Abstract
Objective
This purpose of this review was to examine the relationship between exercise dose and reductions in weight gain during pregnancy in exercise interventions.
Design and Methods
Four electronic research databases (PubMed, Web of Science, CINAHL, and Academic Search Premiere) were used to identify exercise interventions conducted with pregnant women. Eligible articles must have satisfied the following criteria: inclusion of a control condition, exercise as a major intervention component, weight gain measured and reported for each experimental condition, description of exercise dose (frequency, intensity and duration), and utilized an adequate number of control conditions to assess independent effects of exercise on weight gain.
Results
The literature search identified 4837 articles, of these, 174 abstracts were screened and 21 intervention studies (18 exercise-only, 3 exercise/diet) were eligible for review. Only 38% of the interventions achieved statistically significant reductions in weight gain during pregnancy. Successful interventions possessed higher adherence and lower attrition rates and were predominantly conducted among normal weight populations. No clear patterns or consistencies of exercise dose and weight gain were evident.
Conclusions
Adherence and retention rates were strong contributors to the success of exercise interventions on weight gain during pregnancy. However, an exercise dose associated with reductions in weight gain was unquantifiable among these interventions. It is strongly suggested that future researchers investigate methods to increase adherence and compliance, especially among overweight and obese women, and utilize objective measurement tools to accurately evaluate exercise dose performed by the participants and the impact on both body composition and weight gain.
Keywords: physical activity, pregnancy, obesity, programs
Introduction
Evidence suggests that maternal physical activity (PA) has decreased substantially over the past half century,1, 2 in concert with a significant increase in the prevalence of excessive gestational weight gain (GWG) during pregnancy.3, 4 Given that PA is an absolute requirement for metabolic control5 and that the partitioning of nutrient-energy between the mother and fetus is a major determinant of birth outcomes,6 any perturbation of maternal energy metabolism (e.g., increased adiposity, decrements in glycemic control) may induce significant pathologies. Excessive weight gain during pregnancy is associated with several maternal-fetal complications.7–10 Exercise, defined as planned, structured, and repetitive movements with the objective of increasing or maintaining physical fitness,11 has been identified, in addition to diet,12 as a potential contributing solution to excessive GWG due to its profound effects on energy metabolism (e.g., glycemic control13, 14) and may be integral in weight management during pregnancy.15
In non-pregnant populations, there is fairly strong evidence that exercise is associated with weight maintenance among men and women.16 To achieve weight maintenance, defined as a 1% to 3% change in weight, evidence suggests that individuals should engage in at least 150–300 minutes of moderate exercise per week.17 However, during pregnancy the exercise dose for weight maintenance or reduced weight gain is largely unknown. Currently, the American College of Obstetricians and Gynecologists (ACOG) recommends that pregnant women engage in at least 30 minutes of moderate intensity exercise on ‘most’ days of the week. 18 These guidelines were largely based on evidence regarding the effect of exercise on maternal-fetal complications (e.g. adverse birth outcomes, metabolic conditions, preterm delivery) rather than on the potential impact on GWG and its associated outcomes.
The evidence from previous systematic reviews and meta-analyses assessing the effects of exercise interventions on weight gain during pregnancy appears weak as the findings are inconsistent.15, 19, 20 The equivocal nature of the finding may be attributable to only a small number of reviews having assessed the independent effects of exercise on weight gain potentially making it difficult to draw robust conclusions. Additionally, the inconsistency among the findings of these reviews may be in part due to the selection criteria utilized (e.g. restricting samples to overweight and obese women, requiring GWG to be a primary or secondary outcome), or the prescription of an exercise dose that may have been insufficient to reduce weight gain. The latter limitation has largely been ignored in the literature and considering the strong evidence regarding the relationship between exercise dose and weight stability among non-pregnant populations, it is essential to investigate whether this relationship exists among pregnant women. Therefore, the purpose of this study was to systematically review the current literature and examine the exercise dose prescribed in interventions during pregnancy and its influence on GWG. We hypothesized that exercise interventions that were successful at reducing weight gain during pregnancy assigned higher doses of exercise compared to unsuccessful exercise interventions, thereby potentially demonstrating a dose –response effect.
Methods
A systematic review of experimental exercise trials was conducted following the PRISMA (preferred reporting items for systematic review and meta-analysis) statement21 by the primary author (SM) in four electronic research databases, Pubmed, Web of Science, CINAHL and Academic Search Premiere, from inception to February 17th, 2013. We used the following keywords with various combinations to ascertain peer-reviewed articles: (‘pregnancy’ OR ‘prenatal’ OR ‘antenatal’) AND (‘intervention’ OR ‘trial’) AND (‘physical activity’ OR ‘aerobic’ OR ‘exercise’) AND (‘weight’ OR ‘weight gain’ OR ‘gestational weight gain’) AND (‘overweight’ OR ‘obese’ OR ‘obesity’) AND (‘diet’ OR ‘nutrition’). In addition, references of obtained articles were scanned to ensure a complete collection of literature. Search strategies for all research databases used can be found in Table 4. There were no restrictions placed on year of publication, country, pre-pregnancy body mass index (BMI) or gestational age at study entry, however the included articles must satisfy the following criteria:
Inclusion of any control condition (e.g., concurrent, historical, wait-list),
GWG measured and reported for each condition,
Any intervention with exercise as the primary focus (e.g., exercise training, PA counselling)
Complete description of the exercise dose (frequency, duration, and intensity), and
In the case of multiple intervention arms (i.e. exercise and diet), a sufficient number of experimental/control conditions (e.g. exercise-only, exercise plus diet, and/or control conditions) must have been utilized in order to examine the independent effect of exercise on GWG.
In addition, we did not require GWG be a primary or secondary outcome, as such studies providing GWG as a sample characteristic were included. This is a significant limitation of previous reviews that only included interventions with GWG as a primary or secondary outcome as the discovery of potentially effective interventions may have been precluded.22, 23 Moreover, studies following women into the postpartum period were also included.
We extracted the following data for each eligible study: study, participant, behavioral, and intervention characteristics; exercise dose; and weight gain measurements. Study characteristics consisted of information on location, design, sample size, and year of publication. Participant characteristics included maternal age, gestational age at onset of intervention, racial/ethnic composition, and anthropometrics (i.e. BMI, percent body fat, weight). Intervention characteristics consisted of duration, control condition assignment, adherence, attrition, intervention location (e.g. laboratory, gym, home), and exercise-related injuries and/or maternal-fetal complications. Information regarding sedentary and PA behaviors along with their respective measurement methods was extracted. Details regarding the components of exercise dose (i.e. frequency, intensity and duration) were collected. Gestational weight gain for each intervention condition was extracted in addition to measurement methods (e.g. total weight gain, percent body fat).
Prior to analyzing the extracted data, interventions were classified into two groups, ‘successful’ and ‘unsuccessful’, based on their effect on weight gain. A ‘successful’ intervention was defined as a statistically significant difference in weight gain between the exercise and control conditions. Characteristics of ‘successful’ interventions were then identified. Additionally, the difference in weight gain between the exercise and control conditions was calculated to examine the extent to which the exercise regimens may have prevented weight gain for both the ‘successful’ and ‘unsuccessful’ interventions: (|weight gainedexercise – weight gainedcontrol|).
Results
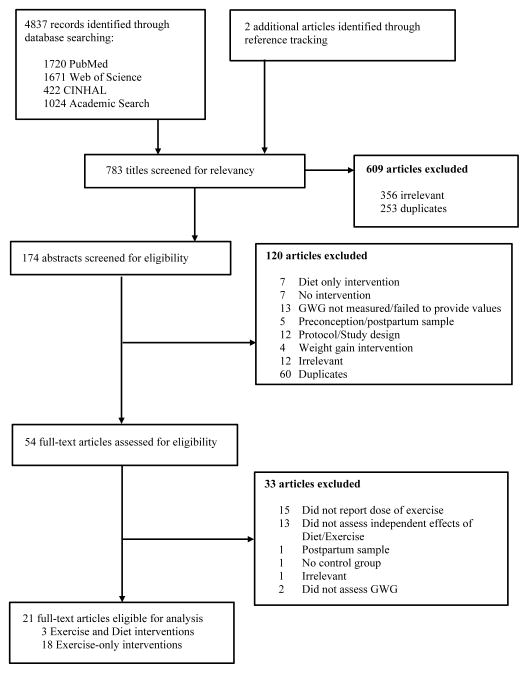
The identification of eligible intervention studies is summarized in Figure 1. First, we identified 4837 potential articles from four databases (Pubmed [n=1720], Web of Science [n=1671], CINHAL [n=422] and Academic Search Premiere [n=1024]). Two additional articles were identified through reference tracking. Of these, 783 article titles were screened and 609 articles were excluded due to relevancy (n=356) and duplications (n=253), resulting in 174 abstracts selected for the initial review. Second, 174 abstracts were screened and 120 failed to meet the inclusion criteria and were excluded (see Figure 1 for reasons for exclusion). The remaining 54 full-text articles were assessed for eligibility, of which 33 were excluded. Eighty-five percent of the 33 articles were deemed ineligible because these studies either did not provide a sufficient number of control conditions to adequately assess the independent effect of exercise on GWG (n=13) or failed to provide a complete description of the dose of exercise (n=15) implemented in the intervention. As a result, 21 studies were eligible for the final review: 18 were exercise only24–41 and 3 were exercise and diet.42–44
Figure 1.
