Abstract
Background:
Coronary heart disease (CHD) is an important cause of morbidity and mortality in Pakistan. The temporal trends in the risk factors for myocardial infarction (MI) and the impact of socioeconomic status on these risk factors remain ambiguous.
Objectives:
The objectives of the present analysis were to investigate the potential association between various risk factors and MI in North Punjab, Pakistan, and to assess the status of the control of the risk factors associated with MI in this population.
Patients and Methods:
The present study included 515 patients admitted to the coronary care units or equivalent cardiology wards of the participating hospitals between 2011 and 2012 in North Punjab, Pakistan. The analysis was focused on identifying the socioeconomic status, lifestyle, family history of MI, and risk factors (i.e. hypertension, diabetes, smoking, and hyperlipidemia). A structured questionnaire was designed to collect data. The lipid profile was recorded from the investigation chart of every patient. For statistical analysis, the Kruskal Wallis, Mann-Whitney U, Wilcoxon, and chi-square tests were used.
Results:
MI was common in the males at the age of 41 - 60 years as compared to the females (P = 0.015). Patients with a positive parental history of CHD experienced MI at a younger age (P = 0.0001) at a body mass index (BMI) ≤ 25 kg/m2. Sedentary lifestyle (70%) and smoking (60%) had a male predominance. Hypertension accounted for nearly 37%, hyperlipidemia 26%, and diabetes 19.4% of the rural and urban subjects (P < 0.01). High-density lipoprotein cholesterol decreased (up to 34 mg/dl), while low-density lipoprotein cholesterol and hypertension increased with age. The mean monthly cost of medicines and physicians’ fees per patient was 2381.132 Pakistani Rupees (24.24 USD).
Conclusions:
Higher BMI, positive family history, smoking, hypertension, hyperlipidemia, and diabetes were the strong predictors of MI in North Punjab, Pakistan. Preventive efforts are needed to start early in life and continue throughout the life course.
Keywords: Myocardial Infarction, Smoking, Hypertension, Diabetes
1. Background
Coronary heart disease (CHD) is the cause of 17.1 million deaths per year throughout the world (1). Thus, CHD is today the largest single contributor to global mortality and will continue to dominate mortality trends in the future. It has been reported that the majority of deaths (39%) in low- and middle-income countries under the age of 70 years are due to CHD (2). Myocardial Infarction (MI) is one of the major complications of CHD. The Asian population is more susceptible to MI (3, 4). It has been estimated that MI is 50% higher in South Asians than in white people in the UK (5).
Pakistan is a developing South Asian country with a population of over 187 million (6). The majority of the population of Pakistan (67.5%) live in rural areas and bear the greatest burden of heart disease (7). The Framingham study (1961, cited in Kannel) reported that obesity, hypertension, smoking, diabetes mellitus, and hypercholesterolemia were the major risk factors for the onset of CHD (8). Another study showed that the high prevalence of MI risk factors in Pakistan with more than 30% of the population over 45 years of age is affected by this disease (2). Punjab is the most developed and populated province accounting for more than 45% of the entire population of Pakistan (9). However, there is a paucity of data on the estimates of CHD risk factor burden or of its control status in Punjab, Pakistan. Moreover, only a little information on MI risk factors has been reported in Peshawar and Rahim yar khan, Pakistan (7).
2. Objectives
The objectives of the present study were to collect epidemiological data on MI in North Punjab and to evaluate the environmental risk factors responsible for MI with a view to lessening the disease burden through modifications in lifestyle.
3. Patients and Methods
3.1. Study Design
This population-based study was carried out in six regions of North Punjab, Pakistan. The urban population from Lahore and Islamabad and the rural population from Faisalabad, Gujranwala, Gujrat, and Sialkot were included in this survey. A total of 515 MI patients were included in this study and divided into 250 urban and 265 rural MI patients.
