Abstract
Background & Aims
Complete eradication of Barrett’s esophagus (BE) often requires multiple sessions of radiofrequency ablation (RFA). Little is known about the effects of case volume on the safety and efficacy of RFA, or the presence or contour of learning curves for this procedure.
Methods
We collected data from the US RFA Patient Registry (from 148 institutions) on patients who underwent RFA for BE from July 2007 to July 2011. We analyzed the effects of the number of patients treated by individual endoscopists and individual centers on safety and efficacy outcomes of RFA. Outcomes, including stricture, bleeding, hospitalization, and complete eradication of intestinal metaplasia (CEIM), were assessed using logistic regression. The effect of center and investigator experience on number of treatment sessions to achieve CEIM was examined using linear regression.
Results
After we controlled for potential confounders, we found that as case experience of endoscopists and centers increased, the numbers of treatment sessions required to achieve CEIM decreased. This relationship persisted after adjusting for patient age, sex, race, length of BE, and presence of pretreatment dysplasia (P<.01). Center experience was not significantly associated with overall rates of CEIM or complete eradication of dysplasia. We did not observe any learning curve with regard to risks of stricture, gastrointestinal bleeding, perforation, or hospitalization (P>.05).
Conclusions
Based on an analysis of a large multicenter registry, efficiency of the treatment, as measured by number of sessions needed to achieve CEIM, increased with case volume, indicating a learning curve effect. This trend began to disappear after treatment of approximately 30 patients by the center or individual endoscopist. However, there was no significant association between safety or efficacy outcomes and prior case volume.
Keywords: endoscopy, training, database analysis, cancer prevention
Barrett’s esophagus (BE) is a premalignant condition affecting 1–2% of the general population, which is associated with increased risk of esophageal adenocarcinoma.1–3, With the increasing incidence of BE and esophageal adenocarcinoma, effective strategies for decreasing cancer risk are essential.4–6 Recent American Gastroenterological Association guidelines suggest that endoscopic eradication therapy is a treatment option for BE, and that endoscopic eradication therapy is the treatment of choice in BE with HGD.7
Radiofrequency ablation (RFA) is a safe and effective endoscopic ablation modality.8, 9 RFA typically requires a range of 2–6 treatment sessions to fully eliminate the BE tissue, generally followed by periodic endoscopic surveillance examinations to assess for BE recurrence.10 Although RFA is now commonly used to treat BE, the association between the volume of cases performed and the outcomes of RFA therapy is unknown.
The aim of this study is to assess the effect of site volume on safety and efficacy outcomes associated with RFA using a U.S. multicenter registry. We hypothesized that increasing case volume might be associated with superior outcomes, after controlling for pertinent potential confounders.
METHODS
U.S. RFA Patient Registry
The U.S. RFA Patient Registry is a multi-center collaboration reporting processes and outcomes of care for patients treated with RFA for BE. In total there are 148 institutions in the registry (113 community-based, 35 academic-affiliated). The methods of the U.S. RFA Registry have been previously described.11 The registry does not specify protocols for care, but provides a framework for treatment and follow-up of patients with BE (non-dysplastic, low-grade dysplasia, high-grade dysplasia, and intramucosal carcinoma). It was developed as a research tool to monitor clinical outcomes for patients undergoing treatment of BE with RFA using the HALO Ablation Systems and is funded by GI Solutions who produces this equipment (Sunnyvale, CA, a subsidiary of Covidien.) All physicians participating in this registry either used Western institutional review board (IRB) approval, or for those institutions with their own IRB, IRB approval through their respective institutions.
Patient Eligibility
Patient were enrolled from July 2007 to July 2011, and followed prospectively. Patients were eligible for inclusion in the registry if: (1) they had endoscopic evidence of columnar metaplasia in the tubular esophagus with accompanying biopsies demonstrating intestinal metaplasia (IM), and (2) they received RFA for BE. Subjects were classified using standardized histological grading, including non-dysplastic BE (NDBE), indefinite for dysplasia (IND), low-grade dysplasia (LGD), high-grade dysplasia (HGD), intramucosal carcinoma (IMC), and invasive adenocarcinoma (EAC).12 Those patients who had previously received one or more RFA treatments prior to enrollment had retrospective data collected, with prospective data collected for subsequent visits. Patients who had not yet undergone treatment were prospectively enrolled in the study.
Data Collection and Record Retention
Information collected in the registry includes demographic data, histology prior to treatment, endoscopic findings, number of treatment sessions, ablation outcomes, and complications. All data were recorded on standardized case report forms (CRFs) using an internet-based secured data entry and processing system. All CRFs are coded with a site code and patient code; no information identifying patients was contained on Registry documents. Data were collated into a central electronic database, with real-time monitoring for logic checks and consistency. Data were analyzed by investigators in the clinical epidemiology program at the UNC Center for Gastrointestinal Biology and Disease (T32 DK07634), who had complete access to the data.