Flow chart of study identification and ascertainment process
Six studies were conducted in the United States, 24, 28, 31, 36–38 two in Canada, 42, 44 three in Brazil,26, 39, 43 two in Norway,32, 34 three in Spain,27, 40, 41 one in the Netherlands,29 two in Iran,25, 35 one in Australia,30 and one in New Zealand.33 Eighty-six percent (n=18) employed a randomized controlled study design24, 25, 27–31, 33, 34, 40, 41, 43 and three studies used a quasi-experimental study design.32, 36, 44 Sample sizes varied considerably across the studies (N=12 to 266).
The mean age of the pregnant women ranged from 23.2 to 33.4 years. These studies varied considerably in weeks of gestation at intervention onset, ranging from eight weeks37, 38 to 24–28 weeks of gestation.44 Four studies implemented their intervention in the first trimester (8–12 weeks of gestation),27, 37, 38, 40 while the remaining 17 studies started their exercise programs in the second trimester (13–28 weeks of gestation).24–26, 28–36, 39, 41–44 The racial/ethnic composition of the study samples was only reported in four studies (19%)24, 28, 29, 33 of which three studies reported a predominantly White sample.24, 29, 33 Moreover, ten of the 21 studies either restricted their sample to normal weight women or a majority of their sample was of normal weight.25, 27, 31, 34, 37–42 Nine studies were conducted in overweight or obese populations,24, 26, 28–30, 33, 35, 43, 44 of which five studies26, 29, 30, 43, 44 restricted their enrollment to overweight/obese women and while four studies24, 28, 33, 35 did not apply any BMI restrictions. The BMI or percent body fat of the participants were unknown in two studies as the authors only reported pre-pregnancy weight in kilograms.32, 36
Eight studies enrolled a sedentary sample population.24, 27, 28, 30, 31, 34, 39, 41 Definitions of ‘sedentary’ varied across the studies. Definitions of ‘sedentary’ included: not exercising > 20 minutes more than once a week,27, 41 no aerobic exercise more than once per week in the past 6 months,28 no participation in a structured program > 60 minutes one time per week or brisk walking > 120 minutes per week,34 not exercising on a regular basis at least one year prior to conception,31 daily PA energy expenditure < 840 kcal per week,24 or no definition provided.30, 39 Eight studies reported information on PA behaviors,24, 26, 29, 30, 32, 34, 41, 44 only three studies tested between-group differences in PA across pregnancy, of which one found a significant result24 and two found no differences in PA.29, 30 Five studies assessed PA to provide additional participant information (e.g. baseline characteristics, confounding variable). 26, 32, 34, 41, 44
A majority of the studies (n=17) instructed participants in control condition to adhere to their current prenatal care routine.25, 27–31, 33–36, 38–44 Conversely, in two studies, the control condition consisted of a stretching routine24, 26 and in two other studies the control condition participated in a lower level of exercise intensity.32, 37 Duration of interventions differed considerably across the studies ranging from eight weeks25 to 30 weeks.27 Of the 21 intervention studies, 16 provided supervised exercise sessions throughout the intervention25–31, 34–38, 40, 41, 43 and three interventions implemented unsupervised exercise sessions.32, 33, 44 One study required participants to attend at least one supervised exercise session per week.42 The remaining study decreased the number of supervised exercise sessions over the duration of the intervention.24 Three interventions consisted of solely home-based exercise programs,30, 32, 33 three others were partly home and facility-based (e.g. hospital, gym, exercise laboratory),42–44 the remaining interventions were conducted at a designated facility (e.g. hospital, gym, exercise laboratory).24–29, 31, 34–41 Adherence to the exercise programs ranged from 16%29 to 97%.27 Four studies did not report any detail regarding adherence to the exercise program.31, 32, 36, 44 Similarly, attrition varied considerably among the studies (0%32, 44 to 40%31). Three studies did not report on study attrition.24, 30, 36 Moreover, the incidence of maternal-fetal complications appeared low, as only a few occurred in most studies. These complications were reported for the following reasons: discontinuation of the study (e.g., persistent bleeding, urinary tract infection) or occurred after the intervention (e.g., preterm delivery),25, 26, 33, 34, 37, 38, 41 as an outcome and/or sample characteristic (e.g., gestational diabetes, gestational hypertension, preterm delivery),29, 39, 43 a combination of these, 27, 28, 32, 40 or did not report this information.24, 30, 31, 35, 36, 42, 44 Additionally, four studies reported that “no exercise-related injuries arose during the intervention period,”29, 34, 41, 43 while the remaining studies did not provide this information.24–28, 30–38, 40, 42, 44
Eleven of the 21 studies designed their programs aligning with the ACOG PA guidelines.18, 24–29, 34, 35, 39, 40, 43 One studies followed the American College of Sports Medicine (ACSM) PA guidelines for pregnant women. 36, 45 Two studies used the Canadian guidelines for PA.42, 44, 46 One of these two studies also utilized the ACSM guidelines in addition to the Canadian guidelines for PA during pregnancy.42 One study modified their program to require more vigorous levels of intensity than ACOG guidelines.31 Six studies did not mention which guidelines, if any, were used when developing their interventions.30, 32, 33, 37, 38, 41
Exercise doses varied substantially across the studies. Frequency of the exercise programs ranged from one to six days per week, with three days as the most prescribed frequency (n=14).25–27, 30, 31, 34–36, 38–42, 44 Likewise, duration varied from 15 minutes to 90 minutes per session. Intensity of the exercise program had the greatest variability of all the components. Exercise intensity was measured via four different methods: percent of age-predicted maximum heart rate (%APMHR/%HRmax [n=8]24–27, 30, 39– 41), percent heart rate reserve (%HRR [n=2]42, 44), percent of peak or maximal oxygen consumption (%VO2 peak/max [n=4]33, 36–38), rating of perceived exertion (RPE/Borg Scale [n=6]24, 27–30, 34). Four studies did not describe their method used to determine the prescribed exercise intensity.31, 32, 35, 43 For studies using the APMHR method, intensities ranged from low (50%)26, 30 to moderate (<80%).41 Studies using %HRR, intensity varied from low (30%)42, 44 to vigorous (70%).42 Studies using %VO2 peak/max ranged from moderate (55%)37, 38 to vigorous (70%).36 Lastly, those studies utilizing the RPE/Borg scale, one study27 used 10 on the scale which equated to light intensity while three studies used 12 to 14 on the scale which corresponded to moderate intensity.24, 28, 34 Four studies reported target heart rates for the exercise program; however the method used to determine these values was not described.31, 32, 35, 43
In order to determine whether participants were adhering to the prescribed exercise intensity, studies used several objective and subjective tools that measured physiological responses to exercise (e.g., heart rate, CO2 production, fatigue). The tools used to determine the adherence to exercise intensities varied among the studies. Twelve of the 21 studies utilized only heart rate monitors during exercise sessions.25, 26, 31–33, 39, 41, 42, 44 Two studies manually assessed heart rates during each exercise session.35, 36 Four studies used the RPE/Borg scale28–30, 34 and three used both heart rate monitors and the RPE/Borg scale.24, 27, 40 Two studies utilized indirect calorimetry; however this was only done once every two weeks.37, 38 The remaining study did not specify any method used to monitor exercise intensity during the exercise sessions.43 In addition, 17 of the 21 studies did not report mean intensity level25–29, 31–35, 37–41, 43, 44 one study reported an average %HRR,42 and one study reported an average value on the Borg Scale.30 Two studies provided average heart rates but the relative exercise intensity (i.e. %HRR, %VO2 peak/max) was unclear.24, 36
GWG was the primary outcome in seven studies,25, 27, 34, 39, 41, 42, 44 the secondary outcome in four studies,28, 32, 37, 38 one of several outcomes in five studies24, 29, 31, 40, 43 and simply a measurement for maternal characteristics in five studies.26, 30, 33, 35, 36 The measurement of GWG varied across the studies. All 21 studies reported total weight gain; 13 of them used this measure as their sole outcome.25, 26, 28–33, 35, 36, 38, 39, 41 Weekly rate of GWG was reported in three studies.42–44 Six studies measured GWG using the 2009 Institute of Medicine (IOM) guidelines.24, 27, 34, 40, 42, 44 Eight studies included at least two of the aforementioned measures of GWG.24, 27, 34, 37, 40, 42–44
The characteristics of ‘successful’ and ‘unsuccessful’ interventions are depicted in Table 1 and Table 2, respectively. Out of the 21 studies, eight interventions were ‘successful’25, 27, 32, 34, 37, 40, 42, 43 and thirteen were ‘unsuccessful’ 24, 26, 28–31, 33, 35, 36, 38, 39, 41, 44 at reducing weight gained during pregnancy. Although the study characteristics were generally similar across the categories (e.g. sample size, study design, exercise dose etc.), there were several notable differences. Among the ‘successful’ interventions, 75% (n=6) of the studies were conducted in women with normal pre-pregnancy BMI.25, 27, 34, 37, 40, 42 Conversely, 62% (n=8) of the ‘unsuccessful’ interventions were implemented in overweight and obese populations.24, 26, 28–30, 33, 35, 44 The prescribed exercise doses did not greatly differ between the ‘successful’ and ‘unsuccessful’ interventions; however adherence and attrition rates were dissimilar. In the ‘successful’ interventions, 63% (n=5) had an adherence rate of ≥70%,25, 27, 34, 37, 40 whereas this level of adherence occurred in 46% of the ‘unsuccessful’ studies.28, 30, 33, 35, 38, 41 Moreover, the proportion of ‘successful’ studies achieving ≤20% attrition was 63%25, 27, 32, 37, 43 versus 23%38, 41, 44 in the ‘unsuccessful’ studies. Furthermore, 63%27, 32, 37, 40, 42 of the ‘successful’ studies implemented interventions ≥20 weeks in duration, versus only 31%24, 28, 38, 41 in the ‘unsuccessful’ interventions. ‘Successful’ interventions, 75%27, 34, 37, 40, 42, 43 used at least two methods of measuring GWG versus only 15%24, 44 of the ‘unsuccessful’ interventions. Among the ‘successful’ interventions, the difference in weight gain between the exercise and control conditions ranged from 1.3 kg to 6.0 kg whereas the difference in weight gain for the ‘unsuccessful’ interventions ranged from 0.2 kg to 1.9 kg.
