Abstract
Background
Currently, anorectal manometry (ARM), which is used to diagnose defecatory disorders and identify anal weakness in fecal incontinence (FI) is generally conducted in specialized laboratories. Our aims were to compare anorectal functions measured with high resolution manometry (HRM) and a novel portable manometry device.
Methods
Anal pressures at rest, during squeeze, and simulated evacuation, and rectal sensation were evaluated with portable and HRM in 20 healthy women, 19 women with constipation and 11 with FI. The relationship between anal pressures measured with portable and HRM was assessed by the concordance correlation coefficient [CCC], Bland Altman test, and paired t tests.
Key Results
Anal pressures at rest [CCC 0.45; 95% CI 0.29, 0.58] and during squeeze [CCC 0.60; 95% CI 0.46, 0.72] measured with portable and HRM were correlated and inversely associated with the risk of FI. During simulated evacuation, the CCC for rectal pressure [0.62; 95% CI 0.43, 0.76] was greater than that for anal pressure [CCC 0.22; 95% CI 0.04, 0.39] and the rectoanal gradient [CCC 0.22; 95% CI 0.02, 0.41]. Rectal sensory thresholds for first sensation, the desire to defecate, and urgency measured by portable and HRM were also significantly correlated between techniques. For several parameters, differences between portable and HRM were statistically significant and the Bland Altman test was positive.
Conclusions & Inferences
Anorectal pressures and rectal sensation can be conveniently measured by portable manometry and are significantly correlated with high resolution manometry.
Keywords: anorectal manometry, constipation, fecal incontinence, rectal sensation
Anorectal manometry (ARM) is widely used to diagnose defecatory disorders and identify anal weakness as well as rectal sensory disturbances in fecal incontinence (FI) (1, 2). However, anal manometry is not universally available, requires expertise to perform, and is relatively expensive. We developed the first handheld, portable manometry device to measure rectal and anal pressures and rectal sensation at the bedside. The aims of this study were to (i) compare anorectal pressures measured by portable and high resolution manometry (HRM); (ii) the utility of anorectal pressures for discriminating between healthy women, FI, and chronic constipation; and (iii) participants with normal and abnormal rectal balloon expulsion.
MATERIALS AND METHODS
Experimental Design
This study was approved by the Institutional Review Board at Mayo Clinic. After providing written informed consent, 20 healthy women, 19 constipated women, and 11 women with FI underwent HRM and portable manometry and a rectal balloon expulsion test with validated techniques on the same day (3, 4). Constipated participants had symptom criteria for functional constipation or constipation-predominant irritable bowel syndrome (5), while women with FI had at least one episode of FI unrelated to a temporary diarrheal illness in the past year. Exclusion criteria were: significant systemic diseases, medications that can anorectal motility or sensation, and prior pelvic radiation or inflammatory bowel disease. Healthy participants did not have symptoms of a functional bowel disorder assessed by Rome criteria, putative risk factors for pelvic floor trauma, or anxiety, or depression as assessed by a questionnaire (6, 7). The severity of fecal incontinence was rated by the Fecal Incontinence and Constipation Assessment (FICA) severity scale (7, 8).
During HRM and portable manometry, pressures were evaluated at rest (20 seconds), three squeeze maneuvers (20 seconds each), and two simulated evacuation maneuvers (before and during rectal distention). Then, rectal sensation was evaluated during stepwise rectal distention. The HRM catheter (Given Imaging) and analysis platform are described elsewhere (3). The eSleeve option program reduces data from multiple, typically 9, equidistant anal sensors, to a single value at each point in time, i.e., the greatest pressure across all anal sensors at 10Hz during rest and squeeze. Summary parameters were calculated as follows: (i) Rest - An average of eSleeve values across 20 seconds at rest, (ii) Squeeze - The maximum eSleeve pressure recorded for 2s during each of 3 maneuvers was obtained. Then, an average of these 3 maximum pressures was calculated. (iii) Simulated evacuation – The eSleeve identified the 3 second period during simulated evacuation when the rectoanal gradient was most positive.
