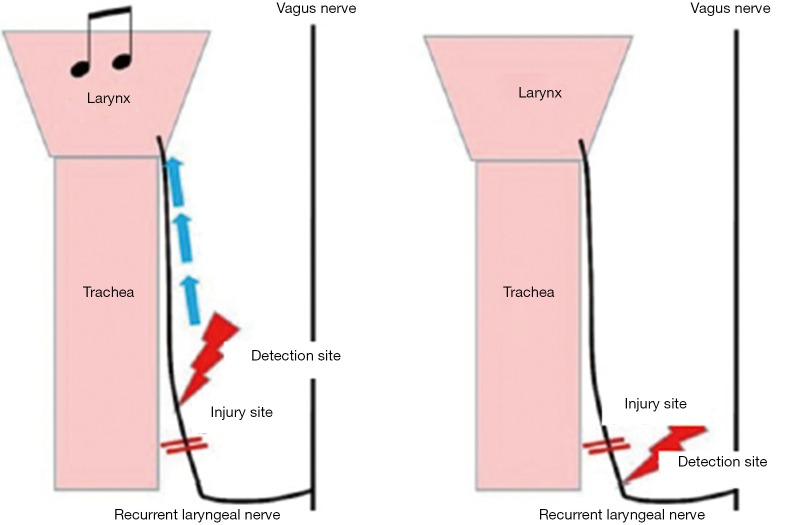
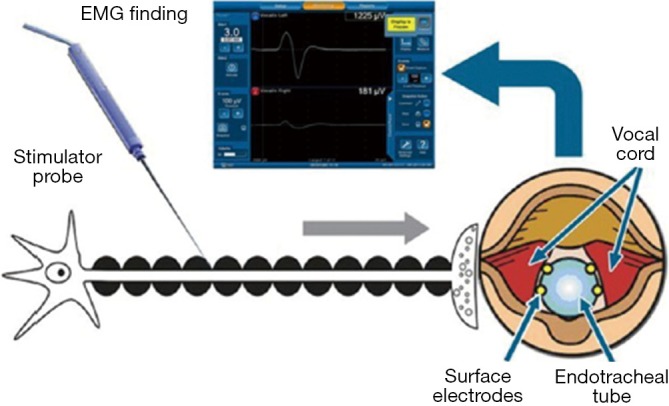
Application of IONM in thyroid surgeries was initially proposed by Shedd in 1966 and by Flisberg in 1970. Based on the principle of electrophysiology, the motor nerve is stimulated by electricity during the surgery, and then the nerve impulses are formed and transferred to the dominant muscles to produce myoelectric signals, forming waves and alerts in electromyography (EMG), which will help the surgeons to judge the functional integrity of nerves (8,9) (Figure 1).
Figure 1.
Basic principles of IONM. IONM, intraoperative neuromonitoring.
Clinical significance and technical advantages of IONM
For doctors who are transforming from generalist to specialist, junior doctors, and surgeons who are facing a complicated thyroid surgery, IONM undoubtedly is a good aid (10-12).
Facilitates the identification and locating of RLN
Before RLN exposure, the nerve can be accurately located at its distribution area using the cross method, which enables the doctor to rapidly determine the anatomic range of RLN as well as its rare anatomic variations such as non-recurrent RLN (13).
Facilitates the exposure and dissection of RLN
During the dissection of RLN, continuous monitoring together with naked-eye observation enables the differentiation between the monitored nerve and its surrounding non-nerve tissues and the accurate tracing of the nerve and its functional branches. Also, the intra-operative navigation is also helpful for the complete resection of lesions.