Table 1.
Study characteristics of ‘successful’ exercise interventions†
| Author (year) | Study Design and Location | Sample Characteristics | Intervention Details | Exercise Dose | GWG Measure‡ | Stat Analysis | Results | |
|---|---|---|---|---|---|---|---|---|
| Bakarat40 (2013) | RCT | Age: 31.57y (EX) | Supervised | Frequency: 3x/week | Total GWG (4) | Unpaired t-test | Total GWG: | |
| N=251 | 31.51y (CON) | Duration: 27–30 weeks | Duration: 55–60 minutes | %IOM | χ2 test | |||
| PA only | Intensity: 55–60% HRmax | Guidelines | EX: 11.72 kg a | p=0.06 | ||||
| Spain | Gestation: 9–13 weeks | Progressive: N/R | CON: 13.66 kg a | |||||
| Adherence: >95% | ||||||||
| BMI: | IOM Guidelines - Excessive | |||||||
| 68.9% (NW) | Attrition: | |||||||
| 23.6% (OW) | EX: 22% CON: 18% | EX: 21.2% a | p=0.026 | |||||
| 6.6% (OB) | CON: 35.6% b | |||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Clapp37 (2002) | Prospective | Age: 31y (Lo-Hi) | Supervised | Lo-Hi: | Total GWG (4) | ANOVA | Total GWG: | |
| RCT | 30y (Mod-Mod) | Duration: 29 weeks | Frequency: 5x/week | % change in BF | ||||
| N=80 | 32y (Hi-Lo) | PA Only | Duration: 20 to 60 minutes (progressed up to week 24) | Lo-Hi: 12 kg a | p<0.02 | |||
| US | Gestation: 8 weeks | Adherence: >90% | Intensity: 55–60% VO2 max | Mod-Mod:14.6kg b | ||||
| %Body Fat: | Attrition: | Hi-Lo: 15.5 kg b | ||||||
| 19% (Lo-Hi) | Mod-Mod: | |||||||
| 18% (Mod-Mod) | 6% (combined) | Frequency: 5x/week | ||||||
| 19% (Hi-Lo) | Duration: 40 minutes | Body Fat% | ||||||
| Intensity: 55–60% VO2 max | ||||||||
| Sedentary sample? N/R | Lo-Hi: 2.8% a | p<0.02 | ||||||
| Hi-Lo: | Mod-Mod: 4.2% b | |||||||
| Frequency: 5x/week | ||||||||
| Duration: 60 to 20 minutes (decreased until week 24) | Hi-Lo: 5.5% b | |||||||
| Intensity: 55–60% VO2 max | ||||||||
| Progressive: Yes | ||||||||
|
| ||||||||
| Haakstad34 (2011) | RCT | Age: 31.2y (EX) | Supervised | Frequency: 2–3/week | Total GWG (1) | ITT analysis | Total GWG: | |
| N=205 | 30.3y (CON) | Duration: 12 weeks | Duration: 60 minutes | %IOM | Independent t- test | ITT Analysis: | ||
| PA only | Intensity: Moderate Borg Scale 12–14 | Guidelines Excessive | χ2 test | EX: 13.0 kg a | p=0.31 | |||
| Norway | Gestation: | |||||||
| 17.3 weeks (EX) | Progressive: N/R | CON: 13.8 kg a | ||||||
| 18.0 weeks (CON) | Adherence: 71% | Per Protocol: | ||||||
| BMI: | Attrition: | EX: 12.5 kg a | p=0.23 | |||||
| 23.8 kg/m2 (EX) | CON: 13.8 kg a | |||||||
| 23.9 kg/m2 (CON) | EX: 19.2% CON: 20.8% | |||||||
| Sedentary sample? Yes | Attendance-24 sessions: | |||||||
| EX: 11.0 kg a | p=0.01 | |||||||
| CON: 13.8 kg b | ||||||||
| IOM Guidelines - Excessive: | ||||||||
| ITT Analysis: | ||||||||
| EX: 33% a | p=0.59 | |||||||
| CON: 38% a | ||||||||
| Per Protocol: | ||||||||
| EX: 19% a | p=0.12 | |||||||
| CON: 38% a | ||||||||
| Attendance-24 sessions: | ||||||||
| EX: 0% a | p=0.006 | |||||||
| CON: 38%b | ||||||||
|
| ||||||||
| Kardel32 (1998) | Quasi | Age: 26.7y (Moderate EX) | Not Supervised | Moderate EX: | Total GWG (1) by sex of child | One-way ANOVA | Total GWG: | |
| N=42 | 28.8y (High EX) | Duration: 20 weeks | Interval Training: | |||||
| PA Only | Frequency: 2x/week | GIRL | ||||||
| Norway | Gestation: 17 weeks | Duration: 25 minutes | Moderate EX: 10.3 kg a | p=0.021 | ||||
| Intensity: 170–180 bpm | High EX: 14.4 kg b | |||||||
| Weight: | Adherence: N/R | HR monitors | ||||||
| 63.0 kg (Moderate EX) | Endurance Training: | BOY: | ||||||
| 59.4 kg (High EX) | Attrition: | Frequency: 2x/week | Moderate EX: 12.6 kg a | |||||
| Duration: 1.5 hours | High EX: 12.6 kg a | p>0.05 | ||||||
| Sedentary sample? N/R | 0% (combined) | Intensity: 120–140 bpm | ||||||
| Strength Training: | ||||||||
| Frequency: 2x/week | ||||||||
| Duration: 1 hr 12 min | ||||||||
| Intensity: N/A | ||||||||
|
High EX: |
||||||||
| Interval Training: | ||||||||
| Frequency: 2x/week | ||||||||
| Duration: 35 minutes | ||||||||
| Intensity: 170–180 bpm | ||||||||
| HR monitors | ||||||||
| Endurance Training: | ||||||||
| Frequency: 2x/week | ||||||||
| Duration: 2.5 hours | ||||||||
| Intensity: 120–140 bpm | ||||||||
| Strength Training: | ||||||||
| Frequency: 2x/week | ||||||||
| Duration: 1 hr 12 min | ||||||||
| Intensity: N/A | ||||||||
| Progressive: N/R | ||||||||
|
| ||||||||
| Nascimiento43 (2009) | RCT | Age: 29.7y (EX) | Supervised | Frequency: 1x/week | Total GWG (1)** | Student’s t-test | Total GWG: | |
| N=82 | 30.9y (CON) | Duration: 16 weeks | Duration: 40 minutes | Weekly GWG | Mann-Whitney | |||
| PA and Diet – Both the EX and CON conditions received diet counselling | Intensity: HR < 140 bpm | U statistic | Overweight | |||||
| Brazil | Gestation: | EX: 10.0 kg a | p=0.001 | |||||
| 17.6 weeks (EX) | Home Counselling: | CON: 16.4 kg b | ||||||
| 17.8 weeks (CON) | In addition to the prescribed exercise sessions, women received home exercise counselling 5x per week. Consisted of protocol exercises or walking | |||||||
| BMI: | Adherence: 62.5% | Obese | ||||||
| 34.8 kg/m2 (EX) | EX: 10.4 kg a | p=0.757 | ||||||
| 36.4 kg/m2 (CON) | Attrition: | CON: 10.9 kg a | ||||||
| Sedentary sample? N/R | EX: 2.5% CON: 2.4% | |||||||
| Progressive: N/R | Weekly GWG: | |||||||
|
Overweight |
||||||||
| EX: 0.28 kg a | p=0.038 | |||||||
| CON: 0.57 kg b | ||||||||
|
Obese |
||||||||
| EX: 0.39 kg a | p=0.577 | |||||||
| CON: 0.36 kg a | ||||||||
|
| ||||||||
| Ruchat42 (2012) | RCT Block | Age: 31y (LI) | Supervised: 1 session required | Frequency: 3–4x/week | Total GWG (4) | ANCOVA | Total GWG: | |
| N=73 | 30.4y (MI) | Duration: 15 minutes | Weekly GWG | Covariates: pre- pregnancy body weight χ2 test | ||||
| Duration: 21.5 week | Increased weekly by 2 minutes until 30 minutes reached | %IOM Guidelines | LI: 15.3 kg a | p=0.72 (LI vs MI) | ||||
| Canada | Gestation: | PA and Diet: LI and MI received diet program | MI: 14.9 kg a | p=0.01 (LI vs CON) | ||||
| 17.5 weeks (Light) | CON: 18.3 kg b | p=0.003 (MI vs CON) | ||||||
| 17.0 weeks (Moderate) | Intensity: LI: 30% HRR | |||||||
| MI: 70% HRR | ||||||||
| BMI: | Adherence: | Progressive: Yes | Weekly GWG: | |||||
| 22.1 kg/m2 (LI) | ||||||||
| 21.7 kg/m2 (MI) | LI: 55% MI: 67% | LI: 0.49 kg a | p>0.05 | |||||
| Attrition: | MI: 0.47 kg a | |||||||
