Abstract
Homelessness affects a large and increasing number of families in the United States, and exposure to violence and other potentially traumatic events is common among homeless families. It is important to understand more about this population and, more specifically, about the relationship between youth mental health and caregiver mental health and trauma exposure among homeless families, in order to better serve the needs of this vulnerable population. The objective of this study is to explore the relationships between caregiver exposure to violence, caregiver depression, and youth depression and behavioral problems among homeless families. Preliminary findings indicate that among this sample of homeless families, caregiver violence exposure has statistically significant relationships with both youth behavioral problems and youth depression symptoms, as mediated by caregiver depression. These findings indicate that youth behavioral health is associated with caregiver mental health, which, in turn, is associated with caregiver trauma exposure. This highlights the importance of taking into account adult mental health while treating youth externalizing and internalizing behaviors and ensuring that caregivers, too, have access to adequate treatment and supports. Furthermore, this treatment should be trauma informed, given the link between trauma and mental health.
Keywords: homeless families, homeless youth, youth mental health, caregiver trauma exposure, caregiver depression, youth depression, youth behavioral problems
Homelessness affects a large number of families in the United States. According to the U.S. Department of Housing and Urban Development (HUD, 2011), on a given night in January 2010, there were a total of 79,446 homeless families in the nation, encompassing 241,951 family members. Of these individuals, 79.1% were in shelters, comprising 29.4% of the overall population in shelters. Moreover, of the sheltered persons in families, 59.3% are children, 31.7% are adult women, and 9.0% are adult men. Of the individuals in homeless families, 20.9% were unsheltered, sleeping in public places, abandoned buildings, or other unconventional locations. These unsheltered homeless families represent 7.8% of the overall unsheltered homeless population. And the numbers of homeless families are rising. Between 2009 and 2010, the total number of homeless persons in families grew by 1.6%, increasing to 241,951 from 238,110. In fact, according to HUD (2011), “the proportion of people who used shelters as part of a family rose in every year from 2007 to 2010. In 2010, 30 percent of homeless persons were served as part of a family; by 2010 35 percent of homeless persons were members of families” (p. 42). Furthermore, there is reason to believe that the number of families and children who experience homelessness over the course of the year is far higher. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2011), the National Center on Family Homelessness analyzed data from each of the states in 2009 and found that 1.5 million children across the country experience homelessness in a year.
Trauma and Mental Health Among Vulnerable Populations
Women who are homeless encounter more danger than those in the general population. Many homeless women have experienced violence and abuse as children and adults (Bassuk et al., 1996). They are more likely to be exposed to physical violence or sexual assault than those who are not homeless. They also face higher rates of victimization than those who are in low-income or marginal housing (Kushel, Evans, Perry, Robertson, & Moss, 2003; Wenzel, Leake, & Gelberg, 2001). Exposure to violence puts these women at greater risk of developing posttraumatic stress disorder (PTSD; Breslau, 2009). Individuals who are exposed to trauma are also at greater risk of depression (Breslau, Davis, Peterson, & Schultz, 2000).
Women exposed to physical violence are more likely to become clinically depressed than those who were not. While living in a shelter may mitigate the ongoing rate of exposure to violence among homeless women, the factors that lead to their homelessness may contribute to their depressive symptoms (Rayburn et al., 2005). Although most research is geared toward women (Huey, Fthenos, & Hryniewicz, 2013; Rayburn et al., 2005; Wenzel, Tucker, Elliott, Marshall, & Williamson, 2004), both homeless men and women face the ongoing risk of victimization (Padgett & Struening, 1992). Both genders also face the association of homelessness with depression (Gory, Ritchey, & Mullins, 1990). In general, economic stressors and genetic factors may lead to parental depression (Davidson & Neale, 1998; Samuels, Shinn, & Buckner, 2010). African American women from socioeconomically disadvantaged communities, for instance, are at an even greater risk of depression than their higher income counterparts (Cutrona et al., 2005).
Rates of depression, PTSD, and substance use are higher in homeless mothers than among mothers with housing (Bassuk, Buckner, Perloff, & Bassuk, 1998; Conrad, 1998; Meadows-Oliver, 2003; Rog, McCombs-Thornton, Gilbert-Mongelli, Brito, & Holupka, 1995). Many homeless children, too, have experienced a great deal of trauma, and many of them experience behavioral health symptoms. According to the National Center on Family Homelessness (2008), 83% of homeless children have been exposed to at least one episode of violence by age 12. Homeless children also experience behavioral health symptoms at rates far higher than in the general population. As compared to 18% of housed children, half of homeless school-age children experience symptoms of depression, withdrawal, or anxiety (National Child Traumatic Stress Network Homelessness and Extreme Poverty Working Group, 2005).
