Abstract
Preliminary research results with antibody of the negative costimulatory molecule programmed cell death ligand-1 (PD-L1) suggested its expression on tumor cells associated with various tumor grade and postoperative prognosis. However, to date, there is no information of PD-L1 expression in colorectal serrated adenocarcinoma (SAC) and its clinical relevance. Therefore, the purpose of this study is to investigate the clinical significance of PD-L1 expression in a large cohort of patients with SAC. Here, we first retrospectively identified all SAC collected at our institution between August 2008 and May 2013. The expression levels of PD-L1 were examined by immunohistochemistry in 120 patients with SAC. We further evaluated the correlation between expression data and clinical parameters, including patient age, sex, tumor size, location, grade, primary tumor classification (pT), lymph node metastasis (pN), distant metastases (pM), and vascular invasion. Strong PD-L1 expression was detected in 25% of SAC. Higher expression of PD-L1 was significantly associated with pN (P=0.003) and pM (P=0.014). Survival analysis showed that patients with higher expression of PD-L1 had a poorer prognosis (P=0.045). However, multivariate regression analysis did not support PD-L1 as an independent prognostic factor (P=0.430). Our data suggest that PD-L1 may represent a new biomarker of metastasis and prognosis for patients with SAC, but as a target in the treatment of SAC is less certain.
Keywords: Serrated adenocarcinoma, PD-L1, immunotherapy, tumor prognosis
Introduction
Colorectal cancer (CRC) is one of the most common cancer in men and women worldwide [1]. In the United States, it is the second leading cause of cancer mortality, exceeded only lung cancer [2]. At present, we understand that CRC is a highly heterogeneous disease characterized by the biological diversity [3]. That means CRC develops as a result of the successive accumulation of multiple molecular factors such as mutation in K-RAS genes and MSI status [4]. It seems that molecular variability leads to more complicated mechanism of CRC. On the other hand, some key molecular alterations can be used as biomarker to predict prognosis, and even therapeutic target [5]. For example, anti-EGFR monoclonal antibodies is used to treat the patients with metastatic CRC [6]. Therefore, the massive molecules are investigated as factors associated with poor prognosis in CRC.
It was recently reported that programmed cell death 1 ligand 1 (PD-L1) are exploited by tumors to evade immune attack. PD-L1, also known as CD274 and B7-H1, is one of B7 family members and broadly expressed on activated T cells, B cells, macrophages, dendritic cells (DC), and some nonimmune cells including human tumors. Programmed cell death 1 (PD1), the receptor for PD-L1, is a member of the CD28 family and highly expressed on T cells when they become activated [7]. In addition, PD1 can also be induced on activated B cells and NK (natural killer) cells [8,9]. In many different human tumors, PD1 is broadly distributed on tumor infiltrating lymphocytes (TILs) [10,11]. Simultaneously, PD-L1 is commonly induced by inflammatory cytokines (such as IFN-γ) and expressed on the tumor cell surface. Then, PD-L1 binds to PD1 that is expressed on TILs. Finally, the molecular interaction between PD-L1 and PD1 maybe inhibit T cell activation [12-15]. Such combination appears as a possible immune resistance mechanism within the tumor microenvironment [13,16]. Thus, PD-L1 is studied as a potent target for T-cell inhibitory mechanisms in many cancers. Recently, a series of articles reported that PD-L1 is expressed in several human cancers, and the expression was associated with poor prognosis in kidney, gastric, breast, ovarian, and esophageal carcinomas [17-21]. Currently, the function of PD-L1 in CRC remains largely unknown and only a few recent reports have showed that PD-L1 may be correlated with prognosis in patients with CRC. Song et al. [22] examined the expression of PD-L1 on CRC by immunohistochemistry (IHC) and assessed the correlation of PD-L1 expression with clinical parameters including overall survival rate (OS). Then the univariate analysis suggested that patients with high PD-L1 expression had a poor OS.
Colorectal serrated adenocarcinoma (SAC) is determined as a new subtype of CRC by the latest WHO classification of tumors of the digestive system and characterized histologically by epithelial serrations, clear or eosinophilic cytoplasm, abundant cytoplasm, and so on [23,24]. Compared with conventional CRC (cCRC), SAC possess unique molecular features including B-RAF mutation, CpG island methylation phenotype (CIMP), and microsatellite instability (MSI). Moreover, SAC has a worse prognosis than cCRC according to the report of Jose et al. [25]. However, no data are available on the expression of PD-L1 in SAC. Therefore, we investigated the PD-L1 expression in SAC and analyzed the possible clinical significance.
Materials and methods
Patients and samples
In present study, a total of 1367 tumor colorectal tissue samples were obtained from the Department of Pathology of the Shanghai Tongji Hospital Affiliated to Tongji University School of Medicine (Shanghai, China). All 1367 patients had been diagnosed with CRC and underwent initial surgical resection between August 2008 and May 2013. These CRC specimens were reviewed to screen for SAC by two expert gastrointestinal pathologists. SAC were diagnosed by using the criteria proposed by Makinen [24].