| Sedentary sample? N/R | CON: N/A* | |||||||
| EX: 21.2% CON: 30.3% | ||||||||
| IOM Guidelines – Excessive Prevented | ||||||||
| LI: 70% a | p=0.32 | |||||||
| MI: 77% a | ||||||||
| N/A in CON* | ||||||||
|
| ||||||||
| Ruiz27 (2013) | RCT | Age: 31.9y (EX) | Supervised | Frequency: 3x/week | Total GWG (1) | ITT analysis | Total GWG | |
| N=962 | 31.6y (CON) | Duration: 30 weeks | Duration: 50–55 minutes | %IOM | One-way | |||
| PA only | Intensity: <60% HRmax | Guidelines | ANCOVA | Total Group | ||||
| Spain | Gestation: 9 weeks | Borg Scale 10 | Covariates: age, gestational age, pre-gravid weight, education Logistic regression | EX: 11.9 kg a | p<0.001 | |||
| BMI: | Adherence: 97% | Progressive: N/R | CON: 13.2 kg b | |||||
| 23.7 kg/m2 (EX) |
NW |
|||||||
| 23.5 kg/m2 (CON) | Attrition: | EX: 12.3 kg a | p<0.001 | |||||
| Sedentary sample? Yes | EX: 14.1% CON: 14.5% | CON: 13.8 kg b | ||||||
| OW/OB | ||||||||
| EX: 11.1 kg a | p=0.51 | |||||||
| CON: 11.6 kg a | ||||||||
| IOM Guidelines - Excessive | ||||||||
|
Total Group |
||||||||
| EX: 23.8% a | (OR:0.625; p=0.002) | |||||||
| CON: 32.0% b | ||||||||
| NW | ||||||||
| EX: 12.6% a | (OR: 0.508; p=0.001) | |||||||
| CON: 22.1% b | ||||||||
|
OW/OB |
||||||||
| EX: 49.3% a | (OR: 0.649; p=0.14) | |||||||
| CON: 58.9% a | ||||||||
|
| ||||||||
| Sedaghati25 (2007) | RCT | Age: 23.28y (EX) | Supervised | Frequency: 3x/week | Total GWG (4) | T-test | Total GWG: | |
| N=100 | 23.26y (CON) | Duration: 8 weeks | Duration: 45 minutes | |||||
| PA only | Intensity: 55–65% | EX: 13.55 kg a | p<0.000 | |||||
| Iran | Gestation: 20–22 weeks | APMHR | CON: 15.10 kg b | |||||
| Adherence: >88% | Progressive: N/R | |||||||
| BMI: | ||||||||
| 24.10 kg/m2 (EX) | Attrition: | |||||||
| 24.30 kg/m2 (CON) | ||||||||
| EX: 20% CON: 0% | ||||||||
| Sedentary sample? N/R | ||||||||
Note:
A successful intervention was defined as a statistically significant difference in gestational weight gain and/or percent body fat between the exercise and control conditions.
Conditions with different letters indicates significant between-group differences. PA= physical activity; EX = exercise condition; CON = control condition; NW=normal weight; OWOB=overweight and obese; GWG=gestational weight gain; N/R=not reported. IOM Guidelines: 2009 Institute of Medicine (IOM) Gestational Weight Gain Guidelines. APMHR= Age-predicted maximum heart rate; HR=heart rate; RCT=randomized controlled trial; quasi= quasi-experimental study design, %BF = percent body fat.
Ruchat (2012) utilized a sample of postpartum (2 months) women (n=45) as a control group, data were available on total GWG but not for weekly rate GWG or IOM excessive weight gain.
denotes the calculation used for total weight gain of the following four definitions: (1) Weight prior to delivery (or last prenatal or lab visit) minus pre-pregnancy weight; (2) weight at the end of the intervention minus weight at the start of the intervention; (3) weight prior to delivery (or last prenatal or lab visit) minus weight at study entry; (4) calculation for total weight gain was not specified. For studies not reporting exact p-values, p<0.05 was used for significant and p>0.05 for non-significant findings, unless specified otherwise.
Table 2.
Study characteristics of ‘unsuccessful’ exercise interventions†
| Author (year) | Study Design and Location |
Sample Characteristics | Intervention Details | Exercise Dose | GWG – Measure‡ | Stat Analysis | Results | |
|---|---|---|---|---|---|---|---|---|
| Barakat41 (2009) | RCT | Age: 30.4y (EX) | Supervised | Frequency 3x/week | Total GWG (1) | ITT analysis | Total GWG: | |
| N=142 | 29.5y (CON) | Duration: 26 weeks | Duration: 35–40 minutes | Unpaired t-tests | ||||
| PA Only | Intensity: ≤80% APMHR | Total Group | ||||||
| Spain | Gestation: 12–13 weeks | Progression: N/R | EX: 11.5 kg | p>0.1 | ||||
| CON: 12.4 kg | ||||||||
| BMI: | Adherence: >90% | |||||||
| EX: | NW | |||||||
| 0% (UW) | Attrition: | EX: 12.2 kg | p>0.1 | |||||
| 68.1% (NW) | EX: 12.5% CON: 10% | CON: 12.6 kg | ||||||
| 19.4% (OW) | ||||||||
| 12.5% (OB) | OW | |||||||
| CON: | EX: 10.9 kg | p>0.1 | ||||||
| 3.1% (UW) | CON: 12.3 kg | |||||||
| 70.3% (NW) | ||||||||
| 21.9% (OW) | OB | |||||||
| 4.7% (OB) | EX: 8.4 kg | p>0.1 | ||||||
| CON: 9.7 kg | ||||||||
| Sedentary sample? Yes | ||||||||
|
| ||||||||
| Cavalcante39 (2009) | Open RCT | Age: 25.8y (EX) | Supervised | Frequency 3x/week | Total GWG (1) | ITT analysis | Total GWG: | |
| N=71 | 24.4 (CON) | Duration: 16–18 weeks | Duration: 50 minutes | % change in BF | Student t-test | |||
| PA Only | Intensity: 70% APMHR | MANOVA | EX: 14.1 kg | p=0.38 | ||||
| Brazil | Gestation: 18–20 weeks | Progression: N/R | CON: 15.1 kg | |||||
| BMI: | Adherence: 51% | Body Fat%: | ||||||
| 24.1 kg/m2 (EX) | ||||||||
| 23.4 kg/m2 (CON) | Attrition: | EX: 6.0% | p=0.07 | |||||
| EX: 38.2% CON: 27.0% | CON: 3.9% | |||||||
| %Body Fat: | ||||||||
| 29.7% (EX) | ||||||||
| 28.2% (CON) | ||||||||
| Sedentary sample? Yes | ||||||||
|
| ||||||||
| Clapp38 (2000) | Prospective | Age: 31y (Total Group) | Supervised | Frequency: 3–5x/week | Total GWG (4) | Unpaired t-tests | Total GWG: | |
| RCT | Duration: 27–30 weeks | Duration: 20 minutes | ||||||
| N=50 | Gestation: 8 weeks | PA Only | Intensity: 55–60% VO2 max | EX: 15.7 kg | p>0.05 | |||
| Progression: Indirect | CON: 16.3 kg | |||||||
| US | Weight: | calorimetry every two weeks | ||||||
| 62.1 kg (EX) | Adherence: >95% | |||||||
| 61.7 kg (CON) | ||||||||
| Attrition: 8% (combined) | ||||||||
| %Body Fat: | ||||||||
| 21.9% (EX) | ||||||||
| 21.3% (CON) | ||||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Collings36 (1983) | Quasi | Age: 26.9y (EX) | Supervised | Frequency: 3x/week | Total GWG (4) | Not described for the sample characteristics | Total GWG: | |
| N=20 | 28.0y (CON) | Duration: 13.4 weeks | Duration: 50minutes | |||||
| PA Only | Intensity: 65–70% Vo2max | EX: 15.8 kg | p>0.05 | |||||
| US | Gestation: 22.5 weeks | Progression: workload adjusted to maintain intensity | CON: 14.0 kg | |||||
| Adherence: N/R | ||||||||
| Weight: | ||||||||
| 60.3 kg (EX) | Attrition: N/R | |||||||
| 64.4 kg (CON) | ||||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Davenport44 (2008) | Quasi | Age: 33.3y(EX) | Not Supervised | Frequency: 3–4x/week | Total GWG (4) | Mann-Whitney | Total GWG: | |