Indeed, violence, abuse, and other types of trauma have significant effects on the well-being and psychological health of those who experience them. A study of adolescents in public high schools found that exposure to violence as victims or witnesses was positively correlated with psychological trauma, including anxiety, depression, stress, anger, and dissociation. There were particularly high rates of symptoms of overall psychological trauma among youth affected by home violence, sexual abuse/assault, and previous experiences of being threatened, hit, beaten, or mugged (Singer, Anglin, Song, & Lunghofer, 1995). Exposure to violence has also been found to be positively correlated with depression, anxiety, and behavioral problems among a sample of homeless and low-income housed children between the ages of 8 and 17 (Buckner, Beardslee, & Bassuk, 2004). Burke, Hellman, Scott, Weems, and Carrion (2011), further, found that children in a low-income, urban community who were exposed to four or more adverse childhood experiences such as neglect and abuse were at increased risk of learning problems and behavior problems.
There are also connections between parent and child experiences of trauma, attachment and relationships between parents and children, and child outcomes. Children and their parents may react to environmental stressors as well as to one another's reactions (Hammen, Burge, & Adrian, 1991). Perpetual exposure to the stress and maternal health impairments associated with homelessness can likely interfere with a child's ability to develop coping abilities. Gewirtz and Edleson (2007) note that there are lower rates of secure attachment among children from high-risk groups (those exposed to more than one risk factor, such as abuse, violence, and poverty). Beyond this, insecure attachment is correlated with the risk of later emotional and behavioral problems, while secure attachment is associated with the child's development of internal regulation. Indeed, Holt, Buckley, and Whelan (2008) indicate that “a secure attachment to a non-violent parent or other significant carer has been cited consistently in the literature as an important protective factor in mitigating trauma and distress” (p. 806). Financial distress and exposure to violence against family members, however, are both likely to increase aggressive behaviors in youth (Anooshian, 2005). In fact, homeless children often witness acts of violence against their mothers (Anooshian, 2005). Children who reside in dangerous communities and witness violent acts, moreover, may have more positive attitudes about aggression than children living in safer neighborhoods (Colder, Mott, Levy, & Flay, 2000).
Relationships Between Caregiver Depression and Youth Externalizing and Internalizing Symptoms
Homeless parents with mental health diagnoses have poorer interactions with their children than undiagnosed low-income caregivers (Howard, Cartwright, & Barajas, 2009), and mental illness may compromise a caregiver's ability to protect their child from dangers associated with homelessness (Coverdale & Turbott, 2000; Gearon & Bellack, 1999).
Caregiver depression, in particular, can have adverse effects on children. There is significant evidence that maternal depression can negatively impact children (Mowbray, Bybee, Oyserman, Mcfarlane, & Bowersox, 2006; Oyserman, Bybee, & Mowbray, 2002). Mothers who are experiencing depression may be less responsive to their children, with tendencies toward inconsistency, disorganization, and interactions in which they are negative, anxious, and critical (Mowbray et al., 2006). Symptoms of withdrawal, hopelessness, and guilt may further contribute to parenting difficulties (Oyserman et al., 2002).
Caregiver depression has been found to be associated with youth behavioral problems and depressive symptoms through a number of studies. Gopalan, Dean-Assael, Klingstein, Chacko, and McKay (2011) found that 56.6% of 212 caregivers involved in a study of urban 7- to 11-year-old youth with disruptive behavior disorders reported symptoms of depression that reached clinically significant levels. Hammen, Burge, and Adrian (1991) found that diagnoses of depression among youth were predicted by stresses in their own lives, maternal depression, and interactions between the two. Other studies (Cummings, Keller, & Davies, 2005; Foster et al., 2008; Kane & Garber, 2009; Marchand, Hock, & Widman, 2002) have also noted statistically significant relationships between parental or caregiver depression and youth behavioral problems, while some have found that this link is less clear (Knox, Burkheart, & Khuder, 2011).