3.2. Data Collection
Data were collected by trained qualified staff from the patients admitted to coronary care units (CCU) or equivalent cardiology wards of the participating hospitals. The patients were screened to identify the MI cases. This study was conducted in accordance with the Good Clinical Practice (GCP) guidelines (declaration of Helsinki). The study protocol was approved by the Ethics Committee of Advanced Studies and Research (ref# AEG-A-AD-25-17/ZOOL/09). Written informed consent was obtained from all the participants. All the cases were enrolled between 2011 and 2012. The participation rate of the patients was 65%. Excluded subjects were 285 out of 800 because of incomplete data on variables. Thus, 515 subjects were included in this study. The inclusion criteria were comprised of MI as the principal diagnosis and admission via the CCU and emergency wards. The diagnosis of MI was based on severe chest pain of 30 minutes duration, characteristic electrocardiographic (ECG) patterns of MI, and significant elevation in cardiac enzymes such as creatine kinase-myocardial band (CK-MB). A structured questionnaire was designed to collect data. The analysis was focused on identifying the socioeconomic status (i.e. income and education), lifestyle (i.e. smoking, leisure time, and physical activity), dietary pattern, personal and family history of MI, and risk factors such as blood pressure, diabetes, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). At this point, arterial pressure was measured three times using a sphygmomanometer. According to the European Society of Hypertension/European Society of Cardiology (ESH/ESC) criteria, cases with systolic blood pressure > 140 mmHg and diastolic blood pressure > 90 mmHg as well as those with a previous history of hypertension and current consumption of antihypertensive medication for blood pressure control were considered hypertensive. Weight and height were also measured in order to calculate the body mass index (BMI) using the formula: weight (in kilograms) divided by the square of height (in meters). Cases with a BMI between 25 and 29 were considered overweight and subjects with a BMI ≥ were considered obese, while those with a total cholesterol level ≥ 200 mg/dl were considered hypercolesterolemics. Fasting blood samples (3 ml - 5 ml) of all the participants were collected by trained staff and were sent to the laboratories of the participating hospitals for lipid profile and blood sugar measurement. Subjects with a fasting glucose level ≥ 126 mg/dl were considered hyperglycemic, and those with a history of diabetes mellitus and using glucose-lowering medicines were considered diabetic. Disease treatment cost was expressed in Pakistani Rupees (Rs). Patients not willing to sign the consent form and those with previous illnesses associated with hepatic and renal failure, human immunodeficiency virus (HIV), or cancer were excluded from the study.
3.3. Data Analysis
Statistical analysis was performed using the R version 2.11. A descriptive analysis was conducted, and the study variables were checked for normal distribution. The Kruskal Wallis, Mann-Whitney U, and chi-square tests were utilized in order to check associations between the different variables. A two-sample two-tailed t-test (pooled variances) for a P value < 0.05 was considered statistically significant.
4. Results
The total number of the male patients was 356 (69.13%) as compared to 159 (30.88%) females in this study. The mean age of the participants from the rural areas was 56.8 ± 14.34 and from the urban areas was 55.7 ± 11.26 with a range of 20 - 80 years, while 53.79% of the patients were in the range of 41 - 60 years of age (P = 0.270) among the rural and urban populations in both genders. Tables 1 and 2 show that among the urban and rural populations, MI was much more common in the males than in the females (P = 0.015), which was highly statistically significant. However, the male MI patients were younger than their female counterparts. The relative difference regarding the MI prevalence between the sexes was greater among the younger subjects of up to 60 years old and smaller among the subjects of more than 60 years of age. The majority of the MI females were aged over 60 years. The demographic characteristics of the male and female subjects are summarized in Table 1.
Table 1. Demographic Distribution of Myocardial Infarction a,b,c.