Treatment Protocol
Data from previous clinical trials were given to all physicians as a guideline for treatment and follow-up of patients. However, because this was a registry study, the endoscopists could deviate from the suggested treatment protocols, depending on specific patient requirements and/or providers’ preferences. The suggested treatment protocol provided to physician investigators has been previously described.13
After enrollment, each patient was interviewed prior to treatment and a Baseline Encounter Form was completed. Our standardized protocol suggested medical therapy with high-dose twice-daily PPIs to minimize any baseline inflammatory changes of the esophageal mucosa and to decrease acid reflux prior to and throughout RFA treatment, unless the patient had a documented history of antireflux surgery.
At the initial visit, patients were treated with one of two ablation devices: the HALO360 Circumferential Ablation System or the HALO90 Focal Ablation System. The decision as to initial treatment modality was based on the burden of disease (Barrett’s segments of >3 cm are generally best treated with the circumferential catheter), as well as operator preference.
Follow-Up Protocol
The first follow-up visit was 2–3 months after treatment initiation. Recommendations for the first follow-up visit included additional circumferential or focal RFA treatment for any visible residual BE, depending on the extent of the disease. If no visible BE was observed, four-quadrant biopsies every cm for baseline dysplasia and every 2 cm for baseline non-dysplastic BE were recommended throughout the length of the pre-treatment BE. If these biopsies were clear of BE on pathologic review, the patients entered the surveillance phase (Figure 1). Initial surveillance was recommended at 3 months for those patients with pre-treatment HGD or IMC, and 6 months for those patients with pre-treatment NDBE, IND, or LGD. If follow-up biopsies revealed IM or dysplasia, recurrent treatment with RFA was recommended at the next endoscopy session.
Figure 1. Suggested follow-up protocol.
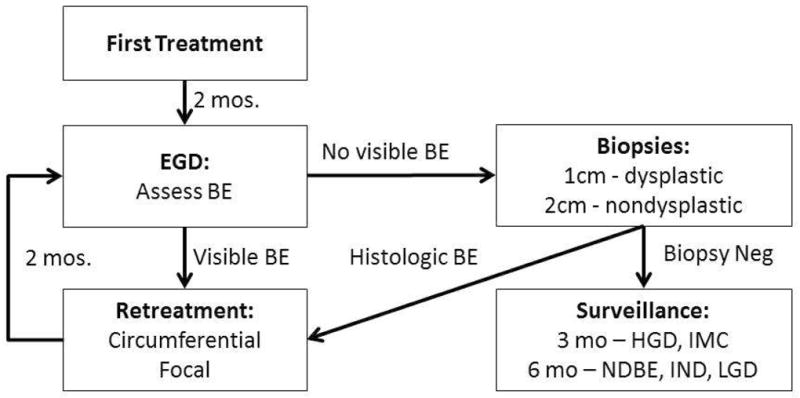
In the U.S. RFA registry the treatment and surveillance protocols were suggested but not enforced.
Adverse events were reported using standardized forms and terminology. Each site also complied with reporting guidelines for their institution regarding reporting adverse events to their IRB and to the FDA under the MDR reporting regulation in 21 C.F.R. Part 803.
Outcomes and Statistical Analysis
Our safety cohort included all patients treated with RFA. Primary safety outcomes included death, perforation, stricture, bleeding, and hospitalization. A stricture was defined as any narrowing of the esophageal lumen requiring dilation. Bleeding was considered clinically significant if it required hospitalization or blood transfusion.
Our efficacy cohort was restricted to subjects in the registry who had an endoscopic biopsy session performed 12 months or more after their initial treatment with RFA. Primary efficacy outcomes included complete eradication of intestinal metaplasia (CEIM), complete eradication of dysplasia (CED), and total number of RFA treatments to CEIM. CEIM was defined as the absence of intestinal metaplasia from all histologic specimens obtained during an endoscopic biopsy session at least 12 months after initial treatment, and no endoscopic evidence of BE. Additionally, to assess differences in outcome using a more stringent definition of CEIM, we also calculated CEIM in patients who had 2 consecutive biopsy sessions with CEIM. CED was defined as the absence of dysplasia from all histologic specimens obtained at least 12 months after initial treatment. Similarly, we also calculated CED in patients who had 2 consecutive biopsy sessions with CED. Total RFA sessions included both circumferential and focal RFA treatments.