Challenges unique to homelessness can also impair parenting skills. Homeless caregivers may have less confidence in their caregiving than low-income parents with housing (Lee et al., 2010). Homeless families and youth may also face particular risks related to parenting stress, parental depression, and negative parenting practices (Holtrop, McNeil, & McWey, 2013). However, many at-risk homeless parents are dedicated to their children, in spite of the numerous stresses that their families face—and homeless families can be resilient (Holtrop et al., 2013).
Method
Data
The data analyzed in this study were drawn from the HIV Out-reach for Parents and Early adolescents (HOPE) Family Program (McKay et al., 2010). This was a family-based HIV and drug abuse prevention program that assessed early adolescent youth outcomes, adult caregiver outcomes, and family-level outcomes. The program targeted pre- and early adolescent homeless youth (aged 11–14 years) who resided in shelters with their caregivers between 2007 and 2010.
Recruitment
Convenience sampling was used to recruit participants from 10 of the 70 Tier II shelters throughout five New York City boroughs. This method enabled the study to obtain data about basic trends in homeless families living together in shelters. Tier II shelters were funded by the Department of Homeless Services and managed by not-for-profit and public agencies. Families also had to meet requirements for residing in Tier II shelters. These shelters can be differentiated from others by the following characteristics: (1) only adult caregivers and their children may reside there, (2) families were determined to be shelter eligible, meaning that their housing situation has been investigated and they were eligible for temporary shelter assistance and help in securing permanent housing, (3) cooking facilities were available for residents, and (4) case managers were employed to assist families in accessing housing and social service resources. Tier II shelters vary in size, that is, approximately 30–100 families might reside in a Tier II shelter.
Sample
The primary focus of this cross-sectional analysis was to examine the relationships between caregiver exposure to violence, caregiver depression, and depression and behavioral problems of homeless youth. Overall, 248 youth and their caregivers participated in either the HOPE Family Program (a multifamily group intervention) or health education based on the random assignment of the 10 family shelters involved. This study is based on secondary analysis of baseline data collected from 209 youth and their caregivers who were assigned to both groups. The youth whose data were used in this study were identified as the first children in their families to be registered for the program, and the data for any additional children in each family were not examined.
The final sample consisted of 209 youth and 209 caregivers, with no exclusions (total N = 418). The information for this study is based on questionnaires completed by study participants at baseline. Caregivers were predominantly female (91%), with 9% of caregivers being male. Youth gender reflected slightly more males (55%) than females (45%). Caregiver ages at the beginning of the study ranged from 20 to 58 (M = 37.95, SD = 6.87). Child ages at the beginning of the study ranged from 9 to 16 (M = 12.32, SD = 1.35). Participating caregivers stemmed from differing ethnic backgrounds; of the 173 who answered these questions (36 missing), 86% were Hispanic, not Black, 71% were Black, not Hispanic, 13% were Black and Hispanic, and 3% were neither. Of the 177 youth answering these questions (32 missing), 92% identified as Black, not Hispanic, 57% identified as Hispanic, not Black, 24% identified as Black and Hispanic, and 4% identified as neither.
Measures
Caregiver Depression
Caregiver mental health was measured using the Brief Symptom Inventory (BSI; Derogatis, 1993), which is a shorter version of the Symptom Checklist-90-Revised (Derogatis, 2000; Derogatis, Rickels, & Rock, 1976). This is a measure intended for adult subjects aged 17 and older. Participants rated symptoms experienced during the past week on a 5-point Likert-type scale (i.e., 0 representing not at all to 4 representing extremely). For this study, the focus was on the depression subscale, which consists of six questions related to areas including “thoughts of ending your life,” “feeling no interest in things,” and “feeling hopeless about the future.” The depression subscale of the BSI has good test–retest reliability (.84) and internal consistency (α = .85; Derogatis, 1993).
Youth Depression Symptoms
Youth completed a self-report measure, the Children's Depression Inventory (CDI; Kovacs, 1985, 1992 as cited in Kovacs & MHS Staff, 2003; Masip, Amador-Campos, Gómez-Benitos, & del Barrio, 2010). They reflected over their experiences from the last 2 weeks to complete a 10-item questionnaire with a 3-point Likert-type scale (0 = absence of symptomatology 1 = mild symptomatology, and 2 = severe symptomatology). The CDI has been widely used for assessing depressive symptoms in childhood and adolescence (Masip et al., 2010). Cronbach's α for the measure is good, ranging between .80 and .94 (Saylor, Finch, Spirito, & Benett, 1984). Test–retest reliability varies between .83 and .84 (Kovacs, 1992; Saylor et al., 1984). The HOPE questionnaire included 16 of the 27 items in the CDI, with items including “I am sad once in a while/many times/all the time,” I like myself/I do not like myself/I hate myself,” and “I do not think about killing myself/I think about killing myself but I would not do it/I want to kill myself.”