| Variables | Women | Men | Total | ||
|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | ||
| No. | 95 (18.45) | 64 (12.43) | 170 (33.01) | 186 (36.12) | 515 (100) |
| Age, y | |||||
| 20 - 40 | 11 (2.14) | 4 (0.78) | 27 (5.24) | 21 (4.08) | 63 (12.23) |
| 41 - 60 | 54 (10.48) | 26 (5.05) | 82 (15.92) | 115 (22.33) | 277 (53.79) |
| ≥ 61 | 30 (5.82) | 34 (6.60) | 61 (11.84) | 50 (9.71) | 175 (33.98) |
| BMI, Kg/m 2 c | |||||
| ≤ 25 | 65 (12.62) | 17 (3.30) | 140 (27.18) | 69 (13.40) | 291 (56.50) |
| > 25 | 30 (5.82) | 47 (9.13) | 30 (5.82) | 117 (22.72) | 224 (43.50) |
| Mean ± Standard Deviation | 23.75 ± 3.88 | 29.04 ± 5.46 | 22.60 ± 3.27 | 29.22 ± 22.89 | 26.00 ± 14.42 |
| Family history | |||||
| -ve Family history | 8 (1.55) | 22 (4.27) | 22 (4.27) | 92 (17.86) | 144 (27.96) |
| +ve Family History | 87 (16.89) | 42 (8.15) | 148 (28.74) | 94 (18.25) | 371 (72.04) |
| Education | |||||
| Illiterate | 50 (9.71) | 36 (6.99) | 49 (9.51) | 66 (12.82) | 201 (39.03) |
| Primary | 27 (5.24) | 11 (2.14) | 50 (9.71) | 48 (9.32) | 136 (26.41) |
| College and above | 18 (3.50) | 17 (3.30) | 71 (13.79) | 72 (13.98) | 178 (34.56) |
| Marital status | |||||
| Married | 93 (18.06) | 62 (12.04) | 158 (30.68) | 178 (34.56) | 491 (95.34) |
| Single | 2 (0.39) | 2 (0.39) | 12 (2.33) | 8 (1.55) | 24 (4.66) |
| Employment status | |||||
| Jobless | 73 (14.17) | 22 (4.27) | 71(13.79) | 47 (9.13) | 213 (41.36) |
| Laborer | 5 (0.97) | 20 (3.88) | 3 (0.58) | 56 (10.87) | 84 (16.31) |
| Housewife | 9 (1.75) | 15 (2.91) | 3 (0.58) | 12 (2.33) | 39 (7.57) |
| Office job/business | 8 (1.55) | 7 (1.36) | 93 (18.06) | 71 (13.79) | 179 (34.76) |
a Data are presented as No. (%) or mean ± SD.
b Rural, Rural Population (Faisalabad, Gujranwala, Gujrat, and Sialkot); Urban, Urban Population (Lahore and Islamabad).
c The body mass index was considered normal at ≤ 25 and overweight at > 25 for both men and women according to the World Health Organization. Bold letters denote greater values.
Table 2. Co-Morbid Conditions and Types of Myocardial Infarction a,b,c.
| Variables | Rural | Urban | Total | P Values |
|---|---|---|---|---|
| Number of patients | 265 (51.4) | 250 (48.5) | 515 (100) | |
| STEMI | 152 (30) | 138 (27) | 290 (56) | 0.657 |
| NSTEMI | 113 (22) | 112 (22) | 225 (44) | 0.657 |
| Smoking | 0.205 | |||
| Smokers | 169 (33) | 145 (28) | 314 (60) | |
| Non-smokers | 96 (19) | 105 (21) | 201 (39) | |
| Life style | 0.0001 | |||
| Sedentary | 151 (29) | 213 (41) | 364 (70) | |
| Physical activity | 114 (22) | 37 (7) | 151 (29) | |
| Other Complications | 1e-8 c | |||
| Diabetes | 35 (7) | 65 (13) | 100 (19.4) | |
| Hypertension | 90 (17) | 100 (19.4) | 190 (37) | |
| Hyperlipidemia | 100 (19.4) | 35 (7) | 135 (26) | |
| Risk Factors ≥ 2 | 40 (8) | 50 (8) | 90 (17) | |
| Age, y | 0.270 | |||
| ≤ 40 | 38 | 25 | 63 | |
| 41 - 60 | 136 | 141 | 277 | |
| ≥ 61 | 91 | 84 | 175 | |
| Mean | 56.83 | 55.79 | 0.523 | |
| Gender | ||||
| Male | 170 | 186 | 356 | 0.0154 |
| Female | 95 | 64 | 159 |
a Abbreviations; NSTEMI, Non-ST-Segment Elevation Myocardial Infarction; and STEMI, ST-Segment Elevation Myocardial Infarction.
b Data are presented as No. (%).
c P < 0.05.
