Abstract
Background:
Urbanization and diet change have increased the prevalence of Vitamin D deficiency. Unfortunately, none of the suggested treatments is widely accepted.
Objectives:
Therefore, we evaluated the most used and suggested protocol for treating Vitamin D deficiency in Percutaneous coronary intervention (PCI) candidate patients referred to our hospital in a short-term clinical trial.
Patients and Methods:
All patients with coronary artery disease, referred to our hospital and candidates for PCI (drug eluted stents) were included. Deficient patients were randomly assigned to treatment (Vitamin D3 pearls of 50,000 IU; one per week for 10 weeks then one pearl every month for maintenance) and non-treatment groups. Vitamin D was measured after nine months.
Results:
After initial evaluation, 116 cases were found to be deficient, and were divided into two equal groups of 58. No significant difference was found between the normal, treated and non-treated groups regarding age and gender. Thirty-two out of 58 (55.1%) subjects were vitamin D deficient and reached normal levels by taking supplements and seven out of 58 (12%) were deficient and reached normal levels without taking supplements, with the difference being significant (P < 0.001).
Conclusions:
The used protocol is not enough for treating Vitamin D deficiency. Furthermore, the protocol should be revised according to baseline Vitamin D classification.
Keywords: Vitamin D, Dietary Supplements, Deficiency
1. Background
Vitamin D is a group of fat-soluble steroids, mainly responsible for calibrating serum calcium, iron, magnesium, phosphate and zinc. Cholecalciferol (Vitamin D3) and ergocalciferol (Vitamin D2) can be ingested from the diet and from supplements. However, newly published articles have referred to Vitamin D as a hormone (1-3).
There are evidences that the function of Vitamin D is not limited to ion balance. Studies have demonstrated that Vitamin D has an important role in preventing cancers, cardiovascular diseases, depression, immune system deficiencies, pregnancy and neonatal disorders. Therefore, treating individuals with low serum Vitamin D, even without any bone malformation, is essential (4, 5).
On the other hand, nowadays, due to urbanization and diet change, the prevalence of Vitamin D deficiency is rising in many societies, as scientists have estimated that the prevalence of hypovitaminosis has exceeded 90% in some countries. Hovsepian et al. (6) and Heshmat et al. (7) showed that moderate to severe deficiency was near 65% and 50% in urban societies of Iran, respectively. Although there are many strategies for treating these patients, many patients with severe chronic disorders, referred to hospitals, have Vitamin D deficiency (8-10). None of the classifications or the suggested treatments is widely accepted and controversies have arisen in most cases.
2. Objectives
In this study we evaluated the most used and suggested protocols for treating Vitamin D deficiency in PCI-candidate patients referred to our hospital in a short-term clinical trial.
3. Patients and Methods
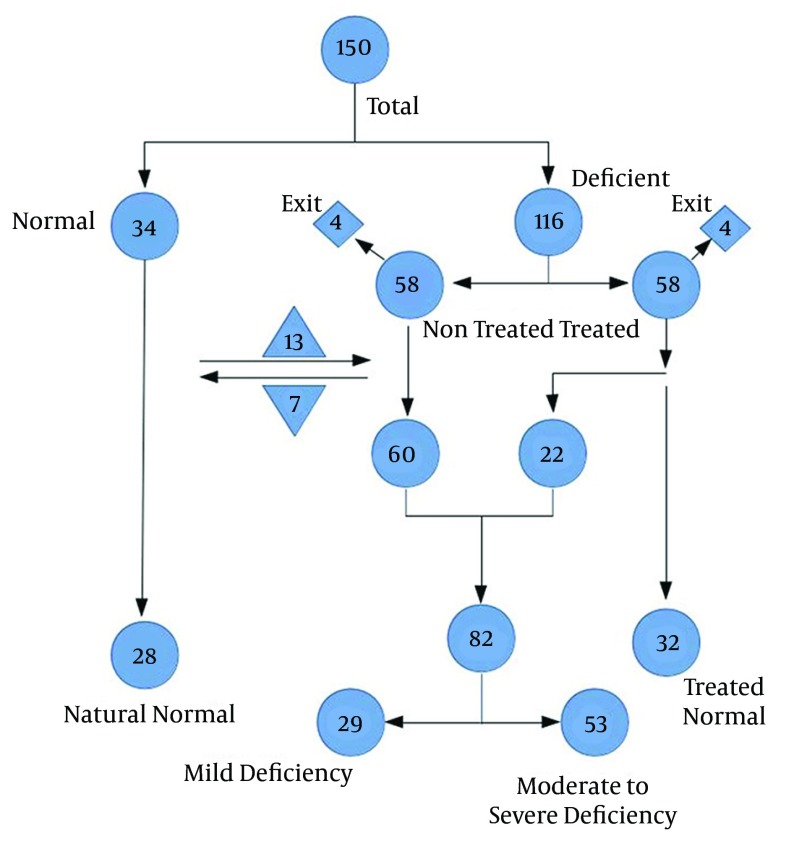
This study was a semi-experimental part of a larger randomized clinical trial on patients with coronary artery disease, candidate for PCI, who had been referred to the Baqiyatallah Hospital. The study duration was nine months, from April 2013 to February 2014. All patients with coronary artery disease, candidate for PCI (drug eluted stents) were included. Patients with acute or chronic renal failure, acute or chronic liver failure, mal-absorption disorders and other heart problems such as rheumatic heart failure and aortic dissection were excluded (Figure 1).