In order to appropriately assess for a learning curve, site outcomes needed to reflect the order that a given patient had treatment within that site’s or endoscopist’s series. We therefore analyzed patient outcomes based upon the number of patients treated at a center as well as outcomes based on the number of patients treated by each endoscopist prior to each individual’s enrollment. We also performed ordinary least squares regression to examine the relationship between the number of patients treated at a center prior to the patient’s first RFA treatment and the number of RFA treatments required to achieve CEIM. We examined trend using linear, quadratic, cubic, and log-transformed parameterizations using an R-squared a priori criterion for goodness of fit. The effect of center and investigator experience on stricture, bleeding, hospitalization, and CEIM were assessed using logistic regression adjusting for age, gender, race, BE length, and presence of pretreatment dysplasia. The effect of center and investigator experience on total treatment sessions needed to achieve CEIM was examined using linear regression, controlling for age, gender, race, BE length, and presence of pretreatment dysplasia. In tabular analyses of efficacy and safety outcomes, statistical significance testing was performed with the Cochrane-Armitage test for trend. The alpha for all significance tests and confidence limits was set at 0.05.
We performed multiple sensitivity analyses to assess the robustness of our findings. Because the definition of CEIM is not standardized, we examined the impact of requiring multiple (up to five) endoscopies without intestinal metaplasia to define CEIM. In order to assess the impact of very low volume sites, we excluded centers and endoscopists below varying thresholds of total case experience. To assess the impact of varying lengths of follow-up time during which study outcomes could occur, we performed right truncation at varying lengths of person-time. Generalized estimating equations (GEE) were used to account for any clustering by site in safety and efficacy outcomes. Statistical analysis was performed using STATA 13.0 and SAS 9.4.
RESULTS
Among 5521 patients included in the U.S. RFA Registry, 4052 (73%) were male, 5126 (93%) were Caucasian, and the mean age was 61.6 years (Table 1). The average length of BE was 4.1 cm with 2674 (48.3%) of patients having non-dysplastic BE at baseline. Patients underwent an average of 2.8 total RFA treatment sessions. Of these 5521 enrollees, 4359 (79%) were taking a twice-daily proton-pump inhibitor and 295 (5.3%) had a pre-treatment fundoplication. In total, 148 centers (113 community-based and 35 academic-affiliated institutions) were included in the registry. 1541 patients (28%) were treated at an academic center, compared to 3980 (72%) patients treated at a community practice. Of all enrolled patients, 4389 (79%) were prospectively enrolled, while the remaining 1132 (21%) had initial collection of some retrospective treatment data, with subsequent prospective collection of remaining treatment and post-treatment surveillance data.
Table 1.
Baseline Characteristics of patients treated with RFA in the U.S. RFA Registry
| N=5521 | |
|---|---|
|
| |
| Age, mean ± SD, years | 61.6 ± 11.4 |
| Race, n (%) | |
| Caucasian | 5126 (92.8) |
| Black | 82 (1.5) |
| Hispanic | 137 (2.5) |
| Asian/Pacific Islander/Other | 40 (0.7) |
| Unreported | 136 (2.5) |
| Male gender, n (%) | 4052 (73.4) |
|
| |
| Length of BE segment, mean ± SD, cm | 4.1 ± 3.3 |
| Pre-treatment fundoplication, n (%) | 295 (5.3) |
| Pre-treatment histology, n (%) | |
| Nondysplastic | 2674 (48.3) |
| Indefinite dysplasia | 406 (7.4) |
| Low-grade dysplasia | 1113 (20.2) |
| High-grade dysplasia | 1054 (19.1) |
| Intramucosal carcinoma | 209 (3.8) |
| Invasive adenocarcinoma | 65 (1.2) |
| Taking twice daily PPI, n (%) | 4359 (79.0) |
|
| |
| Treated with EMR before RFA, n (%) | 495 (9.0) |
| Total RFA treatments, mean ± SD | 2.8 ± 1.8 |
| Circumferential treatments, mean ± SD | 0.7 ± 1.0 |
| Focal treatments, mean ± SD | 2.1 ± 1.5 |
| Total biopsy sessions performed, mean ± SD | 2.8 ± 2.1 |
| Treatment at an academic medical center, n (%) | 1541 (27.9) |
Center Level Safety Analysis
All 5521 patients in the U.S. RFA Registry were included in the safety cohort. The number of patients treated with RFA prior to a given patient’s enrollment at a site was not significantly associated with the risk of stricture, GI bleeding, perforation or hospitalization (p> 0.05) (Table 2). There was a moderate amount of variation in the percentage of patients experiencing stricture at each site (Interquartile Range (IQR) 1.8% – 9.1%, Mean 6.4%, SD 5.5%). In order to assess for detection bias due to the collection of retrospective data, we also performed this site volume analysis including only patients prospectively enrolled, and the results were similar (Supplemental Table 1).
