Abstract
Background: The differential diagnosis of salivary carcinomas is always difficult and challenging. Salivary neoplasms often shows more than one growth pattern and significant morphologic variability may exist within a single tumor and between different tumors. The aim of this study was to examine the role of DOG1 (discovered on gastrointestinal tumor-1) and p63 immunohistochemistry in the diagnosis and differential diagnosis of salivary carcinomas. Methods: we examined the expression of DOG1 and p63 immunohistochemistry in 33 mucoepidermoid carcinomas (MEC), 9 acinic cell carcinomas (ACC), 10 adenoid cystic carcinomas (AdCC) and 4 myoepithelial carcinomas. Results: All ACC showed strong to moderate positivity for DOG1 (P=0.001) and all were totally negative for p63. All MEC expressed strong to moderate positivity for p63 (P=0.001) while only (9.1%) were weak to moderately positive for DOG1. (80%) AdCC were moderately positive for DOG1 in ductal and myoepithelial components and (100%) showed moderate positivity for p63 in myoepithelial cells only (P=0.001). All myoepithelial carcinomas were DOG1 negative, 2 (50%) were weakly positive for p63 while the other 2 were moderately positive (P=0.5). Conclusion: DOG1 is a sensitive marker in the diagnosis of acinic cell carcinoma, p63 is sensitive in the diagnosis of mucoepidermoid carcinoma, the combined use of both markers is helpful and statistically significant in the differential diagnosis of acinic cell carcinoma versus mucoepidermoid carcinoma, both markers can help in the diagnosis of adenoid cystic carcinoma but they have no role in the diagnosis of myoepithelial carcinoma.
Keywords: Salivary carcinomas, DOG1, p63, immunohistochemistry
Introduction
The basic structural component of salivary gland exhibits a two tiered organization comprising luminal (acinar and ductal cells) and abluminal cells (myoepithelial and basal cells). The secretory acini and intercalated ducts are wrapped by myoepithelial cells, while the striated ducts and subsequent conducting portions are supported by basal cells [1]. Most of salivary gland tumors arise from or differentiate towards the same cell lines i.e. epithelial (acinar and ductal), myoepithelial, and basal. This results in a considerable overlap at all levels, compounded by the fact that each of these cells can undergo a variety of metaplastic changes (i.e. oncocytic, sebaceous, squamous, clear, chondroid) [2]. Salivary gland tumors are uncommon and comprise approximately 1% of all neoplasms in the whole body. Malignant salivary neoplasms account for 0.3% of human malignancies and for 3% to 6% of all head and neck cancers [3]. The recent WHO classification of head and neck tumors contains 24 different entities of salivary carcinomas [4]. A more practical and simplified grouping can be used based on the degree of malignancy comprising high grade, intermediate grade and low grade. Another practical grouping is based on the relative frequency of their occurrence and this distinguished mucoepidermoid carcinoma, adenoid cystic carcinoma, and acinic cell carcinoma as a group of most frequently occurring carcinomas [5]. Salivary neoplasms often shows more than one growth pattern and significant morphologic variability may exist within a single tumor and between different tumors [6].
Mucoepidermoid carcinoma is the most common primary malignant salivary tumor of both adults and children [7]. Differential diagnosis of MEC is broad and is dependent on tumor grade and prevalence of variant morphology (oncocytes, clear cells) and MEC may take the form of clear cell carcinoma [8]. Acinic cell carcinoma is a malignant epithelial neoplasm that frequently demonstrates variable microscopic morphologies which can make definitive diagnosis quite challenging, one particular difficult task is the differentiation between the papillary cystic and microcystic acinic cell carcinoma and mucoepidermoid carcinoma as both have cystic changes and mucinous secretions [9]. Myoepithelial carcinomas have varied cell types from spindled to epithelial, plasmacytoid and mixed forms as well as clear cytoplasm that can enter in the differential diagnosis of MEC and other salivary tumors with clear cell change [10]. Adenoid cystic carcinoma shows cribriform, tubular and solid patterns. It contains pseudocysts with basophilic and eosinophilic appearing material; its main differential diagnosis is with polymorphus low grade adenocarcinoma [6]. This histopathological overlap between salivary tumors requires the need for immunohistochemical markers for its microscopic identification.
The gene known as anoctamin-1 (ANO-1,also known as discovered on GIST-1 or (DOG1) was initially noted by gene expression profiling to be differentially expressed in gastric intestinal tumors (GIST-1) when compared with a variety of other mesenchymal tumors. Its main function as a calcium activated chloride channel was recently discovered and has suggested a potential role in secretory cell types such as those of the salivary gland and perhaps tumors derived of these cell types. Interestingly, studies in murine models have demonstrated that DOG1 is not only present but also required for normal salivary and secretory activity, however, DOG1 expression has not been studied well in human salivary tissues [11].