The portable manometry system includes a catheter, with 4 radially-oriented anal and 1 rectal balloon, a wireless manometer, and a computer (Figure). Summary parameters were calculated as follows: (i) Rest – Pressures were averaged for all 4 balloons over 20 seconds. (ii) Squeeze - The maximum pressure recorded by any balloon during 20s was used. (iii) Simulated evacuation – The rectoanal gradient calculated over the 5s period when this was most positive. Anal pressure was averaged across all 4 sensors for this calculation.
Figure.
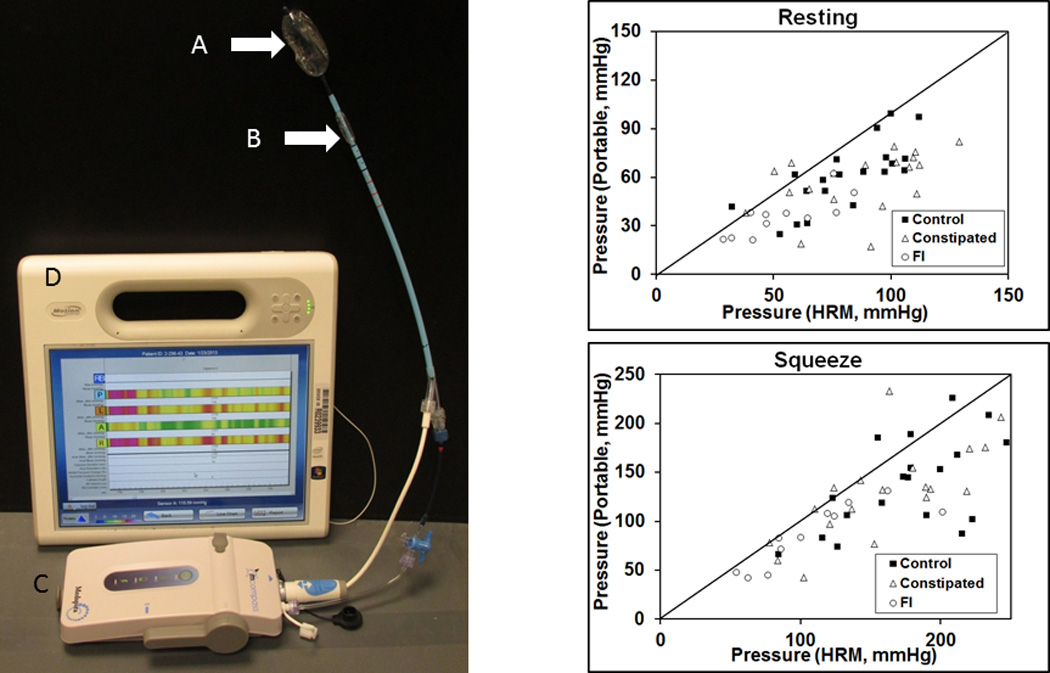
Left panel. Portable manometry device. The device comprises three components: a catheter with (A) rectal and (B) 4 radial anal balloons (arrows, 20 mm long), which is connected to (C) a manometer, that communicates via wireless with (D) a computer. The acquisition module display provides instructions that guide users throughout the study. Right panel. Comparison of anal resting (upper panel) and squeeze pressures (lower panel) measured with HRM and portable manometry.
These endpoints were compared with Lin’s concordance correlation coefficient (CCC)(9), paired t tests, and Bland-Altman plots (10). Logistic regression models evaluated whether rectoanal pressures could discriminate between healthy women and FI, healthy women and constipation, and women with normal and prolonged rectal balloon expulsion times. Except where stated otherwise, data are summarized as Mean ± SEM.
RESULTS
Women with FI (55 ± 3 years) were older (P=.02) than healthy women (age 44 ± 4 years) and patients with chronic constipation (41 ± 2 years). The FICA score suggested mild (4 patients), moderate (6 patients) or severe FI (1 patient) with duration of less than 2 (n=4), between 2–10 (n=6), and greater than 10 years (n=1); 2 had passive FI, 6 had isolated urge FI, and 3 did not meet criteria for either passive or urge FI.