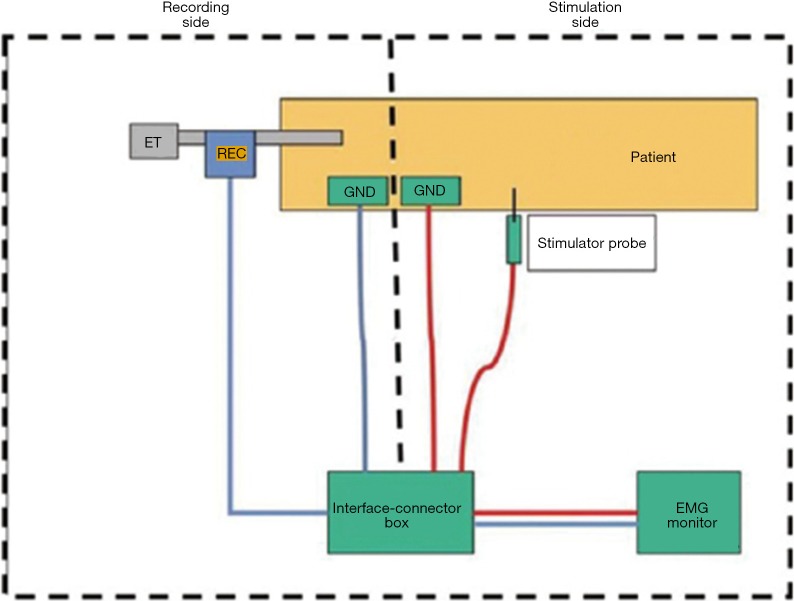
Facilitates the judgment of the functional integrity and injury mechanisms of nerves
Electrophysiological monitoring provides quantitative indicators for judging the functional integrity of nerves, can accurately locate the “injury point” of a nerve (14) (Figure 2), and help the operator to analyze the injury mechanism and timely recognize and resolve the injury during surgery. Thus, it can markedly reduce the incidence of RLN injury.
Figure 2.
Locating nerve “injury site” by IONM. IONM, intraoperative neuromonitoring.
Indications of IONM (15-18)
IONM is a preferred option in the following patients, while its application in the other patients should be upon the doctor’s recommendation: (I) the mass is located at the dorsal side of the thyroid, with suspected recent capsular hemorrhage or thyroid cancer; (II) in patients with hyperthyroidism, pre-operative ultrasound indicates large gland and rich blood supply; (III) in patients with malignant thyroid tumor, neck lymph node dissection is required, especially in patients with swollen central lymph nodes; (IV) patients receiving a second thyroid surgery but with disordered anatomic structures and severe adhesions; (V) patients with retrosternal goiter and/or large thyroid mass, along with suspected RLN dislocation; (VI) pre-operative imaging indicated the presence of transposition of viscera or subclavian artery variation, along with suspected non-recurrent RLN; (VII) patients with unilateral vocal cord paralysis, with the contralateral lobe requiring surgical treatment; (IX) patients requiring total thyroidectomy, in particular an endoscopic surgery; (X) patients requiring a surgery to repair RLN injury; (XI) patients requiring a parathyroid surgery; and (XII) patients with special requirements on sound and tone and thus requiring IONM.
Notably, (I) if intra-operative exploration shows that the thyroid cancer has completely infiltrated the RLN, nerve preservation will unavoidably result in residual tumor; thus, the invaded nerve must be resected to thoroughly remove the tumor. Under such circumstances, the post-operative hoarseness can not be avoided even after the application of IONM; (II) in patients with pre-operative vocal palsy, IONM can be applied to search for the injury site, and nerve repair can be completed with the assistance of IONM; however, it is difficult to completely restore the nerve function.
Since it is impossible to predict all the complex cases before a thyroid or parathyroid surgery, the indications of IONM may be widened if condition allows. The same recommendation has also proposed in international literature: since it is difficult to predict RLN variation before surgery, IONM may be routinely applied if condition allows.
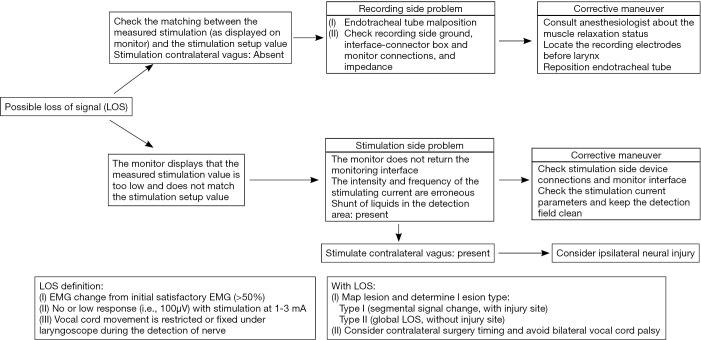
Essential monitoring devices of IONM
The IONM devices can be divided into recording side (recording electrode and its ground electrode) and stimulation side (stimulator probe and its loop electrodes) as well as EMG monitor, interface-connector box, anti-jamming silence detector, and patient simulators (19) (Figure 3).
Figure 3.
Basic monitoring equipment setup. ET, endotracheal tube; REC, recording electrodes; GND, ground electrodes; EMG, electromyography.
Needle-like electrode and intubation surface electrode are two typical recording electrodes, with the latter being routinely recommended (20).