P63 is a P53 homologue required for limb and epidermal morphogenesis. The role of P63 in tumorogenesis is not fully understood at this time. The elucidation of its role has been difficult because P63 encodes six different proteins with distinct and even opposing functions including inhibiting as well as inducing apoptosis. P63 is expressed in basal and myoepithelial cells of human normal and tumor salivary gland tissues [12].
The aim of this study was to examine the role of DOG1 and P63 immunohistochemistry in the diagnosis and differential diagnosis of salivary carcinomas.
Materials and methods
Tissue and patient data
The current study was conducted on all salivary carcinomas received in the pathology lab. of Ain Shams Specialized Hospital during the period from January 2006 to December 2014. After exclusion of cases with insufficient material, fifty six salivary carcinomas were included in our study. The H&E (Haematoxylin and Eosin) slides were reviewed by both authors to confirm the diagnoses according to the WHO (World Health Organization) classification [4]. The histopathological diagnoses were mucoepidermoid carcinomas (33 cases) of which nine were low grade, seventeen intermediate grade and seven cases were high grade (Figure 2A), Adenoid cystic carcinomas (10 cases) (Figure 3A), Acinic cell carcinomas (9 cases) five of which were solid pattern (Figure 1A), three papillary cystic (Figure 1C) and one microcystic, and myoepithelial carcinomas (4 cases). The normal salivary tissue adjacent to tumors was used as internal control.
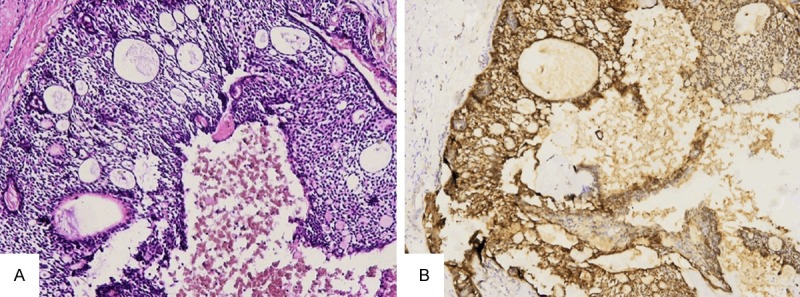
Figure 2.
Mucoepidermoid carcinoma. A. High grade mucoepidermoid carcinoma (H&E × 100). B. P63 in mucoepidermoid carcinoma showing nuclear staining in squamous, intermediate, and clear cells (p63 × 200).
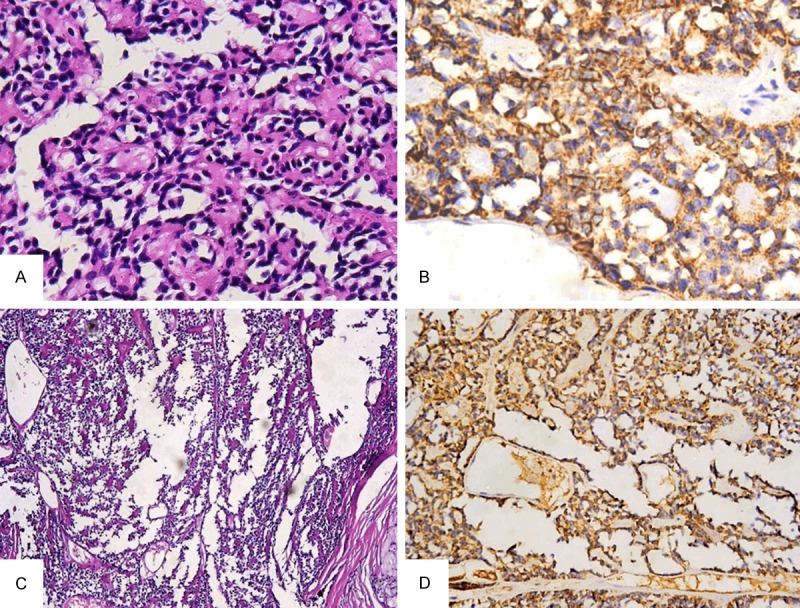
Figure 3.
Adenoid cystic carcinoma. A. Adenoid cystic carcinoma showing cribriform pattern (H&E × 100). B. DOG1 immunostaining in adenoid cystic carcinoma showing 3+ intense stain in both luminal and abluminal cells (DOG1 × 100).