Table 2.
Safety of RFA based on center experience
| # of patients treated at center prior to enrollment
| |||||
|---|---|---|---|---|---|
| 1–10 | 11–20 | 21–30 | > 30 | P value | |
|
| |||||
| Patients, N | 1,280 | 891 | 666 | 2,684 | |
| Stricture, n (%) | 51 (4.0) | 47 (5.3) | 24 (3.6) | 111 (4.1) | 0.76 |
| Bleeding, n (%) | 9 (0.7) | 4 (0.5) | 1 (0.2) | 14 (0.5) | 0.53 |
| Perforation, n (%) | 1 (0.1) | 1 (0.1) | 0 | 0 | 0.12 |
| Hospitalization, n (%) | 15 (1.2) | 8 (0.9) | 6 (0.9) | 18 (0.7) | 0.11 |
| # of patients treated by investigator prior to enrollment
| |||||
|---|---|---|---|---|---|
| 1–10 | 11–20 | 21–30 | > 30 | P value | |
|
| |||||
| Patients, N | 1,741 | 910 | 604 | 2,266 | |
| Stricture, n (%) | 74 (4.3) | 51 (5.6) | 24 (4.0) | 84 (3.7) | 0.19 |
| Bleeding, n (%) | 16 (0.9) | 4 (0.4) | 2 (0.3) | 6 (0.3) | 0.01 |
| Perforation, n (%) | 1 (0.1) | 1 (0.1) | 0 | 0 | 0.22 |
| Hospitalization, n (%) | 25 (1.4) | 6 (0.7) | 6 (1.0) | 10 (0.4) | <0.01 |
Provider Level Safety Analysis
Endoscopists who had previously performed RFA treatments on more than 20 patients treated about half of patients in the registry, while the remainder were treated by endoscopists with 20 or less patients’ experience. There were no differences in stricture or perforation rates based on provider individual experience prior to a given patient’s enrollment (Table 2). Investigator experience was significantly associated with increased bleeding and hospitalization. However, these findings were small in magnitude and not robust to sensitivity analysis if investigators with less than ten total patients in the registry were excluded, suggesting possible selection bias. Modest variation in the proportion of patients with strictures was seen among individual providers (IQR 1.8% – 7.2%, Mean 5.3%, SD 6.0%).
Center Level Efficacy Analysis
In total, 4118 patients had a biopsy session performed 12 months or more after their initial treatment with RFA, and were included in the efficacy analysis. In bivariate analysis, higher center volume was significantly associated with slight improvements in CEIM (p< 0.01) but not with CED (p=0.39) rates (Table 3). However, this association between case volume and improvement in CEIM disappeared in multivariable analysis after controlling for age, gender, race, length and pre-treatment dysplasia (p=0.17). When a more stringent definition of CEIM (2 endoscopies demonstrating CEIM) was applied, the association remained non-significant (p=0.39) (Supplemental Table 2). Additionally, no association between CEIM and site volume was seen in analysis of only patients who were prospectively enrolled (Supplemental Table 3).
Table 3.
Efficacy of RFA based on center experience prior to a given subject’s treatment
| # of patients treated at center prior to enrollment
| |||||
|---|---|---|---|---|---|
| 1–10 | 11–20 | 21–30 | > 30 | P value | |
|
| |||||
| Patients, N | 977 | 685 | 511 | 1,945 | |
| CED, n/N (%) | 519/560 (93) | 342/370 (92) | 263/278 (95) | 957/1,016 (94) | 0.39 |
| CEIM, n (%) | 814 (83) | 575 (84) | 446 (87) | 1,688 (87) | <0.01 |
| Total RFA sessions to CEIM, mean±SD | 3.2 ± 1.8 | 2.9 ± 1.8 | 2.7 ± 1.6 | 2.7 ± 1.6 | <0.01 |
| # of patients treated by investigator prior to enrollment
| |||||
|---|---|---|---|---|---|
| 1–10 | 11–20 | 21–30 | > 30 | P value | |
|
| |||||
| Patients, N | 977 | 685 | 511 | 1,945 | |
| CED, n/N (%) | 663/694 (96) | 329/351 (94) | 199/216 (92) | 929/963 (96) | 0.29 |
| CEIM, n (%) | 1,019 (83) | 537 (85) | 343 (85) | 1,624 (87) | 0.01 |
| Total RFA sessions to CEIM, mean±SD | 3.1 ± 1.8 | 2.9 ± 1.5 | 2.7 ± 1.8 | 2.7 ± 1.7 | <0.01 |
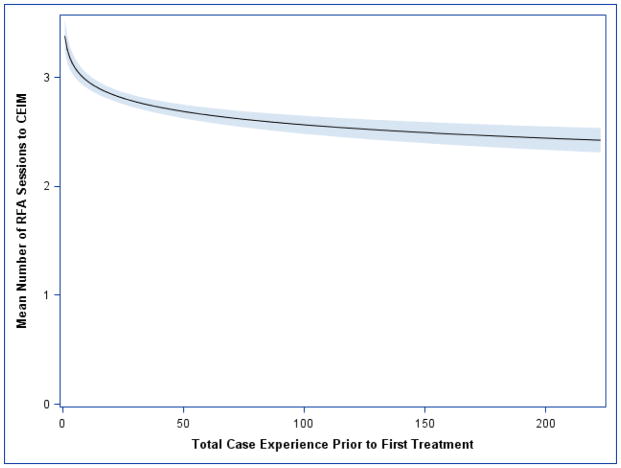
In contrast to the safety and efficacy data, center volume was associated with a lower number of treatment sessions needed to achieve CEIM (p<0.001) and this association persisted after adjusting for BE length, baseline presence of dysplasia, treatment with EMR before RFA, and treatment at an academic medical center (p <0.001). These efficiency findings were highly robust to sensitivity analyses, including the requirement of up to five clean endoscopies to define CEIM. The protective effect of a center’s prior patient experience was best fit (R-Square = 0.016) with a log transformation (Figure 2). This reveals a threshold effect that levels off at about thirty patients, where the first ten patients treated at a center increase the mean number of RFA sessions required by an unadjusted 0.50 (95% CL: [0.36, 0.65]) and multivariable-adjusted 0.30 (95% CL: [0.17, 0.43]) compared to patients treated after a center had more than thirty procedures experience. There was no significant difference in the number of treatment sessions to CEIM between community treatment centers (mean 2.40) and academic centers (mean 2.43, p = 0.63).