Comparison of Anorectal Parameters in All Participants
Rectoanal pressures and rectal sensory thresholds measured with both techniques were significantly correlated (Table 1). However resting and squeeze pressures and the anal pressure during evacuation measured with portable manometry were lower (Figure). For some comparisons (e.g., resting pressure), the Bland-Altman plot was significant, indicating that differences between techniques were related to the average pressure measured with both techniques.
Table 1.
Comparison of Anorectal Parameters in All Participants
| Variable | HRM | Portable Manometry |
HRM vs Portable Manometry | ||
|---|---|---|---|---|---|
| CCC (95% CI) |
Bland- Altmana |
P valueb | |||
| Anal average rest pressure | 77±4 | 54±3 | .45 (.29, .58) | .04 | 0.0001 |
| Maximum anal squeeze | 158±8 | 125±17 | .60 (.46, .72) | .12 | 0.0001 |
| Anal pressure during Valsalva maneuver | 126±8 | 72±4 | .29 (.16, .34) | <0.0001 | 0.0001 |
| Simulated evacuation without rectal distention | |||||
| Rectal pressure | 37±4 | 35±3 | .62 (0.43, .76) | .02 | 0.67 |
| Anal pressure | 80±4 | 53±3 | .22 (.04, .39) | .32 | 0.0001 |
| Rectoanal gradient | −42±5 | −17±4 | .22 (.02, .41) | .34 | 0.0001 |
| Anal relaxation | 8±6 | −24±8 | .39 (.19, .56) | .04 | .0001 |
| Simulated evacuation with rectal distention | |||||
| Rectal pressure | 30±4 | 41±3 | .31 (.07, .51) | .04 | 0.0001 |
| Anal pressure | 75±5 | 47±3 | .15 (−.01, .30) | .0002 | 0.0001 |
| Rectoanal gradient | −45±6 | −6±4 | .25 (.10, .40) | .003 | 0.0001 |
| Anal relaxation | 12±4 | −69±46 | .05 (.01, .09) | <.0001 | .081 |
| First sensation (mL) | 55±4 | 49±4 | 0.53 (.31, .70) | .16 | 0.12 |
| Desire to defecate (mL) | 85±5 | 82±4 | 0.53 (.29, .70) | .07 | 0.5 |
| Urgency (mL) | 121±7 | 113±5 | 0.46 (.20, .66) | .03 | 0.37 |
Abbreviation: HRM, high-resolution manometry
Test for (Pearson) correlation of differences versus overall mean.
Paired comparison between HRM and portable manometry
Differences between Healthy Participants, Constipation, and Fecal Incontinence
Higher anal resting and squeeze pressures measured with HRM and separately with portable manometry were associated with a lower risk of FI (Table 2). Except for the rectoanal gradient measured with HRM, rectoanal pressures measured without (Table 2) and with balloon distention (data not shown) did not discriminate between health and constipation. However, only 6 participants (1 healthy woman, 4 constipated patients, and 1 woman with FI) had a prolonged (i.e., greater than 60 seconds) BET.
Table 2.