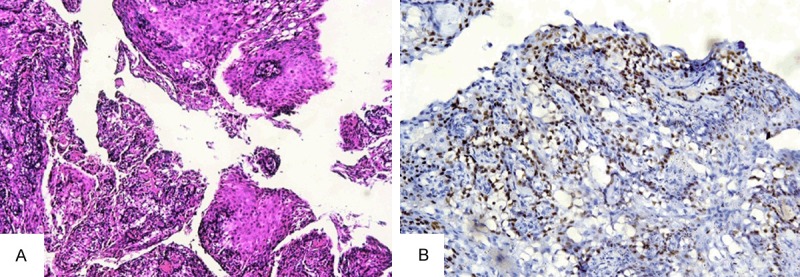
Figure 1.
Acinic cell carcinoma. A. Acinic cell carcinoma showing acinar cell component (H&E × 400). B. DOG1 immunostaining in acinic cell carcinoma showing 3+ granular cytoplasmic stain with foci of partial and complete cell membrane staining (DOG1 × 400). C. Acinic cell carcinoma “papillary cystic variant” (H&E × 100). D. DOG1 immunostaining in acinic cell carcinoma papillary cystic variant showing cytoplasmic and apical luminal stain in tumor cells (DOG1 × 200).
All patients who participated in this study signed a written, informed consent before surgery. The study was approved by the Research Ethical committee at Faculty of Medicine Ain Shams University.
Immunostaining procedure
Immunohistochemical staining was done using the streptavidin biotin immunoperoxidase technique. 4-5 mm thick tissue sections were cut from formalin fixed paraffin embedded blocks onto positively charged slides. Deparaffinization and rehydration were done through graded alcohols. The sections were heated in a microwave oven in 10 mM citrate buffer (pH 6.0) for 20 min for antigen retrival followed by blocking of endogenous peroxidase and incubation in Protein Block Serum-Free Solution (Dako Cytomation) for 10 minutes. Primary antibody was applied to each section followed by overnight incubation. Both DOG1 and P63 were rabbit monoclonal antibodies ‘DOG1 (clone 1.1, Thermo scientific catalog # MS-1933-P0) and P63 (Biocare medical, catalog # CM 163 B)’. Secondary antibody (ultravision large volume detection system kit: Antipolyvalent HRP, ready to use) was added to each section for 30 minutes. 3,3’-diaminobenzidine as the substrate or chromogen was used to form an insoluble brown product. Sections were counterstained with Harris Haematoxylin then mounted in Canada balsam.
Sections of gastrointestinal stromal tumor and the nuclei of the basal epithelium in normal prostate were used as positive control for DOG1 and P63 respectively. Negative control sections were incubated with normal rabbit serum instead of the primary antibody.
Interpretation of DOG1 immunostaining
The distribution and intensity of the stain were evaluated as follows: Distribution: The distribution of stain was evaluated semi-quantitatively according to the percentage of positive cells in at least five areas at a magnification of 400× and assigned to one of the following categories by double blinded pathologists (both authors); 0: no staining, 1+: <5% reactive tumor cells, 2+: 5-50% reactive tumor cells, 3+: >50% reactive tumor cells. Assessment of the staining was based on presence or absence of cell membrane (apical-luminal, basolateral and complete), cytoplasmic staining or both. Intensity: The staining intensity was scored as weak 1+, moderate 2+, and strong 3+. The staining of normal serous acini was used as 2+, more intense staining was graded 3+ and less intense as 1+.
Interpretation of P63 immunostaining
Immunostaining was scored as follows: Negative: less than 10% of tumor nuclei stained, weakly positive: 10-25%, moderately positive: 26-75%, and strongly positive: 76-100% of tumor nuclei stained. Only nuclear reactivity was considered positive. The grading was performed semi-quantitatively by double blinded pathologists (both authors).
Statistical analysis
Categorical variables are expressed as frequencies and percents. Fisher’s exact test was used to examine the relationship between Categorical variables. McNemar and Friedman tests were used to assess the statistical significance of the difference between two or more markers measured for the same study group. A significance level of P < 0.05 was used in all tests. All statistical procedures were carried out using SPSS version 15 for Windows (SPSS Inc, Chicago, IL, USA).
Results
DOG1 immunohistochemical expression
The normal salivary tissue adjacent to tumors used as internal control showed moderate (2+) membranous staining in serous acini in an apical luminal pattern together with cytoplasmic staining, mucinous acini showed less intense (1+) staining in the same pattern. Intercalated ducts were focally positive and more distal ducts were negative.