The demographic and clinicopathological data of all SAC were collected, including patient age, sex, tumor size, location, grade, primary tumor classification (pT), lymph node metastasis (pN), distant metastases (pM), vascular invasion, and survival time by searching in the medical records and telephone follow-ups. This study was conducted with the approval of the Ethics Committee at Tongji Hospital, Tongji University School of Medicine, Shanghai.
Immunohistochemistry
Standard immunohistochemical staining was performed using monoclonal antibodies specific for human PD-L1 (Abcam, Cambridge, UK). Briefly, formalin-fixed, paraffin-embedded samples of SAC were cut into 5-μm sections and adhered to the silanized glass slides. The tissue sections were deparaffinized in xylene and dehydrated through graded alcohols (100%, 95%, 75%). For antigen retrieval, the slides were boiled in tris-EDTA (pH 9.0) by microwaves. Then the sections were treated with 3% H2O2 for 15 min to block endogenous peroxidase activity and rabbit serum to reduce nonspecific binding. Subsequently, the sections were incubated with PD-L1 monoclonal antibody (diluted 1:100) overnight at 4°C. Then they were washed and incubated with peroxidase-linked goat anti-rabbit secondary antibody (DakoCytomation, Glostrup, Denmark) for PD-L1 staining. Lastly, the slides were immersed in 3, 3’-diaminobenzidine (DAB) for signal generation and counterstained with hematoxylin.
To evaluate evaluation the correlation between PD-L1 expression and clinicopathological features, two independent pathologists without prior information of patient outcome examined the immunohistochemical slides on the basis of criteria published by previous reports [21,26]. Briefly, diffuse cytoplasmic staining in epithelial tumor cells was considered positive . Quantification of the stained area was made as follows: 1 ≤ 33% of the tumor cells, 2 = between 33% and 66% of the tumor cells, 3 < 66% of the tumor cells. The staining intensity was stated as: 1 = absent or weak, 2 = moderate, 3 = strong. Whereas staining grade for PD-L1 were calculated according to the multiplication of the area and intensity scores. Staining with final scores of less than 4 was the low-expression group.
Statistical analyses
Statistical analyses were performed by using SPSS 17.0 (SPSS Inc, Chicago, IL). The associations between PD-L1 expression (high or low) and clinicopathologic parameters were done by χ2 test (N < 5) or Fisher’s exact test (N ≤ 5). Two sided p values were calculated and P < 0.05 was considered significant. OS was analyzed by the log rank test, and Kaplan-Meier curves were generated. The Cox-regression analysis, both univariate and multivariate, were used to identify the independency of PD-L1 expression status. Both hazards ratios (HR) and 95% confidence intervals (CI) were displayed for the prognostic effect of PD-L1 expression on survival time. P < 0.05 was considered to be statistically significant.
Results
Clinical profiles of the patients
Among 1367 tissue samples of CRC, 120 cases were classified as SAC on the basis of criteria proposed by prior established criteria [24]. Figure 1A shows the photomicrograph of SAC. Briefly, SAC are characterized by epithelial serrations, clear or eosinophilic and abundant cytoplasm, the nuclei are vesicular and basal, and mucinous differentiation. In addition, necrosis is usually absent. In this study, 120 SAC were found from 1367 CRC, and the frequency of SAC is 8.7% of all CRC. Table 1 shows the clinical features of the patients with SAC. Overall, the average age was 67.0±13.0 years, and the patients with older age (≥ 55 years, 97/120, 80.8%) had a tendency of SAC. Moreover, SAC were more likely to be located in distal colon and rectum (79/120, 65.8%). Of 120 SAC, 18 (15.0%), 95 (79.2%), and 7 (5.8%) were diagnosed as grade of high (G1), medium (G2), and low (G3), respectively. Toward the end of the present study, the median follow-up time was 39 months for patients with SAC.
Figure 1.
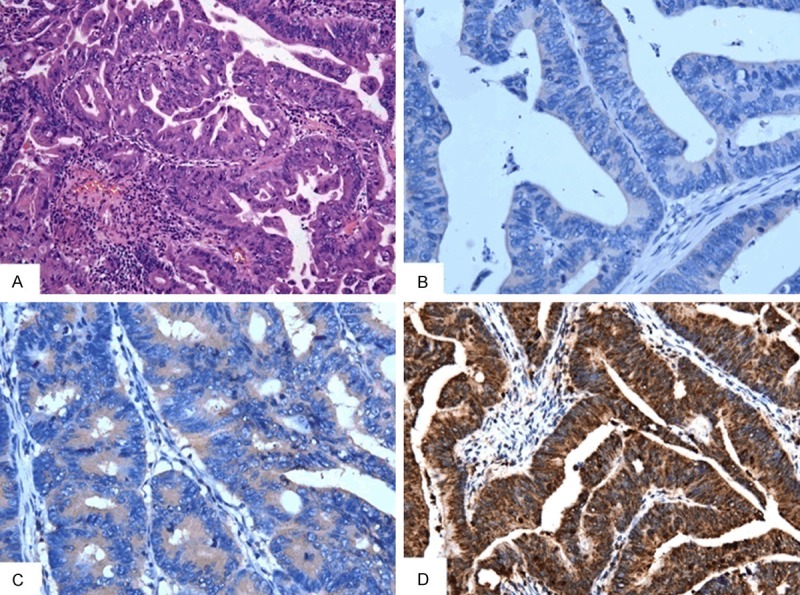
(A) The photomicrograph of colorectal serrated adenocarcinoma (SAC). Moderately differentiated SAC showing tufting serration of the epithelium together with abundant cytoplasm (H&E× 200). (B-D) Immunohistochemical staining of SAC with intensity score 1 (B), score 2 (C), and score 3 (D) expression of PD-L1 are shown (× 200 magnification in all).