Exposure to Violence
Caregivers and adolescents completed six of the seven questions that comprise the Exposure to Violence Subscale from the City Stress Inventory (Ewart & Suchday, 2002). Self-reports were on a Likert-type scale. Participants (both caregivers and youth) rated their responses ranging from 0 through 3: never (0), once (1), a few times (2), and often (3). Statements included “A family member was attacked or beaten” and “Someone threatened to hurt a member of my family.” The complete Exposure to Violence subscale has good internal consistency of r = .85. Test–retest reliability for the complete subscale was .75 (Ewart & Suchday, 2002).
Child Behavioral Problems
Youth behavioral difficulties were measured through the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997; Goodman, Meltzer, & Bailey, 1998). Caregivers rated their children's behaviors on items including, “My child often loses temper” and “My child has at least one good friend.” Each answer ranged from 0 to 2. Caregivers completed all five subscales of this 25-item measure. The subscales include emotional symptoms, conduct problems, hyperactivity/inattention, peer problems, and prosocial behavior. For this study, youth behavioral problems were assessed using the total of the conduct problems and hyperactivity/inattention subscales. Internal consistency for the full scale is satisfactory (.73). Average test–retest reliability is .62 (Goodman, 2001).
Race
Caregivers and youth self-identified their ethnic backgrounds by answering the questions “Are you Hispanic or Latino?” and “Are you Black?” Based on the answers to these two questions, respondents were broken into the following categories: Black, not Hispanic; Hispanic, not Black; Black and Hispanic; and neither.
Age
Caregiver and youth ages were calculated by using the difference between the birth date and the first date on which they were interviewed.
Analytic Strategy
Preliminary univariate and bivariate analyses were conducted using IBM SPSS Statistics 20, 21, and 22. Multivariate relationships were analyzed through Structural Equation Modeling, using Amos 22.
Results
Selected Measures
On a measure of exposure to violence, consisting of six questions from the City Stress Inventory (Ewart & Suchday, 2002) with a range of 0–6, the mean score of the caregivers was 2.68, while the mean score of the youth was 2.52. This indicates that it is common for both caregivers and adolescents in these families to have witnessed or experienced multiple violent, stressful, potentially traumatic events.
On a measure of caregiver depression, the depression subscale from the BSI, which has a range of 0–24, the mean score was 3.89. On a measure of youth depression symptoms, consisting of questions from the CDI (range of 0–32), the mean score was 4.44. These scores indicate that both caregivers and youth commonly experienced some symptoms of depression, but that the average overall rates of depressive symptoms were relatively low.
On a measure representing youth behavioral problems, combining the conduct problems and hyperactivity/inattention sub-scales of the SDQ (range of 0–20), the mean score was 5.62. Considering that scores of 2 for conduct problems and 5 for hyperactivity/inattention are considered to fall within the normal (subclinical) range, this indicates that many caregivers in the sample viewed their children as having relatively low levels of behavioral problems. However, 36.4% of the youth were rated by their caregivers as having scores of 7 or more, indicating that more than one third of the sample had significant behavioral problems, in the eyes of their caregivers.
Selected Preliminary Bivariate Analyses
Statistically significant bivariate relationships were found between caregiver violence exposure and caregiver depression (r = .22, p < .01), caregiver depression and youth depression symptoms (r = .21, p < .01), and caregiver depression and youth behavioral problems (r = .36, p < .01). There was also a statistically significant bivariate relationship between youth depression symptoms and youth behavioral problems (r = .160, p < .05 level; see Table 1).
Table 1.