All nine acinic cell carcinomas (100%) were DOG1 positive (P=0.001) (statistically highly significant, HS), the staining distribution was 3+ in seven cases (77.7%) (Figure 1B), 2+ in two cases (22.2%), regarding the intensity six cases (66.6%) showed strong intensity and three cases (33.3%) showed moderate intensity. All cases showed diffuse granular cytoplasmic staining with foci of partial or complete membranous staining including the papillary cystic (Figure 1D) and microcystic patterns.
Thirty out of thirty three MEC (90.9%) were DOG1 negative, the remaining three cases (9.1%) showed cytoplasmic staining in the mucous and some of the intermediate cell components, the staining intensity was weak in 2 cases and moderate in one case and the distribution was 1+ in the first 2 cases and 2+ in the third one.
Eight out of ten (80%) adenoid cystic carcinomas showed positive DOG1 staining (P=0.001, HS), the distribution was 2+ in seven cases (70%), 3+ in one case (10%) (Figure 3B). The staining intensity was moderate to strong in all cases, the stain was seen both in the ductal and myoepithelial components, the former showed membranous and diffuse cytoplasmic staining while the latter showed only diffuse cytoplasmic staining. All myoepithelial carcinomas (4 cases) (100%) were DOG1 negative. DOG1 immunohistochemical results are summarized in Table 1 and statistical results are summarized in Table 3.
Table 1.
DOG1 immunohistochemical results
| Tumor type | Number of cases | Number of positive cases | % | Distribution of stain | Intensity of stain | Subcellular localization | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| 1+ | 2+ | 3+ | 1+ | 2+ | 3+ | |||||
| MEC | 33 | 3 | 9.1 | 2 | 1 | 0 | 2 | 1 | 0 | Cytoplasm of mucous and intermediate cells |
| ACC | 9 | 9 | 100 | 0 | 2 | 7 | 0 | 3 | 6 | Cytoplasm + foci of membranous staining |
| AdCC | 10 | 8 | 80 | 0 | 7 | 1 | 0 | 8 | 0 | Ductal: cell membrane+ cytoplasm, Myoepithelial: cytoplasm |
| Myoepithelial Carcinoma | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - |
Table 3.
Comparison between different types of tumors as regard sensitivity of diagnosis by DOG1 marker
| Tumor type | P* | Sig | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Mucoepidermoid | Acinic | Adenoid cystic | Myoepithelial carcinoma | ||||||||
|
|
|||||||||||
| N | % | N | % | N | % | N | % | ||||
| DOG1 | Negative | 30 | 90.9% | 0 | .0% | 2 | 20.0% | 4 | 100.0% | 0.001 | HS |
| Positive | 3 | 9.1% | 9 | 100.0% | 8 | 80.0% | 0 | .0% | |||
Fisher exact test;
N = number of cases, Sig = statistical significance, HS = highly significant.
P63 immunohistochemical expression
The normal salivary tissue adjacent to tumors showed P63 expression in the nuclei of basal cells and myoepithelial cells. All 33 (100%) MEC were P63 positive (P=0.001 HS) of which thirty one (93.9%) showed strong diffuse nuclear reactivity in intermediate, squamous, and clear cells while mucous cells were negative (Figure 2B). The remaining two cases (6%) showed moderate positivity in the same cell types. There was no difference in the staining pattern between different tumor grades. All nine (100%) acinic cell carcinomas were totally P63 negative. All adenoid cystic carcinomas (100%) (P=0.001, HS) showed moderate P63 reactivity in the nuclei of abluminal cells while the luminal cells were negative. Two out of four myoepithelial carcinomas (50%) exhibited moderate P63 positivity, the other two cases (50%) showed focal weak positive staining (P=0.5) (statistically non significant, NS). P63 immunohistochemical results are summarized in Table 2 and statistical results in Table 4.
Table 2.
P63 immunohistochemical results
| Tumor type | Number of cases | Number of positive cases | % | IHC score | Cellular localization | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Weak | Moderate | Strong | |||||
| MEC | 33 | 33 | 100 | 0 | 2 | 31 | Intermediate, squamous, clear cells |
| ACC | 9 | 0 | 0 | 0 | 0 | 0 | - |
| AdCC | 10 | 10 | 100 | 0 | 10 | 0 | Abluminal cells |
| Myoepithelial carcinoma | 4 | 4 | 100 | 2 | 2 | 0 | Myoepithelial cells |
Table 4.
Comparison between different types of tumors as regard sensitivity of diagnosis by p63 marker
| Tumor type | P* | Sig | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Mucoepidermoid | Acinic | Adenoid cystic | Myoepithelial carcinoma | ||||||||
|
|
|||||||||||
| N | % | N | % | N | % | N | % | ||||
| P63 | Negative | 0 | .0% | 9 | 100.0% | 0 | .0% | 2 | 50.0% | 0.001 | HS |
| Positive | 33 | 100.0% | 0 | .0% | 10 | 100.0% | 2 | 50.0% | |||
Fisher exact test;
N = number of cases, Sig = statistical significance, HS = highly significant.