Table 1.
Demographic and pathological characteristics of the patients with colorectal serrated adenocarcinoma (n=120)
| Variable | Frequency n (%) | |
|---|---|---|
| Age (years) | < 55 | 23 (19.2) |
| ≥ 55 | 97 (80.8) | |
| Genders | Male | 71 (59.2) |
| Female | 49 (40.8) | |
| Tumor diameter (cm) | < 5 | 66 (55.0) |
| ≥ 5 | 54 (45.0) | |
| Tumor location | Distal/rectum | 79 (65.8) |
| Proximal | 41 (34.2) | |
| Tumor grade | G1 | 18 (15.0) |
| G2 | 95 (79.2) | |
| G3 | 7 (5.8) | |
| Primary tumor classification(pT) | T1 | 6 (5.0) |
| T2 | 11 (9.2) | |
| T3 | 79 (65.8) | |
| T4 | 24 (20.0) | |
| Lymph node metastasis(pN) | N0 | 68 (56.7) |
| N1 | 33 (27.5) | |
| N2 | 19 (15.8) | |
| Distant metastasis | M0 | 101 (84.2) |
| M1 | 19 (15.8) | |
| Vascular invasion | Absent | 100 (83.3) |
| Present | 20 (16.7) | |
| Median follow-up time (months) | SAC | 39 |
Correlation between PD-L1 expression and clinicopathological parameters
Representative examples of PD-L1 staining are shown in Figure 1B-D. PD-L1 was observed in TILs, importantly, in epithelial cells of tumor cells. Among 120 tissue samples, the PD-L1 staining intensity was scored as 1, 2, and 3 in 83 (69.2%), 21 (17.5%), and 16 (13.3%) cases, respectively. In addition, the stained area in cancer cells was scored as 1, 2, and 3 in 76 (63.3%), 21 (17.5%), and 23 (19.2%) cases. Accordingly, the proportion of high expression (final scores ≥ 4) was 25.0% for PD-L1.
Furthermore, we analyzed PD-L1 expression in 120 tumor tissues of SAC and their clinicopathologic characteristics are shown in Table 2. Among the various clinicopathological parameters, pN (P = 0.003) was statistically significant correlation with the higher expression of PD-L1. Importantly, the patients with strong PD-L1 expression were more inclined to pM (P = 0.014). However, PD-L1 expression were not found to be significantly associated with other clinicopathological features such as age, gender, tumor diameter, tumor location, tumor grade, pT, and vascular invasion.
Table 2.
Association between PD-L1 expression level and clinical pathological features in the patients with colorectal serrated adenocarcinoma (n=120)
| PD-L1 expression | ||||
|---|---|---|---|---|
|
|
||||
| Variable | n | Low (%) | High (%) | P value |
| Age (years) | 0.349 | |||
| < 55 | 23 | 19 | 4 (17.4) | |
| ≥ 55 | 97 | 71 | 26 (26.8) | |
| Genders | 0.335 | |||
| Male | 71 | 51 | 20 (28.2) | |
| Female | 49 | 39 | 10(20.4) | |
| Tumor diameter (cm) | 0.832 | |||
| < 5 | 66 | 50 | 16 (24.2) | |
| ≥ 5 | 54 | 40 | 14 (25.9) | |
| Tumor location | 0.096 | |||
| Distal/rectum | 79 | 63 | 16 (20.3) | |
| Proximal | 41 | 27 | 14 (34.1) | |
| Tumor grade | 0.376 | |||
| G1 | 18 | 15 | 3 (16.7) | |
| G2+G3 | 102 | 75 | 27 (26.5) | |
| Primary tumor classification (pT) | 0.174 | |||
| T1+T2 | 17 | 15 | 2 (11.8) | |
| T3+T4 | 103 | 75 | 28 (27.2) | |
| Lymph node metastasis (pN) | 0.003 | |||
| N0 | 68 | 58 | 10 (14.7) | |
| N1+N2 | 52 | 32 | 20 (38.5) | |
| Distant metastases (pM) | 0.014 | |||
| M0 | 101 | 81 | 20 (20.8) | |
| M1 | 19 | 10 | 9 (47.4) | |
| Vascular invasion | 0.258 | |||
| Absent | 100 | 77 | 23 (23.0) | |
| Present | 20 | 13 | 7 (35.0) | |
Prognostic significance of PD-L1 expression
At the end of follow-up, 16 patients had been lost and 35 patients had died of SAC. As already mentioned, the median follow-up time was 39 months for patients with SAC. The survival analysis of Kaplan-Meier showed that the 3-year survival rate of patients with high PD-L1 expression (58.4%) was worse than that with low expression (72.5%). Moreover, the Kaplan-Meier curve and log rank test demonstrated that the high PD-L1 expression in tumor cells were associated with poor OS in SAC (Figure 2, P = 0.045). However, multivariate analysis by the Cox hazard model revealed that PD-L1 was not an independent prognostic factor for OS of the patients with SAC (Table 3, P = 0.430).