Figure 2. Mean Number of Sessions Required to Achieve CEIM by the Center’s Total Case Experience Prior to Patients’ First RFA Treatment.
Efficiency reached a steady state after about thirty patients treated with RFA at a given center.
Provider Level Efficacy Analysis
When comparing the number of patients treated by investigators prior to enrollment, there was no difference in CED rates with 92–96% of patients achieving CED regardless of provider level experience. CEIM rates were mildly improved in providers who performed higher numbers of treatments (87% in providers who treated > 30 patients compared to 83% in providers who treated ≤ 10 patients; p = 0.01) (Table 3). The threshold for provider experience was similar to centers. On average, subjects treated after an endoscopist had completed 30 or more cases needed 0.5 (unadjusted 0.51 95% CL: [0.38, 0.65]) and multivariable-adjusted 0.35 (95% CL: [0.28, 0.47]) less treatment sessions to achieve CEIM (using both definitions of CEIM) compared to endoscopists with 10 or less RFA sessions.
Center Level Sensitivity Analyses
When we excluded centers with less than 7 total patients treated, no attenuation of the learning curve effect was observed for the number of RFA procedures required. However, there was attenuation of the small effect on CEIM, suggesting selection bias as a cause for this difference. Conclusions from safety and efficacy outcomes were similar when treated as rates. Random intercepts fit to each center as well as cluster analysis using generalized estimated equations (GEE) did not alter the conclusions of center level findings. Flexible adjustment for calendar time did not suggest a period effect.
Provider Level Sensitivity Analyses
When we excluded providers with less than ten total patients treated, no attenuation of the learning curve effect was observed for the number of RFA procedures required. The learning curve observed for the proportion of patients achieving CEIM was however attenuated when providers with less than ten total patients treatment were excluded, suggesting selection bias, similar to our center analysis. Conclusions from safety and efficacy outcomes were similar when treated as rates. Random intercepts fit to each provider as well as cluster analysis using GEE did not alter the conclusions of provider level findings. Flexible adjustment for calendar time did not suggest a period effect.
DISCUSSION
We assessed the effect of RFA site volume on safety and efficacy outcomes using the U.S. RFA Registry to assess for evidence of a “learning curve” with respect to the safety and efficacy of RFA treatment. Among the 5521 patients enrolled in the registry, the number of BE patients treated with RFA at a site prior to registry enrollment was not significantly associated with an increased risk of stricture, GI bleeding, perforation, or hospitalization. Although there appeared to be a statistically significant positive association between CEIM rates and volume in bivariate analysis, this association dissolved in multivariable analysis. However, a learning curve effect did appear in the efficiency of the treatment. Higher case volume was independently associated with a lower number of treatment sessions needed to achieve CEIM, after controlling for BE length, baseline presence of dysplasia, treatment with EMR before RFA, and treatment at an academic medical center (p<0.001). This effect seemed to attenuate after approximately 30 patients had been treated by an endoscopist or center, and accounted for approximately 0.5 additional treatments for patients who were in the first 10 patients treated by a provider as compared to patients who were treated after at least 30 RFAs had been performed. Further experience resulted in only a modest, insignificant reduction in number of treatments needed. While 0.5 additional treatments may, on the face of it, appear to be a relatively small number of additional treatments, given the large number of these procedures currently performed, and the significant costs associated with each treatment, the learning curve for RFA is likely associated with significant cumulative costs.