The combined use of both markers was sensitive and statistically significant in acinic cell carcinomas (P=0.001) and mucoepidermoid carcinomas (P=0.004), while it was not significant in adenoid cystic carcinomas and myoepithelial carcinomas (P=0.5) Table 5.
Table 5.
Comparison between sensitivity of DOG1 and P63 in diagnosis of each of tumor type
| DOG1 | P63 | P* | Sig | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Negative | Positive | Negative | Positive | |||||||
|
|
||||||||||
| N | % | N | % | N | % | N | % | |||
| Mucoepidermoid | 30 | 90.9% | 3 | 9.1% | 0 | .0% | 33 | 100.0% | 0.001 | HS |
| Acinic | 0 | .0% | 9 | 100.0% | 9 | 100.0% | 0 | .0% | 0.004 | HS |
| Adenoid cystic | 2 | 20.0% | 8 | 80.0% | 0 | .0% | 10 | 100.0% | 0.5 | NS |
| Myoepithelial carcinoma | 4 | 100.0% | 0 | .0% | 2 | 50.0% | 2 | 50.0% | 0.5 | NS |
Mcnemar test;
N = number of cases, Sig= statistical significance, HS = highly significant, NS = non significant.
Discussion
The acinar ductal unit comprises the basic structural component of salivary gland in which acinar cells line the inner aspect of the acini while ductal epithelial cells line the inner aspect of striated ducts and excretory ducts. Myoepithelial cells surround the outer aspects of acini and are found scattered on the outer aspects of intercalated ducts. Basal (reserve) cells line the outer aspect of excretory ducts. The neoplastic process can arise from acinar/ductal or myoepithelial cells alone, or much more commonly both the inner and outer cell types participate in the tumor [13].
The WHO classification system 2005 recognizes 24 malignant and 10 benign salivary epithelial neoplasms [4]. The common salivary gland carcinomas are mucoepidermoid carcinoma, adenoid cystic carcinoma, and acinic cell carcinoma [14]. The overlap in the histopathological features of various types of salivary carcinomas often causes difficulties in reaching an accurate diagnosis so immunohistochemistry can be of great help to set the proper diagnosis [15]. In this study we examined the expression of DOG1 and P63 in various salivary carcinomas to assess their possible role in the diagnosis and differential diagnosis of these tumors.
Discovered on GIST-1, ANO-1 “anoctamin-1”, calcium activated chloride channel is a protein that was found to be selectively expressed in GIST using gene expression profiling [16]. Recently DOG1 has been characterized in pancreatic centroacinar cells and a subset of islet cells suggesting a potential exocrine/endocrine role [17]. Regarding salivary gland, DOG1 has been shown to be expressed and even required for normal salivary secretion in murine models [18].
DOG1 expression in salivary tissues was found to be localized immunohistochemically mainly in salivary acini, to a lesser extent in mucinous acini and the staining diminished at the level of intercalated ducts and was completely absent more proximally [19]. In our study we observed the same DOG1 staining pattern in the normal salivary tissue adjacent to tumors. In tumor tissues DOG1 showed positivity in all acinic cell carcinomas. The staining distribution (percent of positive cells) ranged from 2+ to 3+ and the staining intensity ranged from 3+ (intense) to 2+ (moderate). Regarding subcellular localization all cases (solid, papillary cystic and microcystic) showed diffuse granular cytoplasmic staining in addition to apical luminal staining and complete membranous staining in some foci. These results were similar to that of Chenevert et al. who found the strongest DOG1 expression in acinic cell carcinoma where all the cases were positive. This was expected as acinic cell carcinoma demonstrates serous acinar differentiation, but unlike our results the subcellular localization in their cases was mostly apical luminal with scattered foci of complete membranous and cytoplasmic staining. Their study did not comment on acinic cell carcinoma variants [19]. The difference in subcellular localization between the two studies can be due to differential distribution of isoforms.