Figure 2.
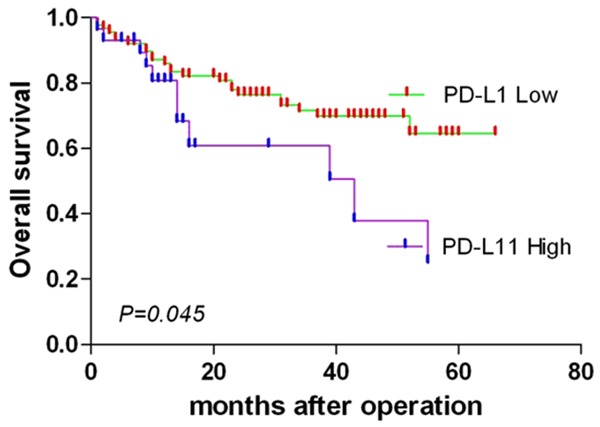
Association of PD-L1 expression with overall survival (OS) in 120 patients with colorectal serrated adenocarcinomas. The OS was significantly lower in PD-L1-higher-expression patients compared with PD-L1-lower-expression patients (P = 0.045).
Table 3.
Univariate and multivariate Cox-regression analysis showing factors including PD-L1 expression on the cancer-specific death of the patients with colorectal serrated adenocarcinoma (n=120)
| Variable | n | Overall survival, Univariate risk ratio | P value | Overall survival, Multivariate risk ratio | P value |
|---|---|---|---|---|---|
| PD-L1 | 0.021 | 0.430 | |||
| Low | 92 | 1 | 1 | ||
| High | 28 | 2.304 (1.133-4.684) | 0.692 (0.277-1.729) | ||
| Age (years) | 0.119 | 0.282 | |||
| < 55 | 23 | 1 | 1 | ||
| ≥ 55 | 97 | 2.567 (0.786-8.387) | 2.011 (0.564-7.175) | ||
| Genders | 0.708 | 0.680 | |||
| Male | 71 | 1 | 1 | ||
| Female | 49 | 1.139 (0.577-2.247) | 1.180 (0.537-2.594) | ||
| Tumor diameter (cm) | 0.254 | 0.492 | |||
| < 5 | 66 | 1 | 1 | ||
| ≥ 5 | 54 | 1.471 (0.757-2.858) | 0.764 (0.354-1.648) | ||
| Tumor location | 0.001 | 0.157 | |||
| Distal/rectum | 79 | 1 | 1 | ||
| Proximal | 29 | 3.086 (1.573-6.052) | 1.825 (0.793-4.197) | ||
| Tumor grade | 0.114 | 0.251 | |||
| G1 | 18 | 1 | 1 | ||
| G2+G3 | 102 | 2.606 (0.795-8.544) | 2.152 (0.581-7.968) | ||
| Primary tumor classification (pT) | 0.103 | 0.698 | |||
| T1+T2 | 17 | 1 | 1 | ||
| T3+T4 | 103 | 3.280 (0.786-13.684) | 1.352 (0 .295-6.205) | ||
| Lymph node metastasis (pN) | 0.006 | 0.178 | |||
| N0 | 68 | 1 | 1 | ||
| N1+N2 | 52 | 2.578 (1.305-5.092) | 1.725 (0.780-3.814) | ||
| Distant metastasis (pM) | < 0.001 | < 0.001 | |||
| M0 | 101 | 1 | 1 | ||
| M1 | 19 | 6.408 (3.268-12.565) | 4.863 (2.053-11.521) | ||
| Vascular invasion | 0.493 | 0.406 | |||
| Absent | 100 | 1 | |||
| Present | 20 | 1.337 (0.583-3.064) | 1.449 (0.604-3.479) |
Discussion
In 1992, Jass et al. [27] found that five colorectal cancers with serrated features resembled the hyperplastic polyp both morphologically and histochemically, then SAC first were described. Subsequently, histological criteria for diagnosis of SAC have been finally proposed by Makinen et al. [28]. Furthermore, Laiho et al. [29] examined the unique molecular characteristics distinguishing SAC from cCRC by unsupervised hierarchical clustering and IHC. In results, ephrin receptor B2 (EPHB2), hypoxia-inducible factor 1-alpha (HIF1-α) and patched (PTCH) were identified as proteins important for genesis of SAC. In addition, some biological behave, including loss of hMLH1 and MGMT, CIMP, MSI, and B-RAF mutation, have also been approved to play an important role in hyperplastic polyp-serrated adenoma-carcinoma (“serrated”) pathway of tumorigenesis [30,31]. Recently, SAC is determined as a new subtype of CRC by the latest WHO classification of tumors of the digestive system [23]. On the basis of different estimates, the incidence of SAC are highly variable and the frequency ranges from 1.5%-12% by morphologic investigations [31,32], or 10%-20% by molecular features [33]. Moreover, SAC has been verified to have a poorer prognosis than cCRC [25]. Based on the above reporters, it suggests that SAC may need to develop more specific therapeutic modalities and follow-up. The costimulatory molecule PD-L1 is well known as a potential target of antitumor immunity in many human cancers [17-21]. To date, little is known about the expression of PD-L1 in SAC. The aim of present study was to investigate the expression of PD-L1 in a cohort of SAC samples and to estimate its clinical significant.