Figure 1. Flowchart Diagram of the Included Patients.
Blood was drawn from all patients and Vitamin D3 was measured by the commercial Enzyme-Linked Immunosorbent Assay (ELISA) for all samples. Patients with Vitamin D levels of 30 IU were considered as normal and excluded from the study. Others were categorized as follows; 29.9 - 20 IU: mild deficiency, 19.9 - 10 IU: moderate deficiency, and < 10 IU: severe deficiency.
Deficient patients were randomly assigned to two groups: patients who received treatment (Vitamin D3 pearls of 50,000 IU; one per week for 10 weeks then one pearl every month for maintenance) and patients who received no treatment. Vitamin D3 was measured again at the end of the nine months and patients were reassigned regarding the above classification. Data was analyzed by the SPSS (v. 20) software using chi-square, t-test, Mann-Whitney-U test.
4. Results
At the initial step of the study, 150 subjects were included with a mean age of 62.46 ± 10.80 years. The male: female ratio was 94:56 (62%:38%). After initial evaluation, 116 cases were found to be deficient, and were divided into two equal groups of 58. No significant difference was found between our normal, treated and non-treated groups regarding age and gender. Thirty-two out of 58 (55.1%) were deficient and reached normal levels by consumption of supplements and seven out of 58 (12%) were deficient and reached normal levels without supplements, with the difference being significant (P < 0.001). Tables 1 and 2 demonstrate the exact classification of both groups; as indicated, changes in the treatment group were significant (P < 0.001). However, in the non-treated group, no significant change was seen (P > 0.05) Tables 1 and 2.
Table 1. Number of Patients in the Treatment Group, Categorized by Initial and Final Vitamin D Levels a.
| Initial Vitamin D | Final Vitamin D Measurement | |||||
|---|---|---|---|---|---|---|
| Normal | Mild | Moderate | Severe | Unknown | Total | |
| Mild | 10 | 4 | 0 | 0 | 1 | 15 |
| Moderate | 16 | 8 | 3 | 0 | 1 | 28 |
| Severe | 6 | 3 | 2 | 2 | 2 | 15 |
| Total | 32 | 15 | 5 | 2 | 4 | 58 |
a As indicated, 32/58 became normal with this protocol. Our study demonstrated that out treatment was more effective on mildly deficient patients (P < 0.001).
Table 2. Number of Patients in the Non-Treatment Group, Categorized by Initial and Final Vitamin D Levels a.
| Initial Vitamin D | Final Vitamin D Measurement | |||||
|---|---|---|---|---|---|---|
| Normal | Mild | Moderate | Severe | Unknown | Total | |
| Mild | 2 | 4 | 2 | 0 | 2 | 10 |
| Moderate | 4 | 2 | 12 | 14 | 1 | 33 |
| Severe | 1 | 0 | 2 | 11 | 1 | 15 |
| Total | 7 | 6 | 16 | 25 | 4 | 58 |
a As indicated, only seven out of 58 became normal without treatment.
5. Discussion
Vitamin D deficiency is a pandemic problem. Some studies have demonstrated prevalence rates as high as 90%, and according to recent studies, there are many conditions, which are more or less relevant to Vitamin D (4, 5). Therefore, paying attention to its causes and treatment is very logical.
According to the literature and clinical evaluation, nearly 50% of the Iranian population is Vitamin D deficient (6, 7); furthermore, our study showed that nearly 75% of PCI-candidate patients have Vitamin D deficiency. These primary results can illustrate the importance of treating Vitamin D deficient individuals, even without any other co-morbidity.