Pearson's Correlations.
| Correlations | |||||
|---|---|---|---|---|---|
| Caregiver Violence Exposure |
Caregiver Depression |
Youth Behavioral Problems |
Youth Depression Symptoms |
||
| Caregiver violence exposure | Pearson correlation | 1 | .221** | .138 | −.061 |
| Sig. (two-tailed) | .006 | .090 | .462 | ||
| N | 164 | 152 | 152 | 150 | |
| Caregiver depression | Pearson correlation | .221** | 1 | .363** | .208** |
| Sig. (two-tailed) | .006 | .000 | .005 | ||
| N | 152 | 195 | 183 | 179 | |
| Youth behavioral problems | Pearson correlation | .138 | .363** | 1 | .160* |
| Sig. (two-tailed) | .090 | .000 | .031 | ||
| N | 152 | 183 | 195 | 182 | |
| Youth depression symptoms | Pearson correlation | −.061 | .208** | .160* | 1 |
| Sig. (two-tailed) | .462 | .005 | .031 | ||
| N | 150 | 179 | 182 | 192 | |
Correlation is significant at the .01 level (two-tailed).
Correlation is significant at the .05 level (two-tailed).
Multivariate Model
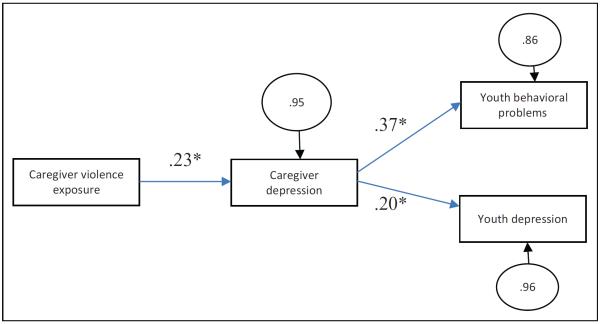
The fit of the model in Figure 1 was evaluated with Amos 20.0, using a maximum likelihood algorithm. A variety of indices of model fit were evaluated. The overall χ2 test of model fit was statistically nonsignificant, χ2(2) = 2.26, p < .33. The root mean square error of approximation was .025. The p value for the test of close fit was .49. The comparative fit index was .993. Modification indices and the standardized root mean square residual could not be run, as there were some missing data. The available indices uniformly point toward good model fit. Inspection of the residuals revealed no significant points of ill fit in the model.
Figure 1.
Multivariate Model *p < .05
Standardized coefficients appear on each path. All of the path coefficients were statistically significant. In other words, caregiver violence exposure has a statistically significant relationship with youth behavioral problems and youth depression symptoms, as mediated by caregiver depression.
The path from caregiver violence exposure to caregiver depression was positive and statistically significant (β = .23, p < .05). The path from caregiver depression to youth behavioral problems was also positive and statistically significant (β = .37, p < .05), as was the path from caregiver depression to youth depression symptoms (β = .20, p < .05).
The error terms indicate the proportion of unexplained variance in the endogenous variables (i.e., they are error variances in standardized form). The variables in the model accounted for approximately 14% of the variance in youth behavioral problems and 4% of the variance in youth depression. The error terms for youth behavioral problems and youth depression were also correlated, and they were not statistically significant.
Discussion
This study implies that youth behavioral health is associated with caregiver mental health, which, in turn, is associated with caregiver trauma exposure. This highlights the importance of taking into account caregiver mental health while treating youth externalizing and internalizing symptoms and ensuring that caregivers, too, have access to adequate treatment and supports. Furthermore, this treatment should be trauma informed, given the link between trauma and mental health.
Each of these areas points to needs related to the preparation of the social work workforce. Social workers serving families and youth—particularly families and youth experiencing homelessness and other major psychosocial stressors—should be educated about the links between trauma exposure and caregiver, youth, and family outcomes. They should, further, be trained in how to provide effective trauma-informed care. These social worker professionals and students should also be provided with training and resources related to the engagement of caregivers and families, even in cases in which the primary focus is on the child. Education about and training in evidence-informed parenting interventions should also be more widely included in the professional development of social workers working with families and children.
There are a number of evidence-based interventions for youth who have experienced trauma. Forty-two such service approaches are profiled on the website of the National Child Traumatic Stress Network (NCTSN, n.d.) as “Empirically Supported Treatments and Promising Practices” that are currently being implemented at NCTSN centers. Further, 16 interventions related to child trauma are currently recognized by the SAMHSA as “Evidence-Based Programs and Practices” as part of their National Registry of Evidence-Based Programs and Practices (SAMHSA, 2013). While not all of the interventions included on these lists highlight the importance of working with caregivers and families, a number of these interventions do focus explicitly on the child–caregiver relationship as a potential source of strength, resilience, and healing in the face of trauma. These include the following: Attachment, Self-Regulation, and Competency: A Comprehensive Framework for Intervention with Complexly Traumatized Youth, Child and Family Traumatic Stress Intervention, Child–Parent Psychotherapy, Combined Parent–Child Cognitive Behavioral Therapy (CPC-CBT): Empowering Families Who Are at Risk for Physical Abuse, Parent–Child Interaction Therapy, Real Life Heroes, Trauma Adapted Family Connections, Trauma Affect Regulation: Guide for Education and Therapy, Trauma-Focused CBT (TF-CBT), and Trauma Systems Therapy.