Here we showed that the cell cytoplasm and membrane of SAC tumor cells do express abundant PD-L1. Strong PD-L1 was expressed on 25.0% SAC. Expectedly, high PD-L1 expression in SAC was significantly associated with pN and pM. Although the multivariate analysis did not support PD-L1 as an independent prognostic factor, the Kaplan-Meier curve and log rank test demonstrated that the patients with high PD-L1 expression had a poor overall survival after enterectomy. Therefore, our results suggest that PD-L1 play an adverse role in the progression of SAC. Simultaneously, our data is also consistent with reports on PD-L1 in other human tumors. In the study on renal cell carcinoma by Thompson et al. [17], patients with high PD-L level were more likely to have poor prognosis. In gastric carcinoma, PD-L1 expression was significantly associated with tumor size, invasion, pN, and survival time of patients [18]. Resembled results were also found in ovarian cancer, and the expression of PD-L1 on tumor cells were considered as an independent prognostic factors [20]. In addition, the patients with pancreatic cancer and positive PD-L1 had a poorer prognosis than negative, and the PD-L1 monoclonal antibody generated significantly therapeutic efficacy on murine pancreatic cancer in vivo [34].
As stated above, the most important finding is that PD-L1 is a significant independent prognostic factor in variable human tumors. To date, the underlying mechanism has not been determined. Base on previous report, the limited activation of tumor-reactive T cells by PD-L1 may be a critical mechanism [7,14,35-39]. Briefly, PD-L1 is expressed on the tumor cell surface and frequently induced by inflammatory cytokines (such as IFN-γ). Subsequently, the combination of PD-L1 and PD1 expressed on TILs maybe limit the activity of T cells, and antitumour immune within the tumor microenvironment is finally inhibited. Notably, this mechanism showed that the induction of PD-L1 expression was primary. However, some recent studies suggested that PD-L1 expression was regulated by different pathways in different types of tumors [22,40]. For instance, PD-L1 expression may be partly regulated by PTEN and not be affected by IFN-γ in CRC [22].
Although our data clearly indicated that the high PD-L1 expression were associated with severe prognosis in SAC, multivariate analysis did not supported PD-L1 as a strong prognostic factor. This result was similar to the previous report on CRC by Song et al. [22]. Based on previous and present results, there may be some possible explanations for this negative data. First, it is well known that there are a lot of microbes in the human gut. The research by Wesemann et al. [41] showed that these commensal microbes within the gut not only regulate the activity of T cell, but also influence the early B cell development. Based on this pattern, the intestinal immune system is modulated by the intestinal microbiome. When the diversity of intestinal microbiota is altered by some abnormal status (such as antibiotic exposure, obesity, and intestinal inflammation), the immunologic function would generate shift accordingly [42-44]. So the intestinal dysfunction as a consequence of CRC may modify the intestinal immune system [45], which is possibly one explanation for the negative data by multivariate analysis. Second, PD-L1, as a possible candidate checkpoint for T-cell inhibitory mechanism in tumor cell, is commonly induced by IFN-γ and Toll-like receptor (TLR) via a MEK/ERK-dependent and MyD88/TRAF6-dependent pathway [40]. As mentioned, PD-L1 expression was regulated by different pathways in different types of tumors [22,40]. Unlike many other tumors, PD-L1 expression is independently associated with the PTEN loss in CRC [22]. It may cause that low PD-L1 expression does not appear to improve survival of the patients with SAC.
In this study, there are several limitations. At present, there is no the consistent criteria for SAC diagnosis. Therefore, it cannot avoid selection inaccurate. Although we strictly diagnose SAC based on prior established criteria [24] and try our best to minimize diagnostic error. Notably, our CRC originally were 1367 in total. But only 120 SAC cases were collected for this investigation after multiple rounds of selection. It is another limitation in this study.