The stimulation probes can be divided into monopolar and bipolar types, with the monopolar Prass probe with ball tip is routinely recommended (21).
Standardized procedures of IONM
Non-standard application of IONM techniques will cause significant monitoring errors. The main aim of standardized IONM procedures is to guide and improve the quality of IONM techniques and avoid any adverse effect due to improper monitoring operations (22-24). The standard procedure of IONM is shown in Table 1.
Table 1. The standard procedures of IONM.
| Procedures | Note |
|---|---|
| Record vocal cord movement before surgery | Use of fiberoptic laryngoscope |
| Recommended anesthesia method for IONM | Intermediate- or short-acting muscle relaxant is recommended for preoperative anesthesia induction. The dosage of intermediate-acting muscle relaxant is smaller than that used for routine anesthesia induction. 1x ED95 intermediate-acting non-depolarizing muscle relaxant is recommended; avoid adding muscle relaxant before the termination of intraoperative monitoring |
| Body position and tube placement | Anesthesia intubation is performed after positioning (intubation under video laryngoscope is recommended) |
| Device connections and checking | |
| The ground electrodes are routinely placed under the skin at the shoulders or xiphoid | |
| Confirm the monitoring system has been effectively established | |
| Check electrode impedance and differences in impedance values | Electrode impedance <5 kΩ, with deviations <1 kω |
| Check initial EMG | Initial fluctuations: about 10 μV |
| Set up event thresholds | Typically 100 μV |
| The current intensity of stimulator probe should be routinely set at 1-3 mA | |
| The monitoring device should be placed far away from electro-surgical devices and be connected with anti-jamming silence detectors | |
| The recording electrode positions should be confirmed during surgery | Directly detect, locate, and record the electrode depth at the antemedial laryngeal line using stimulator probe |
| IONM four-step method | |
| Step 1: V1 signal | Obvious bipolar EMG signal is obtained at the ipsolateral vagus nerve at the plexas thyreoidea inferior level (point B), confirming the successful establishment of the monitoring system. If signal is absent at point B, detect the vagus nerve at the plexas thyroid superior level (point A); the presence of signal at point A confirms the presence of non-recurrent laryngeal nerve (25) (Figure 4) |
| Step 2: R1 signal | Before the exposure of RLN, its EMG signal is located using the Cross method by applying the probe vertical to trachea at its traveling area and then parallel to trachea |
| Step 3: R2 signal | Continuous monitoring is applied during the dissection of RLN and the signal change is compared in a real-time manner. After the RLN is exposed, the most proximal end of the exposed part is detected for EMG signal |
| Step 4: V2 signal | After complete hemostasis is achieved at the surgical field, the EMG signal of the vagus nerve is detected before closing the incision |
| Signal analysis | |
| Basic EMG parameters | The biphasic waveform should be differentiated from the monophasic non-EMG artifacts |
| No obvious decrease in R2 and V2 signals | The basic EMG parameters include amplitude, latency and duration (26) (Figure 5); the RLN has intact function |
| Loss of R2 and V2 signals | If the RLN is injured during the surgical operation, detect the “injury site” and search for the injury cause* |
| Photo recording the exposed RLN during surgery | To confirm the RLN continuity (visual integrity) |
| Postoperative laryngoscopy | |
*, If no “injury site” is detected, it is important to determine whether there is a “real” loss of signal. (I) stimulate the nerve and then observe the contact between endotracheal tube electrode and vocal cord via a laryngoscope; (II) detect signals at vagus nerve and RLN again before closing the incision. IONM, intraoperative neuromonitoring; RLN, recurrent laryngeal nerve.
Figure 4.