The previous limited work examining the learning curve associated with the use of RFA for treatment of BE demonstrates heterogeneous results. Zemlyak and colleagues performed a retrospective study of all patients who underwent RFA of BE with a HALO system at a single institution by a single, experienced endoscopist.14 This study encompassed 70 patients, with the number of RFA treatments required to achieve CEIM ranging from one to seven sessions. When comparing the first 25% of procedures to the latter 75%, or the first 50% to last 50% of procedures, there was no significant difference in time of procedure, complication rate, complication severity, or number of procedures to complete resolution of BE.14 The authors therefore concluded that there did not appear to be an appreciable learning curve associated with RFA treatment for BE, when performed by experienced endoscopists. The small number of cases in this study increases the chance of a type 2 error. This study also has limited generalizability, since all procedures were performed at a single center by one endoscopist. More recently, Fudman et al. performed a retrospective analysis of CEIM rates and endoscopic RFA volume at three tertiary care centers.15 In total, there were seven endoscopists who treated 417 patients with BE with RFA over a 6 year time period. They found that higher RFA volume was associated with increased rates of CEIM. Endoscopists who performed less than 10 RFAs were excluded, and the number of patients treated by each endoscopist varied significantly, ranging between 20–188. Both studies are limited by small numbers of endoscopists. Additionally, there was no standardized treatment and follow up protocol, increasing the potential for detection bias in recurrence and complication rates.
The importance of case volume in safety and efficacy outcomes has been demonstrated in other advanced endoscopic procedures. For example, van Vilsteren and colleagues assessed the efficacy and safety of the first 120 endoscopic resection procedures of early esophageal neoplasia performed by six endoscopists who were participating in an endoscopic resection training program.16 In this study, despite a structured, intense training program, the first 120 resections were associated with a 5% perforation rate, indicating that the number of procedures performed by these physicians may not be sufficient to reach the plateau of the learning curve in endoscopic resection.16 Several other studies on endoscopic mucosal resection and submucosal dissection have demonstrated that the experience and level of training of the endoscopist are associated with a decrease in perforation rate and procedure time.17–19 Additionally, Wani and colleagues evaluated learning curves in EUS among advanced endoscopy trainees (AETs) and noted that there was substantial variability in achieving competency.20 They found that there was a consistent need for more supervision even after AETs had surpassed the minimum number of cases currently recommended.20 Given data demonstrating learning curve issues in other advanced endoscopic procedures, it is not surprising that several important outcomes may improve with increased experience with RFA.
Our study has several limitations. Examination of threshold effects is necessarily imprecise, and the observed threshold at around thirty patients, though robust, should not be taken as exact or definitive. Given that it is a registry study, while we suggested treatment paradigms, they could not be mandated, which introduces the potential for variation among centers in treatment algorithms. Also, while the registry is a powerful tool with a large enrollment, we cannot assess the impact of any cases performed at a given site but not enrolled in the registry, or those performed before the registry was initiated at that site. However, we suspect that the risk of bias due to these effects is low, because the inception of the registry, in July of 2007, was shortly after FDA clearance of the ablation device in April of 2006, and because there was a monetary incentive to enroll patients. Also, similar to other registry studies, no re-interpretation of pathological specimens by a central lab was performed, and it is known that intra- and interobserver variation exists in interpreting BE histology.21, 22 Finally, while our study did not include all sites performing RFA in the U.S. over the observation period, it did include a large proportion, decreasing concerns regarding generalizability. .