Taken together, the most important results in present study contribute to the correlation between PD-L1 expression and clinical parameters in SAC. Finally, current findings indicate that strong PD-L1 expression can promote SAC metastasis and mortality, suggesting that PD-L1 may represent a new biomarker of metastasis and prognosis for patients with SAC. However, PD-L1 as a target in the treatment of SAC is less certain due to the negative results of multivariate analysis. Therefore, further study is warranted to clarify immune escape mechanisms via PD-L1/TILs in SAC.
Acknowledgements
This work was supported in part by the Science and Technology Commission foundation of the National Natural Sxience Foundation of China (81570053) to Xianghua Yi, Key Medical Research of Shanghai (034119868, 09411951600) to Xianghua Yi, Key Medical Research Foundation of Health Bureau of Shanghai (20134034) to Xianghua Yi. The authors thank Weizhe Qiu and Long Zhang for their expert technical support.
Disclosure of conflict of interest
None.
References
- 1.Deschoolmeester V, Baay M, Specenier P, Lardon F, Vermorken JB. A review of the most promising biomarkers in colorectal cancer: one step closer to targeted therapy. Oncologist. 2010;15:699–731. doi: 10.1634/theoncologist.2010-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 3.Minoo P, Zlobec I, Peterson M, Terracciano L, Lugli A. Characterization of rectal, proximal and distal colon cancers based on clinicopathological, molecular and protein profiles. Int J Oncol. 2010;37:707–718. doi: 10.3892/ijo_00000720. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Arnold CN, Niedzwiecki D, Chang DK, Ricciardiello L, Carethers JM, Dowell JM, Wasserman L, Compton C, Mayer RJ, Bertagnolli MM, Boland CR. Characterization of sporadic colon cancer by patterns of genomic instability. Cancer Res. 2003;63:1608–1614. [PubMed] [Google Scholar]
- 5.Lao VV, Grady WM. Epigenetics and colorectal cancer. Nat Rev Gastroenterol Hepatol. 2011;8:686–700. doi: 10.1038/nrgastro.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pritchard CC, Grady WM. Colorectal cancer molecular biology moves into clinical practice. Gut. 2011;60:116–129. doi: 10.1136/gut.2009.206250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ishida Y, Agata Y, Shibahara K, Honjo T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. Embo J. 1992;11:3887–3895. doi: 10.1002/j.1460-2075.1992.tb05481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terme M, Ullrich E, Aymeric L, Meinhardt K, Desbois M, Delahaye N, Viaud S, Ryffel B, Yagita H, Kaplanski G, Prevost-Blondel A, Kato M, Schultze JL, Tartour E, Kroemer G, Chaput N, Zitvogel L. IL-18 induces PD-1-dependent immunosuppression in cancer. Cancer Res. 2011;71:5393–5399. doi: 10.1158/0008-5472.CAN-11-0993. [DOI] [PubMed] [Google Scholar]
- 9.Fanoni D, Tavecchio S, Recalcati S, Balice Y, Venegoni L, Fiorani R, Crosti C, Berti E. New monoclonal antibodies against B-cell antigens: possible new strategies for diagnosis of primary cutaneous B-cell lymphomas. Immunol Lett. 2011;134:157–160. doi: 10.1016/j.imlet.2010.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Sfanos KS, Bruno TC, Meeker AK, De Marzo AM, Isaacs WB, Drake CG. Human prostate-infiltrating CD8+ T lymphocytes are oligoclonal and PD-1+ Prostate. 2009;69:1694–1703. doi: 10.1002/pros.21020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmadzadeh M, Johnson LA, Heemskerk B, Wunderlich JR, Dudley ME, White DE, Rosenberg SA. Tumor antigen-specific CD8 T cells infiltrating the tumor express high levels of PD-1 and are functionally impaired. Blood. 2009;114:1537–1544. doi: 10.1182/blood-2008-12-195792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 13.Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, Roche PC, Lu J, Zhu G, Tamada K, Lennon VA, Celis E, Chen L. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 14.Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, Fitz LJ, Malenkovich N, Okazaki T, Byrne MC, Horton HF, Fouser L, Carter L, Ling V, Bowman MR, Carreno BM, Collins M, Wood CR, Honjo T. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carter L, Fouser LA, Jussif J, Fitz L, Deng B, Wood CR, Collins M, Honjo T, Freeman GJ, Carreno BM. PD-1:PD-L inhibitory pathway affects both CD4(+) and CD8(+) T cells and is overcome by IL-2. Eur J Immunol. 2002;32:634–643. doi: 10.1002/1521-4141(200203)32:3<634::AID-IMMU634>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 16.Blank C, Brown I, Peterson AC, Spiotto M, Iwai Y, Honjo T, Gajewski TF. PD-L1/B7H-1 inhibits the effector phase of tumor rejection by T cell receptor (TCR) transgenic CD8+ T cells. Cancer Res. 2004;64:1140–1145. doi: 10.1158/0008-5472.can-03-3259. [DOI] [PubMed] [Google Scholar]