4.1. Co-Morbid Conditions and Family History Related to Myocardial Infarction
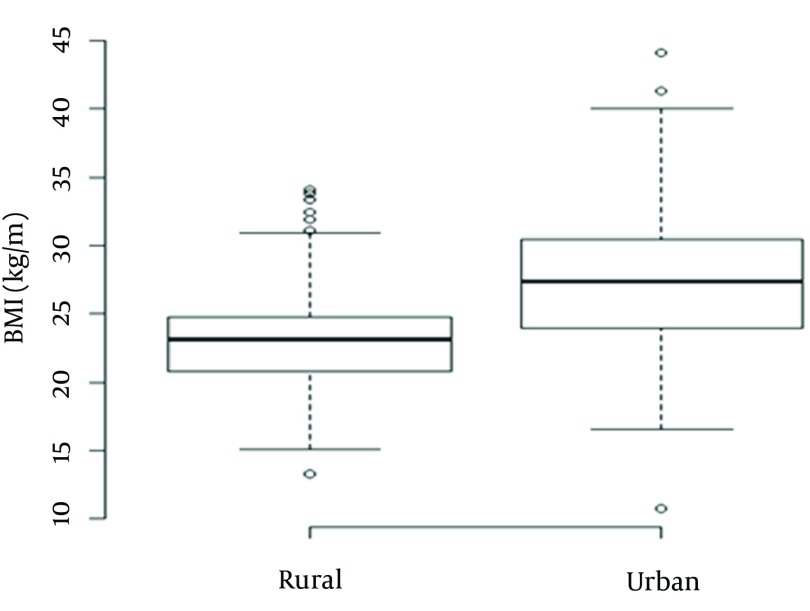
Smoking was more common (Table 2) in the MI patients in the rural areas (33%) than those in the urban areas (28%) (P = 0.205). None of the female patients ever smoked as compared to the males. Twenty-six percent of the selected MI cases had hyperlipidemia (cholesterol level ≥ 200 mg/dl). The prevalence of hypertension was 36% as compared to diabetes (19.4%) in the MI patients (Table 2). As is evident in Tables 3 and 4, the HDL-C level reduced, while the LDL-C level and hypertension rose with age. As is shown in Figure 1, the patients with a first-degree relative positive family history experienced MI at a younger age at a BMI ≤ 25.
Table 3. Risk Factors by Age Group and Gender in the Urban Population a.
| Age, y | ≤ 40 (n = 25) | 40 - 60 (n = 141) | > 60 (n = 84) | |||
|---|---|---|---|---|---|---|
| Gender | Male | Female | Male | Female | Male | Female |
| BMI, mean ± SD | 28.38 ± 5.42 | 29.28 ± 4.58 | 26.79 ± 5.41 | 28.26 ± 5.71 | 26.39 ± 4.27 | 29.61 ± 5.42 |
| STEMI, n | 11 | 3 | 69 | 12 | 28 | 15 |
| NSTEMI, n | 10 | 1 | 46 | 14 | 22 | 19 |
| Non-smokers, n | 4 | 4 | 30 | 24 | 12 | 31 |
| Smokers, n | 17 | 0 | 85 | 2 | 38 | 3 |
| Family history, n | 16 | 4 | 56 | 18 | 22 | 20 |
| Sedentary life, n | 14 | 2 | 100 | 25 | 41 | 31 |
| Physical activity, n | 7 | 2 | 15 | 1 | 9 | 3 |
| Diabetes, n | 4 | 1 | 37 | 8 | 1 | 5 |
| Hypertension, n | 10 | 1 | 24 | 28 | 27 | 10 |
| Hyperlipidemia, n | 6 | 0 | 12 | 2 | 11 | 3 |
| HDL Cholesterol, mg/dl | 37 | 45 | 34 | 38 | 32 | 34 |
| LDL Cholesterol, mg/dl | 135 | 124 | 140 | 130 | 145 | 148 |
a Abbreviations: BMI, Body Mass Index; HDL, High-Density Lipoprotein; LDL, Low-Density Lipoprotein; NSTEMI, Non-ST-Segment Elevation Myocardial Infarction; and STEMI, ST-Segment Elevation Myocardial Infarction.