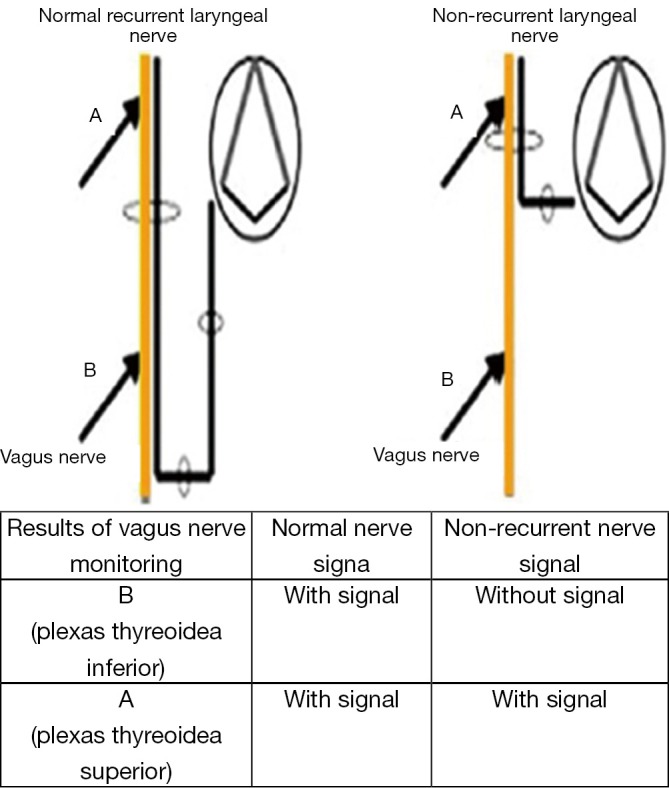
Monitoring setup of non-recurrent laryngeal nerve.
Figure 5.
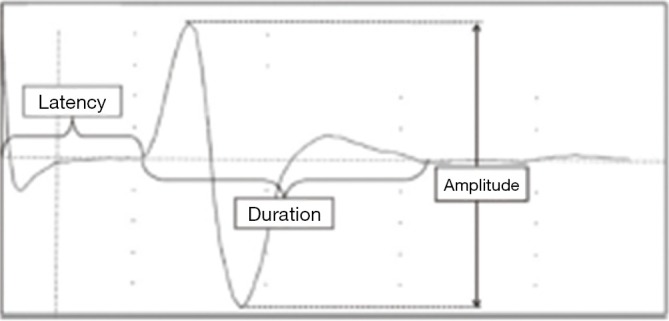
Basic parameters of the EMG wave of IONM. IONM, intraoperative neuromonitoring.
Causes and solutions of common IONM errors
The incidence of IONM error ranges 3.8-23.0% (27). IONM errors can bring great psychological pressure to the operator, delay the surgical process, and even cause the operator make wrong decision. Therefore, it is important to master the causes and solutions of common IONM errors, so as to ensure the surgery is performed in a safe and smooth manner. Table 2 lists the causes and solutions of common IONM errors, and the troubleshooting process (28) is displayed in Figure 6.
Table 2. Causes and solutions of common IONM errors.
| Common IONM errors | Causes | Solutions |
|---|---|---|
| Electrode impedance is too high | The subcutaneous electrodes have not completely removed after its withdrawal from patients | Check whether the subcutaneous electrodes fall off and keep the electrode clean |
| Subcutaneous electrodes >10 kΩ | The impedance of the electrode itself is too high | Replace the electrodes and fix them with tape |
| Stimulator probe electrodes >25 kΩ | The electrode core does not connect well with the interface-connector box | Check the connections of the interface-connector box |
| The interface-connector box does not connect well with the monitor | ||
| Recording electrodes | The recording electrode does not connect well with vocal cord | Adjust the tube depth and angle under fiberoptic laryngoscope |
| Single electrode impedance >5 kΩ | The surface electrode of endotracheal tube is displaced | Indwell the tube under conventional video laryngoscope |
| Impedance deviation>1 kΩ | Application of insulating lubricant before intubation | Avoid the application of insulating medium at the recording electrodes |
| Electrode impedance is zero | Two subcutaneous electrodes contact with each other | Re-indwell the subcutaneous electrodes, with the inter-electrode distance of >1 cm |
| Electrosurgical interference | The probe of anti-jamming detector is not connected | Circle the cable of the electrosurgical device, with the anti-jamming detector clipped on the twisted cable |
| After the establishment of standard monitoring system | Preoperative vocal cord palsy | Re-check the preoperative laryngoscopic records |
| Before thyroid surgery | The nerve detected by the operator is actually not a vagus nerve | Detect at 1 mA after confirming the exposure of vagus nerve |
| V1 signal is absent | The vagus nerve is injured during its exposure | Directly detect the carotid sheath at 3 mA to obtain the V1 signal |
| non-recurrent laryngeal nerve is present | If the signal of vagus nerve is absent at the plexas thyreoidea inferior level, re-check it at the plexas thyreoidea superior level | |
| Anesthesia induction is not performed as recommended | Wail until the muscle relaxant wears off or use a proper dose of a muscle relaxant antagonist | |
| Improper type or dosage of muscle relaxant | Check the matching between the measured stimulation (as displayed on monitor) and the stimulation setup value | |
| The detection current is not high enough | Re-check the connections between the electrodes and the interface-connector box | |
| Check whether the fuse in the interface-connector box has been burned out | ||
| The frequency of stimulus pulse is too low | Stimulus pulse frequency: 4 times/s by default | |
| The setup of event threshold is too high | Routinely 100 μV; avoid changing this parameter value casually | |
| The selected monitoring mode, channel, and volume are improper | Re-check the monitoring mode, channel, and volume setup | |
| The duration of detection for nerve is too short | Each detection should be maintained at least 1s | |
| The probe is damaged, with insulation layer falling off | Avoid reuse | |
| The shunt of the nerve detection area is too large | Clear liquids at the detection area | |
| The muscle for detecting neurological effects is detached from the recording electrode | Re-check whether the electrodes are off | |