Limitations of this study include the following. The sample may not be representative of all homeless families. The cross-sectional design of the study makes it impossible to determine causation. There may be bias related to the self-reporting of data. In some cases, a subset of the questions from a measure or subscale was used; validity and reliability thus may differ from those of the complete measure or subscale. Finally, due to missing data and some use of post hoc analysis, further research should be conducted to confirm these results.
Acknowledgments
A special thanks to the members of the Community Collaborative Board, who worked as coordinators for the HOPE Family Program.
Funding The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by grants from the National Institute of Drug Abuse (R01DAO18574).
Footnotes
This article was previously presented at the Society for Social Work and Research's 18th Annual Conference, San Antonio, Texas, January 15–19, 2014. It was invited and accepted by the Editor.
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anooshian LJ. Violence and aggression in the lives of homeless children. Journal of Family Violence. 2005;20:373–387. [Google Scholar]
- Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. American Journal of Psychiatry. 1998;155:1561–1564. doi: 10.1176/ajp.155.11.1561. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Weinreb LF, Buckner JC, Browne A, Salomon A, Bassuk SS. The characteristics and needs of sheltered homeless and low-income housed mothers. Journal of American Medical Association. 1996;276:640–646. [PubMed] [Google Scholar]
- Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection. Biological Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Buckner JC, Beardslee WR, Bassuk EL. Exposure to violence and low-income children's mental health: Direct, moderated, and mediated relations. American Journal of Orthopsychiatry. 2004;74:413–423. doi: 10.1037/0002-9432.74.4.413. [DOI] [PubMed] [Google Scholar]
- Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse & Neglect. 2011;35:408–413. doi: 10.1016/j.chiabu.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Mott J, Levy S, Flay B. The relation of perceived neighborhood danger to childhood aggression: A test of mediating mechanisms. American Journal of Community Psychology. 2000;28:83–103. doi: 10.1023/a:1005194413796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad BS. Maternal depressive symptoms and homeless children's mental health: Risk and resiliency. Archives of Psychiatric Nursing. 1998;12:50–58. doi: 10.1016/s0883-9417(98)80008-3. [DOI] [PubMed] [Google Scholar]
- Coverdale JH, Turbott SH. Sexual and physical abuse of chronically ill psychiatric outpatients compared with a matched sample of medical outpatients. The Journal of Nervous and Mental Disease. 2000;188:440–445. doi: 10.1097/00005053-200007000-00008. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process mode of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology. 2005;114:3–15. doi: 10.1037/0021-843X.114.1.3. doi:10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson GC, Neale JM, editors. Abnormal psychology. 7th ed John Wiley; New York, NY: 1998. [Google Scholar]
- Derogatis LR. BSI Brief Symptom Inventory: Administration, scoring, and procedures manual. Pearson; San Antonio, TX: 1993. [Google Scholar]
- Derogatis LR. SCL-90-R. In: Kazdin AE, editor. Encyclopedia of psychology. Vol. 7. American Psychological Association; Washington, DC: 2000. pp. 192–193. [Google Scholar]
- Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: A step in the validation of a new self-report scale. British Journal of Psychiatry. 1976;128:280–289. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: Development and validation of a neighborhood stress index. Health Psychology. 2002;21:254–262. doi: 10.1037//0278-6133.21.3.254. doi:10.1037/0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramarante PJ, Rush JA, King CA. Course and severity of maternal depression: Associations with family functioning and child adjustment. Journal of Youth and Adolescence. 2008;37:906–916. doi: 10.1007/s10964-007-9216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearon JS, Bellack AS. Women with schizophrenia and co-occurring substance use disorders: an increased risk for violent victimization and HIV. Community Mental Health Journal. 1999;35:401–419. doi: 10.1023/a:1018778310859. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Edleson JL. Young children's exposure to intimate partner violence: Towards a developmental risk and resilience framework for research and resilience. Journal of Family Violence. 2007;22:151–163. [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire (SDQ) Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self-report version. European Child and Adolescent Psychiatry. 1998;7:125–130. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- Gopalan G, Dean-Assael K, Klingstein K, Chacko A, McKay M. Caregiver depression and youth disruptive behavior difficulties. Social Work in Mental Health. 2011;9:56–70. doi: 10.1080/15332985.2010.494528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gory ML, Ritchey FJ, Mullis J. Depression among the homeless. Journal of Health and Social Behavior. 1990;31:87–102. [PubMed] [Google Scholar]