Table 4. Risk Factors by Age Group and Gender in the Rural Population a.
| Age, y | ≤ 40 (n = 25) | 40 - 60 (n = 141) | > 60 (n = 84) | |||
|---|---|---|---|---|---|---|
| Gender | Male | Female | Male | Female | Male | Female |
| BMI, mean ± SD | 22.36 ± 2.53 | 23.06 ± 6.00 | 23.28 ± 3.36 | 24.39 ± 3.43 | 21.80 ± 3.27 | 22.85 ± 3.63 |
| STEMI, n | 18 | 5 | 48 | 29 | 38 | 14 |
| NSTEMI, n | 9 | 6 | 34 | 25 | 23 | 16 |
| Non-smokers, n | 9 | 11 | 37 | 54 | 35 | 23 |
| Smokers, n | 18 | 0 | 45 | 0 | 26 | 7 |
| Family history, n | 22 | 9 | 74 | 49 | 52 | 29 |
| Sedentary life, n | 16 | 5 | 44 | 34 | 37 | 15 |
| Physical activity, n | 11 | 6 | 38 | 20 | 24 | 15 |
| Diabetes, n | 3 | 2 | 5 | 5 | 10 | 10 |
| Hypertension, n | 7 | 5 | 20 | 20 | 26 | 12 |
| Hyperlipidemia, n | 8 | 1 | 23 | 18 | 36 | 14 |
| HDL Cholesterol, mg/dl | 30 | 38 | 40 | 43 | 40 | 42 |
| LDL Cholesterol, mg/dl | 121 | 125 | 130 | 128 | 140 | 141 |
a Abbreviations; BMI, Body Mass Index; HDL, High-Density Lipoprotein; LDL, Low-Density Lipoprotein; NSTEMI, Non-ST-Segment Elevation Myocardial Infarction; and STEMI, ST-Segment Elevation Myocardial Infarction.
Figure 1. Relationship between the Body Mass Index (kg/m2) and Family History.
4.2. Economic Burden
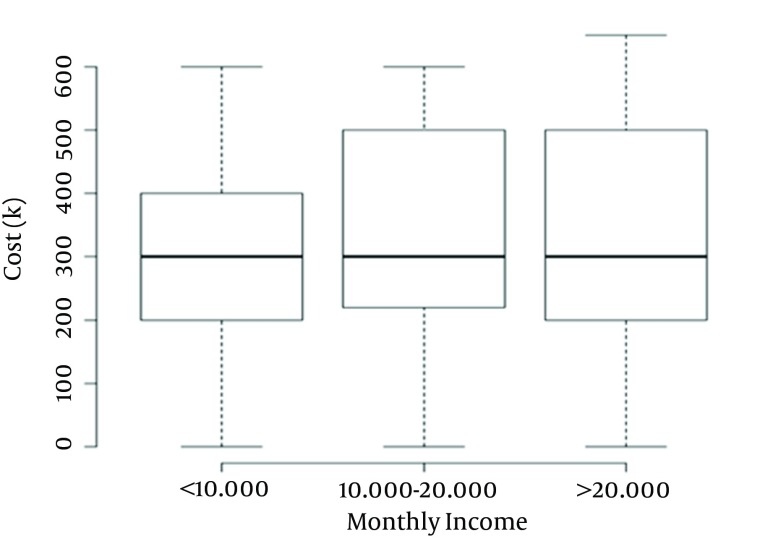
Figure 2 depicts the relationship between the monthly income and the overall cost (i.e. ECG, computerized tomography (CT scan), angiography, surgery, and medication) of the MI patients (P = 0.917). According to the Kruskal test, however, this relationship did not constitute statistical significance. The mean monthly cost of medicines and physicians’ fees was 2381.132 Rs (24.24 USD).
Figure 2. Relationship Between the Surgery Cost and Monthly Income of the Myocardial Infarction Patients.
K: means over one hundred.