| The depth of the surface electrodes of endotracheal tube can be detected and located at the laryngeal anteromedian line | ||
| EMG signal is present while no nerve is detected | Consecutive “sequence” EMG response cannot be explained | Light anesthesia, with spontaneous activity of laryngeal muscle; |
| Artifacts occur in the non-neural traveling area | the recording nerve or muscle is tracted by other nerve or muscle | |
| The detection current is too large | The surface electrode of endotracheal tube is placed too deeply | |
| Direct detect the nerve trunk (1 mA is recommended) | ||
| Adjust according to the anatomic structures and EMG signals during the surgery | ||
| V1 signal is good, confirming the establishment of standard monitoring system, whereas there is the decrease of signal by >50% or LOS during the dissection of RLN | Intraoperative anesthesia or muscle relaxation status changes | Avoid adding muscle relaxant before the termination of monitoring |
| Nerve transection injury | Check the nerve continuity | |
| Nerve injury not visible to the naked eye | Locate the injury site and analyze the possible injury mechanisms: traction injury, heat injury, suction injury, and/or thread-cutting injury | |
| Monitoring system failure | Re-check the electrode connections to ensure a good circuit performance | |
| Recording electrode displacement due to changes in head position or body position during the surgery | Use simulators to re-check the monitor and interface-connector box (e.g., fuse) | |
| Re-check the laryngoscope and adjust the endotracheal tube |
RLN, recurrent laryngeal nerve.
Figure 6.
Algorithm for troubleshooting common IONM errors. IONM, intraoperative neuromonitoring.
The standard application of IONM can help 85% of beginners to smoothly locate the laryngeal nerves, provide quantitative indicators of nerve function for surgeons, assist the surgeons to deal with the complicate anatomic structures and skillfully keep away from the dangerous areas. Also, by using both eyes and ears (by listening to the alerts), the operators can accurately resect the tumor. Thus, IONM has become an effect adjunct for the golden standard of naked-eye protection. With “simple, effective, and practicable” as the basic principles, the Clinical Guidelines on IONM during Thyroid and Parathyroid Surgeries (China Edition) established by Chinese Thyroid Association elucidates the standardized operation procedures and decision-making steps of IONM. Before the application of IONM, the surgeons need to fully know neuromonitoring systems and thoroughly understand the Guidelines and receive corresponding training and verification in a standardized monitoring base. With the assistance of IONM, an experienced surgeon will be able to further lower the incidence of RLN injury and improve the surgical safety and completeness, which can also be a new trend in laryngeal nerve protection during a thyroid surgery (29).
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 2004;136:1310-22. [DOI] [PubMed] [Google Scholar]
- 2.Chiang FY, Wang LF, Huang YF, et al. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery 2005;137:342-7. [DOI] [PubMed] [Google Scholar]
- 3.Chiang FY, Lee KW, Huang YF, et al. Risk of vocal palsy after thyroidecitomy with identification of the recurrent laryngeal nerve. Kaohsiung J Med Sci 2004;20:431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qu XC, Xiao Y, Huang T, et al. Exposure and injury prevention of recurrent laryingeal nerve during thyroid surgery. Chinese Journal of Cancer 2008;18:700-3. [Google Scholar]
- 5.Liu CP, Huang T. Causes and Treatment of Recurrent Laryngeal Nerve Injury during Thyroidectomy. Chin J Bases Clin General Surg 2008;15:314-7. [Google Scholar]
- 6.Dionigi G, Barczynski M, Chiang FY, et al. Why monitor the recurrent laryngeal nerve in thyroid surgery? J Endocrinol Invest 2010;33:819-22. [DOI] [PubMed] [Google Scholar]
- 7.Liu XL, Sun H, Zheng ZL, et al. Application and advances in the monitoring of recurrent laryngeal nerve during thyroid surgeries. Chinese Journal of general surgery, 2009;18:1187-90.