- Hammen C, Burge D, Adrian C. Timing of mother and child depression in a longitudinal study of children at risk. Journal of Consulting and Clinical Psychology. 1991;59:341–345. doi: 10.1037//0022-006x.59.2.341. [DOI] [PubMed] [Google Scholar]
- Holt S, Buckley H, Whelan S. The impact of exposure to domestic violence on children and young people: A review of the literature. Child Abuse & Neglect. 2008;32:797–810. doi: 10.1016/j.chiabu.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Holtrop K, McNeil S, McWey LM. It's a struggle but I can do it. I'm doing it for me and my kids.”: The psychosocial characteristics and life experiences of at-risk homeless parents in transitional housing. Journal of Marital and Family Therapy. 2013 doi: 10.1111/jmft.12050. Advanced online publication. doi:10.1111/jmft.12050. [DOI] [PubMed] [Google Scholar]
- Howard KS, Cartwright S, Barajas RG. Examining the impact of parental risk on family functioning among homeless and house families. American Journal of Orthopsychiatry. 2009;79:326–335. doi: 10.1037/a0016599. [DOI] [PubMed] [Google Scholar]
- Huey L, Fthenos G, Hryniewicz D. If something happened, I will leave it, let it go and move on”: Resiliency and victimized homeless women's attitudes toward mental health counseling. Journal of Interpersonal Violence. 2013;28:295–319. doi: 10.1177/0886260512454717. doi:10.1177/0886260512454717. [DOI] [PubMed] [Google Scholar]
- Kane P, Garber J. Parental depression and child externalizing and internalizing symptoms: Unique effects of fathers' symptoms and perceived conflict as a mediator. Journal of Child and Family Studies. 2009;18:465–472. [Google Scholar]
- Knox M, Burkheart K, Khuder SA. Parental hostility and depression as predictors of young children's aggression and conduct problems. Journal of Aggression, Maltreatment & Trauma. 2011;20:800–811. [Google Scholar]
- Kovacs M. The Children's Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M. Manual of the Children's Depression Inventory. Multi-Heath Systems; Toronto, Canada: 1992. [Google Scholar]
- Kovacs M, Staff MHS. Children's Depression Inventory (CDI): Technical manual update. Multi-Health Systems; Toronto, Canada: 2003. [Google Scholar]
- Kushel MB, Evans JL, Perry S, Robertson MJ, Moss AR. No door to lock: Victimization among homeless and marginally housed persons. Archives of Internal Medicine. 2003;163:2492–2499. doi: 10.1001/archinte.163.20.2492. doi:10.1001/archinte.163.20.2492. [DOI] [PubMed] [Google Scholar]
- Lee SS, August GJ, Gewirtz AH, Klimes-Dougan B, Bloomquist ML, Realmuto GM. Identifying unmet mental health needs in children of formerly homeless mothers living in a supportive housing community sector of care. Journal of Abnormal Child Psychology. 2010;38:421–432. doi: 10.1007/s10802-009-9378-1. [DOI] [PubMed] [Google Scholar]
- Marchand JF, Hock E, Widaman K. Mutual relations between mother's depressive symptoms and hostile-controlling behavior and young children's externalizing and internalizing behavior problems. Parenting Science and Practice. 2002;2:335–353. [Google Scholar]
- Masip AF, Amador-Campos JA, Gómez-Benito J, del Barrio GV. Depression inventory in community and clinical sample. The Spanish Journal of Psychology. 2010;13:990–999. doi: 10.1017/s1138741600002638. [DOI] [PubMed] [Google Scholar]
- McKay MM, Gopalan G, Franco LM, Kalogerogiannis K, Umpierre M, Olshtain-Mann O, Goldstein L. It takes a village to deliver and test child and family-focused services. Research on Social Work Practice. 2010;20:476–482. doi: 10.1177/1049731509360976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meadows-Oliver M. Mothering in public: A meta-synthesis of homeless women with children living in shelters. Journal for Specialists in Pediatric Nursing. 2003;8:130–136. doi: 10.1111/j.1088-145x.2003.00130.x. [DOI] [PubMed] [Google Scholar]
- Mowbray CT, Bybee D, Oyserman D, Mcfarlane P, Bowersox N. Psychosocial outcomes for adult children of parents with severe mental illnesses: Demographic and clinical history predictors. Health & Social Work. 2006;31:99–108. doi: 10.1093/hsw/31.2.99. [DOI] [PubMed] [Google Scholar]
- National Child Traumatic Stress Network National Child Traumatic Stress Network empirically supported treatments and promising practices. n.d. Retrieved August 31, 2013, from http://www.nctsn.org/resources/topics/treatments-that-work/promising-practices.