5. Discussion
Risk factors associated with CHD in the Pakistani population have been relatively insufficiently studied (10). Nevertheless, a thorough knowledge of these factors in the different regions of Punjab, Pakistan, is of a great importance in order to develop national health strategies for their control. The current study found that CHD and its risk factors such as hypertension, diabetes, and obesity are on the increase in our country. Our data revealed that the male MI patients from the rural and urban areas of Punjab, Pakistan, were relatively young (41 - 60 years). Gender difference was also common among our study population (P = 0.015), which chimes in with previous studies reporting that middle-aged men have 2 to 5 times higher risk of MI than women (11, 12). Women of young age are protected from the risk of CHD (13), and hormone replacement therapy reduces the risk of heart disease in postmenopausal women (14). Estrogen is thought to be a major contributor to premenopausal women’s tendency to have normal blood pressure, higher levels of HDL-C, and lower triglyceride levels compared to men (15, 16).
In the current study, a high prevalence of overweight was found among the patients from the urban areas (P = 0.0041) as compared to those from the rural areas. This may be due to less physical inactivity and unhealthy dietary practice, encompassing the high consumption of saturated fats and refined carbohydrates as well as the low consumption of fruits and vegetables among the residents of urban areas. Gupta et al. (17) reported that a higher BMI had a positive relationship with MI. Our data on the BMI demonstrated that the patients with a positive family history of MI suffered heart disease even at a lower BMI ≤ 25, which may be due to consanguineous marriages in Pakistan (18).
Our results showed that a 56% ST-elevation myocardial infarction (STEMI) continues to be a major public health concern in Pakistan. Badran et al. (19) also underlined STEMI, by comparison with non-ST-elevation myocardial infarction (NSTEMI), as a major issue in Pakistan.
In our study, sedentary lifestyle (70%) and smoking (60%) were reported predominantly among the male MI patients. Smoking deteriorates HDL-C (14), raises the blood pressure, and releases free radicals which are injurious to heart’s health. Wu et al. (20) reported that the cessation of smoking can reduce the risk of heart disease by 65%. Non-smokers exposed to passive smoking are also at great risk of MI. Faisal et al. (21) reported a 26% prevalence rate of sedentary lifestyle among patients with CHD in Peshawar, Pakistan. Furthermore, smokers of all age groups have 2 - 3 times higher death rates than non-smokers (22). It has also been proven by an animal study that physical exercise improves the left ventricular function (23).
In the present study, hypertension (36%) emerged as the most important risk factor for the onset of MI, and its incidence was much higher among the patients from the urban areas than among those from the rural regions. This finding is concordant with the results of a previous study reporting that hypertension is much higher in Pakistan than in the other South Asian countries (24). Hypertension is one of the most important risk factors responsible for atherosclerotic events (25). Similar to serum cholesterol, the blood pressure also tends to increase with age, and more prominently in women than in men (26). In our study, hyperlipidemia and diabetes were detected in 26% and 19.4% of our MI patients, respectively. According to the INTERHEART study, hyperlipidemia is a significant risk factor for CHD in South Asia (27). Type II diabetes is a major public health issue in Pakistan (28) and is an important cause of cardiovascular disease (29, 30). The data available in the literature show a more frequent occurrence of other CHD risk factors among diabetic patients (31). Our data showed that LDL-C increased with age. An earlier study reported that plasma LDL-C increases by about 40% between 20 and 60 years of age (32).
Low- and middle-income individuals are faced with a great socioeconomic burden in the pursuit of their treatments. The diagnosis of heart disease via ECG, CT scan, echocardiography, and angiography is costly, while the main burden of disease faced by the patient is at the time of surgery. Our data showed that the mean calculated cost per patient for surgery was 600000 Rs (6108.19 USD), which sometimes drastically affects the financial capacity of the patient. The treatment of CHD is a constant, life-long process. Indeed, patients have to consult their physicians every month, and medicines as well as physicians’ fees are expensive. In our study, the mean calculated monthly cost of medicines and physicians’ fees per patient was 2381.132 Rs (24.24 USD). Even low-income patients are compelled to pay these high expenses, which may contribute to hypertension. One-third of Pakistani people live in poverty and as such cannot afford the increasing burden of such a costly disease.