| N=40 | 33.4y (CON) | Duration: N/R | Duration: 25–40 minutes - not to exceed 40 minutes | GWG per week | U statistic | |||
| PA and Diet | %IOM Guidelines: Excessive by BMI | χ2 test | EX: 12.0 kg | p>0.05 | ||||
| Canada | Gestation: 24–48 weeks | Intensity: 30% HRR | CON: 12.7 kg | |||||
| Progression: N/R | ||||||||
| BMI: | Adherence: N/R | GWG per Week: | ||||||
| 32.9 kg/m2 (EX) | ||||||||
| 32.8 kg/m2 (CON) | Attrition: 0% (combined) | EX: 0.35 kg | p>0.05 | |||||
| CON: 0.35 kg | ||||||||
| Sedentary sample? N/R | IOM Guidelines - Excessive | |||||||
| Cases: GDM | ||||||||
| NW | ||||||||
| EX: 100% | p>0.05 | |||||||
| CON: 100% | ||||||||
|
OW |
||||||||
| EX: 60% | p>0.05 | |||||||
| CON: 50% | ||||||||
|
OB |
||||||||
| EX: 38% | p>0.05 | |||||||
| CON: 43% | ||||||||
|
| ||||||||
| Garshabi35 (2005) | Prospective | Age: 26.3y (EX) | Supervised | Frequency: 3x/week | Total GWG (4) | Student t-test | Total GWG: | |
| RCT | 26.5y (CON) | Duration: 12 weeks | Duration: 60 minutes | |||||
| N=266 | PA Only | Intensity: ≤140 bpm | EX: 14.1 kg | p=0.63 | ||||
| Gestation: 17–22 weeks | Progression: N/R | CON: 13.8 kg | ||||||
| Iran | Adherence: >92% | |||||||
| BMI: | ||||||||
| 25.98 kg/m2 (EX) | Attrition: | |||||||
| 25.58 kg/m2 (CON) | EX: 33.5% CON: 0% | |||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Hopkins33 (2010) | RCT | Age: 31y (EX) | Not Supervised | Frequency: at most 5x/week | Total GWG (3) | ITT analysis | Total GWG: | |
| N=98 | 29y (CON) | Duration: 15 weeks | Duration: 40 minutes | Repeated measures | ||||
| PA Only | Intensity: 65% VO2 max | EX: 8.0 kg | p=0.76 | |||||
| New Zealand | Gestation: 19 weeks | Progression: Yes | ANOVA | CON: 8.2 kg | ||||
| Adherence: 75% | ||||||||
| BMI: | ||||||||
| 26.7 kg/m2 (EX) | Attrition: | |||||||
| 25.5 kg/m2 (CON) | ||||||||
| EX: 4% CON: 24% | ||||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Marquez- Sterling31 (2000) | RCT | Age: 31.3y (EX) | Supervised | Frequency 3x/week | Total GWG (1) | Independent Student’s t-test | Total GWG: | |
| N=20 | 27.8y (CON) | Duration: 15 weeks | Duration: 60 minutes | |||||
| PA Only | Intensity: HR at 120–130 bpm (first two weeks), then increased to 140–150 bpm and then increased to 150–156 bpm | EX: 16.2 kg | p=0.649 | |||||
| US | Gestation: | CON: 15.7 kg | ||||||
| 18.2 weeks (EX) | Adherence: N/R | |||||||
| 20.0 weeks (CON) | ||||||||
| Attrition: | ||||||||
| BMI: | EX: 10% CON: 40% | Progression: Yes | ||||||
| 22.8 kg/m2 (EX) | ||||||||
| 24.5 kg/m2 (CON) | ||||||||
| Sedentary sample? Yes | ||||||||
|
| ||||||||
| Ong30 (2009) | RCT | Age: 30y (Total Group) | Supervised | Frequency 3x/week | Total GWG (4) | Repeated measures | Total GWG: | |
| N=12 | Duration: 10 weeks | Duration: 15–30 minutes | ||||||
| Gestation: 18 weeks | PA Only | then progressed to 40–45 min | ANOVA | EX: 3.7 kg | p=0.155 | |||
| Australia | Intensity: 50–60% HRmax | Independent and paired t- tests | CON: 5.2 kg | |||||
| BMI: | Adherence: 94% | Progression: Increase intensity to 60–70% | ||||||
| 35.1 kg/m2 | ||||||||
| Attrition: | ||||||||
| Sedentary sample? Yes | ||||||||
| N/R | ||||||||
|
| ||||||||
| Oostdam29 (2012) | RCT | Age: 30.8y (EX) | Supervised | Frequency 2x/week | Total GWG (4) | ITT analysis | Total GWG at 32 weeks: | |
| N=121 | 30.1y (CON) | Duration: 17 weeks | Duration: 60 minutes | Linear regression | ||||
| PA Only | Intensity: Strength (30–60% of 1 RM) Aerobic (60–80%) | EX: 6.2 kg | ||||||
| Amsterdam | Gestation: 15 weeks | Covariates: Baseline values, group allocation | CON: 5.6 kg (β=0.65 kg; 95% CI: -1.23, 2.52) | |||||
| Adherence: 16.3% | Borg Scale of 12 | |||||||
| BMI: | Progression: The program will progress when intensity reaches 12. | |||||||
| 33.0 kg/m2 (EX) | Attrition: 29.8% (combined) | |||||||
| 33.9 kg/m2 (CON) | ||||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Price28 (2012) | RCT | Age: 30.5y (EX) | Supervised | Frequency 4x/week | Total GWG (3) | Repeated measures ANOVA | Total GWG: | |
| N=91 | 27.6y (CON) | Duration: 22–24 weeks | Duration: 45–60 minutes | |||||
| PA Only | Intensity: Moderate 12–14 on Borg Scale | EX: 12.4 kg | p=0.15 | |||||
| US | Gestation: 12–14 weeks | CON: 10.5 kg | ||||||
| Adherence: 77% | Walk on own for 30–60 mins | |||||||
| BMI: | Progression: N/R | |||||||
| 26.6 kg/m2 (EX) | Attrition: | |||||||
| 28.7 kg/m2 (CON) | ||||||||
| EX: 27.9% CON: 35.4% | ||||||||
| Sedentary sample? Yes | ||||||||
|
| ||||||||
| Santos26 (2005) | RCT - Block | Age: 26.0y (EX) | Supervised | Frequency 3x/week | Total GWG (4) | ITT analysis | Total GWG: | |
| N=92 | 28.6y (CON) | Duration: 12 weeks | Duration: 60 minutes | Repeated measures | ||||
| PA Only | Intensity: 50–60% HRmax | EX: 5.7 kg | p=0.605 | |||||
| Brazil | Gestation: | <140 bpm | ANCOVA | CON: 6.3 kg | ||||
| 17.5 weeks (EX) | Adherence: 40% | Progression: N/R | Covariates: baseline values of age, gestational age, maternal weight | |||||
| 18.4 weeks (CON) | ||||||||
| EX: 40% CON: 50% | ||||||||
| BMI: | ||||||||
| 28.0 kg/m2 (EX) | Attrition: | |||||||
| 27.5 kg/m2 (CON) | ||||||||
| EX: 19.6% CON: 23.9% | ||||||||
| Sedentary sample? N/R | ||||||||
|
| ||||||||
| Yeo24 (2009) | RCT | Age: | Supervised: Yes, but | Walkers | Total GWG (1) | One-sample t- test | Total GWG: | |
| N=124 | 20–34y: 66.7% (EX) | decreased over time | Frequency 5x/week | % IOM Guidelines | ||||
| 20–34y: 66.7% (CON) | Duration: 20 weeks | Duration: 40 minutes | Excessive | Fisher’s exact test | EX: 15.4 kg | p>0.05 | ||
| US | ≥35y: 31.8% (EX) | PA Only | Intensity: 55–69% APMHR | CON: 15.9 kg | ||||
| ≥35y: 33.3% (CON) | RPE/Borg Scale: 12–13 | |||||||
| Adherence: 65% | IOM Guidelines - Excessive | |||||||
| Gestation: 18 weeks | Stretchers | |||||||
| Attrition: | Frequency 5x/week | EX: 100.0% a | p=0.041 | |||||
| BMI ≥ 29kg/m2: | Duration: 40 minutes | |||||||
| N/R | CON: 88.6%b | |||||||
| 80.9% (EX) | Intensity: None | |||||||
| 81.6% (CON) | Progression: N/R | |||||||
| Sedentary sample? Yes | ||||||||
Note:
A successful intervention was defined as a statistically significant difference in gestational weight gain and/or percent body fat between the exercise and control conditions.