Utility of Anorectal Pressures for Discriminating between Healthy Controls, Constipation, and Fecal Incontinence
| Pressure | Controls | Constipation | Fecal Incontinence |
Univariate Odds Ratio (95% CI) |
Univariate Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Controls vs constipation |
Controls vs FI | ||||
| High resolution manometry | |||||
| Anal resting pressure | 81±5 | 86±6 | 54±6 | 1.01(.98, 1.04) | .95(.91, .99) |
| Anal squeeze pressure | 182±11 | 160±11 | 110±13 | .99(.98, 1.004) | .97(.95, .99) |
| Rectal pressure – SE | 41±4 | 27±5 | 48±11 | .96(.93, 1.00) | 1.00(.98, 1.03) |
| Anal pressure – SE | 75±4 | 90±7 | 70±12 | 1.02(.99, 1.05) | 0.99(.96, 1.03) |
| Rectoanal gradient | −34±4 | −63±8 | −22±9 | .96(.94, .99) | 1.02(.99, 1.06) |
| Anal relaxation (%) | 18±9 | 6±6 | −7±18 | .99(.97, 1.01) | .98(.96, 1.01) |
| Portable manometry | |||||
| Anal resting pressure | 60±5 | 57±4 | 36±4 | .99(.96, 1.03) | .93(.88, .98) |
| Anal squeeze pressure | 142±11 | 129±11 | 86±9 | .99(.98, 1.01) | .97(.95, .995) |
| Rectal pressure – SE | 39±4 | 32±4 | 41±7 | .98(.94, 1.02) | 1.0(.96, 1.05) |
| Anal pressure – SE | 66±5 | 63±6 | 48±6 | .99(.97, 1.02) | .97(.93, 1.01) |
| Rectoanal gradient | −17±5 | −23±8 | −5±5 | .99(.97, 1.02) | 1.02(.99, 1.05) |
| Anal relaxation (%) | −24±12 | −15±10 | −44±24 | 1.0 (0.99, 1.02) | 1.0 (0.98, 1.01) |
Abbreviations: FI, fecal incontinence; SE, simulated evacuation. Bold font represents findings that are statistically significant
Comparison of Anorectal Pressures during Simulated Evacuation and Rectal Balloon Expulsion Time
The median (interquartile range) rectal balloon expulsion time (BET) was 6 (4–16) seconds in controls, 15 (5–52) seconds in constipated patients, and 6 (5–17) seconds in FI. The BET was associated with the rectoanal gradient during simulated evacuation measured with HRM (hazard ratio [HR] 1.02; 95% CI 1.01–1.03) and portable manometry (HR 1.02; 95% CI, 1.00–1.04). A HR of >1 implies that balloon expulsion occurred earlier (i.e., BET was shorter) when the rectoanal gradient was greater. The HR for rectal pressure during evacuation versus BET were (1.01; 95% CI, 1.00–1.04) for HRM and (1.02; 95% CI, 1.00–1.04) for portable manometry. Conversely, the HR for minimum anal pressure during evacuation were <1 for HRM (HR 0.99; 95% CI, 0.98–1.00) and portable manometry (HR 0.99; 95% CI, 0.97–0.999), which indicates that the BET was longer when the minimum anal pressure during evacuation was greater.
DISCUSSION
While these devices employ different pressure sensing technologies, pressure measurements and rectal sensory thresholds measured with both devices were correlated, which supports the criterion validity of measuring anorectal pressures with portable manometry (11). The inclusion of healthy women and women with constipation and FI enabled the techniques to be compared across a range of pressures and also permitted the utility of the device for discriminating between health and disease to be assessed. HRM pressures in this study were comparable to our previous study (3), but significantly greater than pressures measured with portable manometry, probably because the eSleeve analysis in the HRM system only uses the highest pressure along the longitudinal axis of the anal canal to calculate anal resting and squeeze pressure at every instant in time. In contrast, the portable catheter measures pressures along a 2 cm span in each of 4 quadrants. Thus, the eSleeve option can bias toward higher pressures. Allowing for differences in techniques, definitions (e.g., for resting pressure), subject characteristics, and age cutoffs, the pressure values recorded by portable manometry were comparable to pressures recorded by traditional (water-perfused or solid-state) manometry (e.g., anal resting pressure of 67–75 mm Hg in younger and 48–62 mm Hg in older women) (12–14).