- 8.Sun H, Liu XL, Lian LX, et al. Principles and application of the monitoring of recurrent laryngeal nerve. News and Reviews (Ear, Nose, and Throat) 2012;27:137-40.
- 9.Zhou G, Jiang KW, Ye YJ, et al. Intraoperative assessment of recurrent laryngeal nerve function by monitoring EMG of lateral cricoaryteoid muscle. Chinese Journal of General Surgery 2012;27:272-5. [Google Scholar]
- 10.Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 2009;96:240-6. [DOI] [PubMed] [Google Scholar]
- 11.Dionigi G, Bacuzzi A, Boni L, et al. What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 2008;6 Suppl 1:S7-12. [DOI] [PubMed] [Google Scholar]
- 12.Sun H, Liu XL, Zhang DQ, et al. Clinical application of recurrent laryngeal nerve protection and monitoring during thyroidectomy. Chin J Bases Clin General Surg 2010;17:768-71. [Google Scholar]
- 13.Chiang FY, Lu IC, Chen HC, et al. Anatomical variations of recurrent laryngeal nerve during thyroid surgery: how to identify and handle the variations with intraoperative neuromonitoring. Kaohsiung J Med Sci 2010;26:575-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiang FY, Lu IC, Kuo WR, et al. The mechanism of recurrent laryngeal nerve injury during thyroid surgery--the application of intraoperative neuromonitoring. Surgery 2008;143:743-9. [DOI] [PubMed] [Google Scholar]
- 15.Sun H, Liu XL, Fu YT, et al. Application of intraoperative neromonitoring during complex thyroid operation. Chinese Journal of Practical Surgery 2010;30:66-8. [Google Scholar]
- 16.Qin JW, Hei H, Zhuang ST, et al. Locating and protecting recurrent laryngeal nerve in minimally invasive video-assisted thyroidectomy. Cancer Research and Clinic 2010;12:804-5. [Google Scholar]
- 17.Wei T, Li ZH, Zhu JQ. Real-Time Monitoring of Recurrent Laryngeal Nerve During Thyroid Reoperation. Chin J Bases Clin General Surg 2010;17:772-4. [Google Scholar]
- 18.Wang P, Yan HC. Prevention and treatment of complications after complete endoscopic thyroidectomy. Journal of Laparoscopic Surgery 2012;17: 806-9. [Google Scholar]
- 19.Randolph GW, Dralle H, International Intraoperative Monitoring Study Group, et al . Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121 Suppl 1:S1-16. [DOI] [PubMed] [Google Scholar]
- 20.Liu XL, Sun H. Principles and clinical application of intraoperative monitoring of recurrent laryngeal nerve. Chinese Journal of Practical Surgery 2012;32:409-11. [Google Scholar]
- 21.Sun H, Liu XL, Zhao T, et al. New methods for identifying recurrent laryngeal nerve during thyroid surgery. News and Reviews (Ear, Nose, and Throat) 2010;25:46-8.
- 22.Chiang FY, Lee KW, Chen HC, et al. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg 2010;34:223-9. [DOI] [PubMed] [Google Scholar]
- 23.Randolph GW, Kamani D. The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery 2006;139:357-62. [DOI] [PubMed] [Google Scholar]
- 24.Liu XL, Sun H. Optimization and interpretation of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. News and Reviews (Ear, Nose, and Throat) 2010;25:152-4.
- 25.Sun H, Liu XL, Zhao T, et al. Intraoperative neuromonitoring in identification of non-recurrent laryngeal nerve: experience of 6 cases. Chin J Endocr Surg 2010;4:402-4. [Google Scholar]
- 26.Dralle H, Sekulla C, Lorenz K, et al. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 2008;32:1358-66. [DOI] [PubMed] [Google Scholar]
- 27.Chan WF, Lo CY. Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 2006;30:806-12. [DOI] [PubMed] [Google Scholar]
- 28.Sun H, Liu XL. The preservation method of the recurrent laryngeal nerve and superior laryngeal nerve in the thyroid surgery. Chinese Journal of Practical Surgery 2012;32:356-9. [Google Scholar]
- 29.Tian W, Luo J. Comparison of the guidelines on the management of thyroid nodules and differentiated thyroid cancer between China and the United States. Chinese Journal of Practical Surgery 2013;33:475-9. [Google Scholar]