Conditions with different letters indicates significant between-group differences. PA= physical activity; EX = exercise condition; CON = control condition; UW=underweight; NW=normal weight; OWOB=overweight and obese; GWG=gestational weight gain; N/R=not reported. IOM Guidelines: 2009 Gestational Weight Gain Guidelines set forth by the Institute of Medicine. APMHR= Age-predicted maximum heart rate; HR=heart rate; RCT=randomized controlled trial; quasi= quasi-experimental study design, %BF = percent body fat.
denotes the calculation used for total weight gain of the following four definitions: (1) Weight prior to delivery (or last prenatal or lab visit) minus pre-pregnancy weight; (2) weight at the end of the intervention minus weight at the start of the intervention; (3) weight prior to delivery (or last prenatal or lab visit) minus weight at study entry; (4) calculation for total weight gain was not specified. For studies not reporting exact p-values, p<0.05 was used for significant and p>0.05 for non-significant findings, unless specified otherwise.
Similar to the comparison between ‘successful’ and ‘unsuccessful’ interventions, the doses of exercises varied substantially among ‘successful’ interventions. As such, there were no discernible patterns of exercise dose and the calculated reductions in weight gain within the ‘successful’ exercise interventions.
Discussion
The purpose of this review was to examine the relationship between exercise dose and weight gain during pregnancy in exercise interventions. No clear patterns or consistencies among the prescribed dose and the impact on GWG emerged from the literature reviewed. It was anticipated that ‘successful’ interventions would have had a higher prescribed dose of exercise compared to the ‘unsuccessful’ interventions, thereby demonstrating a dose-response effect; however this finding was not confirmed.
It is plausible that a dose-response effect may have been present; however, given the high variability of the exercise dose components (i.e. frequency, intensity and duration) and varying participant and intervention characteristics (including adherence), it was difficult to confirm its existence. Nevertheless, one study among the ‘successful’ interventions potentially illustrated this effect by comparing three conditions of varying patterns of exercise doses across pregnancy (low-to-high dose, moderate-to-moderate dose and high-to-low dose).37 This study found that women in the low-to-high dose exercise condition gained significantly less body fat during pregnancy compared to the other conditions. This finding demonstrated that a progressive dose of exercise from early to late pregnancy may be predictive of weight gain, suggesting that higher dose of exercise may be necessary in the latter trimester of pregnancy to elicit greater reductions in body fat and weight gain. This was demonstrated in both the moderate-to-moderate and high-to-low conditions where the dose of exercise was either maintained or decreased during the time period (20th to 30th weeks of gestation) when the rate adipose tissue deposition was accelerating47 and as such may have been insufficient to reduce body fat or weight gain. Importantly, these findings suggest that high levels of exercise at the start of pregnancy may not be protective of weight gain as demonstrated by the high-to-low dose condition. In this group, women started with a high dose of exercise followed by a low dose. These women gained significantly more weight compared to the low-to-high condition.
Aside from the unexpected results regarding exercise dose, other patterns emerged between the ‘successful’ and ‘unsuccessful’ interventions. A majority (75%) of ‘successful’ interventions were implemented in normal weight pregnant women. One possible reason for the significant reduction in weight gain among these women may be the decreased energy cost with movement. Previous literature has established a positive relationship between body weight and energy expenditure.48, 49 That is, the energy expenditure and therefore physical effort during any given weight-bearing activity is far greater in an individual with a high body weight compared to a lighter individual. This may result in increased difficulty during energy-demanding tasks (i.e. exercise).49 Additionally, 83% of the ‘successful’ and 62% of ‘unsuccessful’ interventions implemented among normal weight and overweight/obese women, respectively, were prescribed weight-bearing exercise. This form of exercise is far more energy-costly for overweight and obese women compared to non-weight bearing exercise.50 Because of this, normal weight women may be more receptive to PA interventions when compared to overweight or obese women. Another explanation for this finding could be that normal weight women may have been more active during the preconception period compared to overweight and obese women and as a result, maintaining PA during pregnancy may have been easier than initiating this health behavior at the onset of pregnancy.
Greater adherence and lower attrition rates were likely the strongest contributors to the significant reduction in weight gain in the ‘successful’ interventions compared to the ‘unsuccessful’ interventions. Haakstad et al. (2011) demonstrated the influence of adherence and attrition rates in their study as the intention-to-treat analysis revealed no significant differences between the exercise and control conditions; however women attending 100% of the exercise sessions gained significantly less weight and 0% exceeded the IOM guidelines compared to less compliant women.34
Another substantial difference between the ‘successful’ and ‘unsuccessful’ interventions was the measure of GWG used across the studies. The most common measurement used was total weight gained during pregnancy, which is simple to use and calculate. However, this aggregate measure provides little detail (e.g., patterns, rates, accumulating tissues) about weight gain compared to other measures. All studies utilized this measure to quantify GWG; however, 75% of ‘successful’ interventions used at least two measures of GWG versus only 15% of ‘unsuccessful’ interventions. It is possible that studies employing multiple measures of GWG placed more emphasis on weight gain, as weight gain was the primary outcome in 88% of the studies utilizing at least two measures of GWG. Other measures of weight gain included weekly rate of weight gain, percent body fat and the 2009 IOM guidelines. While it is acknowledged that using multiple measures of weight gain may increase the likelihood of finding positive results, each of these measures may provide a different piece of information (e.g. mean weight gain, % excessive, early vs late weight gain, % body fat) thus, potentially providing a more complete evaluation of the effect of an exercise intervention on weight gain. Additionally, multiple measures of weight gain may overcome the potential bias of total weight gain, the other measures are not without limitations (e.g. assumption of constant rate of weight gain during pregnancy [0.5–2kg], misclassification).51
An additional limitation regarding the weight gain measurements methods used was the inability to distinguish between the different types of tissues that may accumulate during pregnancy (i.e. adipose, muscle, etc.). While it is established that weight gain during pregnancy can be partly attributed to maternal fat stores, weight of the fetus, supportive tissues (i.e. placenta, uterus, and amniotic fluid) and tissue for lactation processes, the composition of the remaining accumulating tissues is unknown. Differentiating between fat mass and fat-free mass is critical especially when the exposure is exercise. Previous literature suggests that exercise of moderate-to-vigorous intensity can induce increases in muscle mass and reductions in body fat tissue, providing significant metabolic benefits (e.g., glycemic and lipidemic control) to both the mother and fetus.52–55 However, the weight gain measures as opposed to measures of body composition, especially among women engaging in resistance training,26–29, 34, 40, 41, 43, 56 may have resulted in the reporting of null findings, when in fact, significant and beneficial changes in body composition occurred.
This review has a number of significant strengths despite being unable to adequately determine the role of exercise dose and GWG. To the best of our knowledge, this was the first study to attempt to assess the impact of exercise dose on weight gain during pregnancy. In addition, the less-restrictive inclusion criteria utilized in this review resulted in the most comprehensive collection of exercise interventions allowing for a more thorough evaluation of the current evidence. Moreover, this was the first review to evaluate the characteristics of ‘successful’ and ‘unsuccessful’ exercise interventions and reductions GWG which may provide useful information for the development and implementation of future interventions. However, as with any study, this review has limitations. First, it is possible that while conducting the literature search that some eligible interventions were missed, potentially limiting a complete evaluation of the current evidence. Second, due to the heterogeneity of the exercise doses prescribed and insufficient reporting of the dose received, we were unable to assess the impact on GWG as intended. Because of this, the exercise dose associated with reductions in GWG among ‘successful’ interventions is ‘unquantifiable.’ Third, given the large number of ‘unsuccessful’ interventions, inclusion of quasi-experimental studies, and homogeneous samples (i.e. normal weight women) utilized in the ‘successful’ interventions, it is difficult to conclude any causal inferences that are generalizable to all pregnant women.