Although serous acinar differentiation can be recognized on routine H&E stained slides, sometimes when this cell type is less prominent PAS-D (Periodic Acid Schiff stain after diastase digestion) can help to identify zymogen granules, yet sometimes these may be scarce especially in papillary cystic and microcystic variants [20], also other tumors like MEC which frequently show intracytoplasmic, intracystic or intraluminal mucinous material, that are mucicarmine positive, can also stain PAS-D. Moreover occasional acinic cell carcinomas with zymogen granules may aberrantly stain with mucicarmine [9]. So DOG1 positivity can be of great help to confirm the diagnosis of acinic cell carcinoma in these situations. In our study 90.9% of MEC were negative for DOG1. The positive cases (9.1%) stained both the mucous and some of the intermediate cell components. In concordance to our study of Chenevert el al. [19] found a negative DOG1 staining in most mucoepidermoid carcinomas but the positive cases showed only focal weak staining in mucous cell component. Thus DOG1 can be a helpful marker in the differentiation between acinic cell carcinoma and mucoepidermoid carcinoma in problematic cases.
Our results revealed negative DOG1 staining in all examined myoepithelial carcinomas, while the study of Chenevert et al. [19] showed only one positive case that was focally positive. Regarding adenoid cystic carcinomas our findings were mostly similar to both Lopes et al. [21] and Chenevert et al. [19], all three studies demonstrated DOG1 positivity in 70-80% of cases in both ductal and myoepithelial components. The positive DOG1 staining in the myoepithelial component is surprising as normal salivary tissue showed DOG1 negativity in this component. This can be explained by the presence of transformed phenotype of myoepithelial cells in salivary tumors [19]. Since adenoid cystic carcinoma is rarely in the differential diagnosis of acinic cell carcinoma and mucoepidermoid carcinoma so the role of DOG1 for their differentiation is limited.
P63 is a member of the P53 family of transcription factors that plays an important role in the development and differentiation of limbs and epithelial structures [22]. It is expressed in the basal cell layer of the skin and myoepithelial cells of the breast [23,24]. P63 is also a prostate basal cell marker and is required for prostate development [25]. Myoepithelial cell differentiation occurs to variable degrees in pleomorphic adenomas, adenoid cystic carcinomas, polymorphous low grade adenocarcinoma and epithelial myoepithelial carcinoma [26]. Intermediate cells of mucoepidermoid carcinoma also demonstrate ultra-structural characteristics of modified myoepithelial cells [27].
In our study all mucoepidermoid carcinomas showed positive strong to moderate nuclear staining for P63 in intermediate, squamous and clear cells. These results support those of Ralph and Douglas who reported strong positive nuclear staining for P63 in 100% of examined MEC [9]. Seethala et al. [28] as well as Bilal et al. [29] also reported the same results in their studies.
In acinic cell carcinoma all of examined cases were negative for P63, this was in accordance with the study of Seethala et al. [28] and Ralph and Douglas [9]. Who found negative P63 staining in all acinic cell carcinoma variants, while in the study of Bilal et al. [29] there was one positive case out of four examined acinic cell carcinomas, this case was papillary cystic variant and P63 stained intercalated ductal epithelial cells. All adenoid cystic carcinomas (10 cases) examined in our study showed positive moderate staining for P63 in abluminal cells only, these results were similar to the study of Seethala et al. [28] and Bilal et al. [29]. All myoepithelial carcinomas (4 cases) in our work were positive for P63, of which 2 cases showed moderate diffuse positivity and the other two were weakly positive so statistical studies revealed no significant results. In the study of Bilal et al. all myoepithelial carcinomas were positive for P63 but only focally in 10-25 % of tumor cells [29].
In conclusion, we tried in our study to clarify the possible role of DOG1 and P63 in the diagnosis and differential diagnosis between various types of salivary carcinomas. We found that P63 is always positive and statistically significant in diagnosing mucoepidermoid carcinomas while DOG1 is uniformly diffuse, strongly positive, and statistically significant in diagnosing adenoid cystic carcinomas. Since DOG1 can be positive in some cases of MEC (9.1%) so the combined use of both markers can be helpful and is statistically significant in the differentiation between MEC and ACC especially in such cases. The use of each marker can help in the diagnosis of adenoid cystic carcinomas taking in consideration its subcellular localization, while they have no role in the diagnosis of myoepithelial carcinomas.
Limitations of this study included a limited number of available cases for each tumor type and missing of some tumor types either due to their relatively infrequent occurrence or insufficient material in some cases. So we recommend further studies for both markers in all types of salivary carcinomas including larger number of cases.
Acknowledgements
The authors acknowledge Mrs. Manal Hossam El Din for her technical support in immunostaining procedure.
Disclosure of conflict of interest
None.