- 17.Thompson RH, Gillett MD, Cheville JC, Lohse CM, Dong H, Webster WS, Krejci KG, Lobo JR, Sengupta S, Chen L, Zincke H, Blute ML, Strome SE, Leibovich BC, Kwon ED. Costimulatory B7-H1 in renal cell carcinoma patients: Indicator of tumor aggressiveness and potential therapeutic target. Proc Natl Acad Sci U S A. 2004;101:17174–17179. doi: 10.1073/pnas.0406351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu C, Zhu Y, Jiang J, Zhao J, Zhang XG, Xu N. Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in gastric carcinoma and its clinical significance. Acta Histochem. 2006;108:19–24. doi: 10.1016/j.acthis.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Haghshenas MR, Naeimi S, Talei A, Ghaderi A, Erfani N. Program death 1 (PD1) haplotyping in patients with breast carcinoma. Mol Biol Rep. 2011;38:4205–4210. doi: 10.1007/s11033-010-0542-z. [DOI] [PubMed] [Google Scholar]
- 20.Hamanishi J, Mandai M, Iwasaki M, Okazaki T, Tanaka Y, Yamaguchi K, Higuchi T, Yagi H, Takakura K, Minato N, Honjo T, Fujii S. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci U S A. 2007;104:3360–3365. doi: 10.1073/pnas.0611533104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loos M, Langer R, Schuster T, Gertler R, Walch A, Rauser S, Friess H, Feith M. Clinical significance of the costimulatory molecule B7-H1 in Barrett carcinoma. Ann Thorac Surg. 2011;91:1025–1031. doi: 10.1016/j.athoracsur.2010.12.041. [DOI] [PubMed] [Google Scholar]
- 22.Song M, Chen D, Lu B, Wang C, Zhang J, Huang L, Wang X, Timmons CL, Hu J, Liu B, Wu X, Wang L, Wang J, Liu H. PTEN loss increases PD-L1 protein expression and affects the correlation between PD-L1 expression and clinical parameters in colorectal cancer. PLoS One. 2013;8:e65821. doi: 10.1371/journal.pone.0065821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li ZS, Li Q. [The latest 2010 WHO classification of tumors of digestive system] . Zhonghua Bing Li Xue Za Zhi. 2011;40:351–354. [PubMed] [Google Scholar]
- 24.Makinen MJ. Colorectal serrated adenocarcinoma. Histopathology. 2007;50:131–150. doi: 10.1111/j.1365-2559.2006.02548.x. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-Solano J, Perez-Guillermo M, Conesa-Zamora P, Acosta-Ortega J, Trujillo-Santos J, Cerezuela-Fuentes P, Makinen MJ. Clinicopathologic study of 85 colorectal serrated adenocarcinomas: further insights into the full recognition of a new subset of colorectal carcinoma. Hum Pathol. 2010;41:1359–1368. doi: 10.1016/j.humpath.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Erkan M, Kleeff J, Esposito I, Giese T, Ketterer K, Buchler MW, Giese NA, Friess H. Loss of BNIP3 expression is a late event in pancreatic cancer contributing to chemoresistance and worsened prognosis. Oncogene. 2005;24:4421–4432. doi: 10.1038/sj.onc.1208642. [DOI] [PubMed] [Google Scholar]
- 27.Jass JR, Smith M. Sialic acid and epithelial differentiation in colorectal polyps and cancer--a morphological, mucin and lectin histochemical study. Pathology. 1992;24:233–242. doi: 10.3109/00313029209068874. [DOI] [PubMed] [Google Scholar]
- 28.Makinen MJ, George SM, Jernvall P, Makela J, Vihko P, Karttunen TJ. Colorectal carcinoma associated with serrated adenoma--prevalence, histological features, and prognosis. J Pathol. 2001;193:286–294. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH800>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 29.Laiho P, Kokko A, Vanharanta S, Salovaara R, Sammalkorpi H, Jarvinen H, Mecklin JP, Karttunen TJ, Tuppurainen K, Davalos V, Schwartz S Jr, Arango D, Makinen MJ, Aaltonen LA. Serrated carcinomas form a subclass of colorectal cancer with distinct molecular basis. Oncogene. 2007;26:312–320. doi: 10.1038/sj.onc.1209778. [DOI] [PubMed] [Google Scholar]