In light of these findings and given the importance of GWG and the potential intergenerational effects of excessive weight gain57 it is strongly recommended that future researchers allocate their resources to designing a large randomized controlled trial consisting of varying exercise doses and a large anthropometrically (i.e. body fat) diverse sample of pregnant women. This may be more achievable by increasing adherence and compliance to exercise interventions as it is likely that these factors had a strong influence on the success of these interventions. Thus, it suggested that researchers identify strategies on how to improve adherence and compliance in this population (e.g. incentives, decrease participant burden). Moreover, it is recommended that researchers investigate the role of a diet intervention independent of exercise, as the one successful intervention among overweight and obese pregnant women in this review43 included diet, which may explain their significant finding. It is acknowledged that several diet interventions have incorporated exercise;19 however few of these studies provided a sufficient number of control conditions to assess the impact of diet and exercise independently. Further, it is strongly suggested that future researchers utilize appropriate measures of changes in body composition (i.e. body fat and lean body mass) in addition to weight gain. Moreover, it is imperative that investigators validate that the exercise dose prescribed is the exercise dose received and to accomplish this, the utilization of objective measures of exercise dose (i.e. heart rate monitors, indirect calorimetry, accelerometers etc.) are required. Additionally, examining the effects of exercise dose on weight gain across pregnancy (early vs late) and the potential impact on the neonate is encouraged. Lastly, it is recommended that researchers objectively measure daily PA to assess if interventions lead to compensatory changes across the day. Lastly,
Conclusion
Despite the unclear evidence of the effect of exercise dose on GWG, we did find successful interventions that suggest exercise during pregnancy may reduce excessive GWG. In addition, adherence and retention rates were likely strong contributors to the success of exercise interventions on GWG. No injuries and/or maternal or fetal complications related to exercise occurred during these interventions, suggesting that exercise is a relatively safe behavior for women without a high-risk pregnancy to perform during pregnancy. In addition to GWG, exercise during pregnancy possesses a myriad of other health benefits for both mother and child58–62 and therefore should be encouraged in all women during pre and postnatal periods.
Practical implications.
An exercise dose that enables women to control their weight during pregnancy is still unknown; this is likely due to the absence of appropriate measurement methods of the exercise dose received during interventions.
Adherence and compliance are likely to be strong contributors to the success of exercise interventions in pregnant women.
The continuous use of poor measurements of gestational weight gain, changes in body composition and exercise dose will likely perpetuate the production of null findings found in exercise interventions among pregnant women.
Acknowledgments
None. The authors received no external financial support to aid with writing this review.
References
- 1.Archer E, Lavie CJ, McDonald SM, et al. Maternal Inactivity: 45-Year Trends in Mothers’ Use of Time. Mayo Clinic Proceedings. 2013;88(12):1368–1377. doi: 10.1016/j.mayocp.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Archer E, Shook RP, Thomas DM, et al. 45-Year Trends in Women's Use of Time and Household Management Energy Expenditure. PLoS One. 2013;8(2):e56620. doi: 10.1371/journal.pone.0056620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rhodes JC, Schoendorf KC, Parker JD. Contribution of excess weight gain during pregnancy and macrosomia to the cesarean delivery rate, 1990–2000. Pediatrics. 2003;111(Supplement 1):1181–1185. [PubMed] [Google Scholar]
- 4.Helms E, Coulson CC, Galvin SL. Trends in weight gain during pregnancy: a population study across 16 years in North Carolina. Am J Obstet Gynecol. 2006;194(5):e32–e34. doi: 10.1016/j.ajog.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 5.Bergouignan A, Rudwill F, Simon C, Blanc S. Physical inactivity as the culprit of metabolic inflexibility: evidence from bed-rest studies. Journal of Applied Physiology. 2011;111(4):1201–1210. doi: 10.1152/japplphysiol.00698.2011. [DOI] [PubMed] [Google Scholar]
- 6.WHO. PROMOTING OPTIMAL FETAL DEVELOPMENT: Report of a technical consultation. Geneva, Switzerland: World Health Organizatin; 2006. [Google Scholar]
- 7.Rooney BL, Schauberger CW. Excess Pregnancy Weight Gain and Long – Term Obesity: One Decade Later. Obstet Gynecol. 2002;100(2):245–252. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- 8.Naeye RL. Weight gain and the outcome of pregnancy. Am J Obstet Gynecol. 1979;135(1):3–9. [PubMed] [Google Scholar]
- 9.Hedderson MM, Gunderson EP, Ferrara A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet Gynecol. 2010;115(3):597. doi: 10.1097/AOG.0b013e3181cfce4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Z, Du J, Shao L, et al. Prepregnancy body mass index, gestational weight gain, and pregnancy outcomes in China. International Journal of Gynecology and Obstetrics. 109(1):41–44. doi: 10.1016/j.ijgo.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126. [PMC free article] [PubMed] [Google Scholar]
- 12.Thangaratinam S, Rogozińska E, Jolly K, et al. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ: British Medical Journal. 2012;344 doi: 10.1136/bmj.e2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Church T. Exercise in obesity, metabolic syndrome, and diabetes. Prog Cardiovasc Dis. 2011;53(6):412–418. doi: 10.1016/j.pcad.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S. Exercise for the management of type 2 diabetes: a review of the evidence. Acta Diabetol. 2010;47(1):15–22. doi: 10.1007/s00592-009-0126-3. [DOI] [PubMed] [Google Scholar]
- 15.Streuling I, Beyerlein A, Rosenfeld E, Hofmann H, Schulz T, von Kries R. Physical activity and gestational weight gain: a meta-analysis of intervention trials. BJOG. 2011;118(3):278–284. doi: 10.1111/j.1471-0528.2010.02801.x. [DOI] [PubMed] [Google Scholar]
- 16.Fogelholm M, Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain – a systematic review. Obesity Reviews. 2000;1(2):95–111. doi: 10.1046/j.1467-789x.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- 17.USDHHS. 2008 Physical Activity Guidelines for Americans. Washington D.C: USDHHS; 2008. [Google Scholar]
- 18.Artal R, O'Toole M. Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br J Sports Med. 2003;37(1):6–12. doi: 10.1136/bjsm.37.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Streuling I, Beyerlein A, von Kries R. Can gestational weight gain be modified by increasing physical activity and diet counseling? A meta-analysis of interventional trials. The American journal of clinical nutrition. 2010;92(4):678–687. doi: 10.3945/ajcn.2010.29363. [DOI] [PubMed] [Google Scholar]
- 20.Choi J, Fukuoka Y, Lee JH. The effects of physical activity and physical activity plus diet interventions on body weight in overweight or obese women who are pregnant or in postpartum: a systematic review and meta-analysis of randomized controlled trials. Prev Med. 2013;56(6):351–364. doi: 10.1016/j.ypmed.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 22.Kuhlmann AK, Dietz PM, Galavotti C, England LJ. Weight-management interventions for pregnant or postpartum women. Am J Prev Med. 2008;34(6):523–528. doi: 10.1016/j.amepre.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reduce gestational weight gain: a meta – analysis. Obesity Reviews. 2011;12(7):e602–e620. doi: 10.1111/j.1467-789X.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 24.Yeo S. Adherence to walking or stretching, and risk of preeclampsia in sedentary pregnant women. Res Nurs Health. 2009;32(4):379–390. doi: 10.1002/nur.20328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sedaghati P, Ziaee V, Ardjmand A. The effect of an ergometric training program on pregnants weight gain and low back pain. Gazzetta Medica Italiana Archivio per le Scienze Mediche. 2007;166(6):209. [Google Scholar]
- 26.Santos IA, Stein R, Fuchs SC, et al. Aerobic exercise and submaximal functional capacity in overweight pregnant women - A randomized trial. Obstet Gynecol. 2005;106(2):243–249. doi: 10.1097/01.AOG.0000171113.36624.86. [DOI] [PubMed] [Google Scholar]