Anorectal parameters measured with HRM and portable manometry were of comparable utility for discriminating between controls and patients with constipation and FI, which also supports the criterion validity of the device (11). Anal resting and squeeze pressures measured by HRM and portable manometry were lower in women with FI than in controls even after adjusting for age (15–17). Likewise, rectal pressure, minimum anal pressure, and the rectoanal gradient during simulated evacuation measured by HRM and portable manometry discriminated between participants with a normal and prolonged BET, which is indicative of pelvic floor dysfunction. Many healthy women had a negative rectoanal gradient during simulated evacuation with HRM (3, 18), and to a lesser extent, with portable manometry, which highlights the limited utility of this variable for discriminating between healthy people and patients with defecatory disorders
During rectal balloon distention, sensory thresholds measured by both devices were correlated and not significantly different. Although different, the balloons used for HRM and portable manometry have similar dimensions at comparable distending volumes, i.e., for HRM, balloon dimensions at 60 mL (48 mm long and 46 mm wide) and 120 mL (60 mm long and 58 mm wide) and for portable manometry, at 60 mL (50 mm long and 51 mm wide) and 120 mL (53 long and 63 mm wide). As observed previously (19, 20), rectal sensory threshold volumes measured by portable manometry were lower in FI.
This bedside device is portable, hence offers convenience. While the precise time required to conduct the procedure depends on rectal sensation (i.e., the pressure required to reach urgency), in general, data acquisition takes 10 minutes or less. Thereafter, the program uses the event markers identified during data collection to summarize anorectal parameters in a report, which generally takes two minutes.
While the study was conducted with rigorous techniques, it has its limitations. We enrolled only 20 healthy women because the objective was to validate pressure measurements rather than generate normal values. A larger dataset of healthy participants is necessary to define normal values for portable manometry in men and women, particularly because normal values are lower with portable than HRM. Further studies should assess the usability of this device for experienced and novice users. In summary, our observations suggest that anorectal pressures and rectal sensation can be conveniently and accurately measured by portable manometry.
Key Messages.
Anorectal manometry (ARM) is widely used for identifying anorectal sensorimotor dysfunctions in patients with constipation and fecal incontinence. At present, anorectal manometry is generally performed in specialized laboratories, requires expertise, and is expensive.
We compared anorectal pressures and rectal sensation measured by a handheld, portable manometry device and high resolution manometry in 20 healthy women, 19 constipated women, and 11 women with fecal incontinence.
Anal pressures at rest and during squeeze measured with portable and HRM were correlated but lower with portable manometry.
During simulated evacuation, rectoanal pressures measured with both techniques were correlated and discriminated between participants with normal and prolonged balloon expulsion time.
Acknowledgments
Funding: This study was supported by a grant from Medspira Inc, by Grant Number DK 78924 from the National Institutes of Health to Dr. Bharucha, and by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Author Contributions:
AEB, RS, and ARZ designed the research study.
KF conducted the anorectal studies and analyzed the data.
LAS reviewed the data.
ARZ conducted the statistical analysis.
AEB and ARZ wrote the paper.
All authors approved the final version of this manuscript.
Disclosures: Dr. Bharucha and Mr. Stroetz are inventors of the portable manometry catheter used in this research that has been licensed to Medspira Inc. Dr. Bharucha, Mr. Stroetz, and Mayo Clinic have contractual rights to receive royalties from the licensing of this technology. Mayo Clinic holds equity in the company to which the technology is licensed. This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and is being conducted in compliance with Mayo Clinic Conflict of Interest policies.