- 30.Oh K, Redston M, Odze RD. Support for hMLH1 and MGMT silencing as a mechanism of tumorigenesis in the hyperplastic-adenoma-carcinoma (serrated) carcinogenic pathway in the colon. Hum Pathol. 2005;36:101–111. doi: 10.1016/j.humpath.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 31.O'Brien MJ, Yang S, Mack C, Xu H, Huang CS, Mulcahy E, Amorosino M, Farraye FA. Comparison of microsatellite instability, CpG island methylation phenotype, BRAF and KRAS status in serrated polyps and traditional adenomas indicates separate pathways to distinct colorectal carcinoma end points. Am J Surg Pathol. 2006;30:1491–1501. doi: 10.1097/01.pas.0000213313.36306.85. [DOI] [PubMed] [Google Scholar]
- 32.Tuppurainen K, Makinen JM, Junttila O, Liakka A, Kyllonen AP, Tuominen H, Karttunen TJ, Makinen MJ. Morphology and microsatellite instability in sporadic serrated and non-serrated colorectal cancer. J Pathol. 2005;207:285–294. doi: 10.1002/path.1850. [DOI] [PubMed] [Google Scholar]
- 33.O’Brien MJ, Yang S, Huang CS, Shepherd C, Cerda S, Farraye FA. The serrated polyp pathway to colorectal carcinoma. Diagnostic Histopathology. 2008;14:78–93. [Google Scholar]
- 34.Nomi T, Sho M, Akahori T, Hamada K, Kubo A, Kanehiro H, Nakamura S, Enomoto K, Yagita H, Azuma M, Nakajima Y. Clinical significance and therapeutic potential of the programmed death-1 ligand/programmed death-1 pathway in human pancreatic cancer. Clin Cancer Res. 2007;13:2151–2157. doi: 10.1158/1078-0432.CCR-06-2746. [DOI] [PubMed] [Google Scholar]
- 35.Keir ME, Liang SC, Guleria I, Latchman YE, Qipo A, Albacker LA, Koulmanda M, Freeman GJ, Sayegh MH, Sharpe AH. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203:883–895. doi: 10.1084/jem.20051776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nishimura H, Okazaki T, Tanaka Y, Nakatani K, Hara M, Matsumori A, Sasayama S, Mizoguchi A, Hiai H, Minato N, Honjo T. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science. 2001;291:319–322. doi: 10.1126/science.291.5502.319. [DOI] [PubMed] [Google Scholar]
- 37.Nishimura H, Nose M, Hiai H, Minato N, Honjo T. Development of lupus-like autoimmune diseases by disruption of the PD-1 gene encoding an ITIM motif-carrying immunoreceptor. Immunity. 1999;11:141–151. doi: 10.1016/s1074-7613(00)80089-8. [DOI] [PubMed] [Google Scholar]
- 38.Okazaki T, Honjo T. PD-1 and PD-1 ligands: from discovery to clinical application. Int Immunol. 2007;19:813–824. doi: 10.1093/intimm/dxm057. [DOI] [PubMed] [Google Scholar]
- 39.Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2008;26:677–704. doi: 10.1146/annurev.immunol.26.021607.090331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu J, Hamrouni A, Wolowiec D, Coiteux V, Kuliczkowski K, Hetuin D, Saudemont A, Quesnel B. Plasma cells from multiple myeloma patients express B7-H1 (PD-L1) and increase expression after stimulation with IFN-{gamma} and TLR ligands via a MyD88-, TRAF6-, and MEK-dependent pathway. Blood. 2007;110:296–304. doi: 10.1182/blood-2006-10-051482. [DOI] [PubMed] [Google Scholar]
- 41.Wesemann DR, Portuguese AJ, Meyers RM, Gallagher MP, Cluff-Jones K, Magee JM, Panchakshari RA, Rodig SJ, Kepler TB, Alt FW. Microbial colonization influences early B-lineage development in the gut lamina propria. Nature. 2013;501:112–115. doi: 10.1038/nature12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deshmukh HS, Liu Y, Menkiti OR, Mei J, Dai N, O'Leary CE, Oliver PM, Kolls JK, Weiser JN, Worthen GS. The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nat Med. 2014;20:524–530. doi: 10.1038/nm.3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwiertz A, Gruhl B, Lobnitz M, Michel P, Radke M, Blaut M. Development of the intestinal bacterial composition in hospitalized preterm infants in comparison with breast-fed, full-term infants. Pediatr Res. 2003;54:393–399. doi: 10.1203/01.PDR.0000078274.74607.7A. [DOI] [PubMed] [Google Scholar]
- 44.Pflughoeft KJ, Versalovic J. Human microbiome in health and disease. Annu Rev Pathol. 2012;7:99–122. doi: 10.1146/annurev-pathol-011811-132421. [DOI] [PubMed] [Google Scholar]
- 45.Droeser RA, Hirt C, Viehl CT, Frey DM, Nebiker C, Huber X, Zlobec I, Eppenberger-Castori S, Tzankov A, Rosso R, Zuber M, Muraro MG, Amicarella F, Cremonesi E, Heberer M, Iezzi G, Lugli A, Terracciano L, Sconocchia G, Oertli D, Spagnoli GC, Tornillo L. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur J Cancer. 2013;49:2233–2242. doi: 10.1016/j.ejca.2013.02.015. [DOI] [PubMed] [Google Scholar]