Abbreviations
- DOG1
discovered on gastrointestinal tumor-1
- MEC
mucoepidermoid carcinoma
- AdCC
adenoid cystic carcinoma
- ACC
acinic cell carcinoma
- WHO
World Health Organization
- PAS
periodic acid Schiff
- HS
highly significant
- NS
non significant
References
- 1.Cheuk W, Chan JK. Advances in salivary gland pathology. Histopathology. 2007;51:1–20. doi: 10.1111/j.1365-2559.2007.02719.x. [DOI] [PubMed] [Google Scholar]
- 2.Simpson RH. Classification of tumors of the salivary glands. Histopathology. 1994;24:187–191. doi: 10.1111/j.1365-2559.1994.tb01303.x. [DOI] [PubMed] [Google Scholar]
- 3.Speight PM, Barrett AW. Prognostic factors in malignant tumours of the salivary glands. Br J Oral Maxillofac Surg. 2009;47:587–593. doi: 10.1016/j.bjoms.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Barnes L, Eveson JW, Reichart P, Sudansky D, editors. World healh organization classification of tumors: Pathology and genetics of the head and neck tumors. Lyon, France: IARC Press; 2005. [Google Scholar]
- 5.Luukkaa H, Klemi P, Leivo I, Koivunen P, Laranne J, Makitie A, Virtaniemi J, Hinkka S, Grenman R. Salivary gland cancer in Finland 1991-96: An evaluation of 237 cases. Acta Otolaryngol. 2005;125:207–14. doi: 10.1080/00016480510003174. [DOI] [PubMed] [Google Scholar]
- 6.Turk AT, Wenig BM. Pitfalls in the Biopsy Diagnosis of Intraoral Minor Salivary Gland Neoplasms: Diagnostic Considerations and Recommended Approach. Adv Anat Pathol. 2014;21:1–11. doi: 10.1097/PAP.0000000000000000. [DOI] [PubMed] [Google Scholar]
- 7.Guzzo M, Ferrari A, Marcom I, Collini P, Gandda L, Pizzi N, Casanova M, Mattavelli F, Scaramellini G. Salivary gland neoplasms in children: the experience of the Instituto Nazionale Tumori of Milan. Pediatr Blood Cancer. 2006;47:806–10. doi: 10.1002/pbc.20637. [DOI] [PubMed] [Google Scholar]
- 8.Griffith CC, Seethala RR. Mucoepidermoid Carcinoma of Minor Salivary Glands: Potential Pitfalls and Prognostic Challenges. Pathology Case Reviews. 2011;16:146–151. [Google Scholar]
- 9.Sams RN, Gnepp DR. P63 Expression Can Be Used in Differential Diagnosis of Salivary Gland Acinic Cell and Mucoepidermoid Carcinomas. Head Neck Pathol. 2013;7:64–68. doi: 10.1007/s12105-012-0403-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Savera AT, Sloman A, Huvos AG, Klimstra DS. Myoepithelial Carcinoma of the Salivary Glands A Clinicopathologic Study of 25 Patients. Am J Surg Pathol. 2000;24:761–774. doi: 10.1097/00000478-200006000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Lee CH, Liang CW, Espinosa I. The utility of discovered on gastrointestinal stromal tumor 1(DOG1) antibody in surgical pathology-the GIST of it. Adv Anat Pathol. 2010;17:222–232. doi: 10.1097/PAP.0b013e3181d973c2. [DOI] [PubMed] [Google Scholar]
- 12.Yang A, Kaghad M, Wang Y, Gillett E, Fleming MD, Dötsch V, Andrews NC, Caput D, McKeon F. p63, a p53 homolog at 3q27-29, encodes multiple products with transactivating, death- inducing, and dominant-negative activities. Mol Cell. 1998;2:305–16. doi: 10.1016/s1097-2765(00)80275-0. [DOI] [PubMed] [Google Scholar]
- 13.Leivo I. Insights into a complex group of neoplastic disease: Advances in histopathologic classification and molecular pathology of salivary gland cancer. Acta Oncol. 2006;45:662–668. doi: 10.1080/02841860600801316. [DOI] [PubMed] [Google Scholar]
- 14.Ellis GL, Auclair PL. Malignant epithelial tumors. In: Rosai , Sobin LH, editors. Tumors of the salivary glands. Atlas of Tumor Pathology, 3rd series, fascicle 17. Washington, DC: Armed Forces Institute of Pathology; 1995. pp. 163–72. [Google Scholar]
- 15.Crivelini MM, de Sousa SO, de Araujo VC. Immunohistochemical study of acinic cell carcinoma of minor salivary gland. Oral Oncol. 1997;33:204–8. doi: 10.1016/s0964-1955(96)00064-4. [DOI] [PubMed] [Google Scholar]