Of note, many patients with non-dysplastic BE and some with invasive adenocarcinoma were treated with RFA in this registry. While most academic centers have reported primarily dysplastic cohorts, there are obviously a large number of non-dysplastic cases being done in real world practice, especially in community treatment centers. It is important to also point out that this registry spans 5 years and that many patients in this registry started treatment in 2007, prior to current guidelines.7 Also of note, there is considerable heterogeneity in societal guidelines as to the appropriate use of RFA in BE. While the current AGA guidelines state that “RFA, with or without EMR, should be a therapeutic option for select individuals with nondysplastic Barrett’s esophagus who are judged to be at increased risk for progression to high-grade dysplasia or cancer,” as well as those with LGD, the British Society of Gastroenterology endorses its use only in BE with high-grade dysplasia.23 As to the smaller number of patients with invasive adenocarcinoma, it is somewhat difficult to discern the intent of these treatments from the Registry data. We speculate that some of these treatments might have been with palliative intent, or perhaps for those with T1b adenocarcinoma, in whom data do suggest that endoscopic therapy may have curative efficacy.24
Our study has several strengths. This is by far the largest study to examine the effect of experience on the safety and efficacy of endoscopic therapy for BE. In addition, this study includes physician participants from 148 institutions, both community-based and academic-affiliated. The large diversity of practice settings, the variety of procedural volumes at the sites, and the inclusion of a large number of endoscopists improves the external validity of our results. Additionally, study definitions were a priori, and data were collected in a standardized fashion. Finally, we took into account the experience of the center on a per patient basis at the time of that patient’s treatment, as opposed to labeling a center as “high volume” or “low volume.” Thus, temporal changes due to experience, even in centers destined to be high volume centers, would be detected. This approach is superior to studies which divide centers by overall volume, obscuring any differential outcomes due to the early experience in high volume centers. Additionally, we have provided information with regards to the experience of both the treating center as well as the individual endoscopist
In conclusion, by using a nationwide registry of RFA treatment for BE, we found that increasing site volume and increased endoscopist case volume were associated with fewer treatment sessions to achieve CEIM, suggesting that the learning curve for RFA impacts the efficiency with which the site and physician deliver this service. However, site and case volume did not appear to impact stricture, bleeding or hospitalization rates. Additionally, there was no robust association between site volume and treatment efficacy rates. This suggests that RFA results are comparable regardless of whether the procedure is performed at a high volume or low volume center. Based on these data, concentration of RFA treatment at higher volume centers would not be expected to impact safety, or the ultimate likelihood of complete eradication of all intestinal metaplasia, but might result in cost savings due to a decreased number of treatments needed to achieve this outcome. Given the shape of this relationship, the benefits of centralization may be expected to decrease dramatically after a total patient experience of 30 cases.
Supplementary Material
Acknowledgments
This research was funded by T32 DK07634 and K24DK100548 from the National Institutes of Health and GI Solutions, a subsidiary of Covidien Medical.
Footnotes
Author Contributions: Sarina Pasricha: study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis; Cary Cotton: analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis; Kelly E. Hathorn: study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content; Nan Li: study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis; William J. Bulsiewicz: study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis; W. Asher Wolf: analysis and interpretation of data, critical revision of the manuscript for important intellectual content, statistical analysis; V. Raman Muthusamy: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Srinadh Komanduri: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Herbert C. Wolfsen: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Ron E. Pruitt: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Atilla Ertan: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Gary W. Chmielewski: study concept and design, acquisition of data, interpretation of data, critical revision of the manuscript for important intellectual content; Nicholas J. Shaheen: study concept and design, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, study supervision.
Relevant Financial Disclosures: Dr. Shaheen receives research funding from CSA Medical, Covidien Medical, NeoGenomics, Takeda Pharmaceuticals and Oncoscope. He is a consultant for Oncoscope. Drs. Muthusamy, Komanduri, Wolfsen, Pruitt, Ertan, and Chmielewski received research funding from Covidien.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–31. doi: 10.1053/j.gastro.2005.08.053. [DOI] [PubMed] [Google Scholar]