- National Child Traumatic Stress Network Homelessness and Extreme Poverty Working Group Facts on trauma and homeless children. 2005 Retrieved from http://www.nctsnet.org/nctsn_assets/pdfs/promising_practices/Facts_on_Trauma_and_Homeless_Children.pdf.
- Oyserman D, Bybee D, Mowbray C. Influences of maternal mental illness on psychological outcomes for adolescent children. Journal of Adolescence. 2002;25:587–602. doi: 10.1006/jado.2002.0506. [DOI] [PubMed] [Google Scholar]
- Padgett D, Struening EL. Victimization and traumatic injuries among the homeless: Associations with alcohol, drug, and mental problems. American Journal of Orthopsychiatry. 1992;62:525–534. doi: 10.1037/h0079369. [DOI] [PubMed] [Google Scholar]
- Rayburn NR, Wenzel SL, Elliott MN, Hambarsoomians K, Marshall GN, Tucker JS. Trauma, depression, coping, and mental health service seeking among impoverished women. Journal of Consulting and Clinical Psychology. 2005;73:667–677. doi: 10.1037/0022-006X.73.4.667. [DOI] [PubMed] [Google Scholar]
- Rog DJ, McCombs-Thornton KL, Gilbert-Mongelli AM, Brito MC, Holupka CS. Implementation of the homeless families program: 2. Characteristics, strengths, and needs of participant families. American Journal of Orthopsychiatry. 1995;65:514–528. doi: 10.1037/h0079675. [DOI] [PubMed] [Google Scholar]
- Samuels J, Shinn M, Buckner J. Homeless children: Update on research, policy, programs, and opportunities. 2010 Retrieved from http://aspe.hhs.gov/hsp/10/homelesschildrenroundtable/index.shtml.
- Saylor CF, Finch AJ, Spirito A, Bennett B. The Children's Depression Inventory: A systematic evaluation of psychometric properties. Journal of Consulting and Clinical Psychology. 1984;52:955–967. doi: 10.1037//0022-006x.52.6.955. [DOI] [PubMed] [Google Scholar]
- Singer MI, Anglin TM, Song L, Lunghofer L. Adolescents' exposure to violence and associated symptoms of psychological trauma. Journal of American Medical Association. 1995;273:477–482. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Current statistics on the prevalence and characteristics of people experiencing homelessness in the United States. 2011 Retrieved from http://www.nrchmi.samhsa.gov/ResourceFiles/hrc_factsheet.pdf.
- Substance Abuse and Mental Health Services Administration NREPP: SAMHSA's National Registry of Evidence-based Programs and Practices. 2013 Retrieved from http://www.nrepp.samhsa.gov/ViewAll.aspx.
- The National Center on Family Homelessness The characteristics and needs of families experiencing homelessness. 2008 Retrieved from http://www.familyhomelessness.org/media/147.pdf.
- U.S. Department of Housing and Urban Development The 2010 annual homeless assessment report to Congress. 2011 Retrieved from http://portal.hud.gov/hudportal/HUD?src¼/press/press_releases_media_advisories/2011/HUDNo.11-121.
- Wenzel SL, Leake B, Gelberg L. Risk factors for major violence among homeless women. Journal of Interpersonal Violence. 2001;16:739–752. [Google Scholar]
- Wenzel SL, Tucker JS, Elliott MN, Marshall GN, Williamson SL. Physical violence against impoverished women: A longitudinal analysis of risk and protective factors. Women's Health Issues. 2004;14:144–154. doi: 10.1016/j.whi.2004.06.001. doi:10.1016/j.whi.2004.06.001. [DOI] [PubMed] [Google Scholar]