REFERENCES
- 1.Bharucha AE, Rao SSC. An update on anorectal disorders for gastroenterologists. Gastroenterology. 2014;146:37.e2–45.e2. doi: 10.1053/j.gastro.2013.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wald A, Bharucha AE, Cosman BC, Whitehead W. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109:1141–1157. doi: 10.1038/ajg.2014.190. [DOI] [PubMed] [Google Scholar]
- 3.Noelting J, Ratuapli SK, Bharucha AE, Harvey D, Ravi K, Zinsmeister AR. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012;107:1530–1536. doi: 10.1038/ajg.2012.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratuapli S, Bharucha AE, Harvey D, Zinsmeister AR. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil. 2013;25:e813–e820. doi: 10.1111/nmo.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 6.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 7.Bharucha AE, Locke GR, Seide BM, Zinsmeister AR. A new questionnaire for constipation and faecal incontinence. Aliment Pharmacol Ther. 2004;20:355–364. doi: 10.1111/j.1365-2036.2004.02028.x. [DOI] [PubMed] [Google Scholar]
- 8.Bharucha AE, Zinsmeister AR, Locke GR, Schleck C, McKeon K, Melton LJ. Symptoms and quality of life in community women with fecal incontinence. Clin Gastroenterol Hepatol. 2006;4:1004–1009. doi: 10.1016/j.cgh.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead WE, Palsson OS, Levy RL, Feld AD, VonKorff M, Turner M. Reports of "satisfactory relief" by IBS patients receiving usual medical care are confounded by baseline symptom severity and do not accurately reflect symptom improvement. Am J Gastroenterol. 2006;101:1057–1065. doi: 10.1111/j.1572-0241.2006.00535.x. [DOI] [PubMed] [Google Scholar]
- 10.Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346:1085–1087. doi: 10.1016/s0140-6736(95)91748-9. [DOI] [PubMed] [Google Scholar]
- 11.Bland JM, Altman DG. Statistics Notes: Validating scales and indexes. BMJ. 2002;324:606–607. doi: 10.1136/bmj.324.7337.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bannister JJ, Abouzekry L, Read NW. Effect of aging on anorectal function. Gut. 1987;28:353–357. doi: 10.1136/gut.28.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jameson JS, Chia YW, Kamm MA, Speakman CT, Chye YH, Henry MM. Effect of age, sex and parity on anorectal function. Br J Surg. 1994;81:1689–1692. doi: 10.1002/bjs.1800811143. [DOI] [PubMed] [Google Scholar]
- 14.Fox JC, Fletcher JG, Zinsmeister AR, Seide B, Riederer SJ, Bharucha AE. Effect of aging on anorectal and pelvic floor functions in females. Dis Colon Rectum. 2006;49:1726–1735. doi: 10.1007/s10350-006-0657-4. [DOI] [PubMed] [Google Scholar]
- 15.Mittal RK, Sheean G, Padda BS, Lieber R, Raj Rajasekaran M. The external anal sphincter operates at short sarcomere length in humans. Neurogastroenterol Motil. 2011;23 doi: 10.1111/j.1365-2982.2011.01700.x. 643-e258. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE, Edge J, Zinsmeister AR. Effect of nifedipine on anorectal sensorimotor functions in health and fecal incontinence. Am J Physiol Gastrointest Liver Physiol. 2011;301:G175–G180. doi: 10.1152/ajpgi.00557.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bharucha AE, Daube J, Litchy W, Traue J, Edge J, Enck P, Zinsmeister AR. Anal sphincteric neurogenic injury in asymptomatic nulliparous women and fecal incontinence. Am J Physiol Gastrointest Liver Physiol. 2012;303:G256–G262. doi: 10.1152/ajpgi.00099.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrington EV, Brokjaer A, Craven H, Zarate N, Horrocks EJ, Palit S, Jackson W, Duthie GS, et al. Traditional measures of normal anal sphincter function using high-resolution anorectal manometry (HRAM) in 115 healthy volunteers. Neurogastroenterol Motil. 2014;26:625–635. doi: 10.1111/nmo.12307. [DOI] [PubMed] [Google Scholar]
- 19.Andrews C, Bharucha AE, Camilleri M, Low PA, Seide B, Burton D, Baxter K, Zinsmeister AR. Rectal sensorimotor dysfunction in women with fecal incontinence. Am J Physiol Gastrointest Liver Physiol. 2007;292:G282–G289. doi: 10.1152/ajpgi.00176.2006. [DOI] [PubMed] [Google Scholar]
- 20.Chan CL, Scott SM, Williams NS, Lunniss PJ. Rectal hypersensitivity worsens stool frequency, urgency, and lifestyle in patients with urge fecal incontinence. Dis Colon Rectum. 2005;48:134–140. doi: 10.1007/s10350-004-0774-x. [DOI] [PubMed] [Google Scholar]