Our data demonstrated that the MI patients living in the urban areas, in comparison with those living in the rural regions, had a high level of MI risk factors (i.e. physical inactivity, hypertension, and diabetes) and should, therefore, be treated as a high-risk group for prevention and treatment. Moreover, this study demonstrated that effective risk factor control is still poor in Punjab, Pakistan. Accordingly, public health programs, comprising lifestyle interventions and different pharmacological therapies, should be implemented in order to reduce the risk of CHD in Pakistan. Preventive efforts are needed to start early in life and should continue throughout the life course.
The most significant limitation of the present study is its small sample size of MI patients from Punjab Province, Pakistan. Be that as it may, our findings could assist in future well-targeted intervention and awareness campaigns, aimed at residents of urban areas in particular, with a view to lessening the burden of CHD. Our findings, however, require confirmation by further research.
Acknowledgments
This study was financially supported by a grant from the Higher Education Commission (H.E.C.), Islamabad, Pakistan.
References
- 1.Siddiqui TI, Kumar KSA, Dikshit DK. Platelets and atherothrombosis: causes, targets and treatments for thrombosis. Curr Med Chem. 2013;20(22):2779–97. doi: 10.2174/0929867311320220004. [DOI] [PubMed] [Google Scholar]
- 2.Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kearney P, Whelton M, Reynolds K, Muntner P, Whelton P, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 4.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 5.Bellary S, O'Hare JP, Raymond NT, Mughal S, Hanif WM, Jones A, et al. Premature cardiovascular events and mortality in south Asians with type 2 diabetes in the United Kingdom Asian Diabetes Study - effect of ethnicity on risk. Curr Med Res Opin. 2010;26(8):1873–9. doi: 10.1185/03007995.2010.490468. [DOI] [PubMed] [Google Scholar]
- 6.Gaafar T, Moshni E, Lievano F. The challenge of achieving measles elimination in the eastern Mediterranean region by 2010. J Infect Dis. 2003;187 Suppl 1:S164–71. doi: 10.1086/368035. [DOI] [PubMed] [Google Scholar]
- 7.Rizvi SF, Khan MA, Kundi A, Marsh DR, Samad A, Pasha O. Status of rheumatic heart disease in rural Pakistan. Heart. 2004;90(4):394–9. doi: 10.1136/hrt.2003.025981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kannel W. Risk stratification in hypertension: new insights from the Framingham study*1. Am J Hypertension. 2000;13(1):S3–S10. doi: 10.1016/s0895-7061(99)00252-6. [DOI] [PubMed] [Google Scholar]
- 9.Shafique K, Mirza SS, Mughal MK, Arain ZI, Khan NA, Tareen MF, et al. Water-pipe smoking and metabolic syndrome: a population-based study. PLoS One. 2012;7(7):e13776. doi: 10.1371/journal.pone.0039734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–53. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 11.Willcox BJ, He Q, Chen R, Yano K, Masaki KH, Grove JS, et al. Midlife risk factors and healthy survival in men. JAMA. 2006;296(19):2343–50. doi: 10.1001/jama.296.19.2343. [DOI] [PubMed] [Google Scholar]
- 12.Reis JP, Loria CM, Lewis CE, Powell-Wiley TM, Wei GS, Carr JJ, et al. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA. 2013;310(3):280–8. doi: 10.1001/jama.2013.7833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toyofuku M, Goto Y, Matsumoto T, Miyao Y, Morii I, Daikoku S, et al. [Acute myocardial infarction in young Japanese women]. J Cardiol. 1996;28(6):313–9. [PubMed] [Google Scholar]
- 14.Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation. 1999;99(9):1165–72. doi: 10.1161/01.cir.99.9.1165. [DOI] [PubMed] [Google Scholar]
- 15.Wenger NK. Coronary disease in women. Annu Rev Med. 1985;36:285–94. doi: 10.1146/annurev.me.36.020185.001441. [DOI] [PubMed] [Google Scholar]