The pharmacological forms of Vitamin D are 50000 IU pearls Vitamin D3 and the 300000 IU injection form. Multivitamins usually contain less than 400 IU in each tablet. The calcium-D contains 200 IU of Vitamin D. Therefore, the tablet of calcium-D is not sufficient for treatment and maintenance treatment in patients who require therapy. Weekly pearl of 50000 IU of Vitamin D3 for a period of eight weeks given to the patient to replenish the deficiency of Vitamin D is the most used protocol worldwide. In the maintenance phase, 50000 IU Vitamin D3 is administered every two to four weeks (1, 2, 11-12).
Our results demonstrated that even using 10 weeks of loading doses instead of standard eight weeks, normalized 32 out of 58 (55.1%) patients with Vitamin D deficiency and seven out of 58 (12%) reached normal levels without supplement. Thus, the difference is less than 45%, which seems to be very low. However, this protocol is more effective in mildly deficient patients (66%) compared to moderate (57%) and severely (40%) deficient individuals.
It seems that the used protocol is not enough for treating Vitamin D deficient patients and the protocol should be replaced by protocols that are more efficient. Furthermore, the protocol should be revised according to baseline Vitamin D classification and we recommend that more severe deficient patients should receive higher doses for a longer period; however, more researches should be carried out in other societies and under other conditions, which have a close relationship with Vitamin D.
Acknowledgments
We would like to thank all participants and their families for assisting us in conducting this study.
Footnotes
Author’s Contributions:Zahra Jozanikohan and Davood Kazemi Saleh cooperated in all parts of the study equally.
Funding/Support:The Vice-Chancellor of Research of Baqyatallah University of Medical Sciences supported this research.
References
- 1.Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080S–6S. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 2.Larijani B, Moradzadeh K, Keshtkar AA, Hossein-Nezhad A, Rajabian R, Nabipour I, et al. Normative Values of Vitamin D Among Iranian Population: A Population Based Study. Int J Osteoporo Metabol Disor. 2008;1(1):8–15. doi: 10.3923/ijom.2008.8.15. [DOI] [Google Scholar]
- 3.Bolland MJ, Grey A, Gamble GD, Reid IR. The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis. Lancet Diabetes Endocrinol. 2014;2(4):307–20. doi: 10.1016/S2213-8587(13)70212-2. [DOI] [PubMed] [Google Scholar]
- 4.Byers T. Anticancer vitamins du Jour--The ABCED's so far. Am J Epidemiol. 2010;172(1):1–3. doi: 10.1093/aje/kwq112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hovsepian S, Amini M, Aminorroaya A, Amini P, Iraj B. Prevalence of vitamin D deficiency among adult population of Isfahan City, Iran. J Health Popul Nutr. 2011;29(2):149–55. doi: 10.3329/jhpn.v29i2.7857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heshmat R, Mohammad K, Majdzadeh SR, Forouzanfar MH, Bahrami A, Omrani Ranjbar GH, et al. Vitamin D deficiency in Iran: A multi-center study among different urban areas. Iranian J Public Health. 2008;37(sup):72–8. [Google Scholar]
- 7.Aguilar del Rey FJ. [Protocol of treatment of vitamin D deficiency]. Med Clin (Barc). 2014;142(3):125–31. doi: 10.1016/j.medcli.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Joshi K, Bhatia V. Vitamin D treatment and toxicity: primum non nocere. Indian Pediatr. 2014;51(1):64. [PubMed] [Google Scholar]
- 9.Kazemisaleh D, Jozani Z, Assar O, Lotfian I. The effect of vitamin D deficiency on coronary artery stenosis severity in angioplasty patients in Baqiatallah hospital in 2013. Arak Med Uni J. 2013;16(79):70–5. [Google Scholar]
- 10.Holick MF. Vitamin D and Health: Evolution, Biologic Functions, and Recommended Dietary Intakes for Vitamin D. ClinRevi Bone Mineral Metabol. 2009;7(1):2–19. doi: 10.1007/s12018-009-9026-x. [DOI] [Google Scholar]
- 11.Adams JS, Hewison M. Update in vitamin D. J Clin Endocrinol Metab. 2010;95(2):471–8. doi: 10.1210/jc.2009-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minaee S, Amin A, Ardeshiri M, Naderi N, Taghavi S. Effects of Vitamin D supplementation on biochemical and functional parameters in patients with congestive heart failure. Cardiovas therap. 2012;30:4–5. [Google Scholar]