- 27.Ruiz JR, Perales M, Pelaez M, Lopez C, Lucia A, Barakat R. Mayo Clinic proceedings. Vol. 88. Elsevier; 2013. Supervised Exercise–Based Intervention to Prevent Excessive Gestational Weight Gain: A Randomized Controlled Trial; pp. 1388–1397. [DOI] [PubMed] [Google Scholar]
- 28.Price BB, Amini SB, Kappeler K. Exercise in pregnancy: effect on fitness and obstetric outcomes–a randomized trial. Med Sci Sports Exerc. 2012;44(12):2263–2269. doi: 10.1249/MSS.0b013e318267ad67. [DOI] [PubMed] [Google Scholar]
- 29.Oostdam N, van Poppel M, Wouters M, et al. No effect of the FitFor2 exercise programme on blood glucose, insulin sensitivity, and birthweight in pregnant women who were overweight and at risk for gestational diabetes: results of a randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2012;119(9):1098–1107. doi: 10.1111/j.1471-0528.2012.03366.x. [DOI] [PubMed] [Google Scholar]
- 30.Ong M, Guelfi K, Hunter T, Wallman K, Fournier P, Newnham J. Supervised home-based exercise may attenuate the decline of glucose tolerance in obese pregnant women. Diabetes Metab. 2009;35(5):418–421. doi: 10.1016/j.diabet.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Marquez-Sterling S, Perry AC, Kaplan T, Halberstein RA, Signorile JF. Physical and psychological changes with vigorous exercise in sedentary primigravidae. Med Sci Sports Exerc. 2000;32(1):58–62. doi: 10.1097/00005768-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Kardel KR, Kase T. Training in pregnant women: effects on fetal development and birth. Am J Obstet Gynecol. 1998;178(2):280–286. doi: 10.1016/s0002-9378(98)80013-6. [DOI] [PubMed] [Google Scholar]
- 33.Hopkins SA, Baldi JC, Cutfield WS, McCowan L, Hofman PL. Exercise training in pregnancy reduces offspring size without changes in maternal insulin sensitivity. J Clin Endocrinol Metab. 2010;95(5):2080–2088. doi: 10.1210/jc.2009-2255. [DOI] [PubMed] [Google Scholar]
- 34.Haakstad LA, Bø K. Effect of regular exercise on prevention of excessive weight gain in pregnancy: a randomised controlled trial. The European Journal of Contraception and Reproductive Health Care. 2011;16(2):116–125. doi: 10.3109/13625187.2011.560307. [DOI] [PubMed] [Google Scholar]
- 35.Garshasbi A, Faghih Zadeh S. The effect of exercise on the intensity of low back pain in pregnant women. International Journal of Gynecology & Obstetrics. 2005;88(3):271–275. doi: 10.1016/j.ijgo.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Collings CA, Curet L, Mullin J. Maternal and fetal responses to a maternal aerobic exercise program. Am J Obstet Gynecol. 1983;145(6):702–707. doi: 10.1016/0002-9378(83)90576-8. [DOI] [PubMed] [Google Scholar]
- 37.Clapp JF, III, Kim H, Burciu B, Schmidt S, Petry K, Lopez B. Continuing regular exercise during pregnancy: effect of exercise volume on fetoplacental growth. Am J Obstet Gynecol. 2002;186(1):142–147. doi: 10.1067/mob.2002.119109. [DOI] [PubMed] [Google Scholar]
- 38.Clapp JF, III, Kim H, Burciu B, Lopez B. Beginning regular exercise in early pregnancy: effect on fetoplacental growth. Am J Obstet Gynecol. 2000;183(6):1484–1488. doi: 10.1067/mob.2000.107096. [DOI] [PubMed] [Google Scholar]
- 39.Cavalcante SR, Cecatti JG, Pereira RI, Baciuk EP, Bernardo AL, Silveira C. Water aerobics II: maternal body composition and perinatal outcomes after a program for low risk pregnant women. Reprod Health. 2009;6(1):19126239. doi: 10.1186/1742-4755-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barakat R, Perales M, Bacchi M, Coteron J, Refoyo I. A Program of Exercise Throughout Pregnancy. Is It Safe to Mother and Newborn? Am J Health Promot. 2013 doi: 10.4278/ajhp.130131-QUAN-56. [DOI] [PubMed] [Google Scholar]
- 41.Barakat R, Lucia A, Ruiz JR. Resistance exercise training during pregnancy and newborn's birth size: a randomised controlled trial. Int J Obes. 2009;33(9):1048–1057. doi: 10.1038/ijo.2009.150. [DOI] [PubMed] [Google Scholar]
- 42.Ruchat S-M, Davenport MH, Giroux I, et al. Nutrition and exercise reduce excessive weight gain in normal-weight pregnant women. Med Sci Sports Exerc. 2012;44(8):1419–1426. doi: 10.1249/MSS.0b013e31825365f1. [DOI] [PubMed] [Google Scholar]
- 43.Nascimento S, Surita F, Parpinelli M, Siani S, Pinto e Silva J. The effect of an antenatal physical exercise programme on maternal/perinatal outcomes and quality of life in overweight and obese pregnant women: a randomised clinical trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2011;118(12):1455–1463. doi: 10.1111/j.1471-0528.2011.03084.x. [DOI] [PubMed] [Google Scholar]
- 44.Davenport MH, Mottola MF, McManus R, Gratton R. A walking intervention improves capillary glucose control in women with gestational diabetes mellitus: a pilot study. Applied physiology, nutrition, and metabolism. 2008;33(3):511–517. doi: 10.1139/H08-018. [DOI] [PubMed] [Google Scholar]
- 45.American College of Sports Medicine. Guidelines for Graded Exercise Testing and Exercise Prescription. 2. Lea & Febiger; 1980. [Google Scholar]
- 46.Wolfe LA, Davies GAL. Canadian guidelines for exercise in pregnancy. Clin Obstet Gynecol. 2003;46(2):488–495. doi: 10.1097/00003081-200306000-00027. [DOI] [PubMed] [Google Scholar]
- 47.Villar J, Cogswell M, Kestler E, Castillo P, Menendez R, Repke JT. Effect of fat and fat-free mass deposition during pregnancy on birth weight. Am J Obstet Gynecol. 1992;167(5):1344–1352. doi: 10.1016/s0002-9378(11)91714-1. [DOI] [PubMed] [Google Scholar]
- 48.Leibel RL, Rosenbaum M, Hirsch J. Changes in Energy Expenditure Resulting from Altered Body Weight. N Engl J Med. 1995;332(10):621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 49.Archer E, Hand GA, Hébert JR, et al. Validation of a Novel Protocol for Calculating Estimated Energy Requirements and Average Daily Physical Activity Ratio for the U.S. Population: 2005–2006. Mayo Clinic Proceedings. 2013;88(12):1398–1407. doi: 10.1016/j.mayocp.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 50.Lafortuna CL, Agosti F, Galli R, Busti C, Lazzer S, Sartorio A. The energetic and cardiovascular response to treadmill walking and cycle ergometer exercise in obese women. European journal of applied physiology. 2008;103(6):707–717. doi: 10.1007/s00421-008-0758-y. [DOI] [PubMed] [Google Scholar]
- 51.Hutcheon JA, Bodnar LM, Joseph K, Abrams B, Simhan HN, Platt RW. The bias in current measures of gestational weight gain. Paediatr Perinat Epidemiol. 2012;26(2):109–116. doi: 10.1111/j.1365-3016.2011.01254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tremblay A, Simoneau J-A, Bouchard C. Impact of exercise intensity on body fatness and skeletal muscle metabolism. Metabolism. 1994;43(7):814–818. doi: 10.1016/0026-0495(94)90259-3. [DOI] [PubMed] [Google Scholar]
- 53.Johnson NA, Sachinwalla T, Walton DW, et al. Aerobic exercise training reduces hepatic and visceral lipids in obese individuals without weight loss. Hepatology. 2009;50(4):1105–1112. doi: 10.1002/hep.23129. [DOI] [PubMed] [Google Scholar]
- 54.Irving BA, Davis CK, Brock DW, et al. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008;40(11):1863. doi: 10.1249/MSS.0b013e3181801d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bryner RW, Toffle RC, Ullrich IH, Yeater RA. The effects of exercise intensity on body composition, weight loss, and dietary composition in women. J Am Coll Nutr. 1997;16(1):68–73. doi: 10.1080/07315724.1997.10718651. [DOI] [PubMed] [Google Scholar]
- 56.Coffey V, Hawley J. The Molecular Bases of Training Adaptation. Sports Med. 2007;37(9):737–763. doi: 10.2165/00007256-200737090-00001. [DOI] [PubMed] [Google Scholar]
- 57.Drake AJ, Reynolds RM. Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction. 2010;140(3):387–398. doi: 10.1530/REP-10-0077. [DOI] [PubMed] [Google Scholar]
- 58.Yeo S, Steele NM, Chang MC, Leclaire SM, Ronis DL, Hayashi R. Effect of exercise on blood pressure in pregnant women with a high risk of gestational hypertensive disorders. The Journal of reproductive medicine. 2000;45(4):293–298. [PubMed] [Google Scholar]
- 59.Voldner N, FrØSlie KF, Bo K, et al. Modifiable determinants of fetal macrosomia: role of lifestyle-related factors. Acta Obstet Gynecol Scand. 2008;87(4):423–429. doi: 10.1080/00016340801989825. [DOI] [PubMed] [Google Scholar]
- 60.Lox CL, Treasure DC. Changes in Feeling States Following Aquatic Exercise During Pregnancy. Journal of Applied Social Psychology. 2000;30(3):518–527. [Google Scholar]
- 61.Kramer MS. Aerobic exercise for women during pregnancy. Cochrane Database Syst Rev. 2006;(2):CD000180. doi: 10.1002/14651858.CD000180. [DOI] [PubMed] [Google Scholar]
- 62.Bung P, Artal R, Khodiguian N, Kjos S. Exercise in Gestational Diabetes: An Optional Therapeutic Approach? Diabetes. 1991;40(Supplement 2):182–185. doi: 10.2337/diab.40.2.s182. [DOI] [PubMed] [Google Scholar]