- 16.West RB, Corless CL, Chen X, Rubin BP, Subramanian S, Montgomery K, Zhu S, Ball CA, Nielsen TO, Patel R, Goldblum JR, Brown PO, Hein rich MC, Van de Rijn M. The novel marker, DOG1, is expressed ubiquitously in gastrointestinal stromal tumors irrespective of KIT or PDGFRA mutation status. Am J Pathol. 2004;165:107–113. doi: 10.1016/S0002-9440(10)63279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergmann F, Andrulis M, Hartwing W, Penzel R, Gaida MM, Herpel E, Schirmacher P, Mechtersheimer G. Discovered on gastrointestinal tumor1 (DOG1) is expressed in pancreatic centroacinar cells and in solid-pseudopapillary neoplasms- novel evidence for a histogenic relationship. Hum Pathol. 2011;42:817–823. doi: 10.1016/j.humpath.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Ousingsawat J, Martins JR, Schreiber R, RocK JR, Harfe BD, Kunzelman K. Loss of TMEM16 A causes a defect in epithelial Ca2+ dependent chloride transport. J Biol Chem. 2009;284:28698–28703. doi: 10.1074/jbc.M109.012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chenevert J, Duvvuri U, Chiosea S, Dacic S, Cieply K, Kim J, Shiwarski D, Seethala RR. DOG1: a novel marker of salivary acinar and intercalated duct differentiation. Mod Pathol. 2012;25:919–929. doi: 10.1038/modpathol.2012.57. [DOI] [PubMed] [Google Scholar]
- 20.Ihrler S, Blasenbreu-Vogt S, Sendelhofert A, Lang S, Zeitz C, Lohrs U. Differential diagnosis of salivary acinic cell carcinoma and adenocarcinoma (NOS). A comparison of immunohistochemical markers. Pathol Res Pract. 2002;198:777–783. doi: 10.1078/0344-0338-00336. [DOI] [PubMed] [Google Scholar]
- 21.Lopes LF, West RB, Bacchi LM, Van de Rijn M, Bacchi CE. DOG1 for the diagnosis of gastrointestinal stromal tumor (GIST): comparison between 2 different antibodies. Appl Immunohistochem Mol Morphol. 2010;18:333–337. doi: 10.1097/PAI.0b013e3181d27ec8. [DOI] [PubMed] [Google Scholar]
- 22.Westfall MD, Pietenpol JA. p63: molecular complexity in development and cancer. Carcinogenesis. 2004;25:857–864. doi: 10.1093/carcin/bgh148. [DOI] [PubMed] [Google Scholar]
- 23.Yang A, Kaghad M, Wang Y, Gillett E, Fleming MD, Dotsch V, Andrews NC. P63, a p53 homolog at 3q27-29, encodes multiple products with transactivating, death-inducing, and dominant-negative activities. Mol Cell. 1998;2:5–16. doi: 10.1016/s1097-2765(00)80275-0. [DOI] [PubMed] [Google Scholar]
- 24.Barbareschi M, Pecciarini L, Cangi MG, Macri E, Rizzo A, Viale G, Doglioni C. p63, a p53 homologue, is a selective nuclear marker of myoepithelial cells of the human breast. Am J Surg Pathol. 2001;25:1054–1060. doi: 10.1097/00000478-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Signoretti S, Waltregny D, Dilks J, Isaac B, Lin D, Garraway L, Yang A. P63 is a prostate basal cell marker and is required for prostate development. Am J Pathol. 2000;157:1769–1775. doi: 10.1016/S0002-9440(10)64814-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellis GL, Auclair PL. Classification. In: Rosai J, Sobin LH, editors. Tumors of the Salivary Glands. Washington, DC: Armed Forces Institute of Pathology; 1996. pp. 27–29. [Google Scholar]
- 27.Dardick I, Gliniecki MR, Heathcote JG, Burford-Mason A. Comparative histogenesis and morphogenesis of mucoepidermoid carcinoma and pleomorphic adenoma. An ultra structural study. Virchows Arch A Pathol Anat Histopathol. 1990;417:405–17. doi: 10.1007/BF01606029. [DOI] [PubMed] [Google Scholar]
- 28.Seethala RR, Livolsi VA, Zhang PJ, Pasha TL, Baloch ZW. Comparison of p63 and p73 expression in benign and malignant salivary gland lesions. Head Neck. 2005;27:696–702. doi: 10.1002/hed.20227. [DOI] [PubMed] [Google Scholar]
- 29.Bilal H, Handra Luca A, Charles BJ, Fouret P. P63 is expressed in basal and myoepithelial cells of human normal and tumor salivary gland tissues. J Histochem Cytochem. 2003;51:133. doi: 10.1177/002215540305100201. [DOI] [PubMed] [Google Scholar]