- 16.Reslan OM, Khalil RA. Vascular Effects of Estrogenic Menopausal Hormone Therapy. Reviews on Recent Clinical Trials. 2012;7(1):47–70. doi: 10.2174/157488712799363253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta R, Rastogi P, Sarna M, Gupta VP, Sharma SK, Kothari K. Body-mass index, waist-size, waist-hip ratio and cardiovascular risk factors in urban subejcts. J Assoc Physicians India. 2007;55:621–7. [PubMed] [Google Scholar]
- 18.Ul Haq F, Jalil F, Hashmi S, Jumani MI, Imdad A, Jabeen M, et al. Risk factors predisposing to congenital heart defects. Ann Pediatr Cardiol. 2011;4(2):117–21. doi: 10.4103/0974-2069.84641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Badran HM, Elnoamany MF, Khalil TS, Eldin MM. Age-related alteration of risk profile, inflammatory response, and angiographic findings in patients with acute coronary syndrome. Clin Med Cardiol. 2009;3:15–28. doi: 10.4137/cmc.s2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu F, Chen Y, Parvez F, Segers S, Argos M, Islam T, et al. A prospective study of tobacco smoking and mortality in Bangladesh. PLoS One. 2013;8(3):e13776. doi: 10.1371/journal.pone.0058516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faisal AW, Ayub M, Waseem T, Khan RS, Hasnain SS. Risk factors in young patients of acute myocardial infarction. J Ayub Med Coll Abbottabad. 2011;23(3):10–3. [PubMed] [Google Scholar]
- 22.Pratipanawatr T, Rawdaree P, Chetthakul T, Bunnag P, Ngarmukos C, Benjasuratwong Y, et al. Smoking and death in Thai diabetic patients: the Thailand Diabetic Registry cohort. J Med Assoc Thai. 2013;96(3):280–7. [PubMed] [Google Scholar]
- 23.de Waard MC, Duncker DJ. Prior exercise improves survival, infarct healing, and left ventricular function after myocardial infarction. J Appl Physiol (1985). 2009;107(3):928–36. doi: 10.1152/japplphysiol.91281.2008. [DOI] [PubMed] [Google Scholar]
- 24.Dodani S, Mistry R, Khwaja A, Farooqi M, Qureshi R, Kazmi K. Prevalence and awareness of risk factors and behaviours of coronary heart disease in an urban population of Karachi, the largest city of Pakistan: a community survey. J Public Health (Oxf). 2004;26(3):245–9. doi: 10.1093/pubmed/fdh154. [DOI] [PubMed] [Google Scholar]
- 25.McGee DL, Diverse Populations C. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15(2):87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 26.Flack JM, Neaton JD, Daniels B, Esunge P. Ethnicity and Renal Disease: Lessons From the Multiple Risk Factor Intervention Trial and the Treatment of Mild Hypertension Study. Am J Kidney Dis. 1993;21(4):31–40. doi: 10.1016/s0272-6386(12)80859-6. [DOI] [PubMed] [Google Scholar]
- 27.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52. doi: 10.1016/s0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 28.Rees SD, Islam M, Hydrie MZ, Chaudhary B, Bellary S, Hashmi S, et al. An FTO variant is associated with Type 2 diabetes in South Asian populations after accounting for body mass index and waist circumference. Diabet Med. 2011;28(6):673–80. doi: 10.1111/j.1464-5491.2011.03257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fuller JH, Stevens LK, Wang SL. Risk factors for cardiovascular mortality and morbidity: The WHO multinational study of vascular disease in diabetes. Diabetologia. 2001;44(S2):S54–64. doi: 10.1007/pl00002940. [DOI] [PubMed] [Google Scholar]
- 30.Jafar TH, Levey AS, White FM, Gul A, Jessani S, Khan AQ, et al. Ethnic differences and determinants of diabetes and central obesity among South Asians of Pakistan. Diabet Med. 2004;21(7):716–23. doi: 10.1111/j.1464-5491.2004.01140.x. [DOI] [PubMed] [Google Scholar]
- 31.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 32.Kreisberg RA, Kasim S. Cholesterol metabolism and aging. Am J Med. 1987;82(1):54–60. doi: 10.1016/0002-9343(87)90272-5. [DOI] [PubMed] [Google Scholar]