- 2.Hvid-Jensen F, Pedersen L, Drewes AM, et al. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med. 2011;365:1375–83. doi: 10.1056/NEJMoa1103042. [DOI] [PubMed] [Google Scholar]
- 3.Sharma P. Clinical practice. Barrett’s esophagus. N Engl J Med. 2009;361:2548–56. doi: 10.1056/NEJMcp0902173. [DOI] [PubMed] [Google Scholar]
- 4.van Soest EM, Dieleman JP, Siersema PD, et al. Increasing incidence of Barrett’s oesophagus in the general population. Gut. 2005;54:1062–6. doi: 10.1136/gut.2004.063685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sikkema M, de Jonge PJ, Steyerberg EW, et al. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–44. doi: 10.1016/j.cgh.2009.10.010. quiz e32. [DOI] [PubMed] [Google Scholar]
- 6.Sharma P, Falk GW, Weston AP, et al. Dysplasia and cancer in a large multicenter cohort of patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2006;4:566–72. doi: 10.1016/j.cgh.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association technical review on the management of Barrett’s esophagus. Gastroenterology. 2011;140:e18–52. doi: 10.1053/j.gastro.2011.01.031. quiz e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–88. doi: 10.1056/NEJMoa0808145. [DOI] [PubMed] [Google Scholar]
- 9.Kim HP, Bulsiewicz WJ, Cotton CC, et al. Focal endoscopic mucosal resection before radiofrequency ablation is equally effective and safe compared with radiofrequency ablation alone for the eradication of Barrett’s esophagus with advanced neoplasia. Gastrointest Endosc. 2012 doi: 10.1016/j.gie.2012.04.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyday WD, Corbett FS, Kuperman DA, et al. Radiofrequency ablation of Barrett’s esophagus: outcomes of 429 patients from a multicenter community practice registry. Endoscopy. 2010;42:272–8. doi: 10.1055/s-0029-1243883. [DOI] [PubMed] [Google Scholar]
- 11.Pasricha S, Bulsiewicz WJ, Hathorn KE, et al. Durability and Predictors of Successful Radiofrequency Ablation for Barrett’s Esophagus. Clin Gastroenterol Hepatol. 2014 doi: 10.1016/j.cgh.2014.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voltaggio L, Montgomery EA, Lam-Himlin D. A clinical and histopathologic focus on Barrett esophagus and Barrett-related dysplasia. Arch Pathol Lab Med. 2011;135:1249–60. doi: 10.5858/arpa.2011-0019-RA. [DOI] [PubMed] [Google Scholar]
- 13.Shaheen NJ, Kim HP, Bulsiewicz WJ, et al. Prior fundoplication does not improve safety or efficacy outcomes of radiofrequency ablation: results from the U.S. RFA Registry. J Gastrointest Surg. 2013;17:21–8. doi: 10.1007/s11605-012-2001-8. discussion p 28–9. [DOI] [PubMed] [Google Scholar]
- 14.Zemlyak AY, Pacicco T, Mahmud EM, et al. Radiofrequency ablation offers a reliable surgical modality for the treatment of Barrett’s esophagus with a minimal learning curve. Am Surg. 2012;78:774–8. [PubMed] [Google Scholar]
- 15.Fudman DI, Lightdale CJ, Poneros JM, et al. Positive correlation between endoscopist radiofrequency ablation volume and response rates in Barrett’s esophagus. Gastrointest Endosc. 2014;80:71–7. doi: 10.1016/j.gie.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Vilsteren FG, Pouw RE, Herrero LA, et al. Learning to perform endoscopic resection of esophageal neoplasia is associated with significant complications even within a structured training program. Endoscopy. 2012;44:4–12. doi: 10.1055/s-0031-1291384. [DOI] [PubMed] [Google Scholar]
- 17.Choi IJ, Kim CG, Chang HJ, et al. The learning curve for EMR with circumferential mucosal incision in treating intramucosal gastric neoplasm. Gastrointest Endosc. 2005;62:860–5. doi: 10.1016/j.gie.2005.04.033. [DOI] [PubMed] [Google Scholar]
- 18.Ohyama T, Kobayashi Y, Mori K, et al. Factors affecting complete resection of gastric tumors by the endoscopic mucosal resection procedure. J Gastroenterol Hepatol. 2002;17:844–8. doi: 10.1046/j.1440-1746.2002.02814.x. [DOI] [PubMed] [Google Scholar]
- 19.Deprez PH, Bergman JJ, Meisner S, et al. Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy. 2010;42:853–8. doi: 10.1055/s-0030-1255563. [DOI] [PubMed] [Google Scholar]
- 20.Wani S, Coté GA, Keswani R, et al. Learning curves for EUS by using cumulative sum analysis: implications for American Society for Gastrointestinal Endoscopy recommendations for training. Gastrointest Endosc. 2013;77:558–65. doi: 10.1016/j.gie.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Montgomery E, Bronner MP, Goldblum JR, et al. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum Pathol. 2001;32:368–78. doi: 10.1053/hupa.2001.23510. [DOI] [PubMed] [Google Scholar]
- 22.Reid BJ, Haggitt RC, Rubin CE, et al. Observer variation in the diagnosis of dysplasia in Barrett’s esophagus. Hum Pathol. 1988;19:166–78. doi: 10.1016/s0046-8177(88)80344-7. [DOI] [PubMed] [Google Scholar]
- 23.Fitzgerald RC, di Pietro M, Ragunath K, et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut. 2014;63:7–42. doi: 10.1136/gutjnl-2013-305372. [DOI] [PubMed] [Google Scholar]
- 24.Manner H, Pech O, Heldmann Y, et al. Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion. Clin Gastroenterol Hepatol. 2013;11:630–5. doi: 10.1016/j.cgh.2012.12.040. quiz e45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.